bone scintigraphy
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
bone functions
support, movement, protection, blood cell formation, mineral storage
bone formation
osteoblasts lay down osteoid (organic matrix) → amorphous calcium phosphate (ACP) salts convert to crystalline hydroxyapatite (HA) and solidify the matrix to remodel bone (HA and ACP are in inorganic matrix)
osteogenic/osteoprogenitor cells
unspecialised stem cells that develop into osteoblasts
osteoblasts
build bone, synthesise soft matter in the matrix which is hardened by mineral deposition
osteocytes
former osteoblasts trapped in their matrix to maintain calcium and phosphate ion levels
osteoclasts
dissolve bone
how does bone remodeling occur?
remodeling results from bone dissolving osteoclasts and bone depositing osteoblasts
bone radiopharmaceuticals
99mTc MDP (methylene diphosphonate)
99m Tc HDP (hydroxy methylene diphosphonate)
bone typical administered activity
~800MBq +- 10%
bone radiopharmaceutical administration
Injected intravenously (IV)
bone radiopharmaceutical mechanism of localisation
diphosphonates bind to calcium ions in the inorganic matrix (chemisorption)
hydroxl in HDP also binds to Calcium → tridentate binding
amorphous calcium phosphate (ACP) salts bind well to diphosphonate
hydroxyapatite (HA) crystals do not bind as well to radiopharmaceutical → less uptake of radiopharmaceutical in mature bone compared to immature bone
difference in HA and ACP uptake allows for detection of lesions in areas of increased osteoblastic activity
more osteoblastic activity → more ACP that converts to HA → more radiopharmaceutical uptake
bone dynamic scanning
(128x128) 2-3sec/frame 20 frames
consider 5sec/frame for extremities
bone blood pool scanning
a. statics: 500K counts or 2 min/image (128x128)
b. whole body: 25cm/min (1024x256)
bone delayed scanning
(2.5-4 hours later)
a. statics: 500K counts or 5 min/image (256x256)
b. whole body: 10cm/min (1024x256)
c. SPECT/CT: 15secs/frame, 64 frames (32 each head)
when is a 3 phase bone scan used?
when assessment of inflammation and/or vascularity is important → osteomyelitis (infection), fractures, inflammatory arthropathy
when is a 2 phase bone scan used?
when assessment of inflammation and/or vascularity is important → inflammatory arthritis, osteolytic bone lesions
when a single phase bone scan used?
when assessment of inflammation/vascularity is NOT important → metastatic disease with osteosclerotic lesions (breast and prostate cancer)
bone desired image analysis
normal biodistribution is SYMMETRICAL some areas may be hotter/colder, may be due to positioning/distance from detectors - CHECK IF IT MATCHES BOTH SIDES
bone patient history of interest
medications, allergies, history of cancer, past surgeries, falls or incidents causing injury, breastfeeding/pregnant, history of broken bones or fractures, type of pain and duration of pain
bone patient advice
avoid pregnant women/children
what are the 3 main primary bone tumours?
osteosarcoma
chondrosarcoma
Ewing’s sarcoma
primary malignant bone tumour
originate from bone itself
secondary malignant bone tumour
metastasise to bone from other body parts such as breast or prostate
osteosarcoma
(most common primary bone cancer) → develops from osteoblasts and most common in metaphyseal region of long bones, (50% knee) → good outcomes if amputation is possible
REQUIRES 3 PHASE BONE SCAN
chondrosarcoma
malignant bone cancer starting in cartilage cells → relatively slowly growing
REQUIRES 3 PHASE BONE SCAN
Ewing’s sarcoma
develops in mesenchyme in bone marrow (embryonic mesoderm with loosely packed unspecialised cells) → common in long bones and pelvis
REQUIRES 3 PHASE BONE SCAN
osteochondroma
(benign bone tumours) → common, develop from growth plates → no symptoms, can be discovered incidentally → can be attached directly to bone or connected by a stem like structure
REQUIRES 3 PHASE BONE SCAN
secondary malignant bone tumour from thyroid, bronchus, lymphoma or renal carcinoma primaries
REQUIRES 2 PHASE BONE SCAN
