Filtration, Reabsorption and Secretion
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
125 Terms
urine production begins with the filtration of ___________. this filtrate is modified through both tubular ____________ and ____________. what reaches the collecting duct is urine.
plasma, reabsorption, secretion
urine is formed by ___________ then by _____________ and _____________.
filtration, reabsorption, secretion
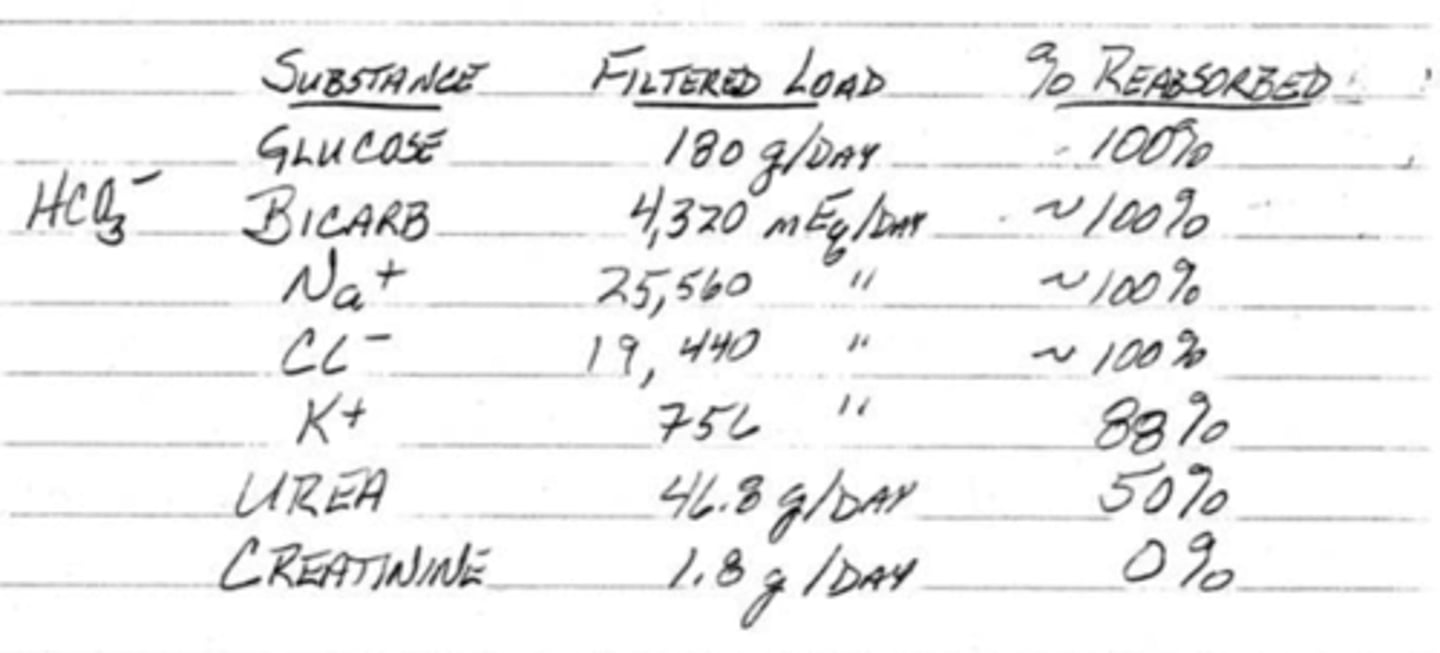
(t/f) all substances in plasma will go through filtration, reabsorption, and secretion, no matter it's composition
false; substances are handled differently. some may not be filtered, reabsorbed, or secreted while some may only be filtered and so on
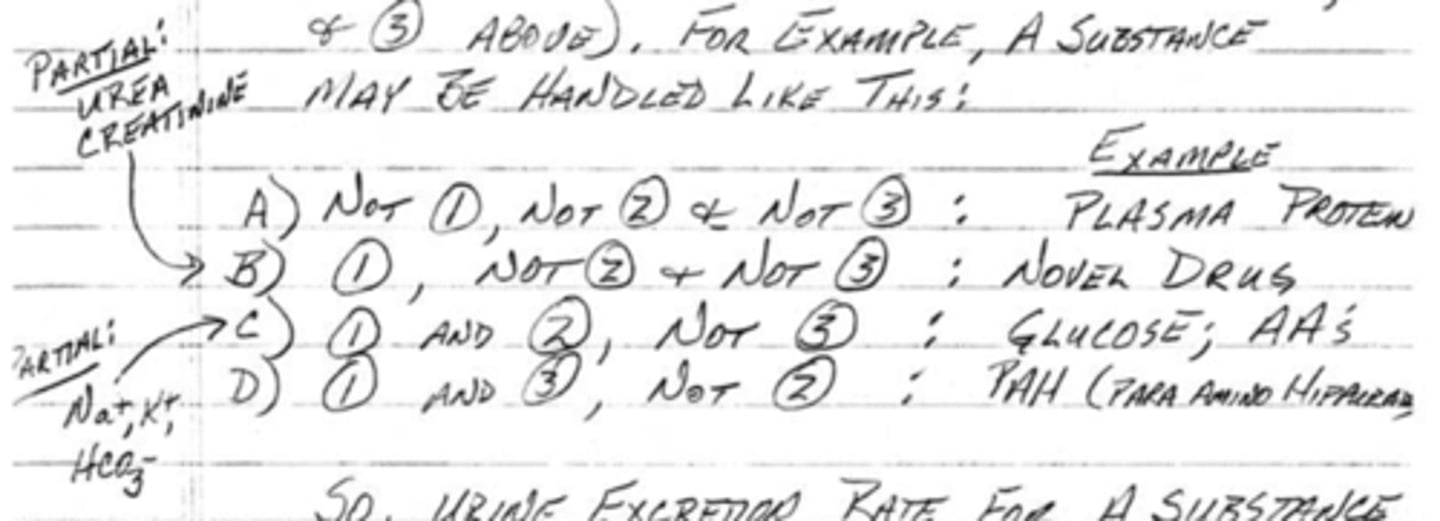
what is the formula for urine excretion rate?
filtration - reabsorption + secretion
(t/f) plasma proteins will be filtered, reabsorbed, and secreted
false; plasma proteins do not go through any of these processes
(t/f) novel drugs (as well as urea and creatinine) will be filtered, reabsorbed, and secreted
false; novel drugs will be filtered, but not reabsorbed or secreted
(t/f) glucose and amino acids (as well as Na+, K+, and HCO3-) will be filtered, reabsorbed, and secreted
false; glucose and amino acids will be filtered and reabsorbed, but not secreted
(t/f) PAH (para-amino hippurate) will be filtered, reabsorbed, and secreted
false; PAH (para-amino hippurate) will be filtered and secreted, but not reabsorbed
where does filtration occur?
in the glomerulus; the plasma is filtered by the glomerulus and then into Bowman's capsule
(t/f) when blood is filtered in the glomerulus, there is a complete but temporary loss of everything in the tubular filtrate from the body
true
what is the glomerular filtration rate? how much is filtrate is filtered per day?
the amount of filtrate the kidneys produce each minute; 180 liters per day (plasma volume of the body is only 3 liters)
plasma is entirely filtered ____ times per day or ____ times per hour
60, 2.5
how many times is ECF filtered per day?
13
what are 2 reasons as to why it is necessary to filter 180 liters of plasma per day if it will just be reabsorbed?
1. allows the kidneys to rapidly and precisely regulate the extracellular volume and content
2. allows the kidneys to get rid of novel compounds in the blood
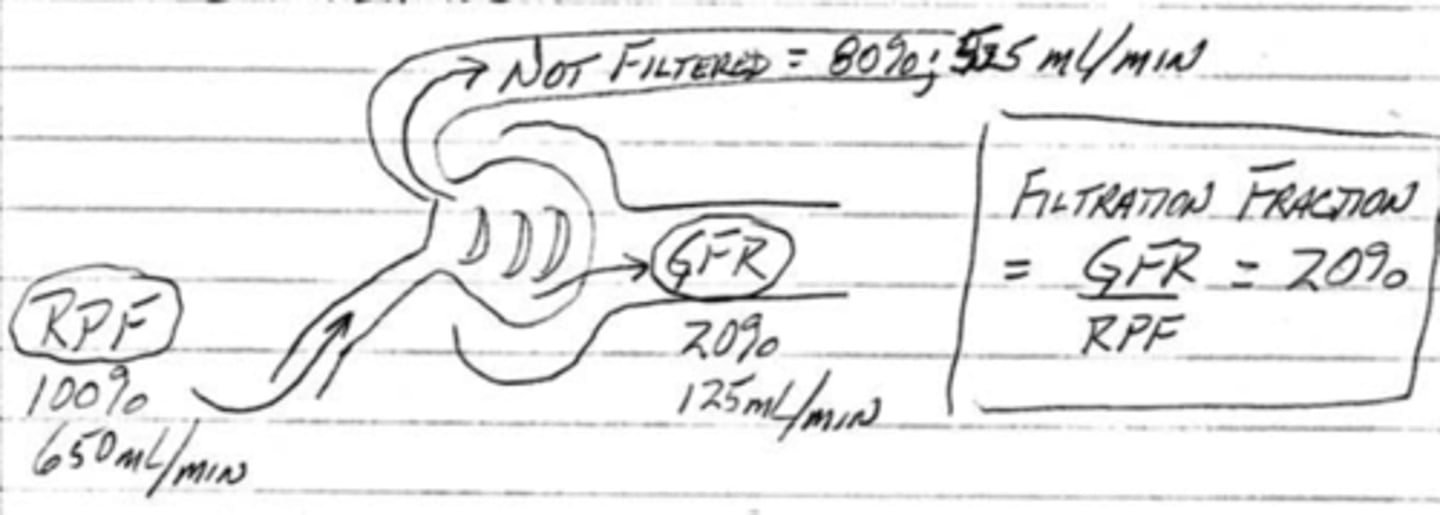
GFR is _____% of the renal plasma flow. what does this mean in terms of the plasma that flows to the kidney per minute?
20; out of the 650 ml per min of plasma that flows to the kidneys, only 20% of it (125 ml) becomes filtrate, while the remaining 80% (525 ml) stays as plasma and enters the peritubular capillaries
filtration is accomplished by the glomerular filter. what are the 3 layers/components of this structure?
1. capillary endothelium
2. basement membrane
3. podocytes
what are the cells that contain foot processes and form slit pores in the glomerular filter?
podocytes
(t/f) plasma proteins along with water, ions, glucose, and urea are able to pass through the foot processes of podocytes
false; plasma proteins cannot freely pass through the podocytes
renal diseases like proteinuria and albuminuria may occur due to defects in what structure of the glomerular filter?
defects in the foot processes of podocytes
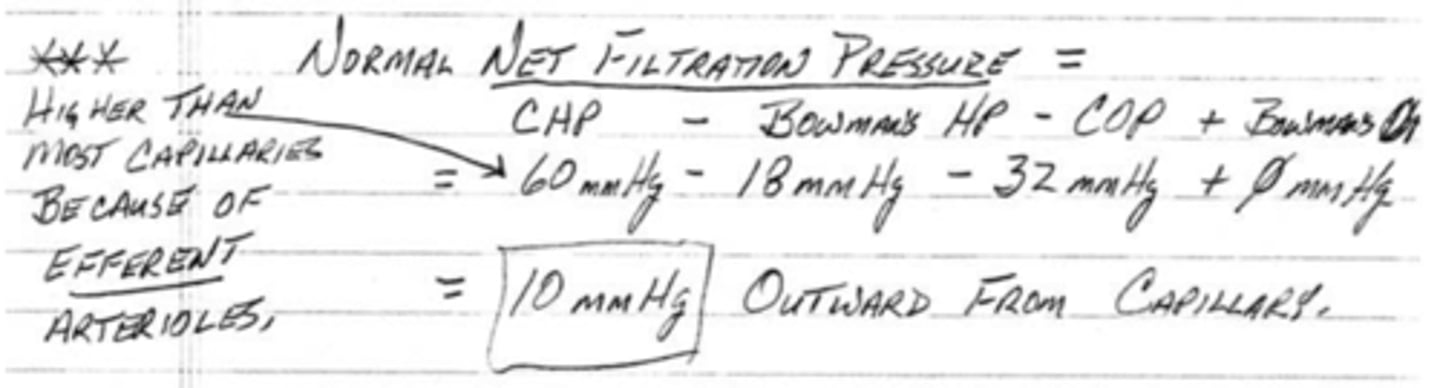
what is the normal net filtration pressure out of the capillary and into the Bowman's capsule?
