04_Male Hormones in Development & Reproduction
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
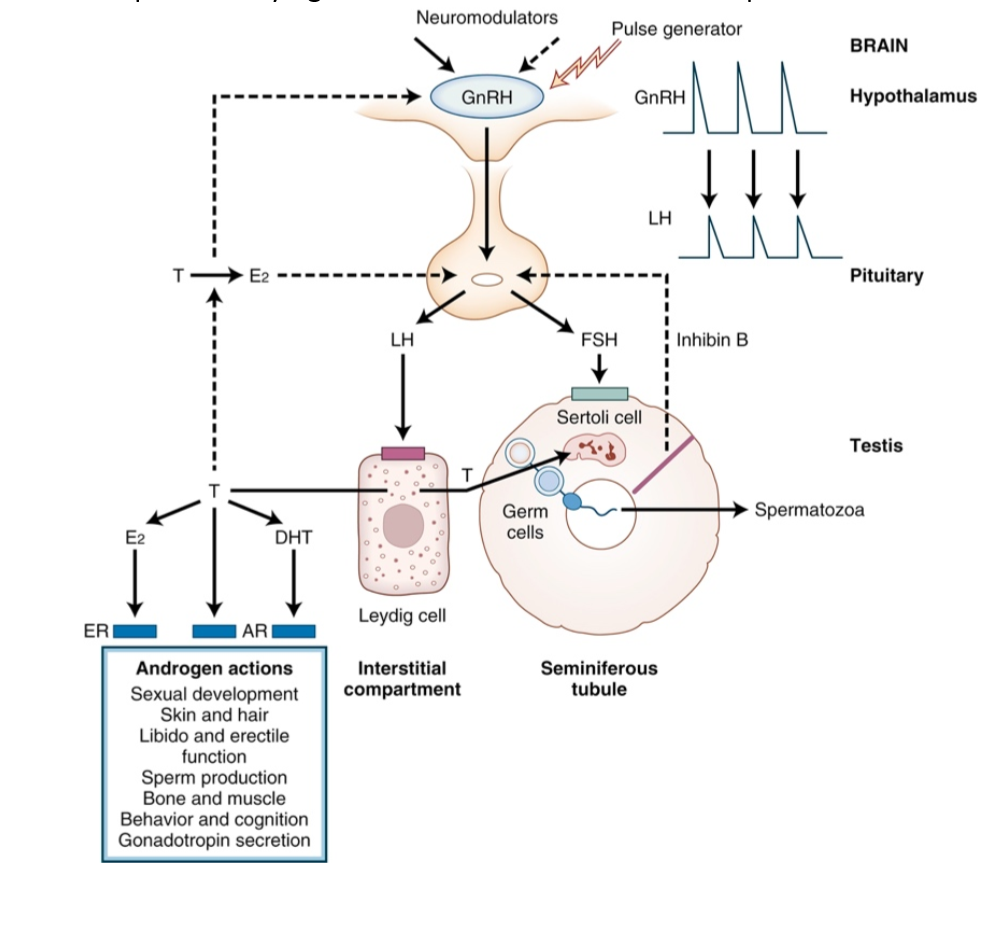
Testes
Organs responsible for producing testosterone (Leydig cells) and spermatozoa (Sertoli cells).
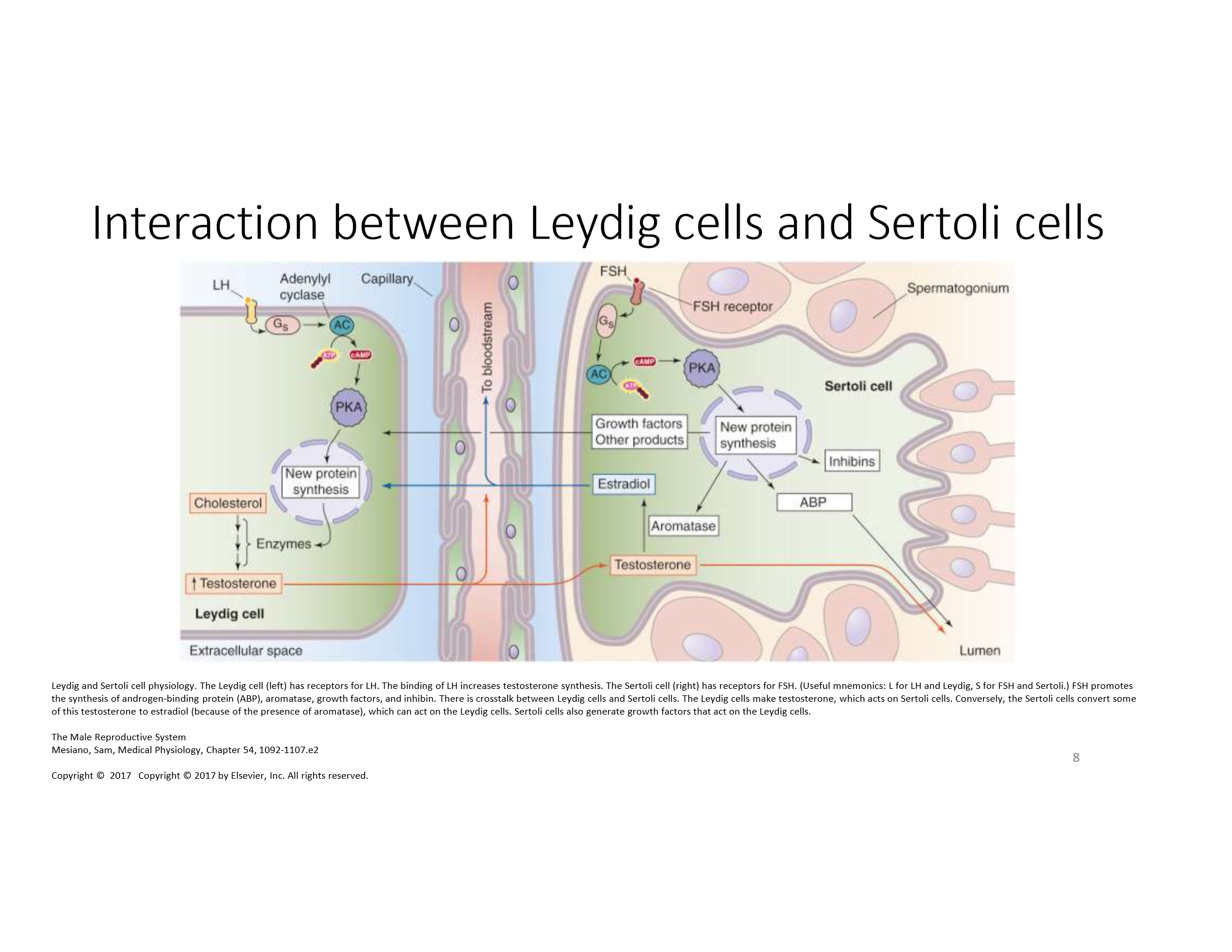
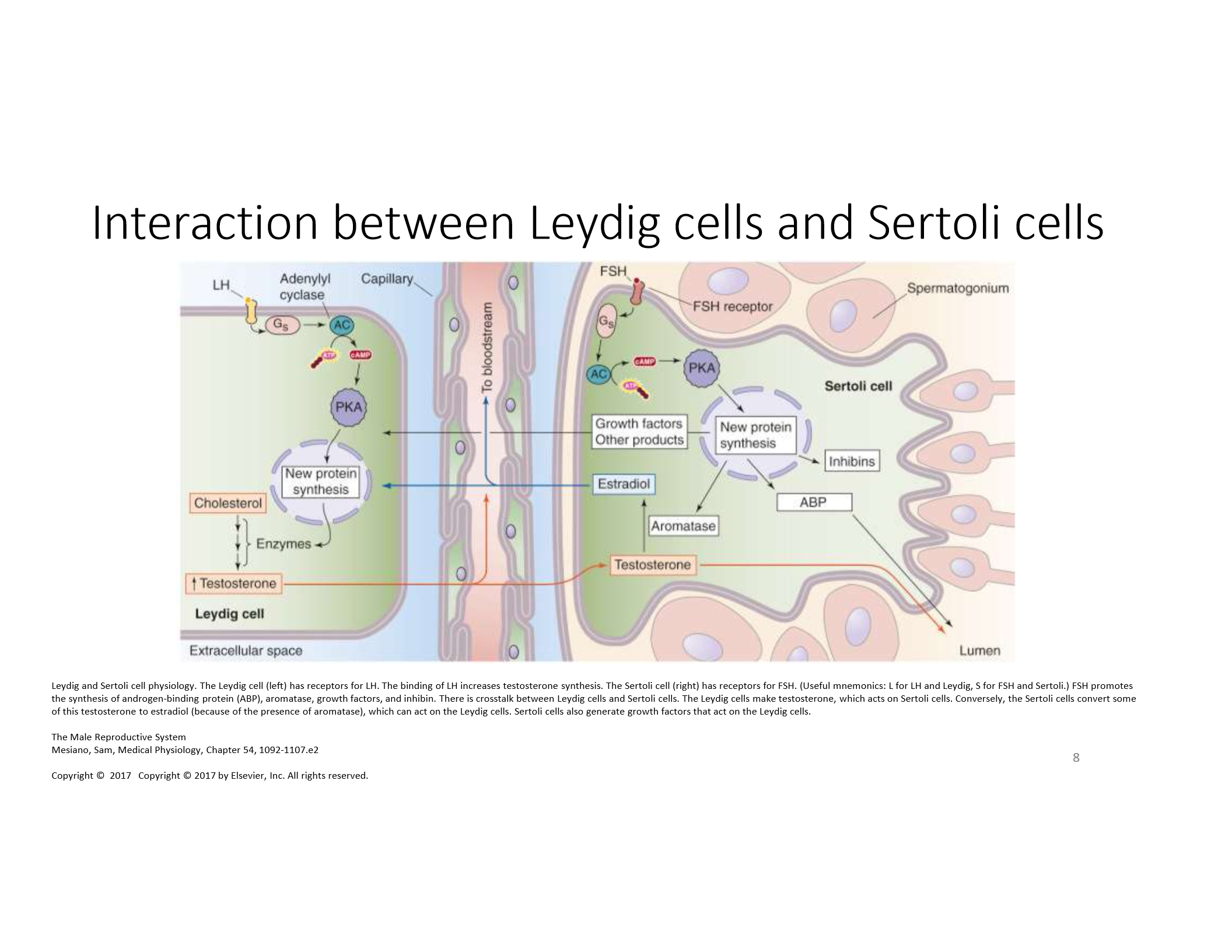
Leydig Cells
Respond to LH to produce testosterone; use cholesterol and enzymes like CYP11A1 and 17β-HSD3.
