3. Pigments and Deposits
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
What are some examples of normal substances which accumulate in cells?
- Water, lipid, protein, CHO
What are the two types of abnormal substances which can accumulate in cells?
- Exogenous (Minerals, viral particles)
- Endogenous (abnormal synthesis or metabolism)
In addition to normal cell components and exogenous/endogenous abnormal substances, what else can accumulate in cells?
- Pigments
What are the possible mechanisms of accumulation of substances in a cell?
- Production is normal, but metabolism is inadequate to remove it (i.e. lipids)
- Abnormal production due to genetic or acquired defects in production, transport, packaging, and secretion of substances (i.e. lysosomal storage diseases)
- Exogenous substance is not metabolized and accumulates (i.e. carbon, silica)
Accumulation often occurs where?
- At the site of deposition or metabolism
What is lipidosis? When is it normal?
- Pathologic lipid accumulation in cells
- In some species it is normal (i.e. cat kidney, shark liver)
What is an example of lipidosis?
- Delivery of free fatty acids (NEFAs) to the liver in excess of metabolic capacity (obese anorexic animal)
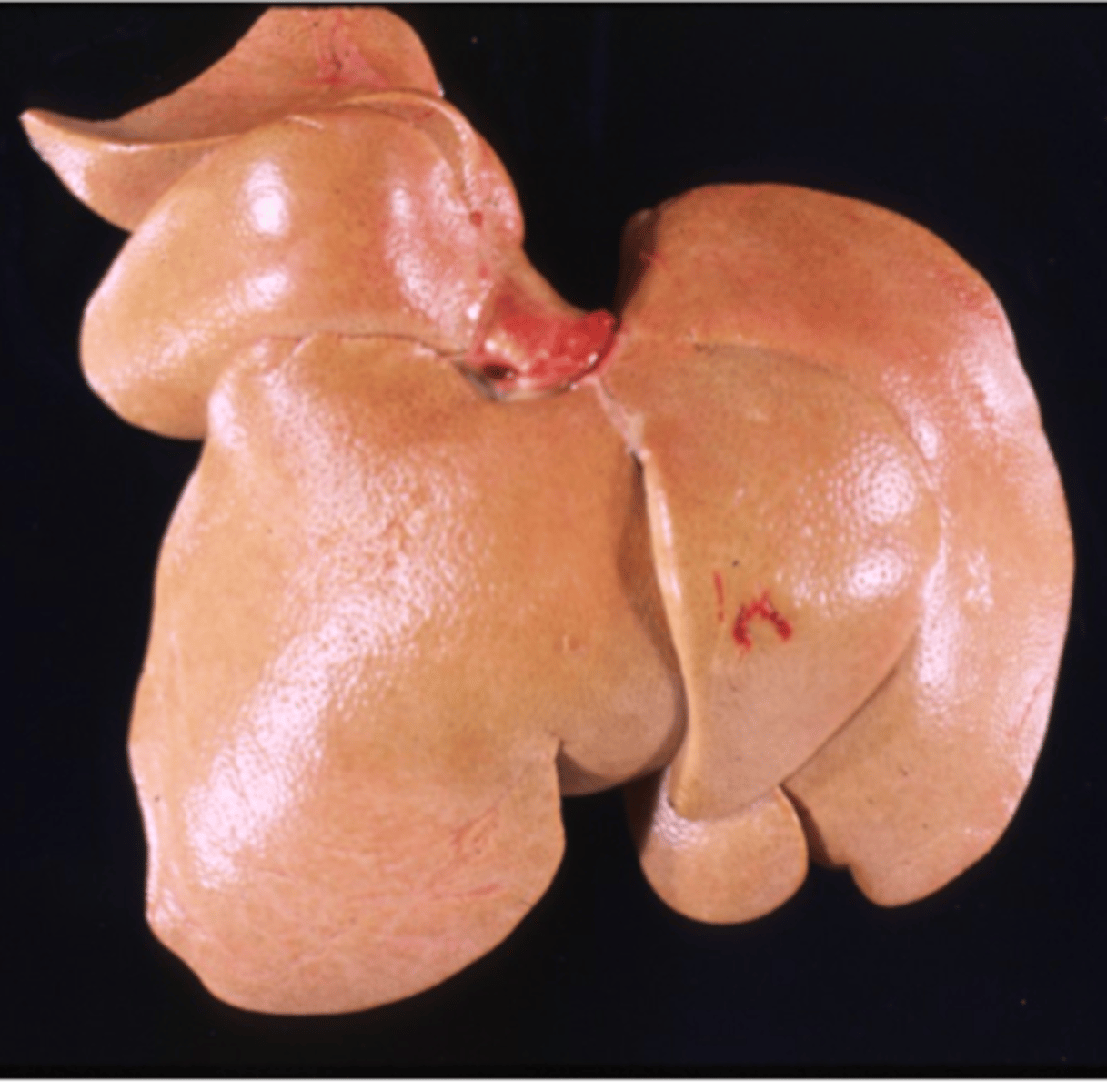
How does lipidosis appear grossly in the liver?
- Enlarged, soft (friable), greasy, pale yellow liver
- Description of image: The liver is diffusely enlarged, soft, and pale tan/yellow. It has a greasy texture on cut surface.