10 mmHg
what is renal clearance?
volume of plasma (ml/min) cleared of a particular substance in a given time
if X is filtered, but not secreted or absorbed, then what is the renal clearance equal to?
glomerular filtration rate (125 ml/min)
if X is filtered and secreted, then what is the renal clearance equal to?
renal plasma flow; this is greater than the GFR, because more of this substance, later on, will be secreted
if X is filtered and reabsorbed, then what is the renal clearance equal to?
0; the substance was not cleared out of the body
what is the renal clearance of glucose in a healthy adult equal to? what would it be in someone with diabetes?
0; glucose would be filtered but not reabsorbed leading to a renal clearance greater than 0 ml/min
what is the formula for renal clearance?
Cx = ([substance in urine] * (volume of urine))/[substance in plasma]
![<p>Cx = ([substance in urine] * (volume of urine))/[substance in plasma]</p>](https://knowt-user-attachments.s3.amazonaws.com/c0fcf9ca-3edb-41dc-b00d-d9d78087325e.jpg)
by comparing renal clearances of substances, you can determine if a compound is _______________ or _______________
reabsorbed, secreted
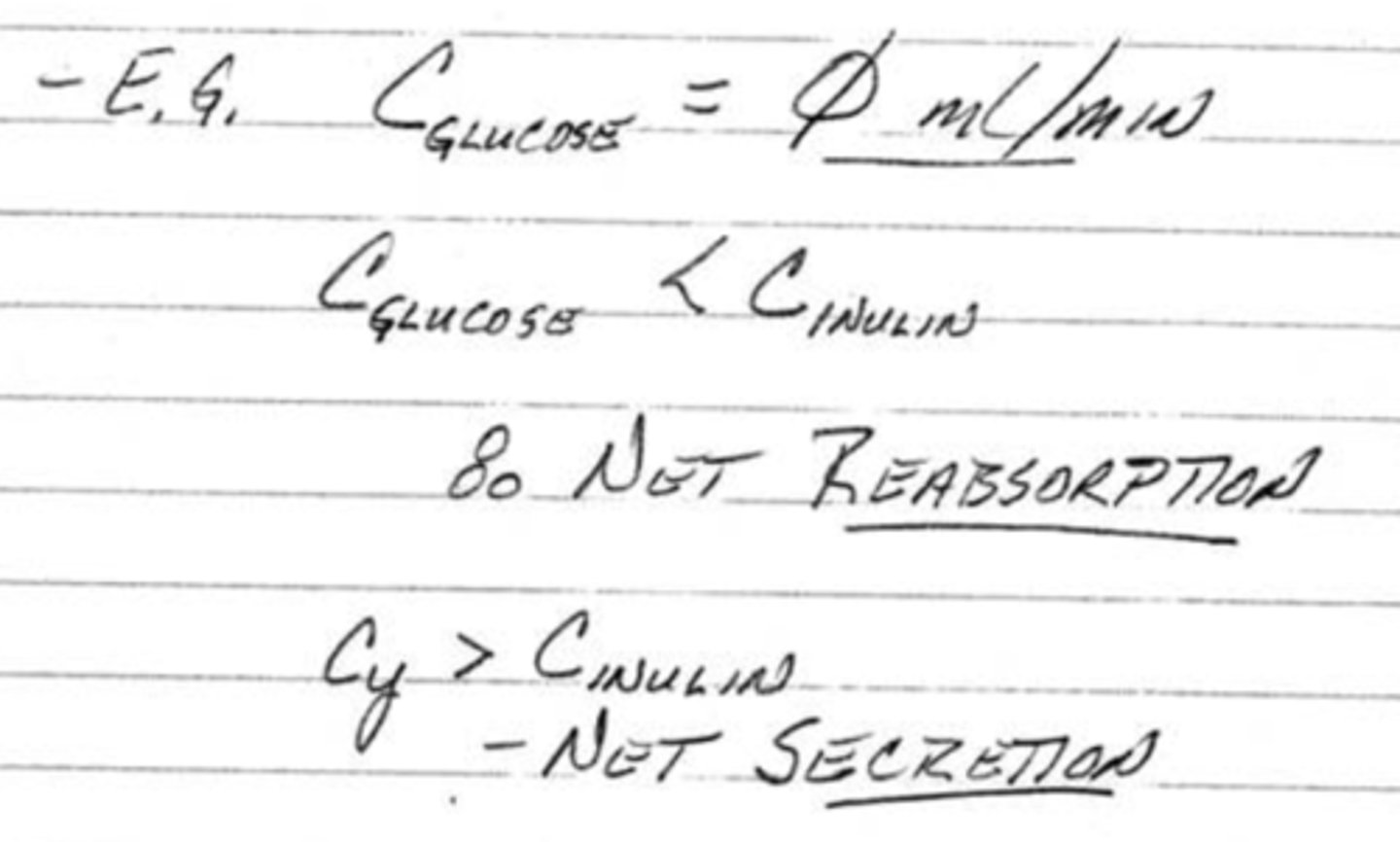
what does a renal clearance between 0 and 125 mean?
partial reabsorption
what does a renal clearance between 125 and 650 mean?
partial secretion
what does a renal clearance equal to 650 mean?
the substance has been completely secreted
how do kidney stones affect the GFR?
a decrease in the GFR because of the blockage not allowing for adequate flow and also resulting in higher hydrostatic pressure in bowman's capsule
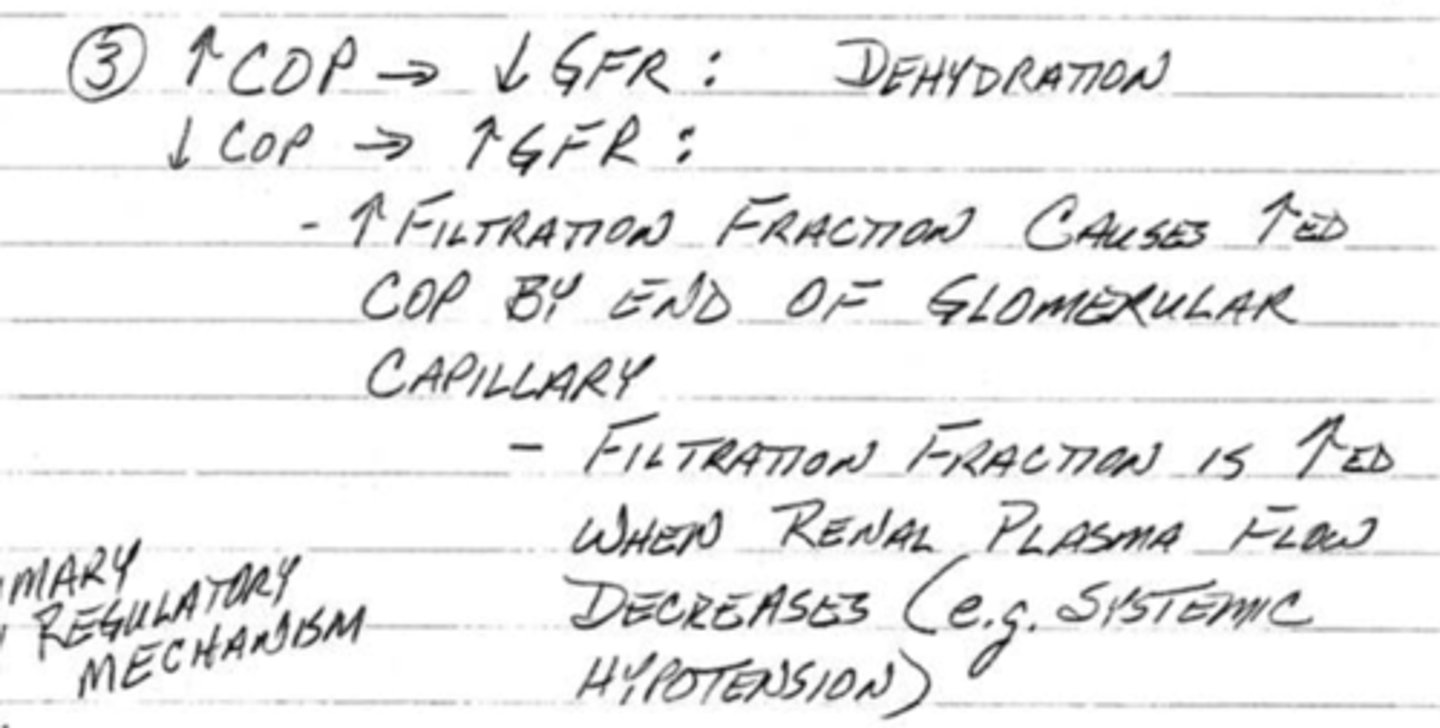
how does dehydration affect the GFR?
decrease in GFR because there is an increase in the concentration of the plasma protein (resulting in more osmotic pressure)
capillary osmotic pressure and glomerular filtration rate are (directly/inversely) correlated
inversely
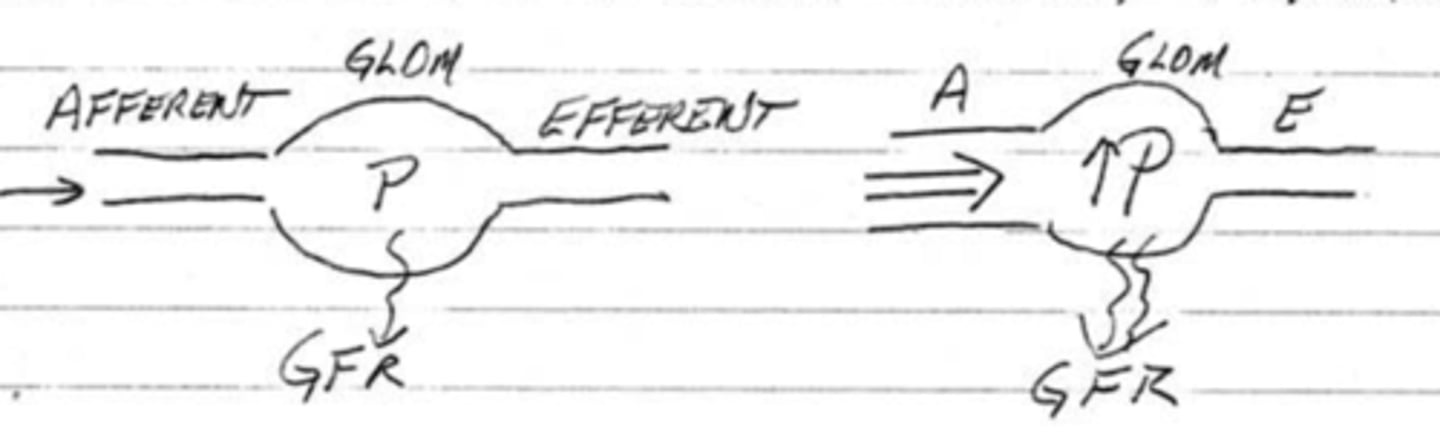
capillary hydrostatic pressure and glomerular filtration rate are (directly/inversely) correlated
directly; this is the primary regulatory mechanism
glomerular capillary hydrostatic pressure is under control of 3 variables. they are ____________, ____________ _____________, and __________ ____________ resistance.