Sertoli Cells
Respond to FSH; support spermatogenesis; secrete ABP, inhibins, aromatase, and growth factors.
GnRH (Gonadotropin-Releasing Hormone)
Secreted by hypothalamus; stimulates LH and FSH release from anterior pituitary. Negatively inhibited by LH and FSH.
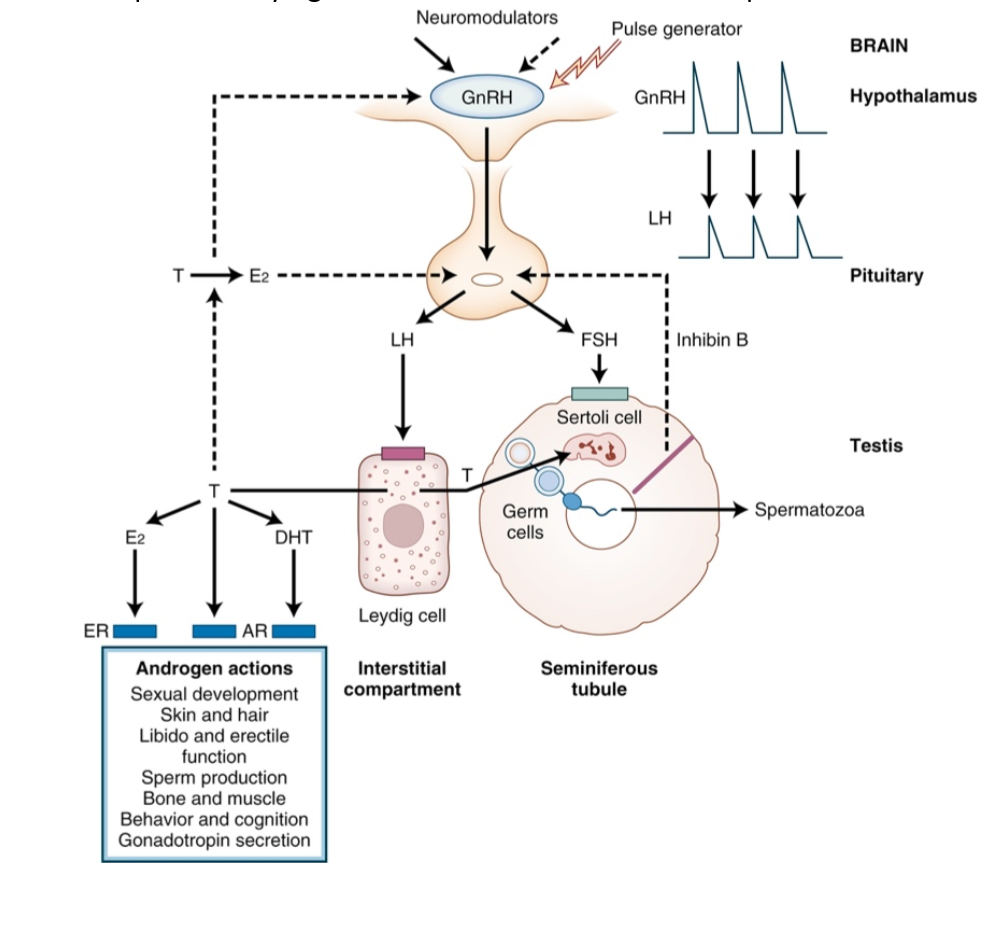
LH (Luteinizing Hormone)
Stimulates Leydig cells to produce testosterone via cAMP/PKA signaling.
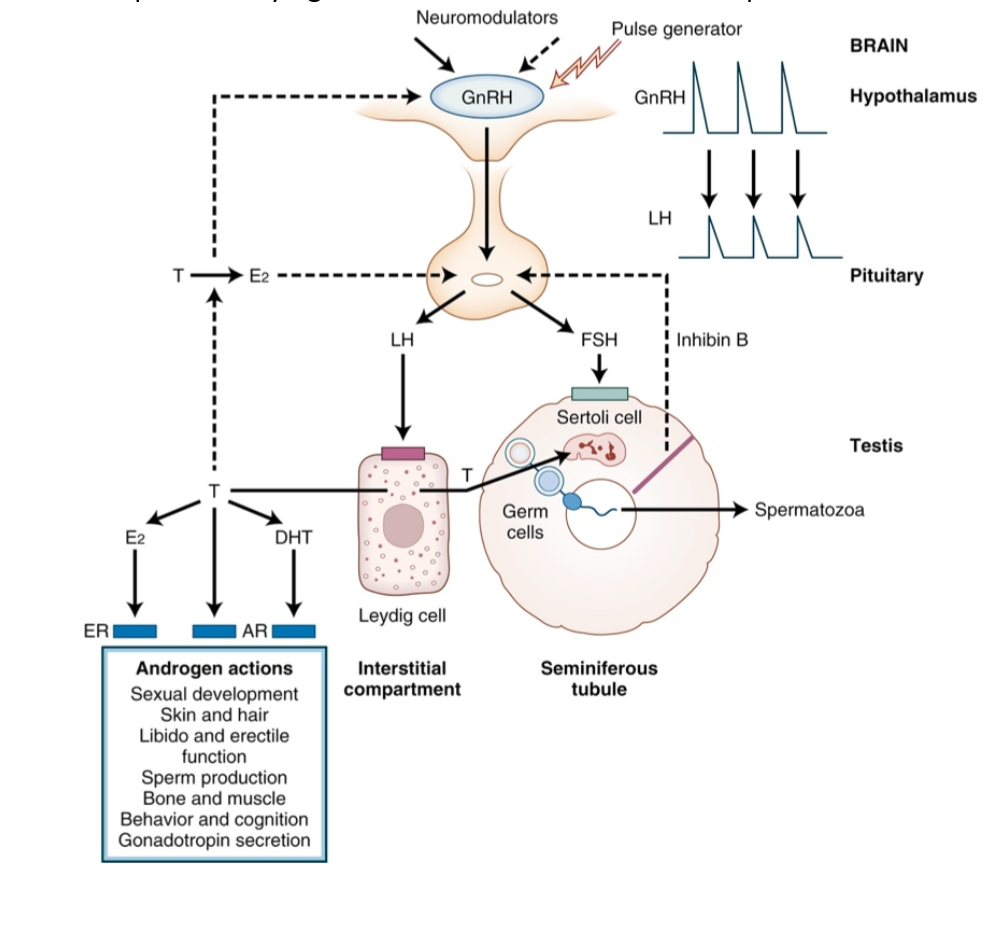
FSH (Follicle-Stimulating Hormone)
Stimulates Sertoli cells to support spermatogenesis and secrete ABP, inhibins, aromatase.
Androgen-Binding Protein (ABP)
Secreted by Sertoli cells; binds testosterone in seminiferous tubules to maintain high local concentrations.
Aromatase
Enzyme that converts testosterone to estradiol in Sertoli cells.
Inhibins
Secreted by Sertoli cells; provide negative feedback to inhibit FSH secretion.
StAR Protein
Transfers cholesterol into mitochondria for steroidogenesis.
17β-HSD3
Leydig cell enzyme that converts androstenedione to testosterone.
Sex Determination
Genetic process driven by SRY gene and SOX9; leads to testis development.