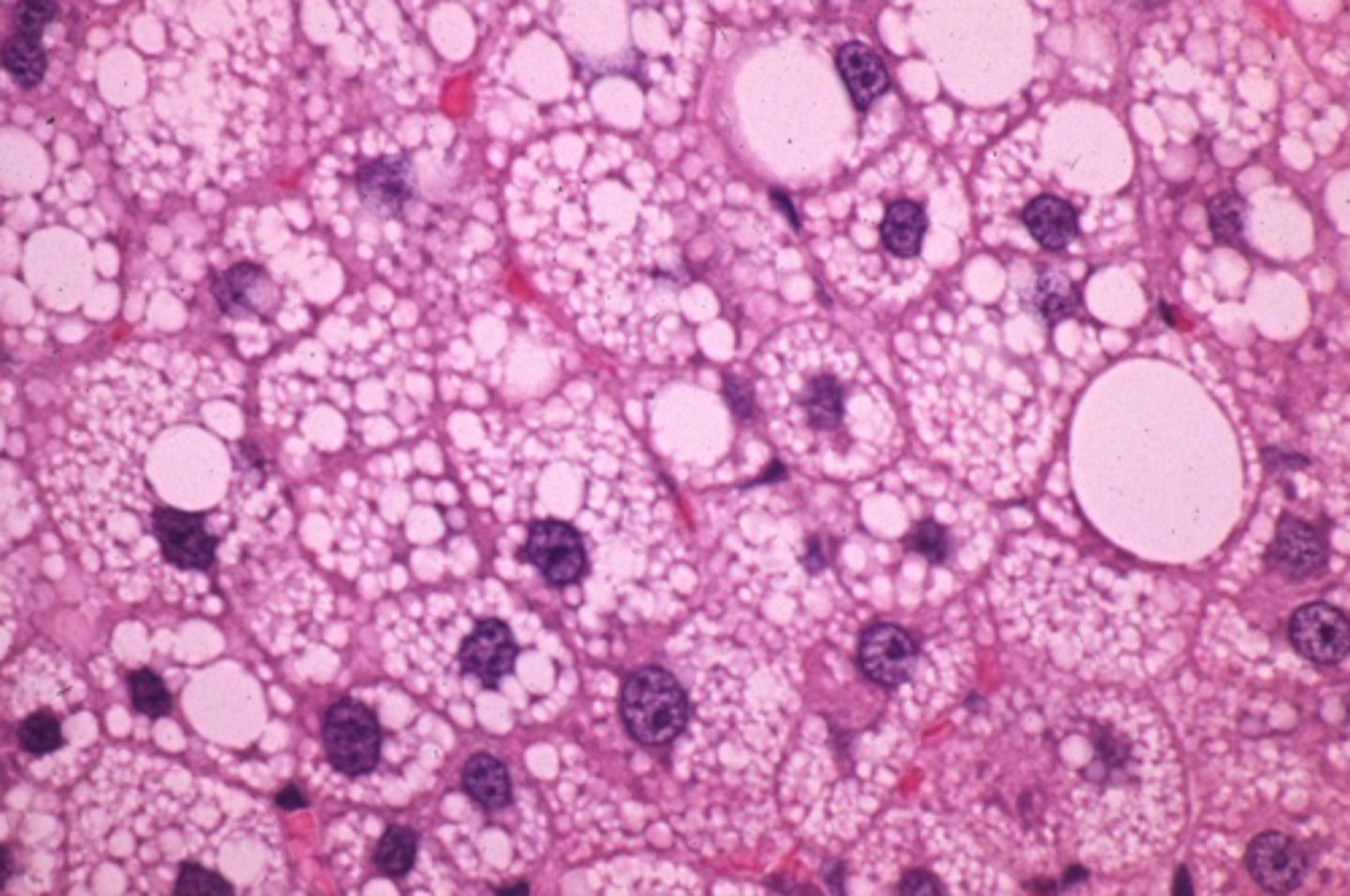
How does lipidosis appear histologically in the liver?
- Vacuoles with sharp borders in cytoplasm of swollen hepatocytes
What is glycogenosis? When is it physiological?
- Accumulation of excess glycogen in cells
- Physiologic in neonates
What are some causes of glycogenosis?
- Abnormal glucose/glycogen metabolism (diabetes mellitus)