systemic, afferent arteriole, efferent arteriole
the GFR will increase if the systemic pressure (decreases/increases)
increases
the GFR will increase if the afferent arteriole (vasoconstricts/vasodilates)
vasodilates
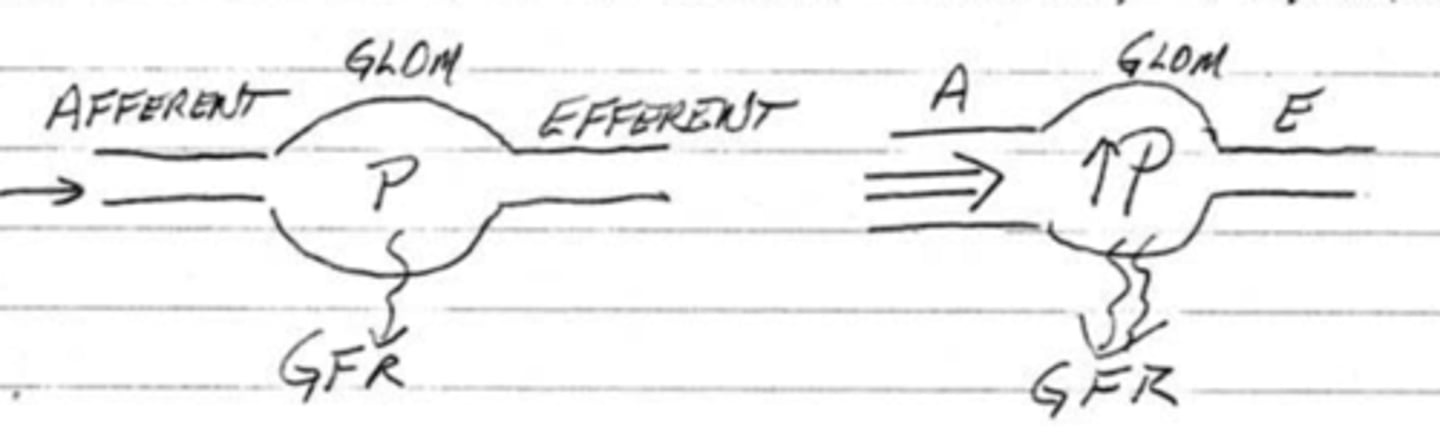
the GFR will increase if the efferent arteriole (vasoconstricts/vasodilates)
vasoconstricts
(t/f) primary regulation of GFR is done by systemic pressure, not by the pressure of the afferent and efferent arterioles
false; the primary regulation is done by the arterioles as the systemic pressure is buffered by autoregulation
what happens to the filtration fraction if both the afferent and efferent arterioles are dilated?
a decrease in the filtration fraction
what happens to the filtration fraction if both the afferent and efferent arterioles are constricted?
an increase in the filtration fraction
what is filtration fraction?
percentage of total plasma volume that filters into the tubule; FF = GFR/RPF
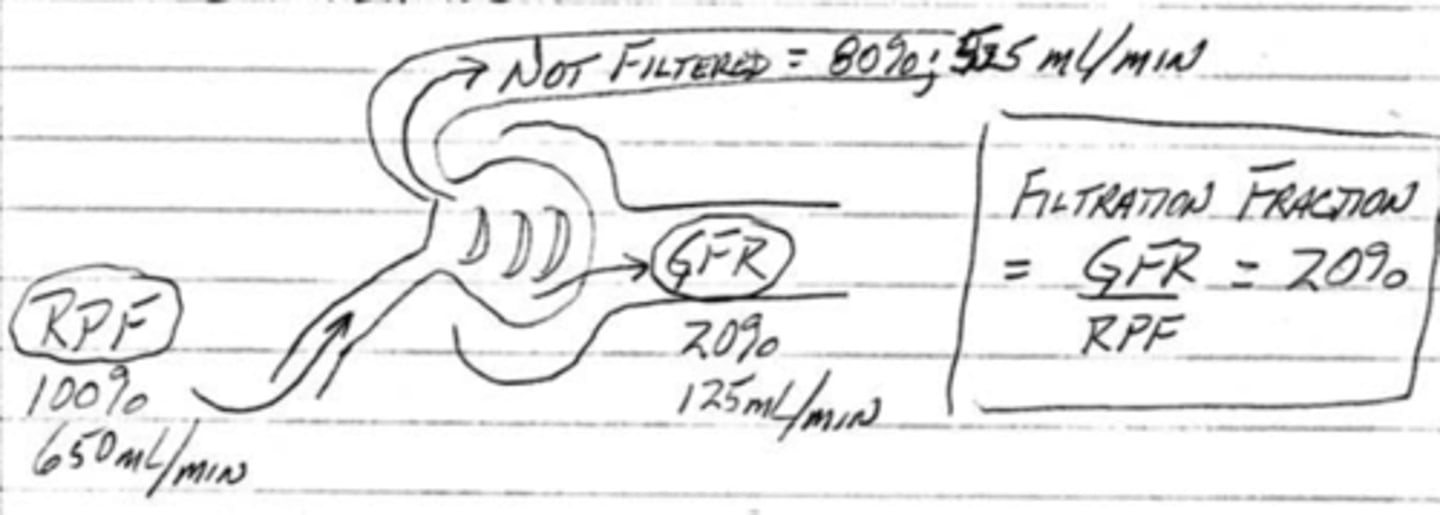
what is renal plasma flow?
the rate of plasma flowing through the kidney (625 ml/min)
(parasympathetics/sympathetics) will reduce the total renal blood flow therefore decreasing GFR
sympathetics
(parasympathetics/sympathetics) will increase the total renal blood flow therefore increasing GFR
parasympathetics
how does norepinephrine, epinephrine, and endothelin affect afferent and efferent arterioles?
causes constriction which decreases renal blood flow and GFR
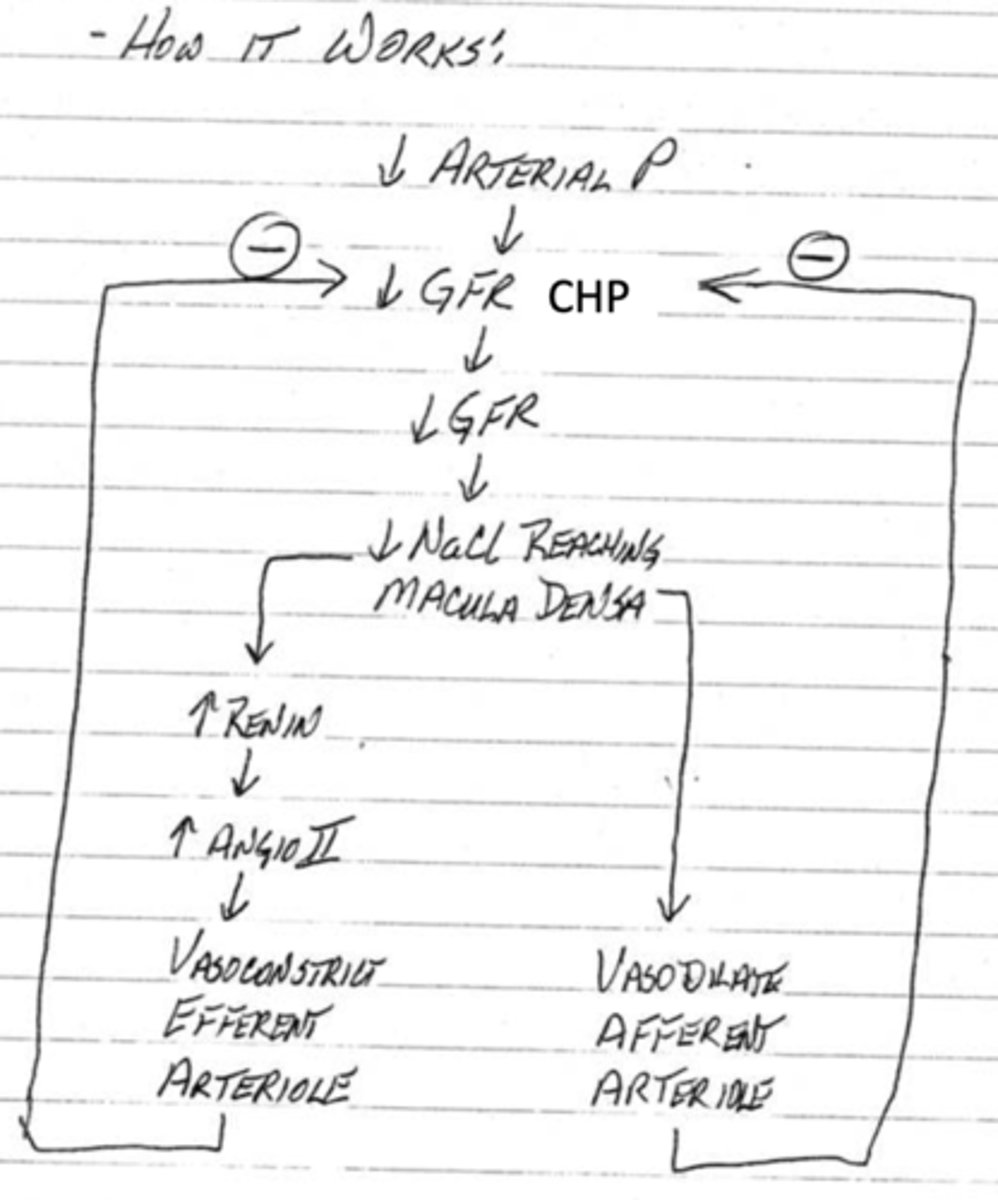
how does angiotensin ii affect efferent arterioles?
causes powerful constriction of the efferent arterioles which increases GFR
how does nitric oxide affect afferent and efferent arterioles?
produces vasodilation which increases GFR
prostaglandins, like aspirin, are weak (vasoconstrictors/vasodilators) and counter severe (vasoconstriction/vasodilation) which will (decrease/increase) GFR
vasodilators, vasoconstriction, decrease
what is regulating GFR to be 180 liters per day?
autoregulation; even though systemic pressure is different between people, the range of 75-160 mmHg has little effect in GFR
an increase in blood pressure results in a(n) (decrease/increase) in urination
increase
what is the name of the system that regulates the autoregulation crucial for GFR stability?
tubuloglomerular feedback
what is the purpose of the macula densa found in the (distal/proximal) convoluted tubule?