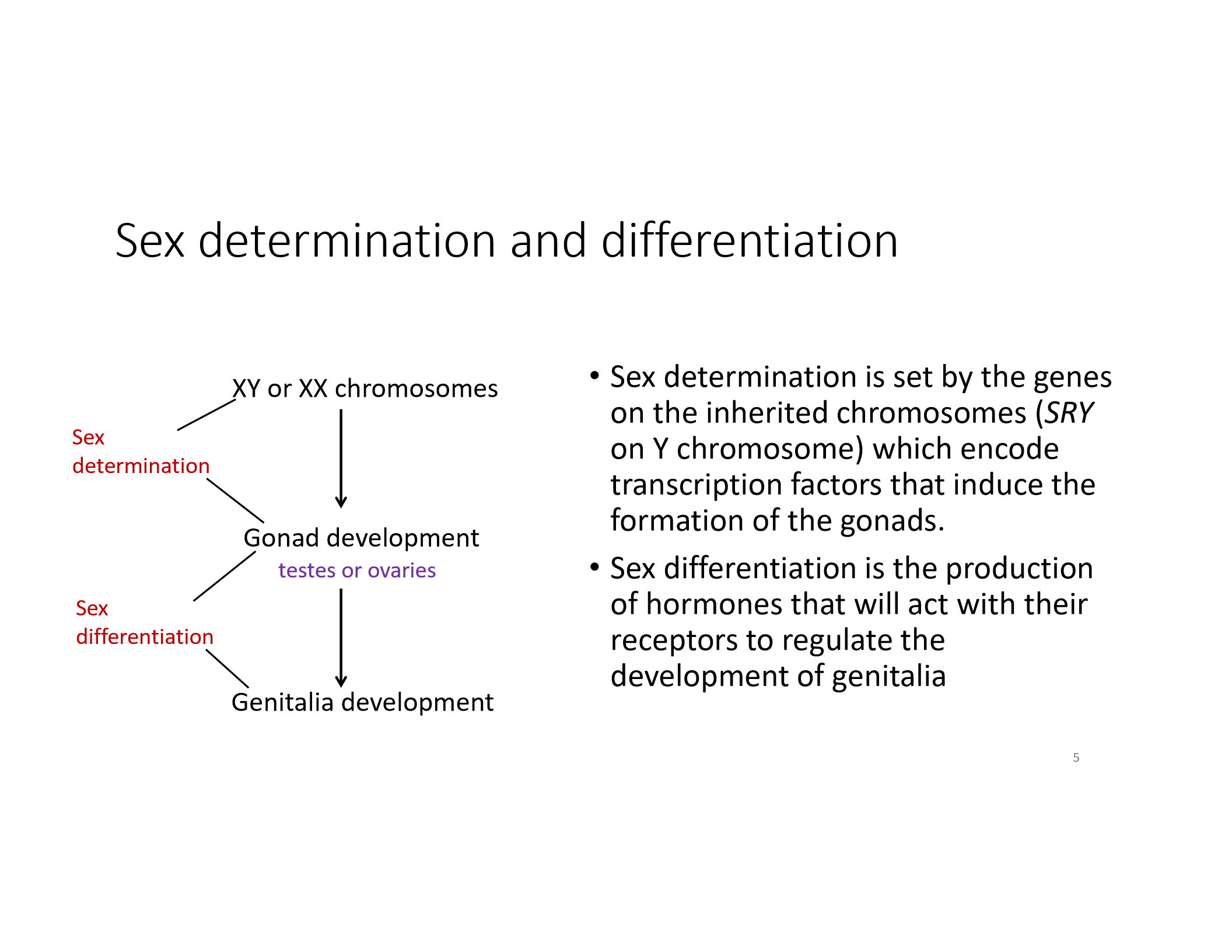
Sex Differentiation
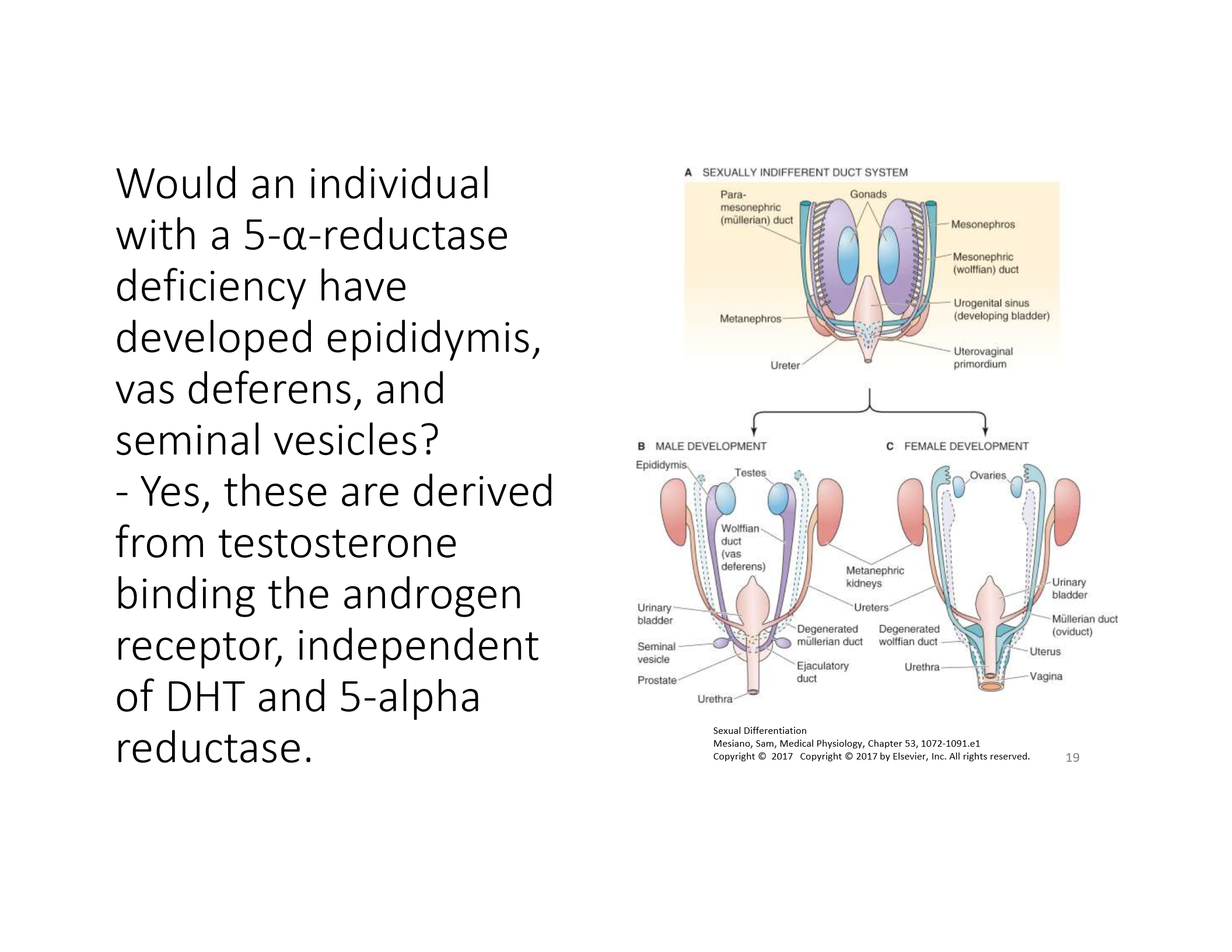
Hormonal process; testosterone and DHT lead to male genitalia and secondary sex traits.
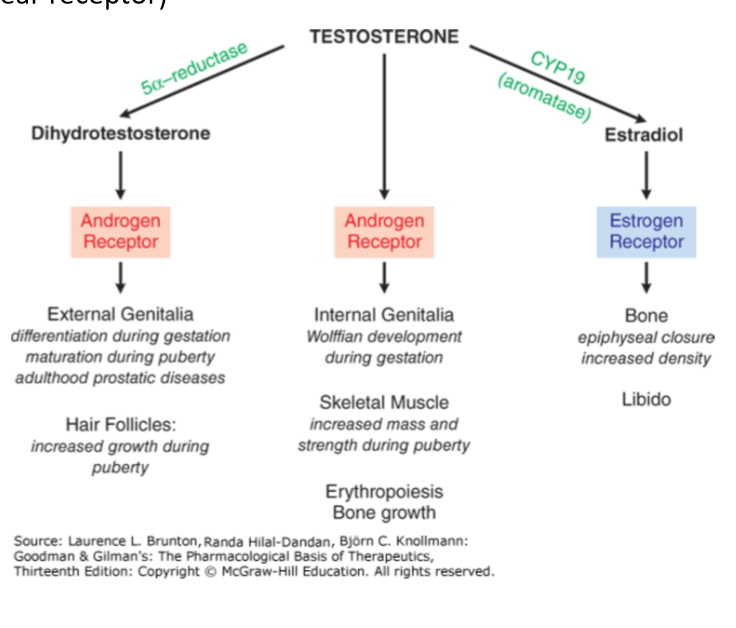
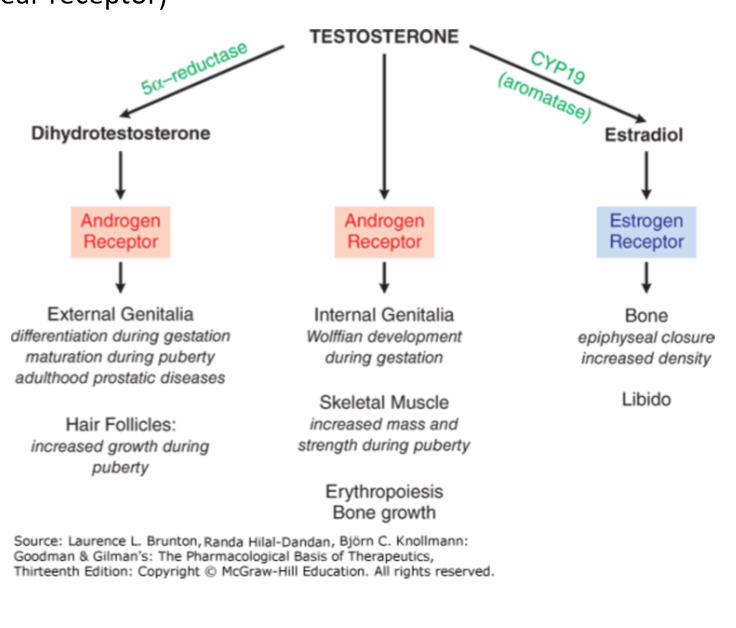