- Corticosteroid excess (Hyperadrenocorticism, iatrogenic)
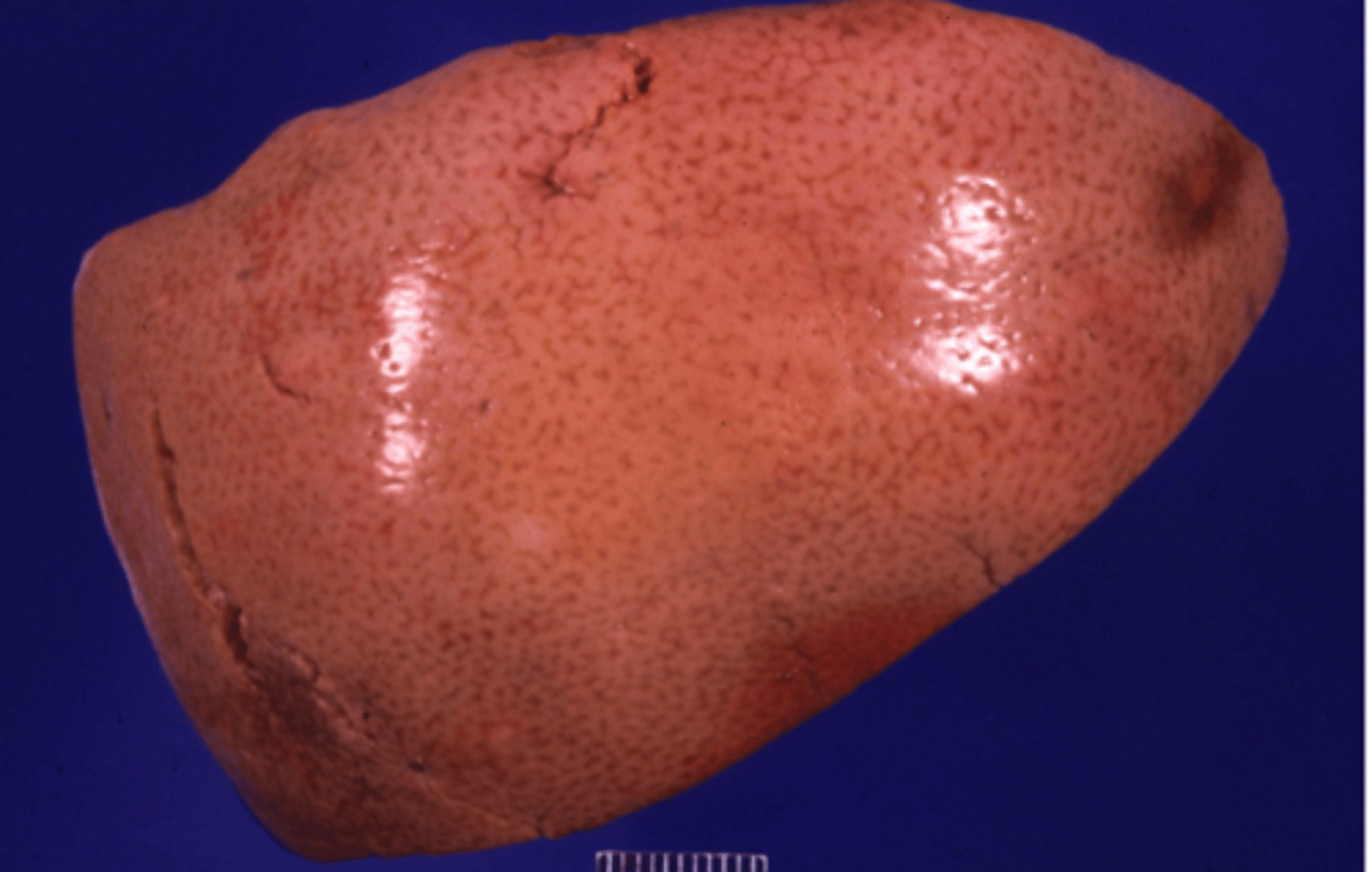
How does glycogenosis appear grossly in the liver?
- Enlarged pale liver (Similar to liver with lipidosis but not yellow and greasy)
- Description of image: The liver is diffusely enlarged. it is pale/tan and it is extremely soft.
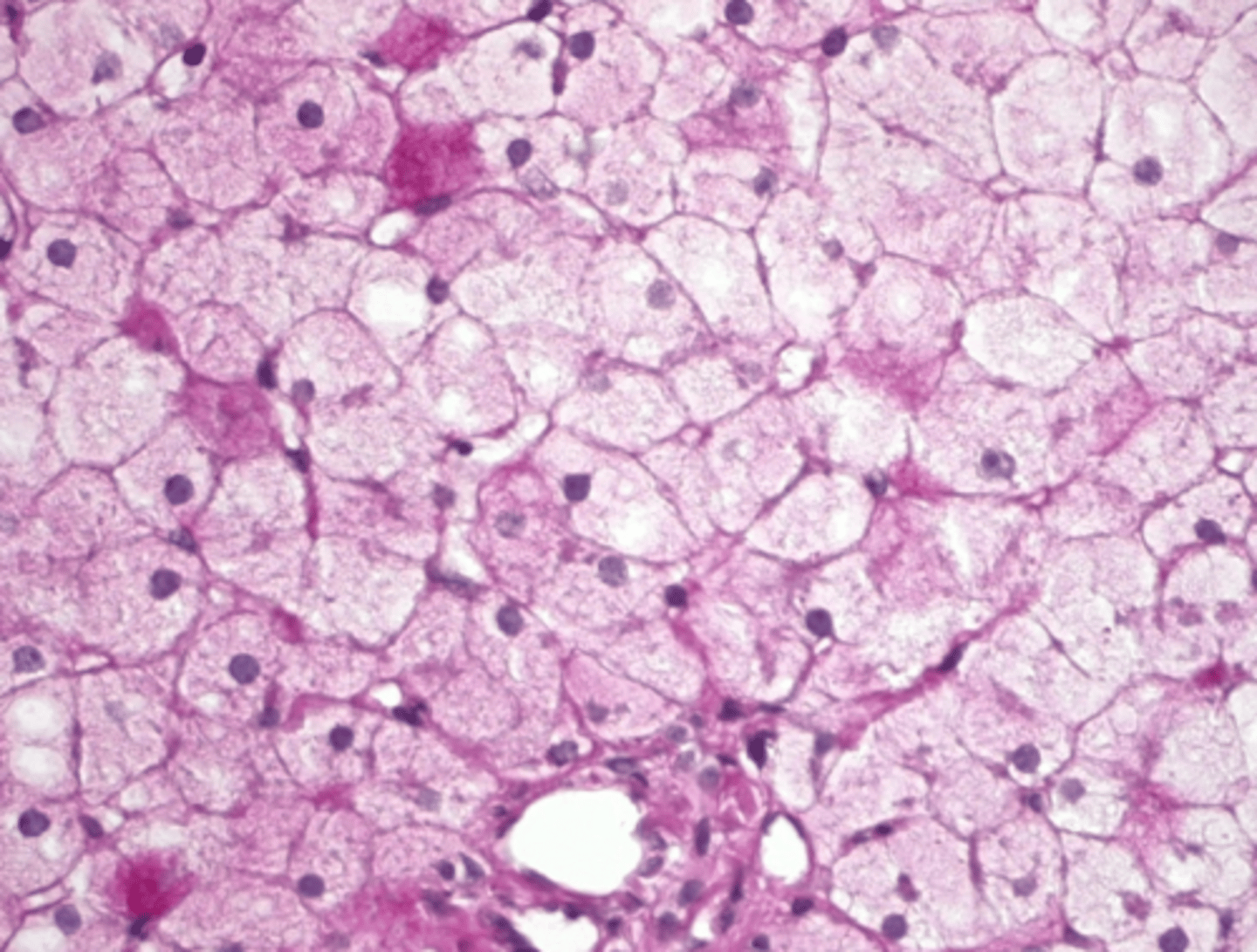
How does glycogenosis appear histologically in the liver?