distal; monitors the Na+ and Cl- concentration
describe how the tubuloglomerular feedback works
1. arterial pressure decreases cause a decrease in GFR and CHP
2. the decrease in GFR means there is a decrease in NaCl reaching the macula densa
3. this drop will directly cause the afferent arteriole to dilate
4. this drop will also cause an increase in renin which causes an increase in angiotensin ii which then causes the efferent arteriole to constrict
5. both of these changes will inhibit the decrease in GFR and CHP
(t/f) intrinsic smooth muscle contraction will also play a role in autoregulation along with the macula densa
true
urine output is largely regulated by how much filtrate is (reabsorbed/secreted)
reabsorbed
bulk reabsorption takes place in the (distal/proximal) convoluted tubule
proximal
fine-tuning reabsorption takes place in the (distal/proximal) convoluted tubule
distal
(t/f) fine-tuning reabsorption can take place in the collecting tubules
true
(t/f) tubular reabsorption is not very selective. instead it is highly permeable to many substances.
false; it is highly selective
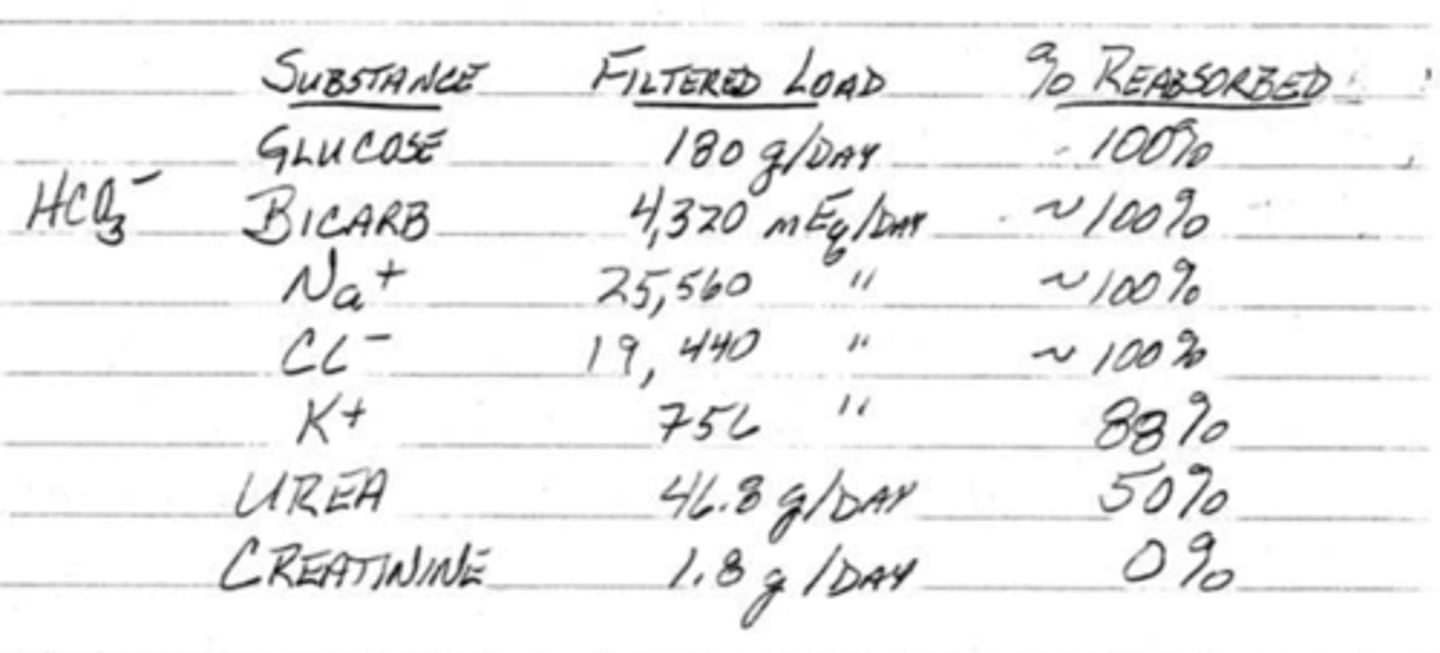
(t/f) it is very easy for the body to get rid of creatinine and urea
false; creatinine is easy to get rid of, but urea is hard to get rid of entirely
(t/f) reabsorption is a purely passive activity driven by differences in concentration
false; reabsorption has both passive and active components
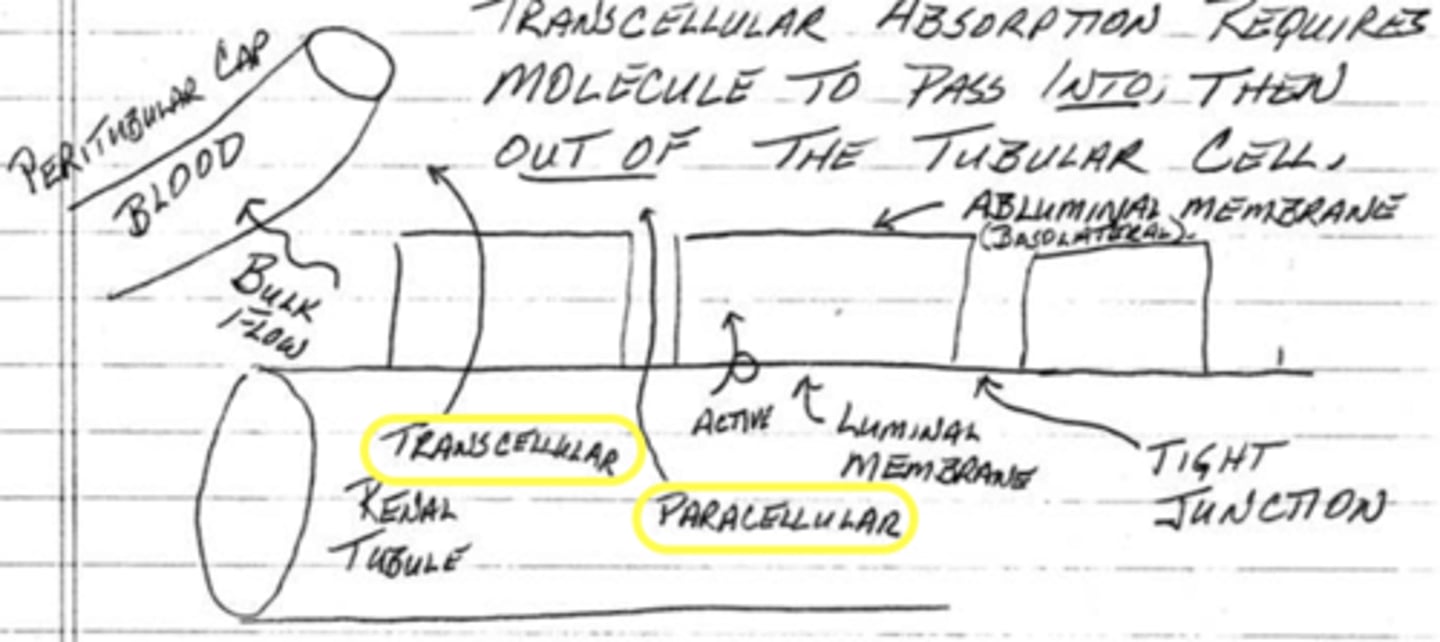
what are the 2 ways that reabsorption can take place?
1. across tubular cells (transcellular)
2. between tubular cells (paracellular)
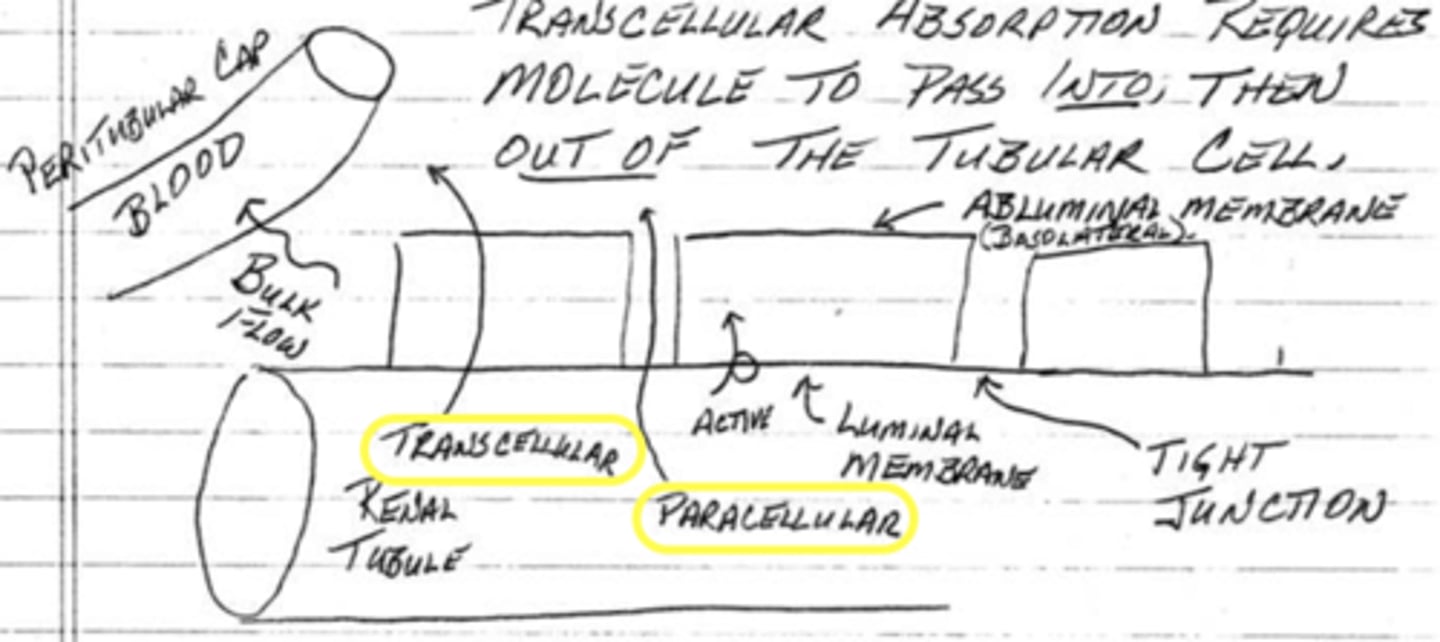
(paracellular/transcellular) reabsorption requires active transport to enter into the ISF
transcellular
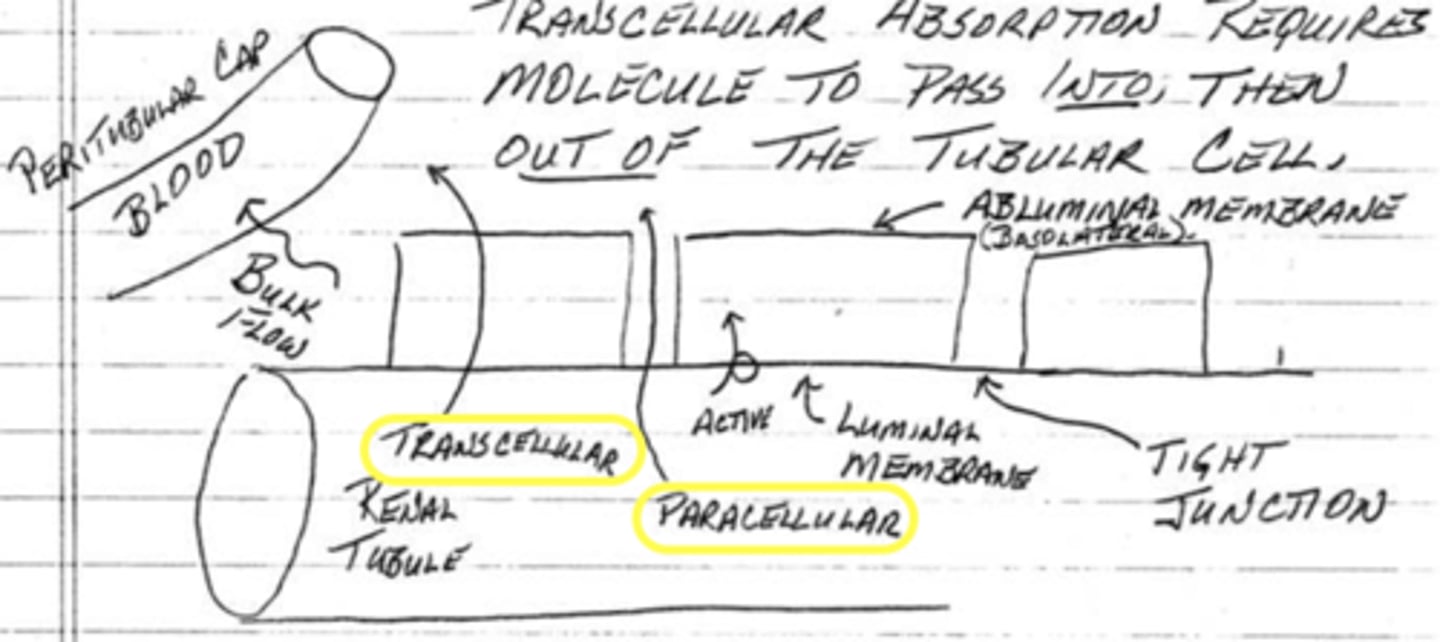
(paracellular/transcellular) reabsorption uses passive transport to enter the ISF