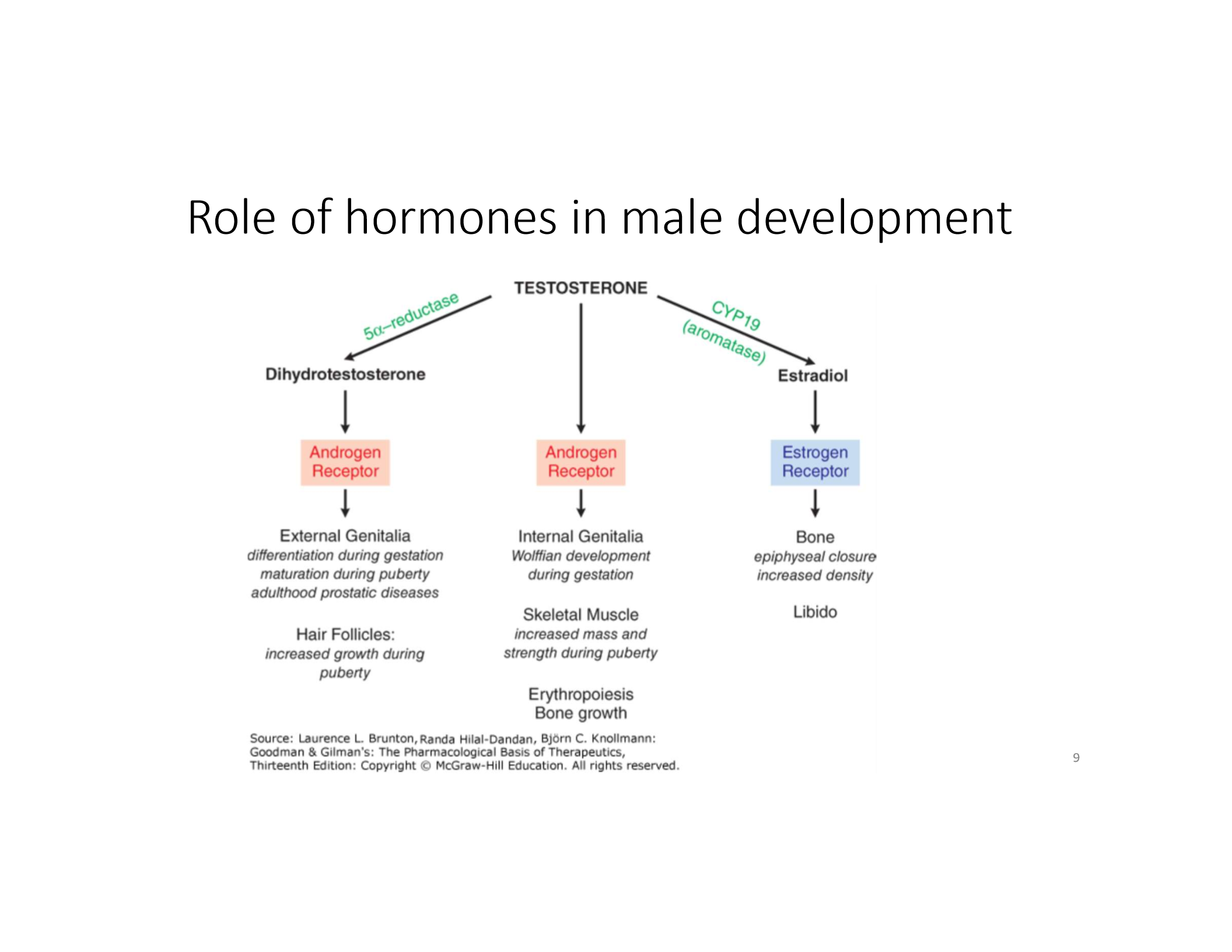
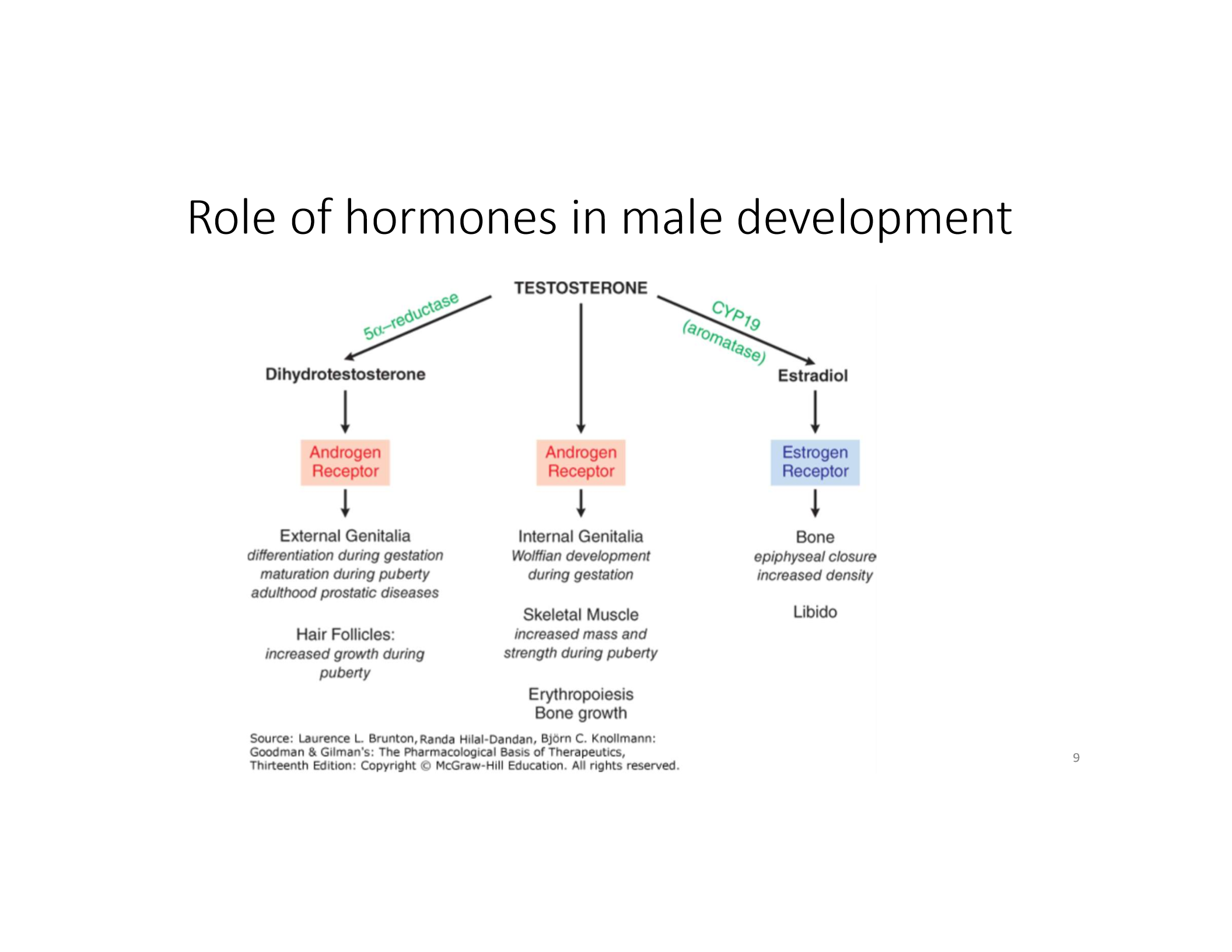
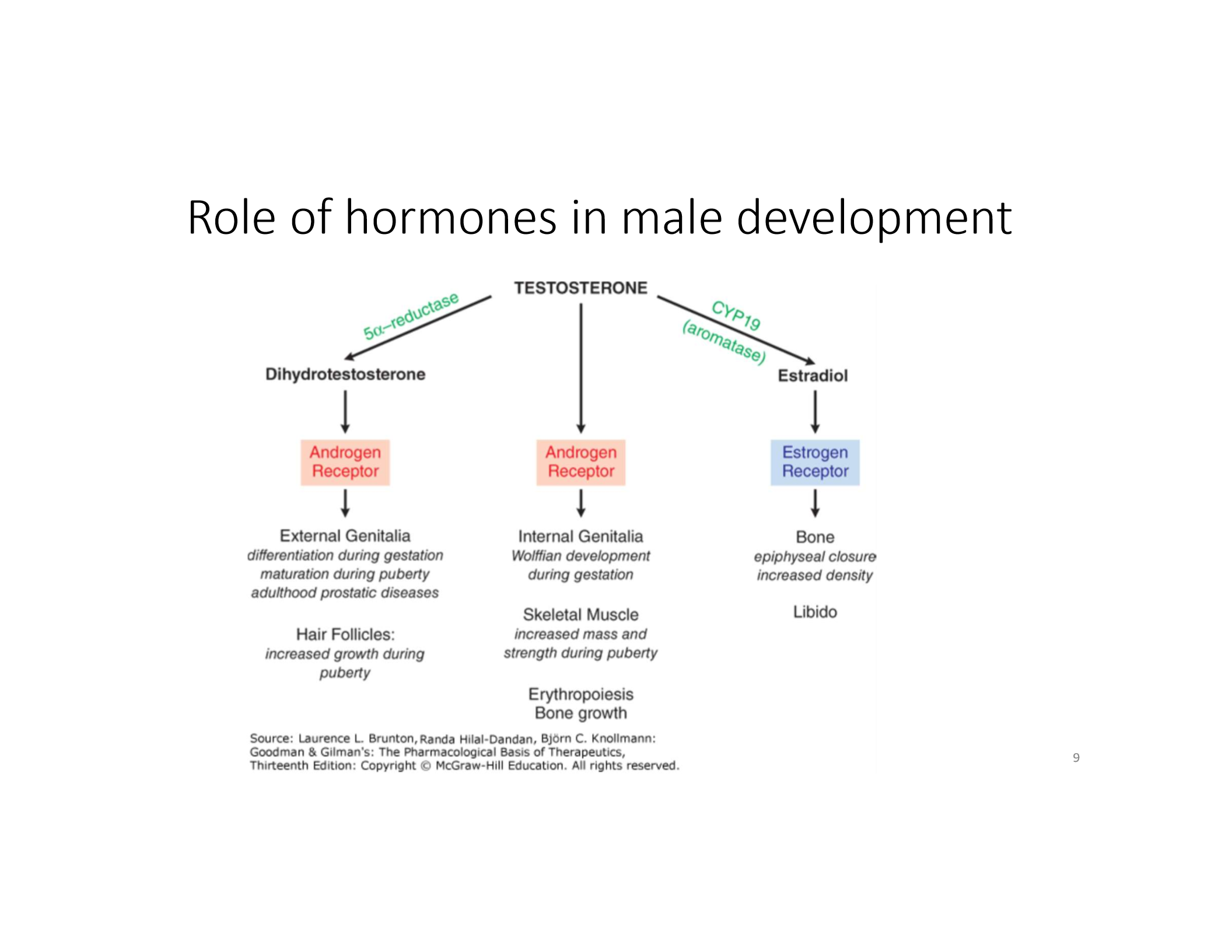
Dihydrotestosterone (DHT)
Formed from testosterone via 5α-reductase; essential for external genitalia and prostate development.