- Vacuoles in swollen hepatocytes with indistinct borders, "fluffy" or "lacy" cytoplasm (not sharp borders)
What are lysosomal storage diseases? What are the types based on?
- A group of genetic enzyme deficiencies resulting in pathologic accumulation of complex carbohydrates
- Many types based on specific enzyme affected
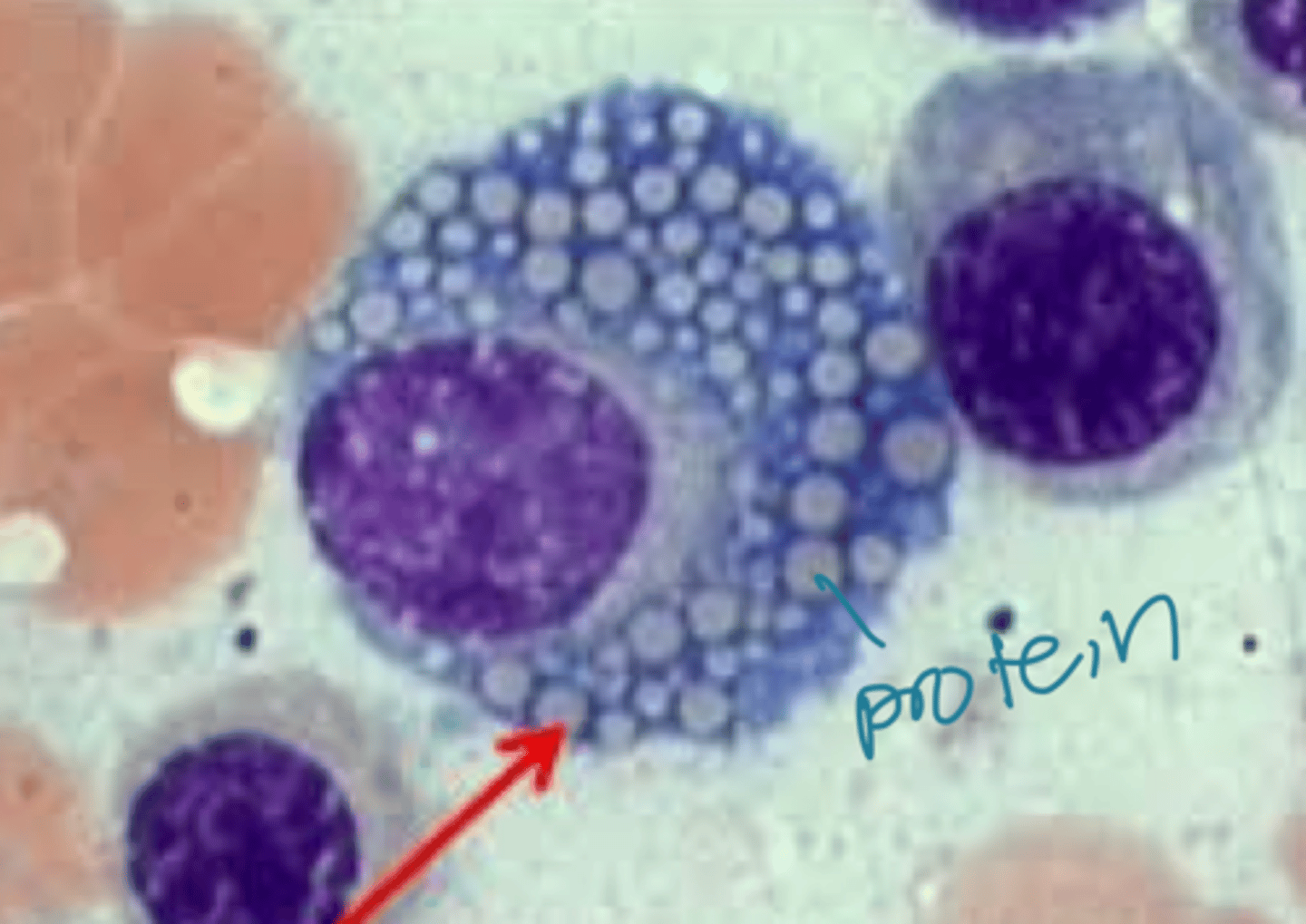
When protein production outweighs metabolism, what will be observed?