paracellular
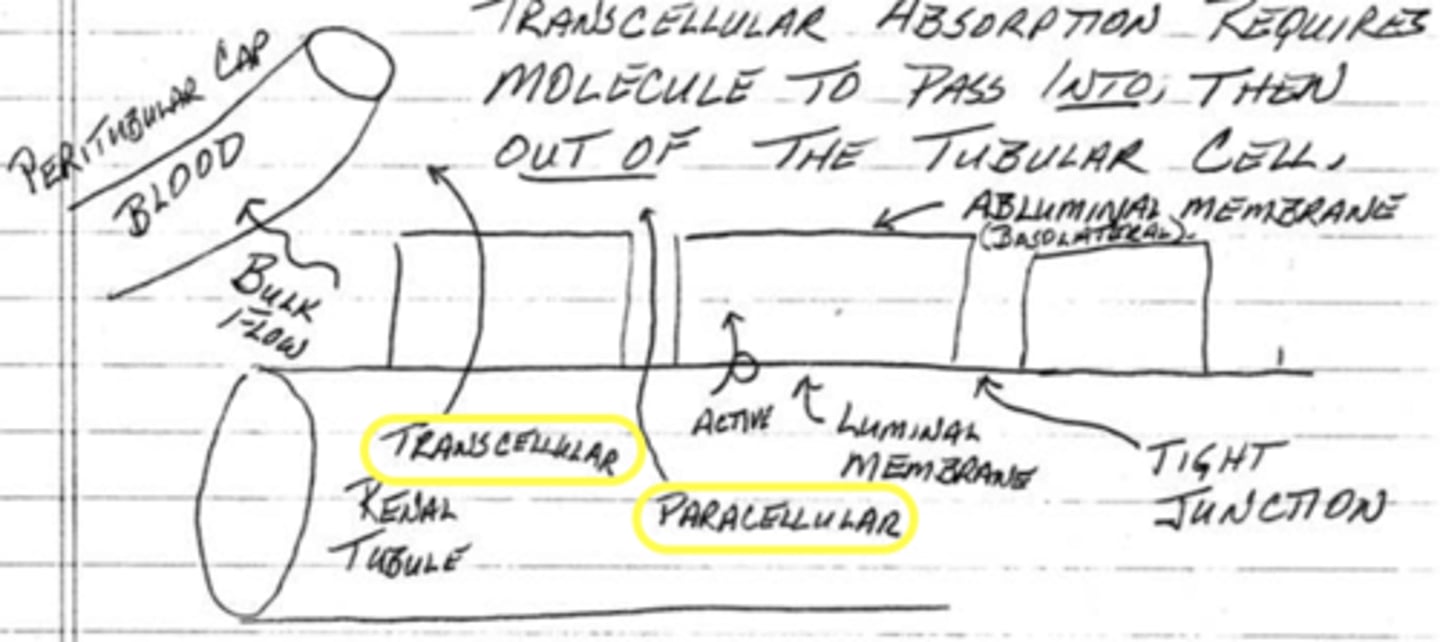
reabsorption is primarily (paracellular/transcellular) into the ISF
transcellular
ions and water can be partially reabsorbed into the ISF through paracellular transport by crossing __________ ____________ of cells
tight junctions
(t/f) reabsorption of plasma into the ISF occurs via bulk flow
true
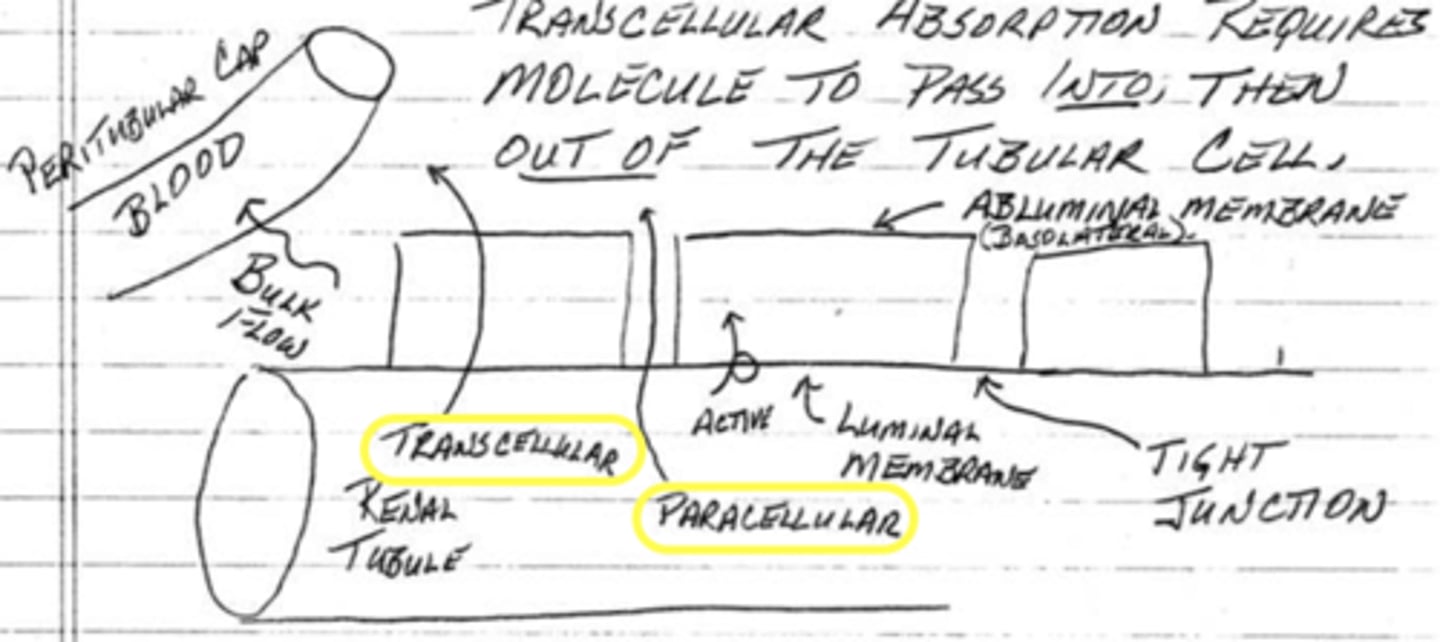
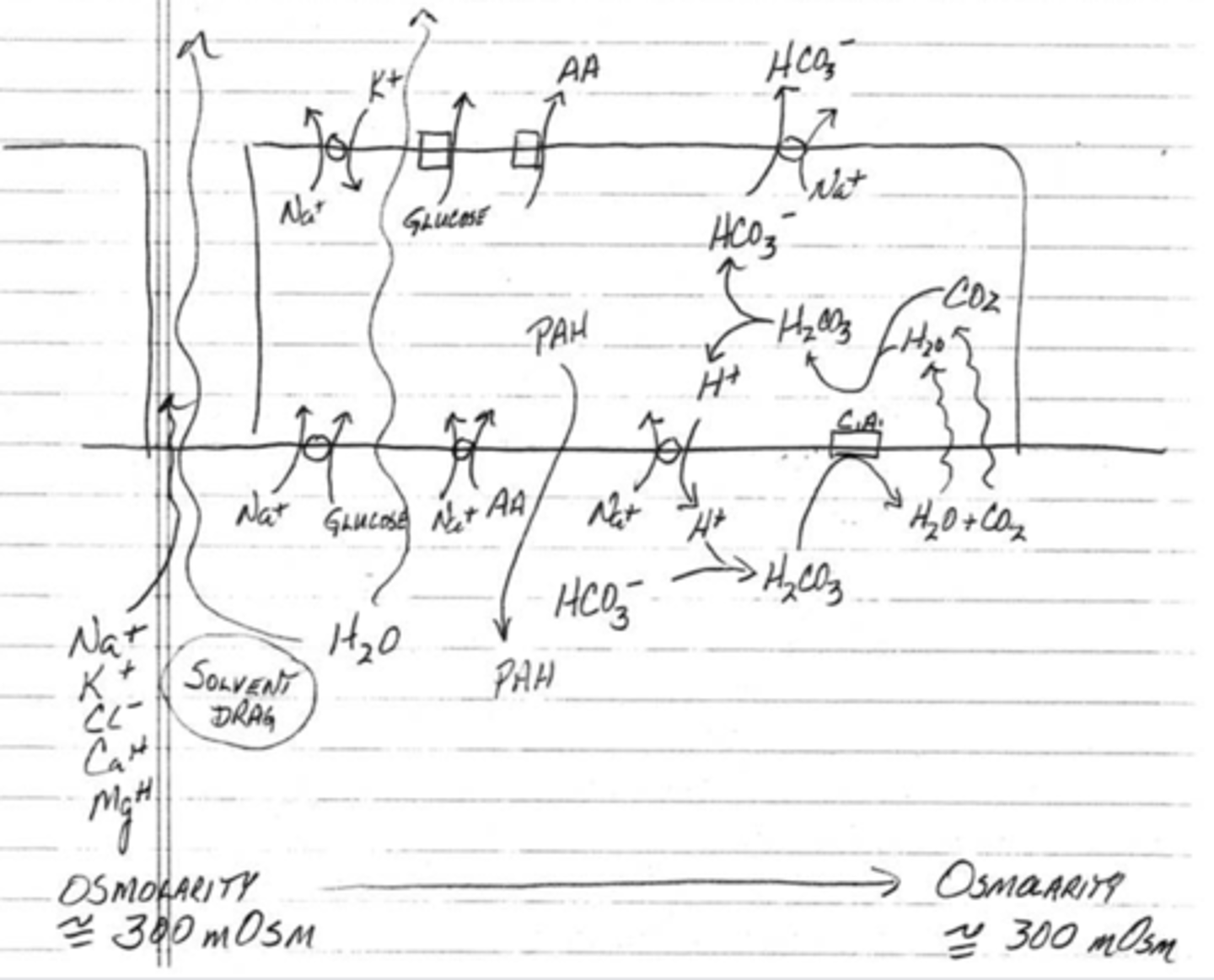
describe how sodium and water are reabsorbed through transcellular transport
1. sodium and water are able to diffuse through the abluminar cell
2. once inside the cell, the sodium will need an ATP pump in order to be removed out of the cell and into the plasma/ISF
3. water will then passively diffuse out of the cell because it follows the sodium;
this is a primary active transport
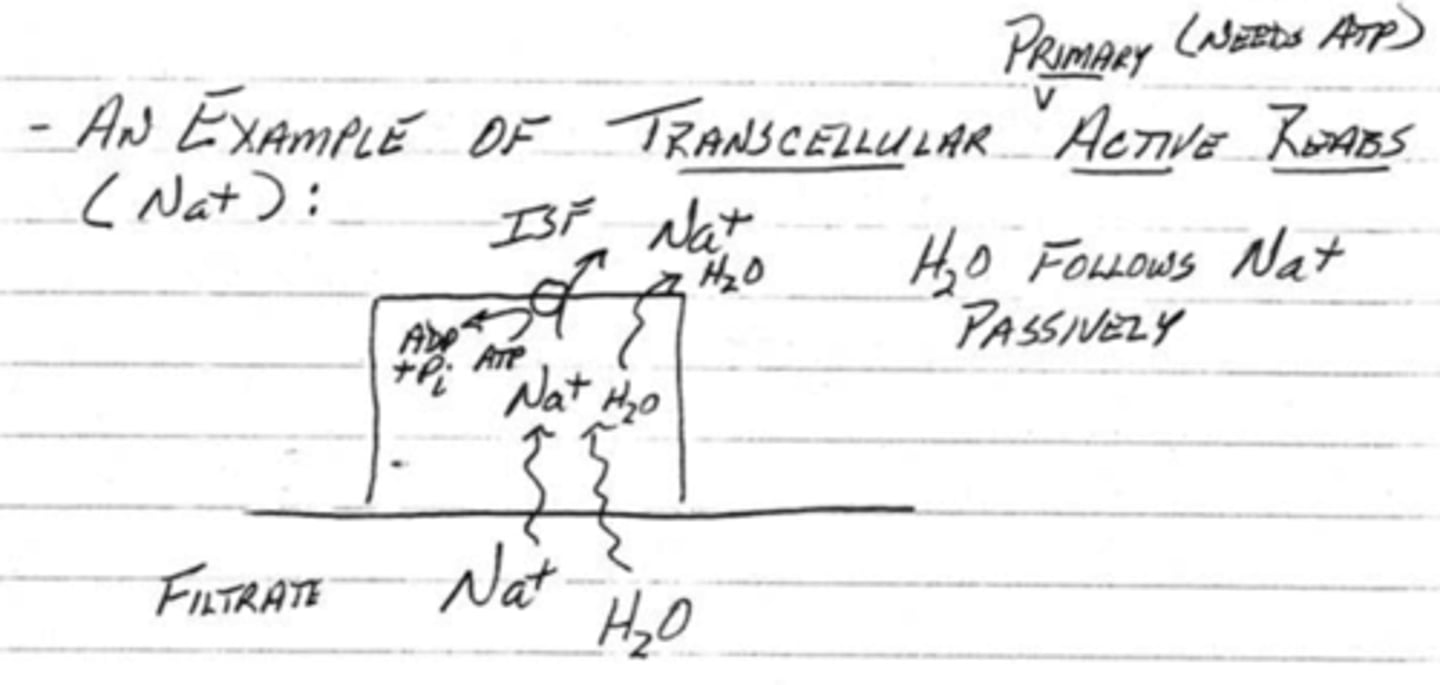
describe how sodium and glucose (or amino acids) are reabsorbed through transcellular transport
1. glucose enters the abluminar cell by using the gradient energy of sodium
2. once inside the cell, the sodium will need and ATP Na+/K+ pump in order to be removed out of the cell and into the ISF
3. glucose will then by removed out of the cell and into the plasma/ISF through facilitated diffusion;
sodium is transported through primary active transport while glucose or amino acids use secondary active transport
transcellular transport in reabsorption is done by active transport and facilitated diffusion. these both use proteins and are saturable. what does this mean?
transcellular transport has a transport maximum/limit. if the tubular load is greater than the maximum, then the substance will become lost in urine as it cannot be reabsorbed.
normal glucose levels are around _______ mg per 100 ml
100
when glucose levels exceed _____-_____ mg per 100 ml, glucose begins to appear in urine as it all won't be reabsorbed