Estradiol in Males
Formed from testosterone via aromatase; contributes to bone density, libido.
Wolffian Ducts
Develop into male internal genitalia under testosterone influence.
Müllerian Ducts
Regress in males due to Anti-Müllerian Hormone (AMH) from Sertoli cells.
DHT
Hormone responsible for external genitalia development and pubertal hair growth.
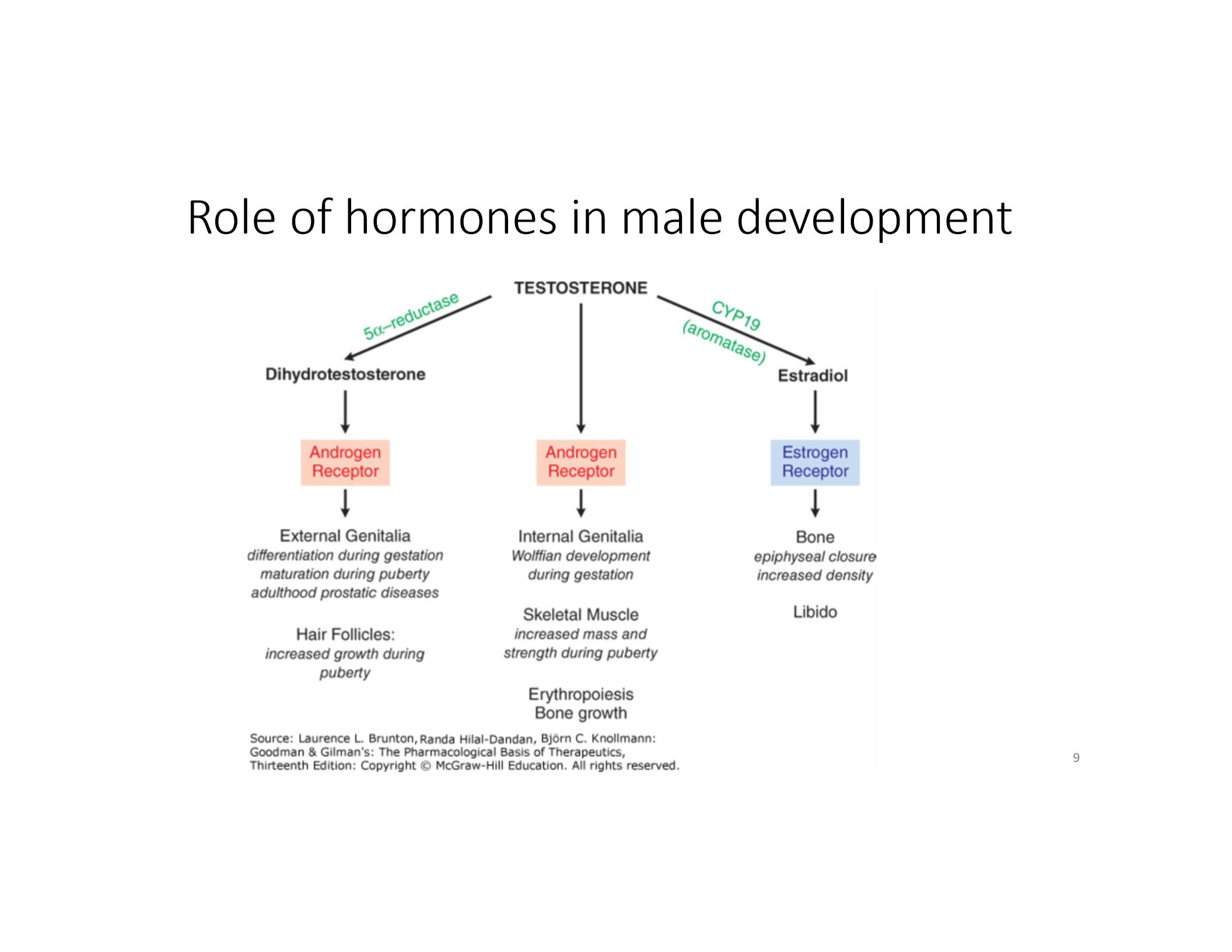
Testosterone
Hormone responsible for internal genitalia development, Wolffian development, and increased skeletal muscle mass.
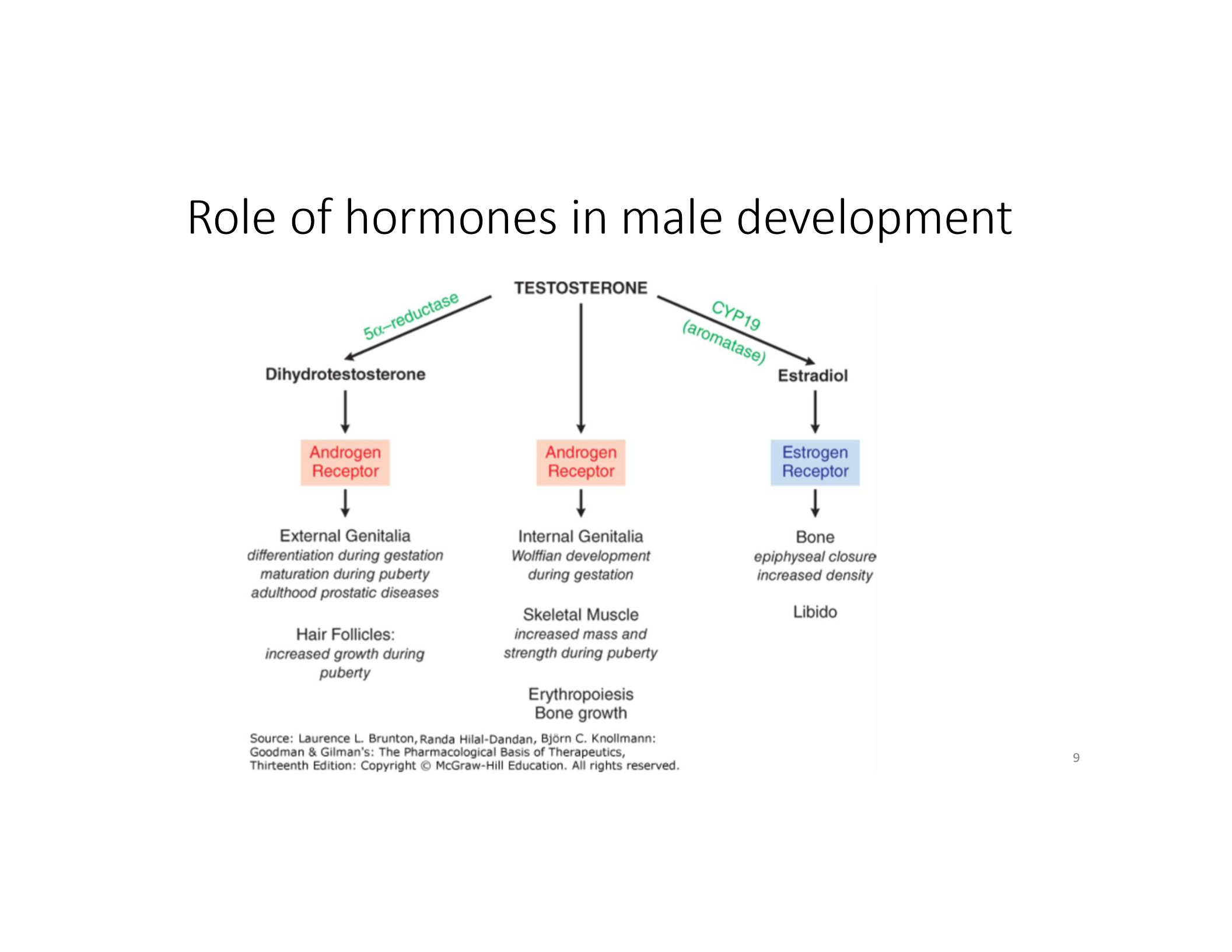
Estradiol
Hormone responsible for bone changes.