- Russell bodies (immunoglobulins) in constipated plasma cells ("Mott cells")
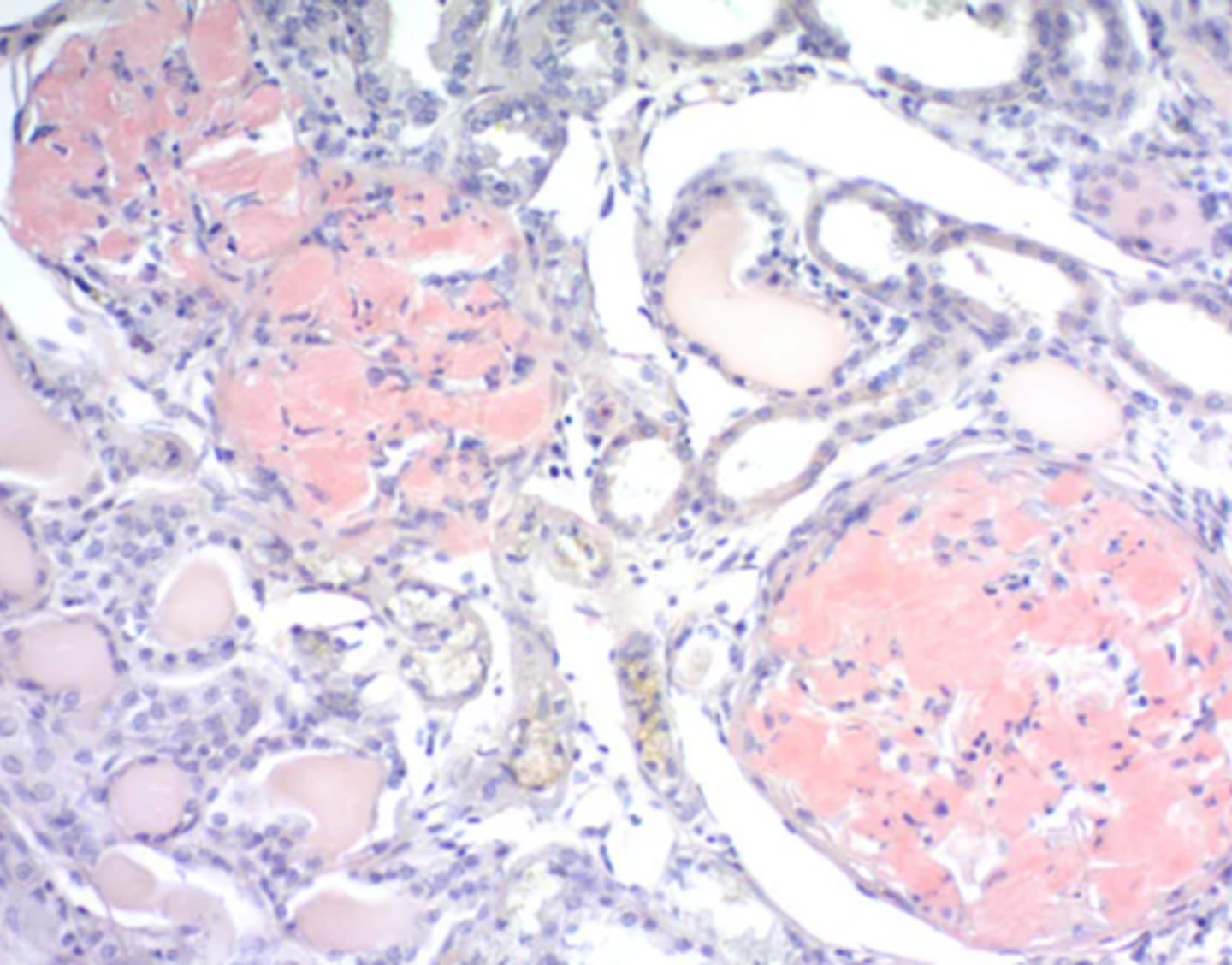
- Reabsorption droplets in renal tubules (due to protein loss in urine)
What does the presence of abnormal proteins lead to?
- Viral inclusion bodies
What causes defective protein folding?
- Prion disease
What is amyloid?
- "starch-like" protein, named for positive staining with iodine; Heterogenous family of glycoproteins in Beta-pleated sheets form aggregates which are poorly digestible
What is the effect of amyloid accumulation?
- Extracellular accumulation -> space occupying effects -> Increase distance between cells and decrease nutritional supply -> Organ damage
What are the two major categories of amyloid? Which is more common in humans and which is more common in animals?