200-250
what is the equation for the tubular load of a particular substance?
tubular load = [substance in plasma] * GFR
what is polyuria?
excessive urination
what is polydipsia?
excessive thirst
(t/f) Tmax for glucose is the highest
true
(t/f) sodium has a Tmax because it is actively transported
false; sodium does not have a Tmax because although it is actively transported, it can also be passively reabsorbed
(t/f) water has a Tmax
false; water does not have a Tmax as it is reabsorbed passively with sodium
most water reabsorption occurs by passing through the ___________ ____________ of cells. when water is flowing back to the body, ___________ ____________ causes ions to flow with it.
tight junctions, solvent drag
in the loop of Henle, the distal convoluted tubule, and the collecting tubule/duct, the tight junctions become (less/more) permeable to water. what does this mean?
less; this is where water reabsorption is regulated
70% of reabsorption occurs in the (distal/proximal) convoluted tubule
proximal
what is the purpose of the brush border found in the proximal convoluted tubule?
to expand surface area
____% of filtered load of Na+, water, and Cl- are reabsorbed in the proximal convoluted tubule
70
____% of filtered glucose and amino acids are reabsorbed in the proximal convoluted tubule
100
____% of filtered bicarbonate is reabsorbed in the proximal convoluted tubule
80
(t/f) osmolarity in the proximal convoluted tubule changes
false; osmolarity remains constant because water follows solutes via osmosis maintaining isosmotic conditions so even though large volumes of water and solutes are reabsorbed, they are reabsorbed proportionally (300 mOsm)
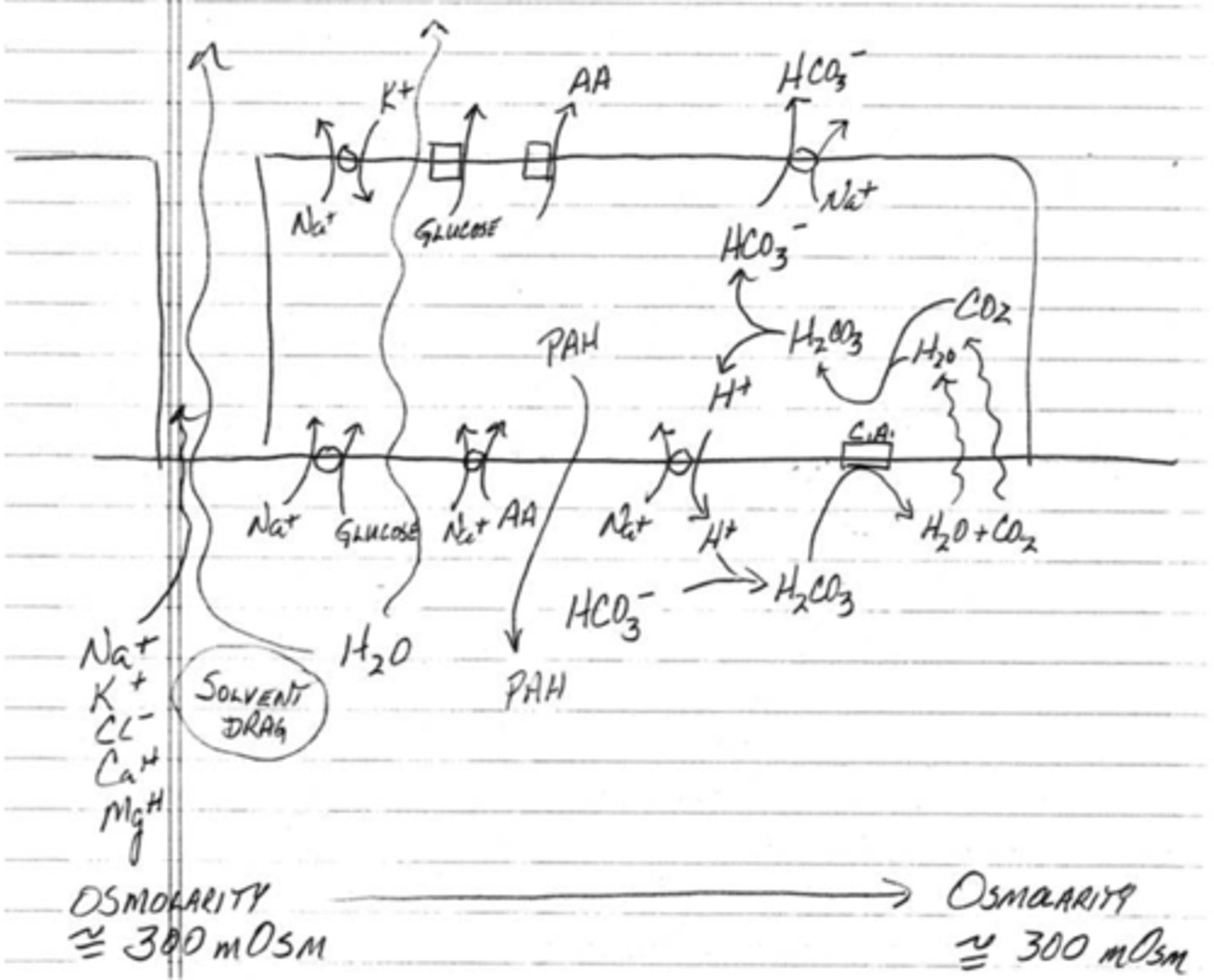
what are 3 compounds that are secreted into urine in the proximal convoluted tubule?