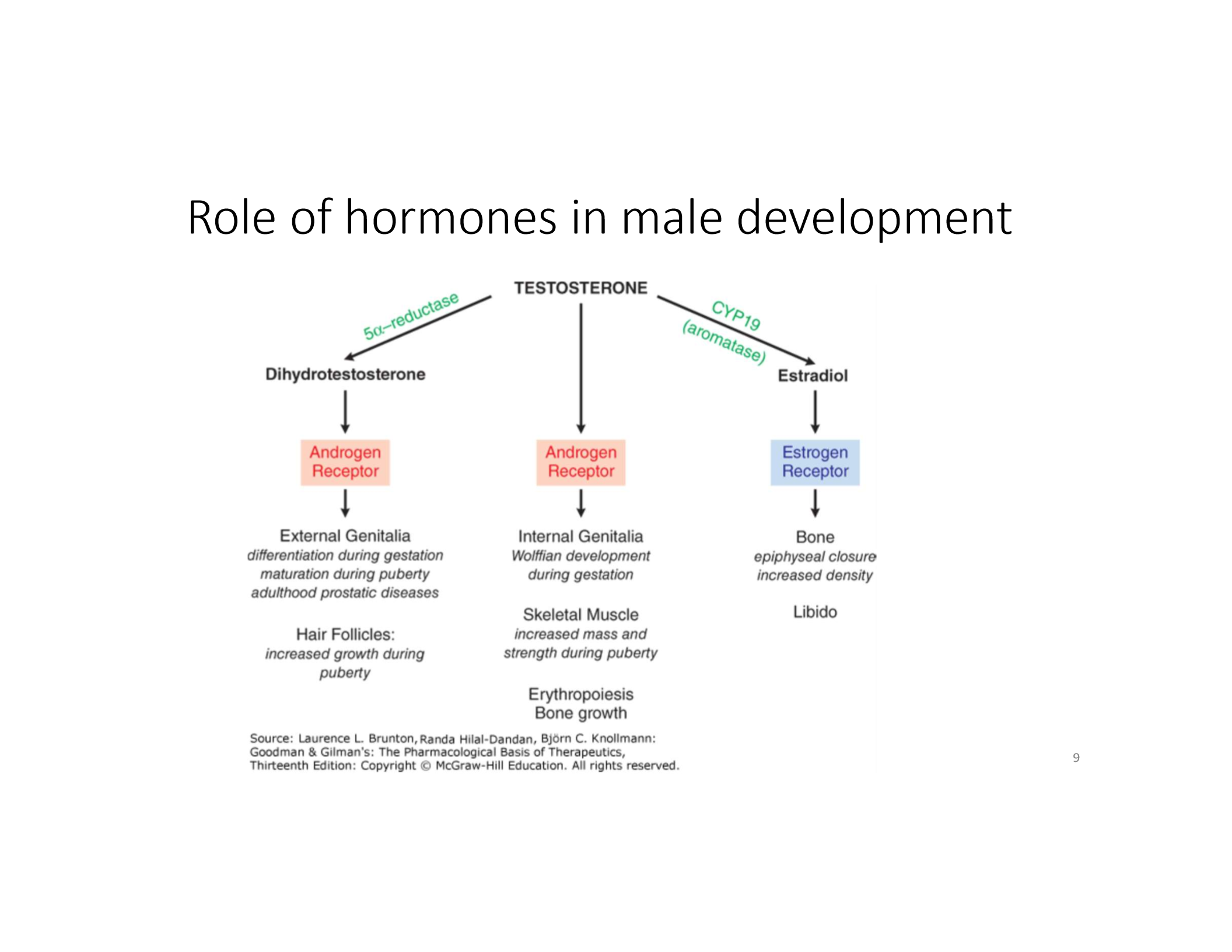
What can testosterone be converted into in males?
DHT (via 5-alpha-reductase) or estradiol (via aromatase)!
What are the two main functions of the testes?
Produce testosterone (Leydig cells) and spermatozoa (Sertoli cells).
What hormone stimulates Leydig cells and what do they produce?
LH stimulates Leydig cells to produce testosterone.
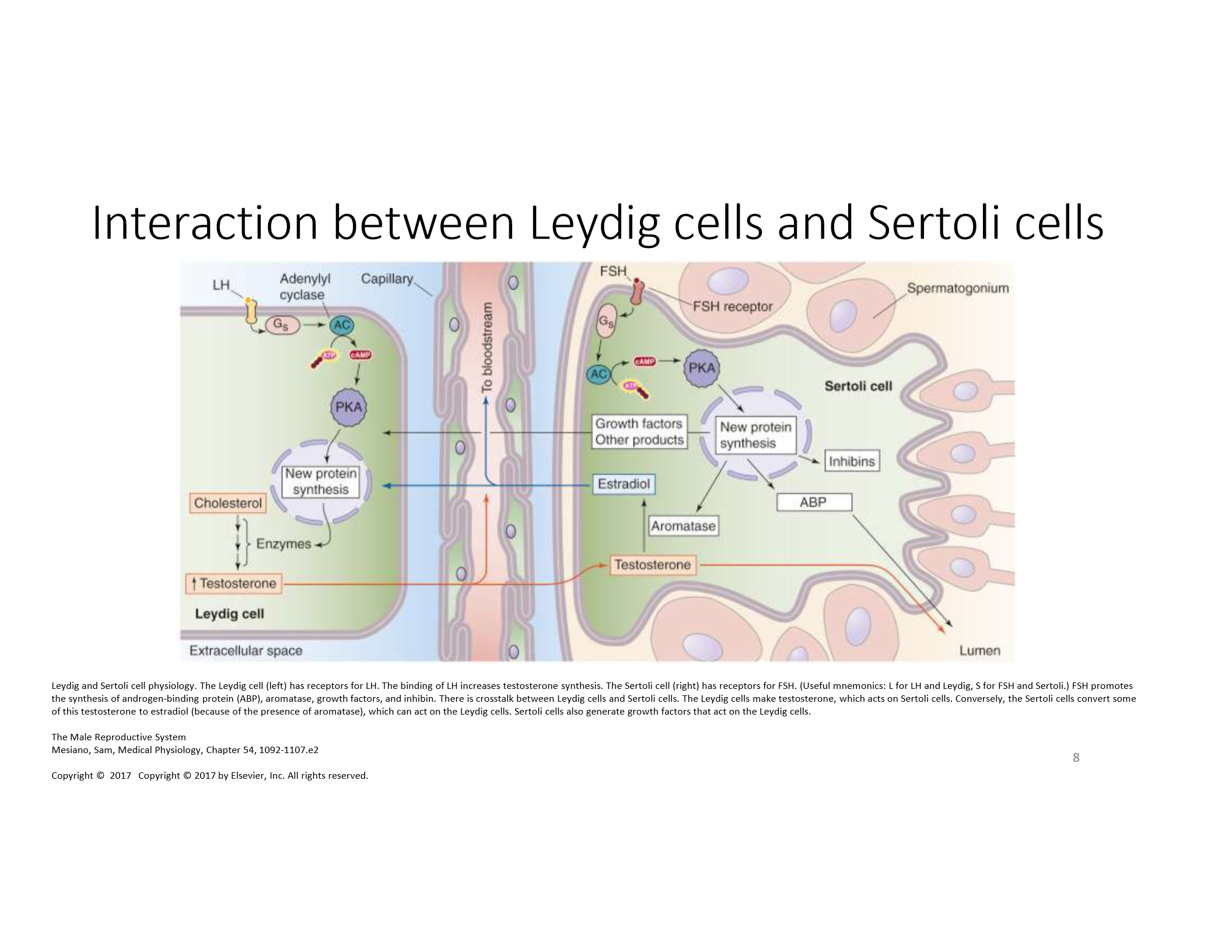
What hormone stimulates Sertoli cells and what is their function?
FSH stimulates Sertoli cells to support spermatogenesis and secrete key factors like ABP.
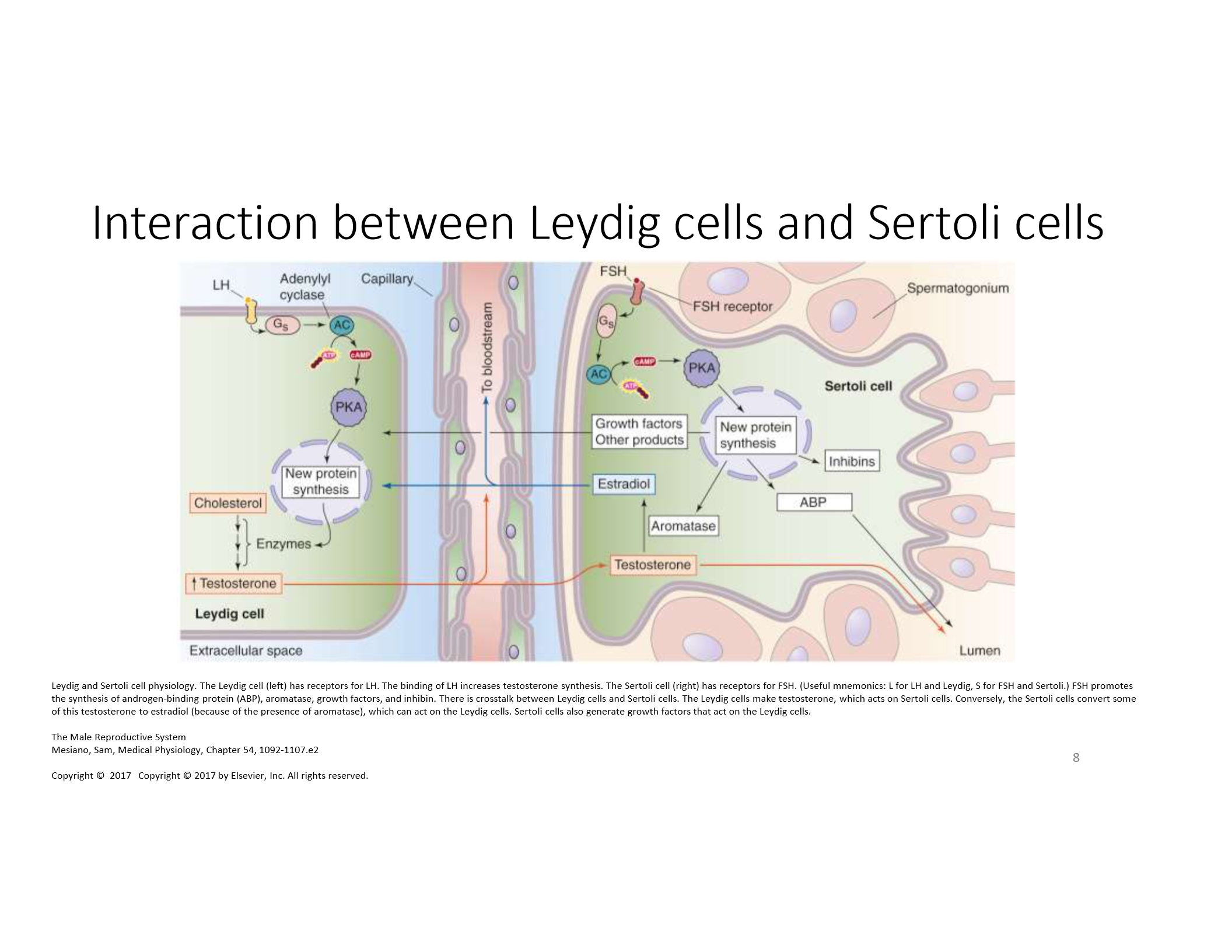
How does testosterone synthesis begin in Leydig cells?