- AL amyloid: Most common in humans
- AA amyloid: Most common in animals
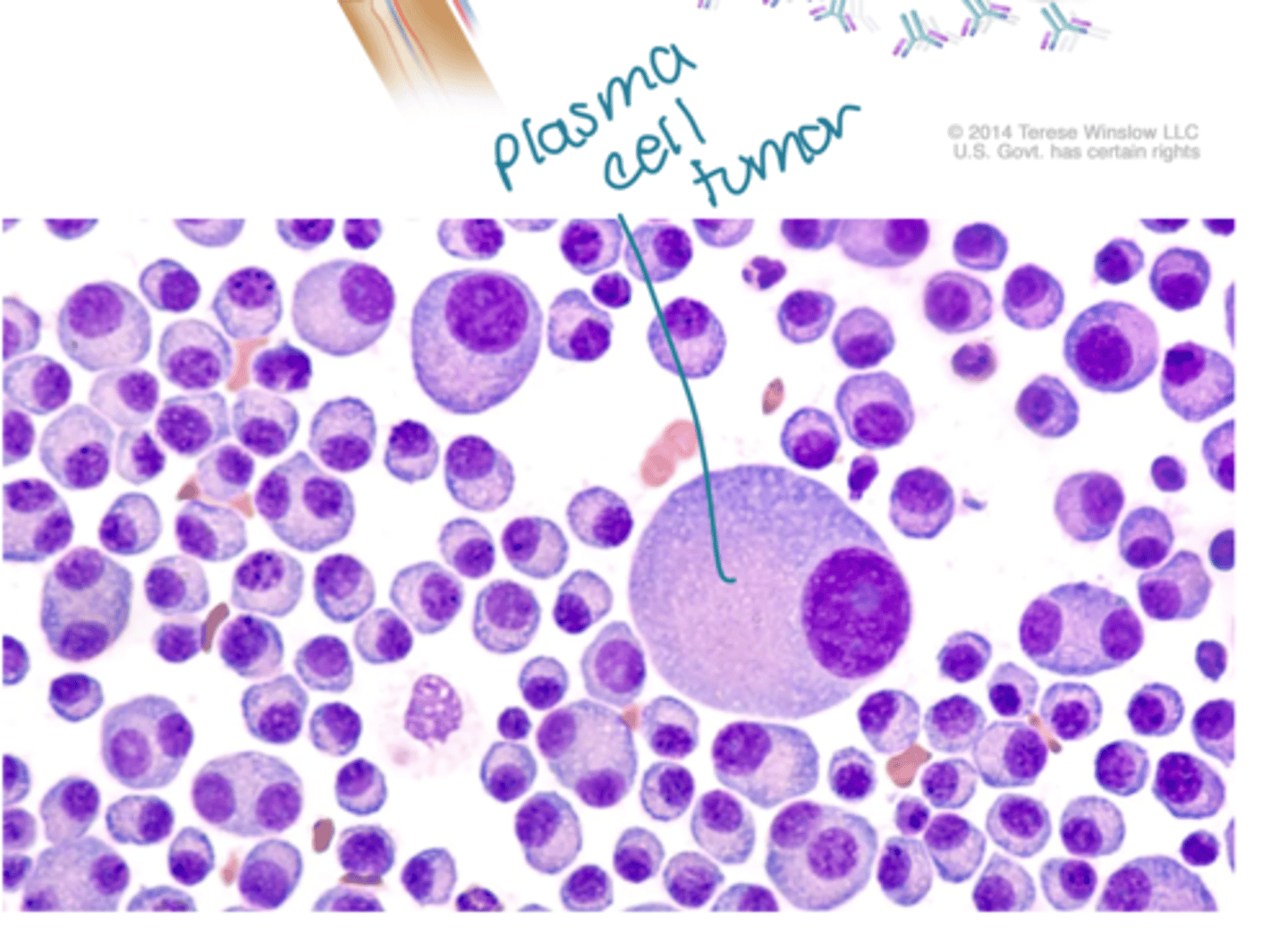
What causes AL amyloidosis? What is it composed of?
- Hematopoietic neoplasia (plasma cells) producing antibodies
- Composed of immunoglobulin light chains secreted in blood, precipitate in capillary basement membranes
What causes AA amyloidosis? Where does it usually accumulate?
- Inflammation anywhere in the body leads to the production of serum amyloid A (SAA), a pro-inflammatory acute phase protein. Chronic inflammation leads to chronic SAA production leading to deposition systemically and locally.
- Generally deposited in liver, kidney, spleen, LN and intestines, nasal submucosa in horses, pancreatic islets in cats
In which species is AA amyloidosis particularly common?
- Especially common in primates and avians
What are some other types of amyloid? Describe them briefly.
- Hereditary amyloid: Rare in animals; Sharpes and Abysinians most common
- Beta amyloid (AB amyloid): Alzheimer's disease (Brains of old dogs)
Where does amyloid accumulate relative to cells? How does it stain? Describe its shape.
- Extracellular (+/- macrophages)
- Eosinophilic (pink)
- Amorphous
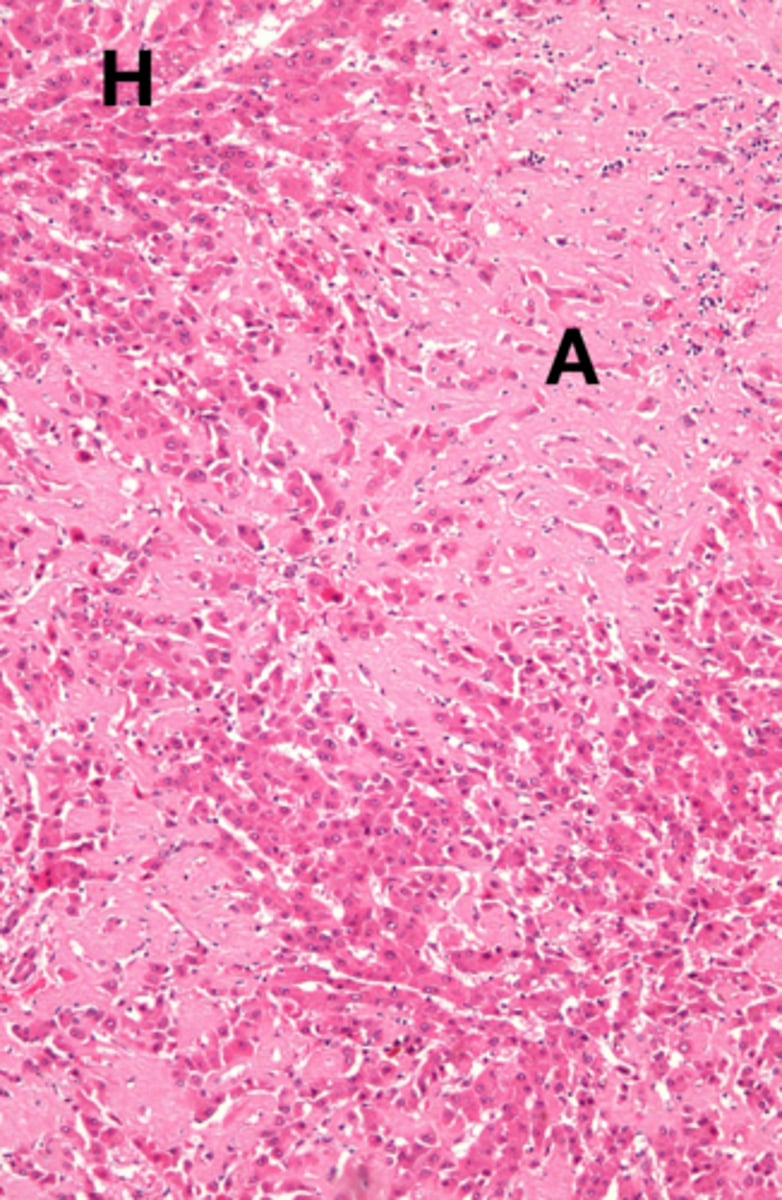
How does accumulation of amyloid affect local tissues?