secondary malignant bone tumour from breast, prostate or gastric primaries
REQUIRES SINGLE PHASE BONE SCAN
osteolytic lesions
where there is a loss of bone density → structural instability
REQUIRES 2 PHASE BONE SCAN
3 main causes of osteolytic bone lesions
multiple myeloma
primary bone lymphoma
metastatic bone cancer
multiple myeloma
cancer of plasma cells
REQUIRES 2 PHASE BONE SCAN
primary bone lymphoma
non Hodgkin lymphoma affecting bone that leads to bone destruction and osteolytic lesions
REQUIRES 2 PHASE BONE SCAN
metastatic bone cancer
due to release of factors that stimulate bone breakdown by osteoclasts → primary cancers breast, lung, prostate, kidney
REQUIRES SINGLE/2 PHASE BONE SCAN
osteosclerotic bone lesions
where there is increased bone density or thickening → can be benign or malignant
REQUIRES 2 PHASE BONE SCAN
osteosclerotic bone lesions potential causes
metastatic cancer
Paget’s disease
osteopetrosis
infection
Paget’s disease
excessive breakdown and formation of bone tissue → monostotic (one bone) or polystotic (multiple bones)
REQUIRES SINGLE/2 PHASE BONE SCAN
osteopetrosis
dense and brittle bones
REQUIRES 2 PHASE BONE SCAN
what is a superscan
metastatic lesions uniform across entire skeleton → absence of kidneys or bladder → everywhere is dark
what is an osteoblastic flare phenomenon
occurs <3 months chemotherapy treatment → existing lesions very hot, small lesions become visible → result of chemo treatment → new lesions after 6 months could be disease progression
types of benign bone tumours
osteoid osteoma
fibrous dysplasia
osteochondroma
osteoid osteoma
rare, affects young individuals → for young children it can deform bone or cause increased bone size
REQUIRES 3 PHASE BONE SCAN
fibrous dysplasia
abnormal growth or development of fibrous tissue within bone → can affect single or multiple bones → caused by genetic mutation leading to replacement of normal bone with fibrous tissue → can be monostotic (single bone) or polystotic (multiple bones)
REQUIRES 2 PHASE BONE SCAN
rheumatoid arthritis
autoimmune disease, inflammation in joints, common in women
REQUIRES SINGLE/2 PHASE BONE SCAN
- consider including plantar and palmar scans
avascular necrosis
aka osteonecrosis → bone tissue dies due to lack of blood supply → affects epiphysis of long bones at weight bearing joints → common at femoral head, knee, talus of foot and humeral head
REQUIRES 3 PHASE BONE SCAN
osteomyelitis
infection of bone usually by bacteria → can be acute (initial stage) or chronic (when acute is not adequately treated)
acute can develop quickly and requires prompt treatment → rapid onset of symptoms
chronic → persistent infection and inflammation often leading to bone necrosis
REQUIRES 3 PHASE BONE SCAN
hematogenous osteomyelitis
bacteria from a distant infection site (skin infection or UTI) travels through bloodstream and settles in blood → often in children long bones and adult vertebrae or pelvis
REQUIRES 3 PHASE BONE SCAN
contiguous osteomyelitis
infection spreads to bone from adjacent infected tissue (ie. open fracture, bone exposed to outside environment), infected joint replacement, infected soft tissue around bone
REQUIRES 3 PHASE BONE SCAN
bacterial osteomyelitis
caused by bacteria such as Staphylococcus aureus
REQUIRES 3 PHASE BONE SCAN
fungal osteomyelitis
less common, but can occur in immunocompromised individuals
REQUIRES 3 PHASE BONE SCAN
prosthetic loosening
detachment of movement of artificial joint from the bone it was implanted in → causes general reduction in quality of life
REQUIRES 3 PHASE BONE SCAN
- prosthetic seen as cold spot
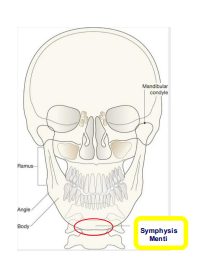
symphysis menti
at chin
sternal notch
top of sternum
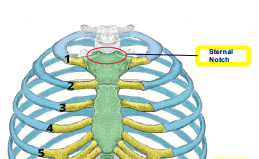
xiphoid process
bottom of sternum

right and left costal margins
ends of ribs

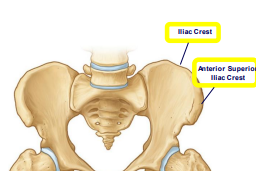
(anterior superior) iliac crest
hips
greater trochanter
proximal femur

vertebral column numbers
cervical: 7 C1-C7
thoracic: 12 T1-T12
lumbar: 5 L1-L5
sacrum: 5 fused
coccyx: 4 fused