LH binds to its receptor, triggering cAMP/PKA pathway, leading to conversion of cholesterol to testosterone.
What role does ABP play in the male reproductive system?
ABP binds testosterone in seminiferous tubules to keep local levels high for spermatogenesis.
What enzyme converts testosterone to DHT, and why is this important?
5α-reductase; DHT is essential for external genitalia development and prostate growth.
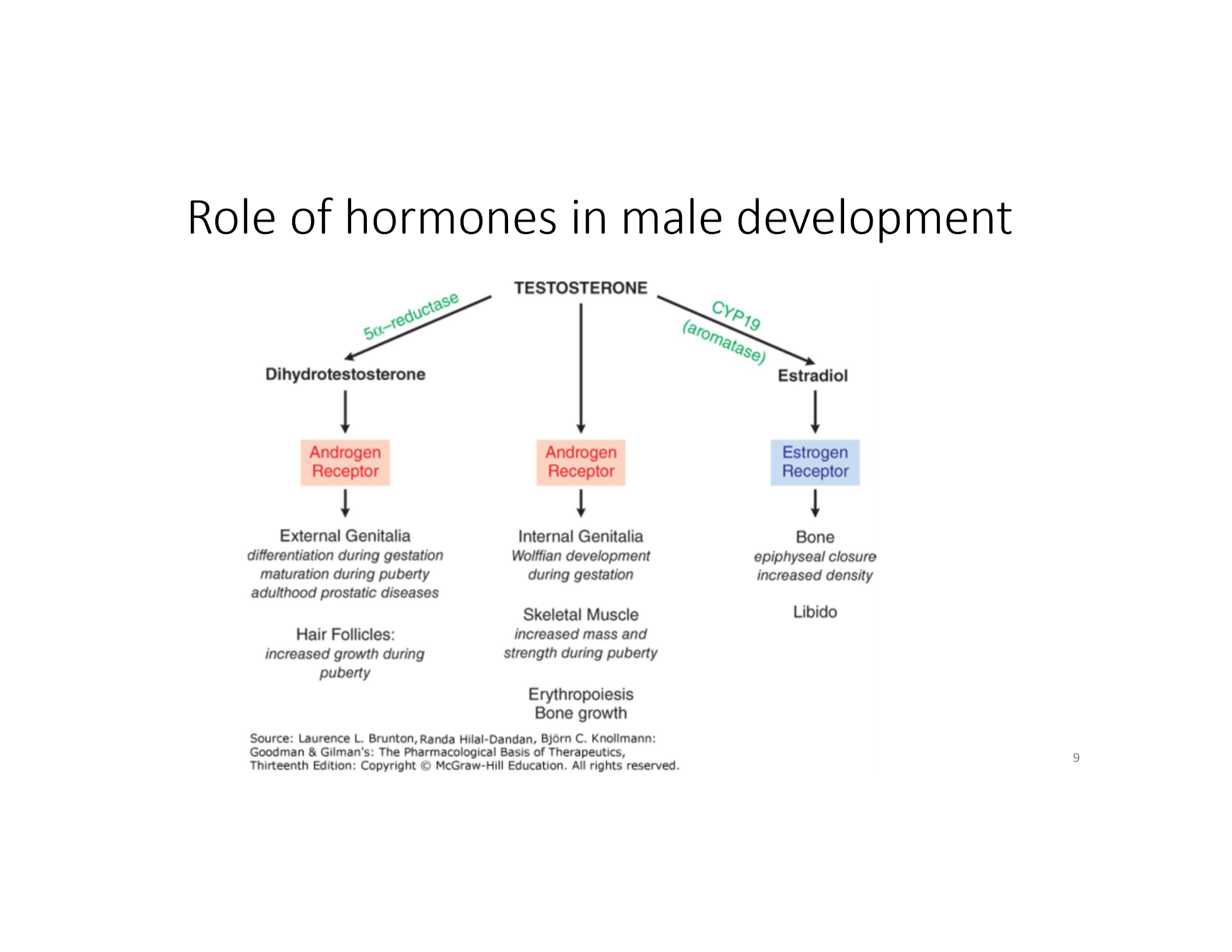
What is the function of aromatase in males?
Converts testosterone to estradiol, which is important for bone density and libido.
How does inhibin regulate FSH levels?
Inhibin provides negative feedback to reduce FSH secretion from the anterior pituitary.
What determines genetic sex and initiates testis development?
The SRY gene on the Y chromosome and the SOX9 gene.
What hormone causes regression of Müllerian ducts in males?
Anti-Müllerian hormone (AMH), secreted by Sertoli cells.
When are testosterone levels highest during life?
During fetal genital development, neonatal period, puberty, and early adulthood. LH and FSH are highest during puberty as well.
What is the function of GnRH in male reproduction?
Stimulates anterior pituitary to release LH and FSH.
What does LH do in males?
Stimulates Leydig cells in testes to produce testosterone.
What does FSH do in males?
Stimulates Sertoli cells to support spermatogenesis.
What do Sertoli cells produce to regulate FSH?
Inhibin B, which inhibits FSH secretion via negative feedback.
How does testosterone regulate the HPG axis?
Exerts negative feedback on both the hypothalamus (↓ GnRH) and pituitary (↓ LH).
What is the role of testosterone in sperm production?
Maintains the seminiferous epithelium and supports spermatogenesis via Sertoli cell stimulation.
What two hormones are essential for spermatogenesis?
FSH (activates Sertoli cells) and testosterone (from LH-stimulated Leydig cells).
What happens to spermatogenesis with exogenous testosterone use?
Decreases due to suppressed LH/FSH → reduced intratesticular testosterone.
What is the role of testosterone in sperm production?
Maintains the seminiferous epithelium and supports spermatogenesis via Sertoli cell stimulation.
What two hormones are essential for spermatogenesis?
FSH (activates Sertoli cells) and testosterone (from LH-stimulated Leydig cells).
What happens to spermatogenesis with exogenous testosterone use?
Decreases due to suppressed LH/FSH → reduced intratesticular testosterone.
What enzyme converts testosterone to DHT?
5α-reductase.
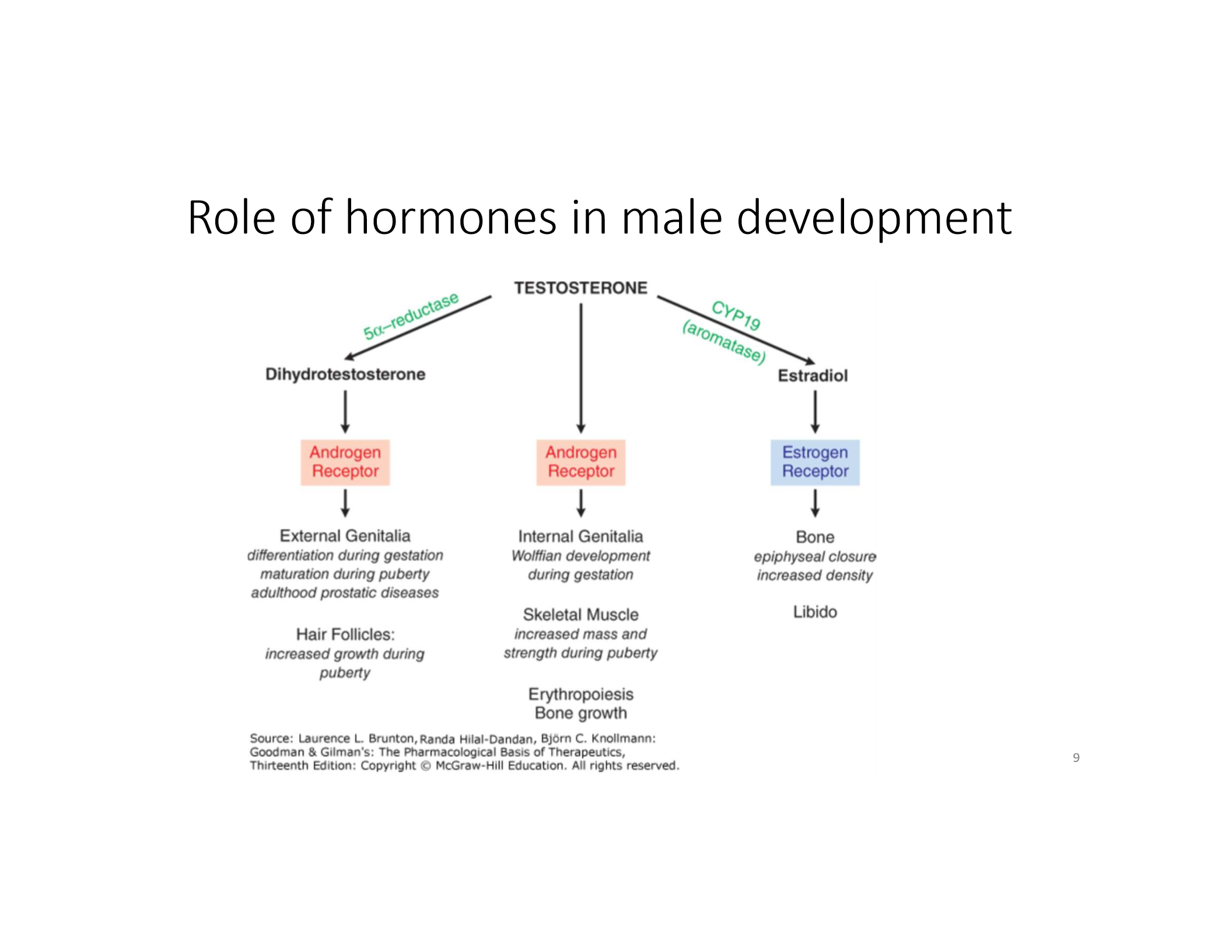
What is the role of DHT in male development?