- Leads to compression, death and loss of adjacent cells; Affected tissue is swollen, firm, waxy and pale
How can one confirm the presence of amyloid in tissue? Without this method, amyloid is difficult to distinguish from _________________.
- Congo red stain which highlights amyloid as pink/red
- Collagen
What is pathologic calcification?
- Abnormal deposition of calcium salts in tissues (mineralization)
What causes pathologic calcification?
- Result of localized or systemic disruption in calcium metabolism
Describe calcified tissue.
- Hard, white and gritty
Is calcification the same as ossification? Explain.
- No
- Calcification is calcium deposits while ossification is tissue turning into bone, which may mineralize
What are the four types of pathologic calcification? Indicate which two types are the primary types.
1) Dystrophic - Primary type
2) Metatstatic - Primary type
3) Idiopathic
4) Iatrogenic
What causes dystrophic calcification?
- Localized disruption in calcium homeostasis secondary to regional tissue death (necrosis) of any type or cause. Dead cells lose the ability to regulate calcium, causing it to accumulate in the mitochondria, leading to cell death and localized calcification.
Dystrophic calcification is most common/severe where?
- In tissues with high calcium storage (muscle)
Dystrophic calcification indicates what?
- A site of previous tissue injury
With dystrophic calcification, what happens to systemic calcium levels?
- Systemic calcium metabolism/levels are normal
Provide an example of a disease which leads to dystrophic calcification.
- White muscle diseases (selenium/vitamin E deficiency which are important antioxidants -> free radical tissue damage) leads to dystrophic calcification
What causes metastatic calcification?
- Systemic disruption in calcium homeostasis (hypercalcemia) which leads to calcium precipitation in tissues, leading to tissue damage.
Where does metastatic calcification generally occur?
- Occurs in otherwise normal/healthy tissue
What are some major causes of metastatic calcifiation in vet med?
- Renal failure
- Vitamind D toxicity
- Hyperparathyroidism (+/- paraneoplastic)
- Bone destruction
Explain the difference in cause between dystrophic and metastatic calcification.
- Dystrophic calcification is caused by tissue necrosis while metastatic calcification is caused by systemic hypercalcemia.
Explain the difference in serum calcium levels between dystrophic and metastatic calcification.
- Dystrophic: Normal
- Metastatic: High
Explain the difference in location between dystrophic and metastatic calcification.
- Dystrophic: Local, site of tissue damage
- Metastatic: Multisystemic, otherwise normal tissue
Explain the difference in relationship to tissue damage between dystrophic and metastatic calcification.
- Dystrophic: Result of previous tissue damage
- Metastatic: Cause of tissue damage
Explain the difference in sites between dystrophic and metastatic calcification.
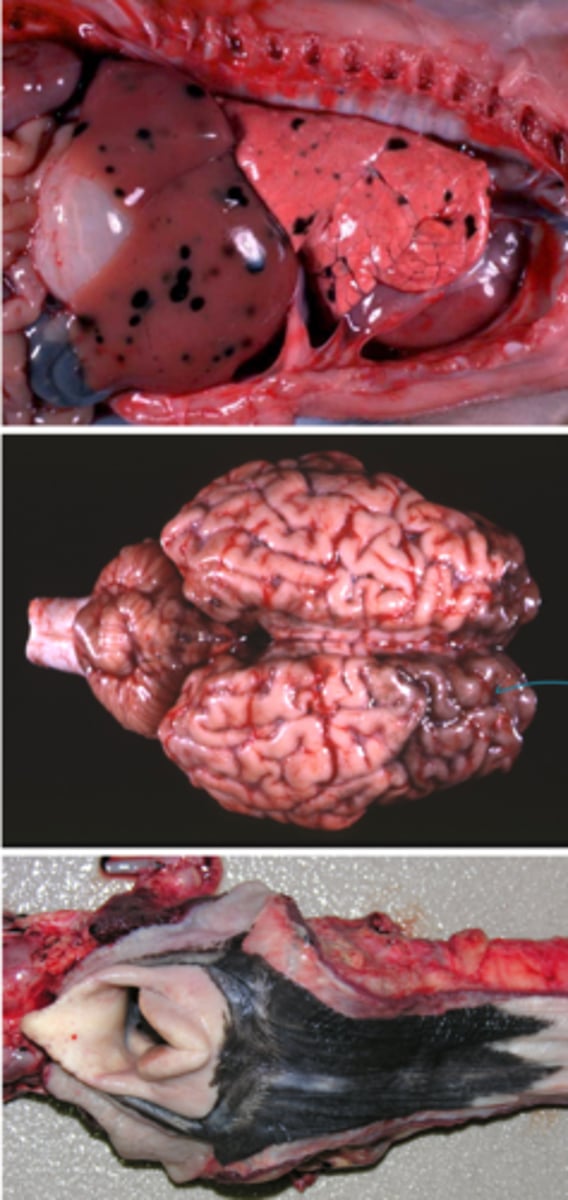
What is gout/explain its pathophysiology? In what species does it occur? In what species is it common?