1. bile salts
2. uric acid
3. PAHs
describe how bicarbonate is reabsorbed through transcellular transport
1. the abluminar cell secretes protons in exchange for sodium
2. bicarbonate will bind to the proton to form carbonic acid
3. carbonic acid is then formed into water and carbon dioxide using carbonic anhydrase
4. water and carbon will then passively diffuse into the abluminar cell where it well then form back into carbonic acid
5. carbonic acid can then give off a proton and return to become a bicarbonate
6. bicarbonate can then be reabsorbed by being pumped with sodium across the abluminar membrane to re-enter the ISF/plasma
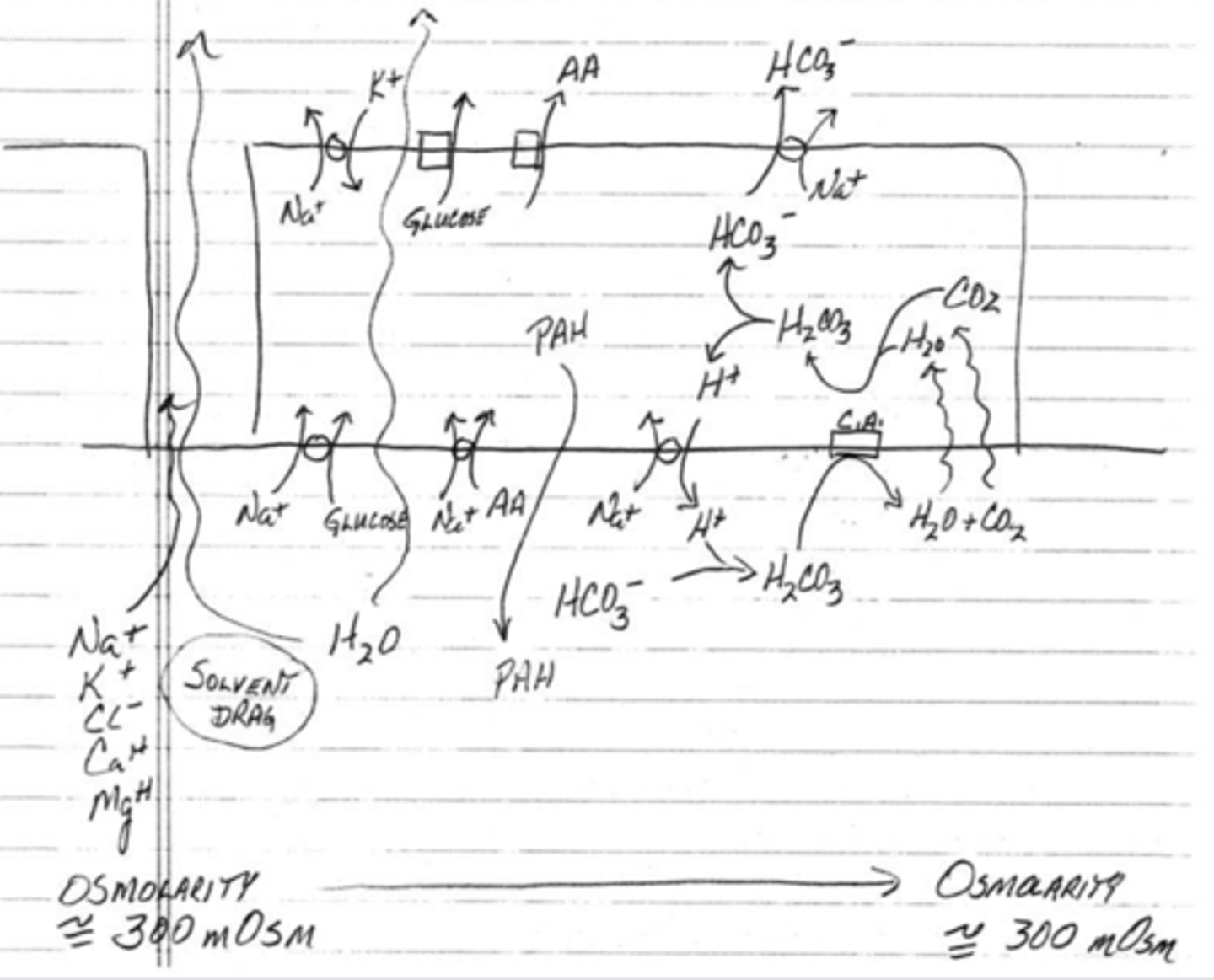
in what form is bicarbonate being reabsorbed into the body at the luminar membrane?
carbon dioxide
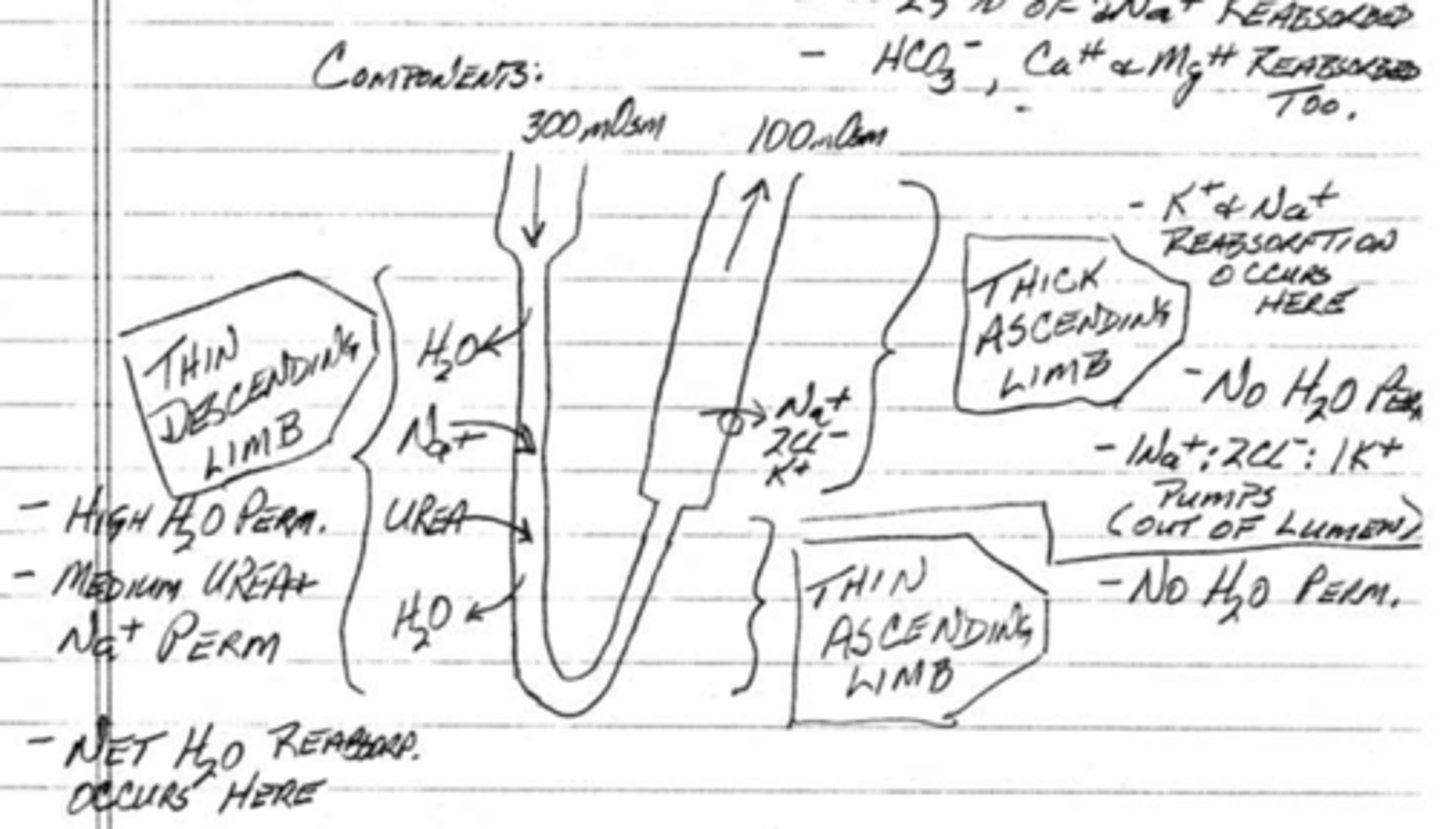
what is the major purpose of the loop of Henle?
to produce an osmotic gradient
____% of water is reabsorbed in the loop of Henle
15
____% of sodium and potassium is reabsorbed in the loop of Henle
25
(t/f) bicarbonate, calcium, and magnesium will not be reabsorbed in the loop of Henle
false; these will still be reabsorbed in the loop of Henle