- Deposition of sodium urate crystals or urates in tissues resulting from chronically elevated serum uric acid
- Occurs only in species lacking urease (i.e. humans/primates)
- Common in reptiles and birds
What are some causes of/risk factors for gout?
- Renal disease (Cannot excrete urate as efficiently)
- Dehydration
- High protein diet (Increase input)
What are the two types of gout based on where the sodium urate crystals/urates are deposited?
- Visceral gout: Deposition in organs
- Articular gout: Deposition in joints
What are some examples of exogenous pigments?
- Carbon, silica, duct
- Tattoos
- Carotenoids (B-carotene)
- Drugs (tetracyclines)
- Infectious agents (fungi, parasites)
What are some examples of endogenous pigments?
- Melanin
- Lipofuscin
- Blood pigments (bilirubin, porphyrins, hemosiderin)
What is melanin produced by?
- Melanocytes
What is melanosis?
- Dark black, incidental pigmentation of tissues
In what tissues is melanosis normal? What must it be differentiated from?
- Normal in skin, viscera, meninges of some species (especially LA)
- Differentiate from melanoma (neoplasm of melanocytes)
What is lipofuscin?
- An aging or "wear and tear" pigment
What is autophagy?
- Cellular process of recycling damaged organelles by digesting them into their components
How does lipofuscin relate to autophagy?
- Lipofuscin is the indigestible end-product of autophagic metabolism
Where does accumulation of lipofuscin generally occur?
- In terminally differentiated cells of older animals (i.e. cardiomyocytes, neurons)
What color is lipofuscin?
- Golden-yellow
What effect does lipofuscin have on cells?
- Inert, harmless to cells
Is lipofuscin accumulation visible microscopically or grossly?
- Marked accumulation may lead to brown staining of tissue, but often visible only microscopically
What are some hemoglobin breakdown products?
- Porphyrin
- Bilirubin (unconjugated)
- Bilirubin (conjugated)
- Urobilinogen
- Stercobilin
- Hemosiderin (Fe)
What is the difference between conjugated and unconjugated bilirubin?
- Unconjugated: Protein-bound, not water soluble, not excretable
- Conjugated: Water soluble, excretable
What is icterus? Describe it.
- The accumulation of excess bilirubin in the blood (hyperbilirubinemia)
- Yellow discoloration of tissue (aka jaundice)
What are the three mechanisms of icterus? Describe them.
1) Pre-hepatic: Too much incoming U-bilirubin for the liver to handle
2) Hepatic: Liver is disease and cannot process U-bilirubin into C-bilirubin
3) Post-hepatic: Biliary tree is obstructed and C-bilirubin cannot be excreted in urine/feces
What are some causes of pre-hepatic icterus?
- Internal hemorrhage
- Hemolysis
What will be observed clinically in pre-hepatic icterus?
- Elevated unconjugated bilirubin
- No elevation in urine bilirubin
What is a cause of hepatic icterus? What will be observed clinically?
- Severe liver disease
- Mix of increased u-bilirubin and c-bilirubin (depending on the degree of liver disease) +/- elevation in urine bilirubin (conjugated)
What is a cause of post-hepatic icterus? What will be observed clinically?
- Biliary obstruction (intrahepatic or extrahepatic)
- Clinically: Increased c-bilirubin, elevation in urine bilirubin
In what tissues can icterus often be observed?
- Mucous membranes
- Sclera, conjunctiva
- Viscera
- Fat, subcutis
- Great vessels
How is porphyrin formed? What is it?
- Heme group minus iron
- Photoreactice intermediate; recycled or broken down into bilirubin by the liver
What is porphyrin a normal component of? What can this lead to?
- Animal tears and saliva
- Can cause local irritation ("sore nose" in sick gerbils)
What is porphyria? What does it lead to?
- Inherited metabolic defect in heme synthesis
- Porphyrin accumulates in blood, teeth, bones ("pink tooth"); Bones fluoresce under UV light
What is chlorophyll? How is it metabolized?
- Photoreactive pigment produced by plants
- Metabolized in the liver to phyloerythrin
How does chlorophyll relate to animal health?
- Severe liver disease in herbivores may result in accumulation of phylloerythrin, leading to despotition in skin, causing photosensitization and skin damage via free radical formation
What is hemosiderin?
- Iron-protein complex (Ferritin), storage form of iron
Hemosiderin is a __________ granular pigment stotred in ____________ cells.
- Brown
- Kuppfer
Can the body remove excess iron?
- No
What are some causes of systemic iron excess?
- Hemolytic crisis, blood transfusion
- Iatrogenic (excess dietary intake or supplemental iron)
- Decrease erythropoiesis
What are some causes of local iron excess?
- Local hemorrhage
- Chronic passive congestion (lungs, liver) - "Heart failure cells"
What are hemosiderosis and hemochromatosis?
- Hemosiderosis: Excess accumulation of hemosiderin in tissues; not causing tissue damage
- Hemochromatosis: Extreme accumulation of hemosiderin with damage to cells and organs