in the thin descending limb of the loop of Henle, what is being reabsorbed? what are 2 compounds being secreted?
water;
1. sodium
2. urea
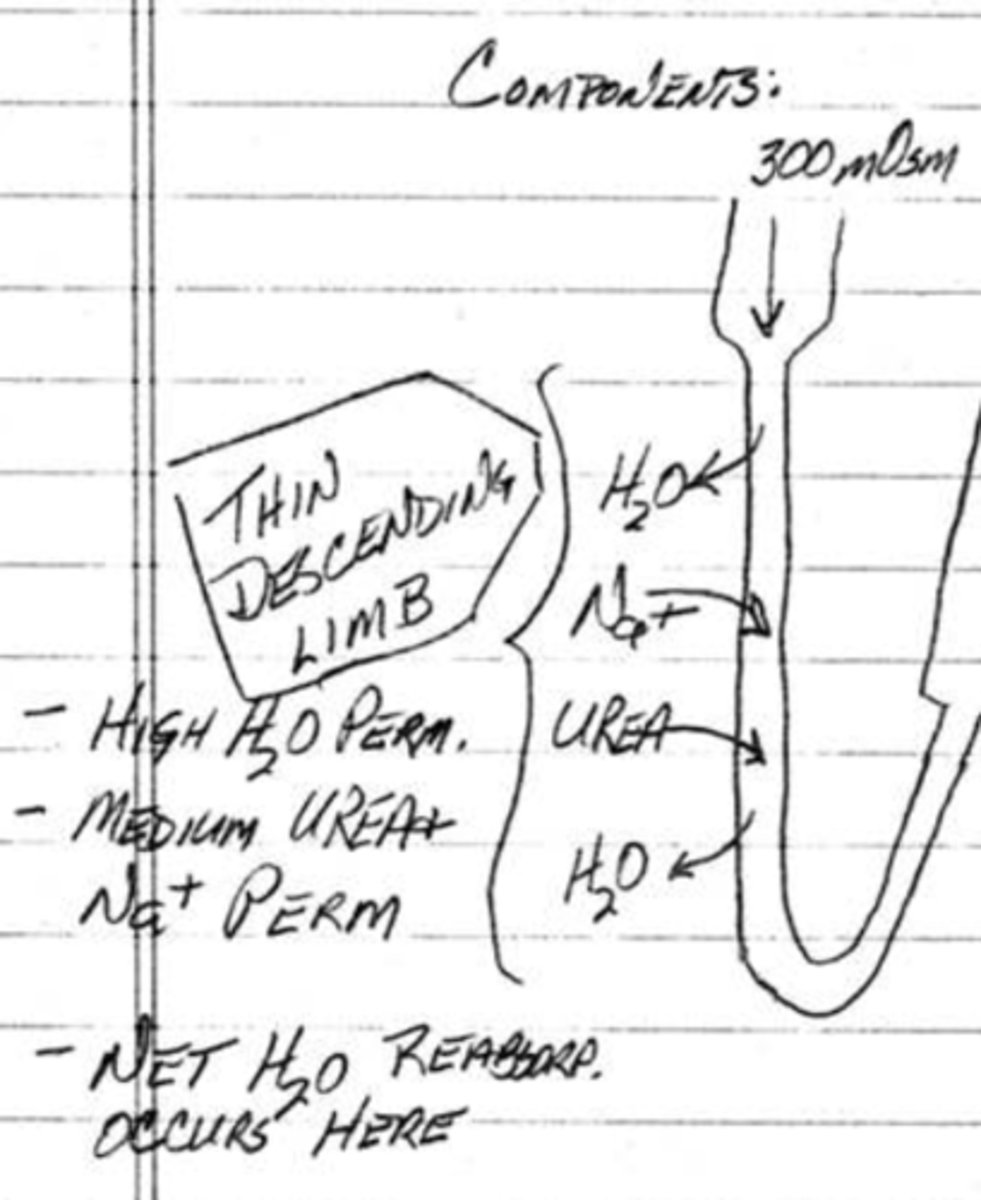
(t/f) in the thin ascending limb of the loop of Henle, water is able to be reabsorbed as their is a high water permeability
false; water is not reabsorbed because there is no water permeability at this point of the loop
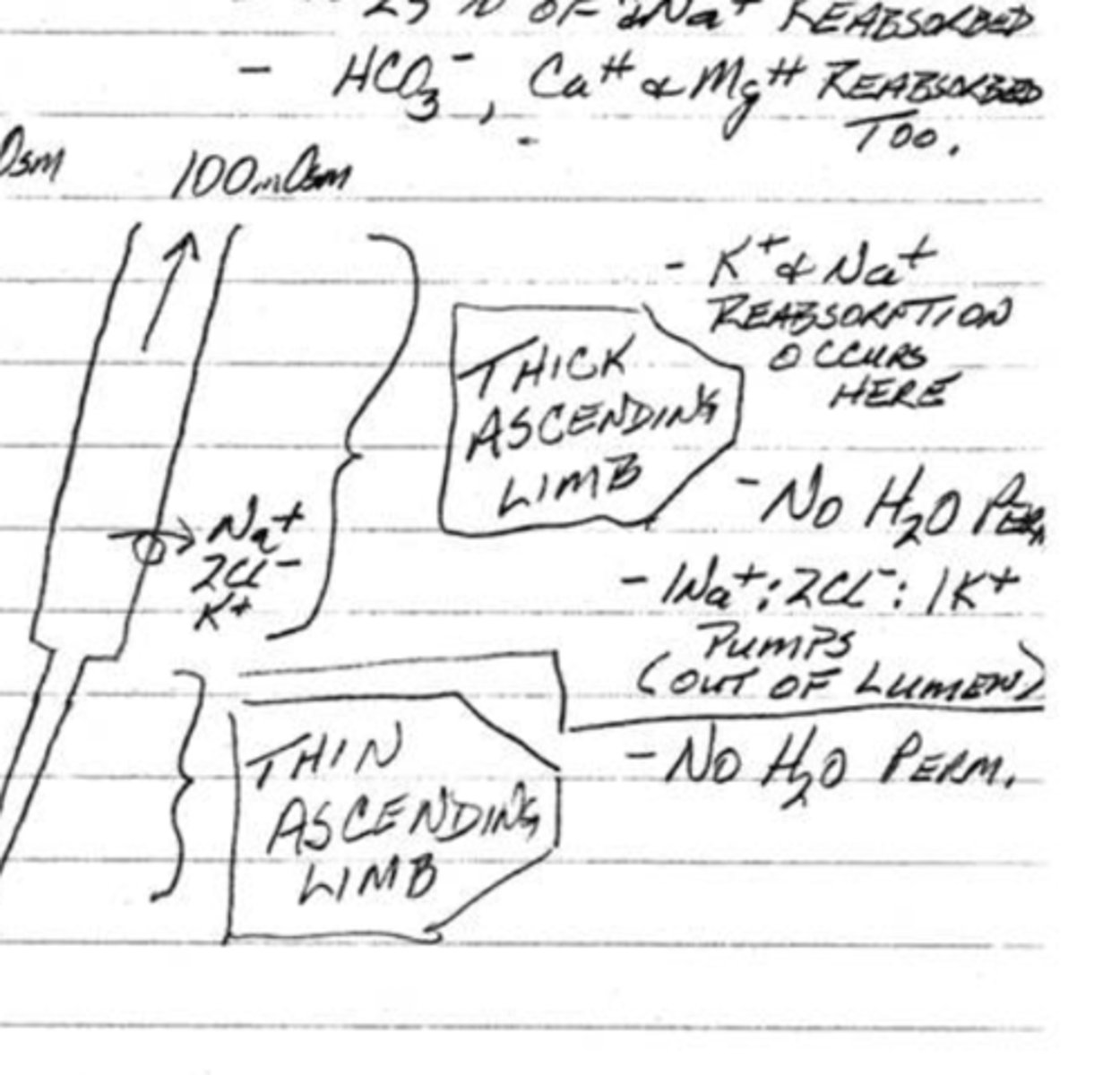
(t/f) in the thick ascending limb of the loop of Henle, water is unable to be reabsorbed as their is no water permeability
true
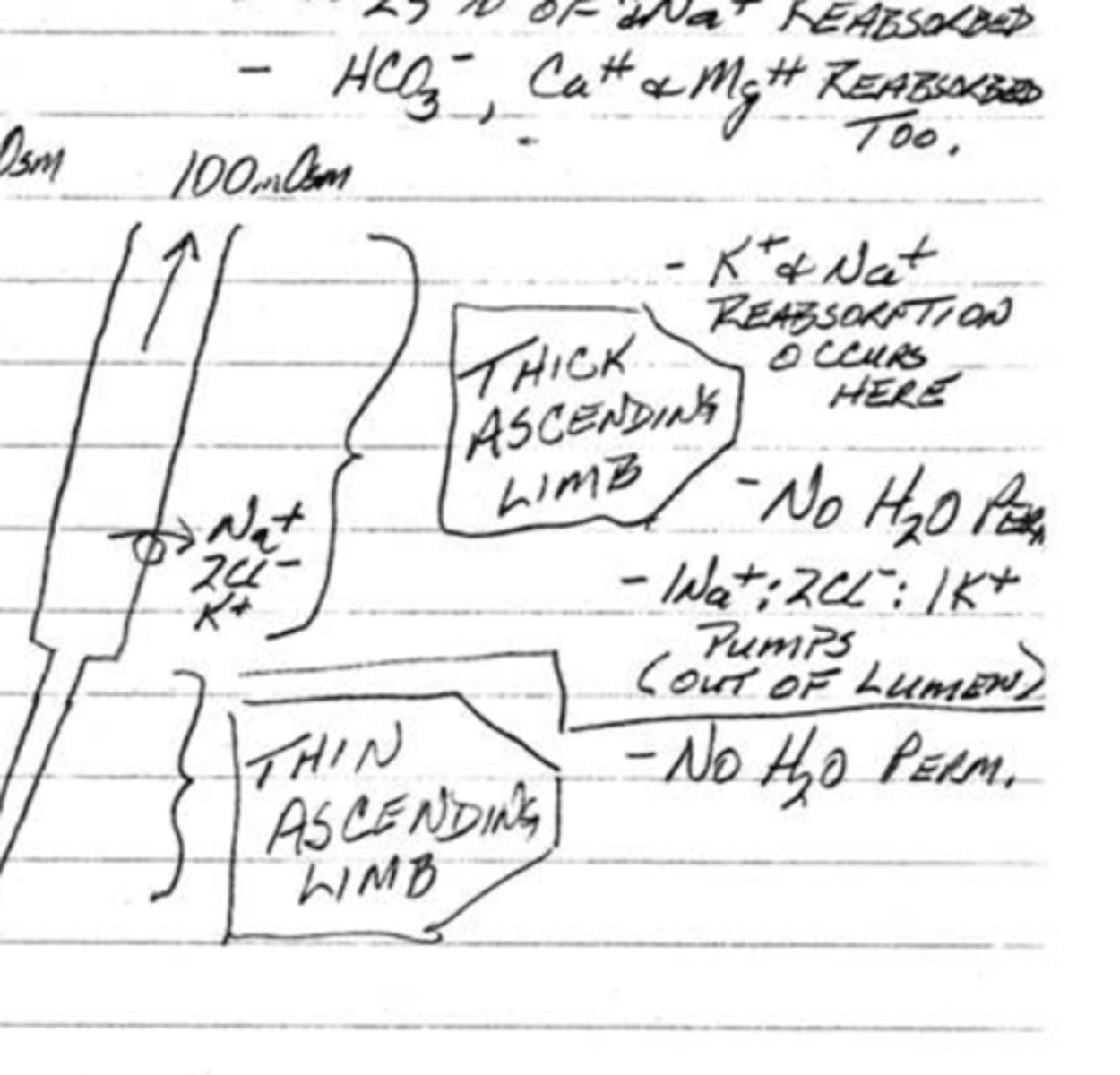
in the thick ascending loop of Henle, what are 3 compounds being reabsorbed (include their ratios)?
1. sodium
2. chloride
3. potassium;
1Na+;2Cl-;1K+
describe the osmolarity of the loop of Henle as you start from the descending limb, down to the lowest part of the loop, and at the ascending limb
descending limb: 300 mOsm
lowest part of the loop: 1200 mOsm
ascending limb: 100 mOsm
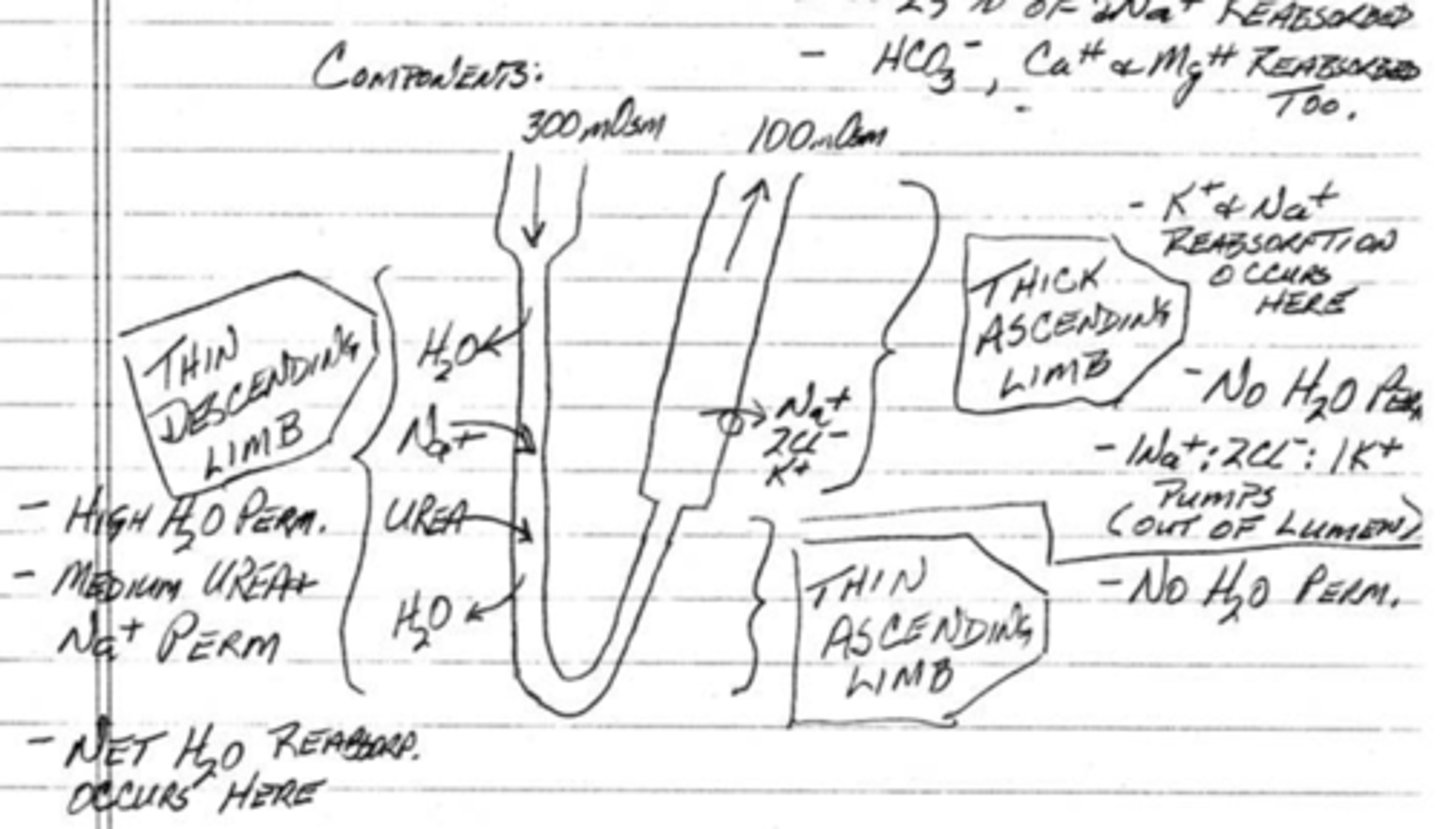
(t/f) urea is reabsorbed at the thick ascending limb of the loop of Henle
false; urea is not reabsorbed into the body, but it is secreted in the descending limb of the loop of Henle