Stimulates development of external genitalia (penis, scrotum), prostate, and male-pattern features.
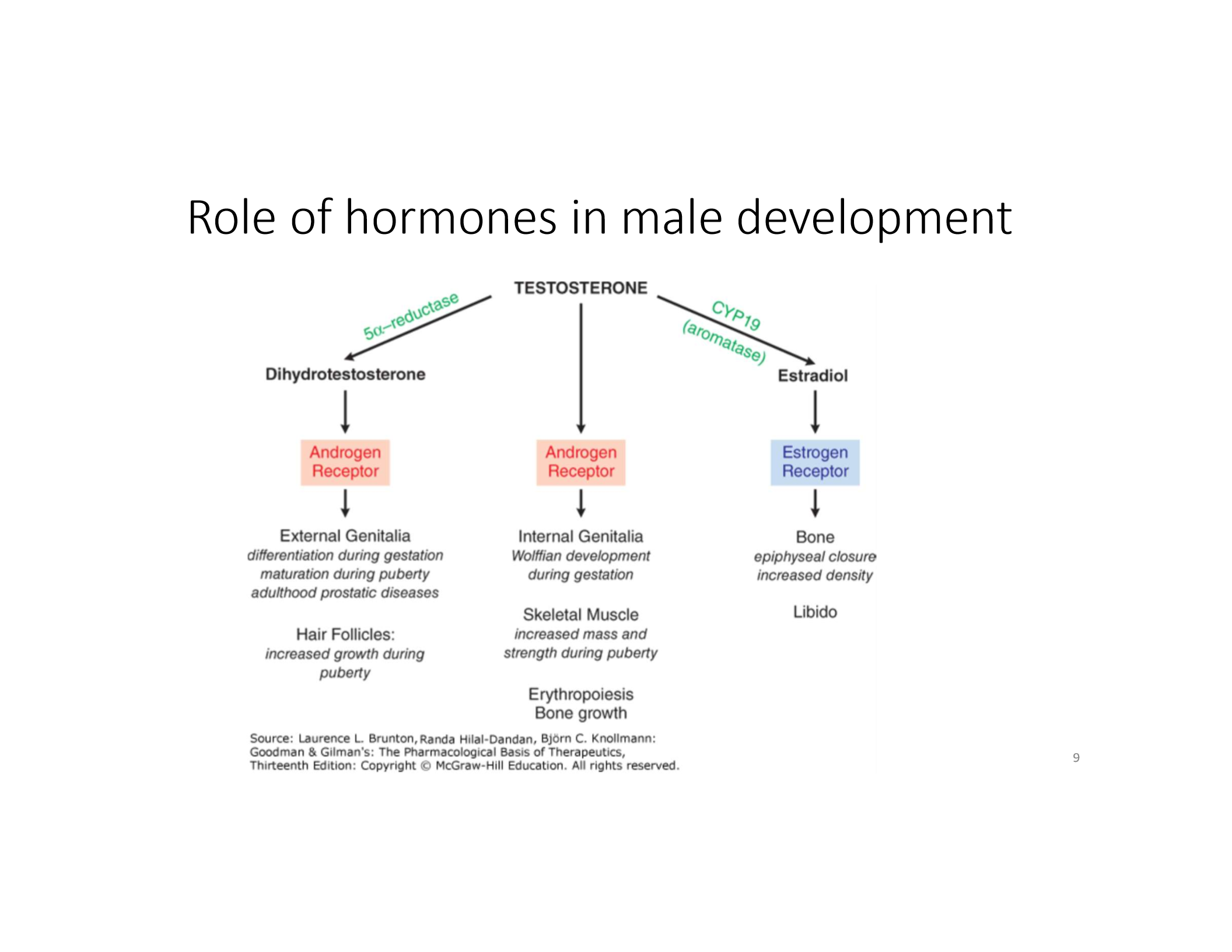
What hormone is critical for internal genitalia (epididymis, vas deferens, seminal vesicles)?
Testosterone.
What hormone prevents development of female internal genitalia in males?
Anti-Müllerian hormone (AMH), produced by Sertoli cells.
What hormonal change initiates puberty in males?
Pulsatile secretion of GnRH → ↑ LH/FSH → ↑ testosterone.
What is the first physical sign of male puberty?
Testicular enlargement.
List the sequence of pubertal events in males.
Testicular enlargement → pubic hair → penile growth → growth spurt → voice deepening.
What is primary hypogonadism?
Testicular failure → low testosterone, high LH/FSH (hypergonadotropic).
What is secondary hypogonadism?
Hypothalamic or pituitary dysfunction → low testosterone, low LH/FSH (hypogonadotropic).
Lab findings for primary vs. secondary hypogonadism?
• Primary: ↓ testosterone, ↑ LH/FSH • Secondary: ↓ testosterone, ↓ LH/FSH
Causes of primary hypogonadism?
Klinefelter syndrome, testicular trauma, chemotherapy, mumps orchitis.
Causes of secondary hypogonadism?
Kallmann syndrome, pituitary tumors, anabolic steroid use.
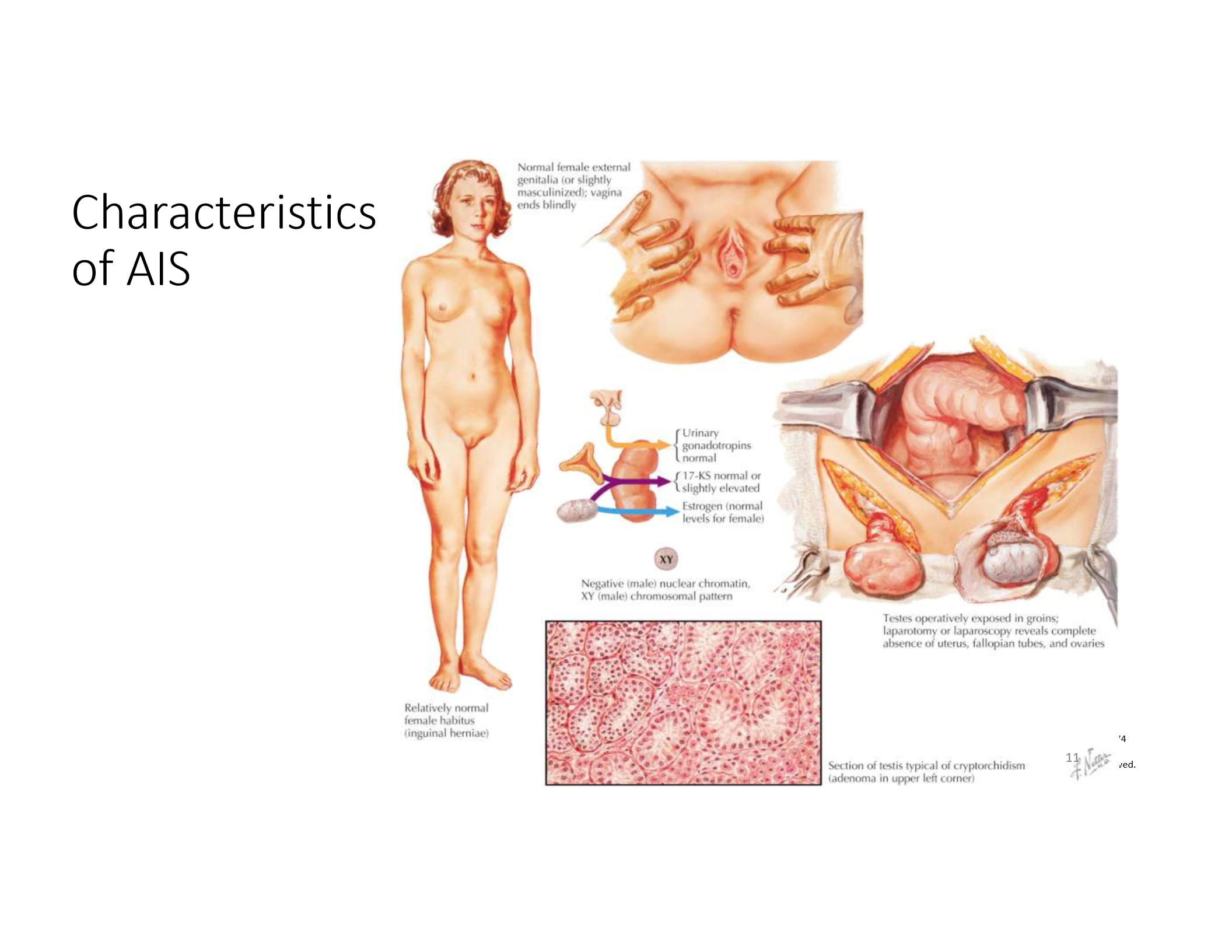
What is androgen insensitivity syndrome (AIS)?
46,XY individuals with non-functional androgen receptors → female external genitalia, no uterus, undescended testes.
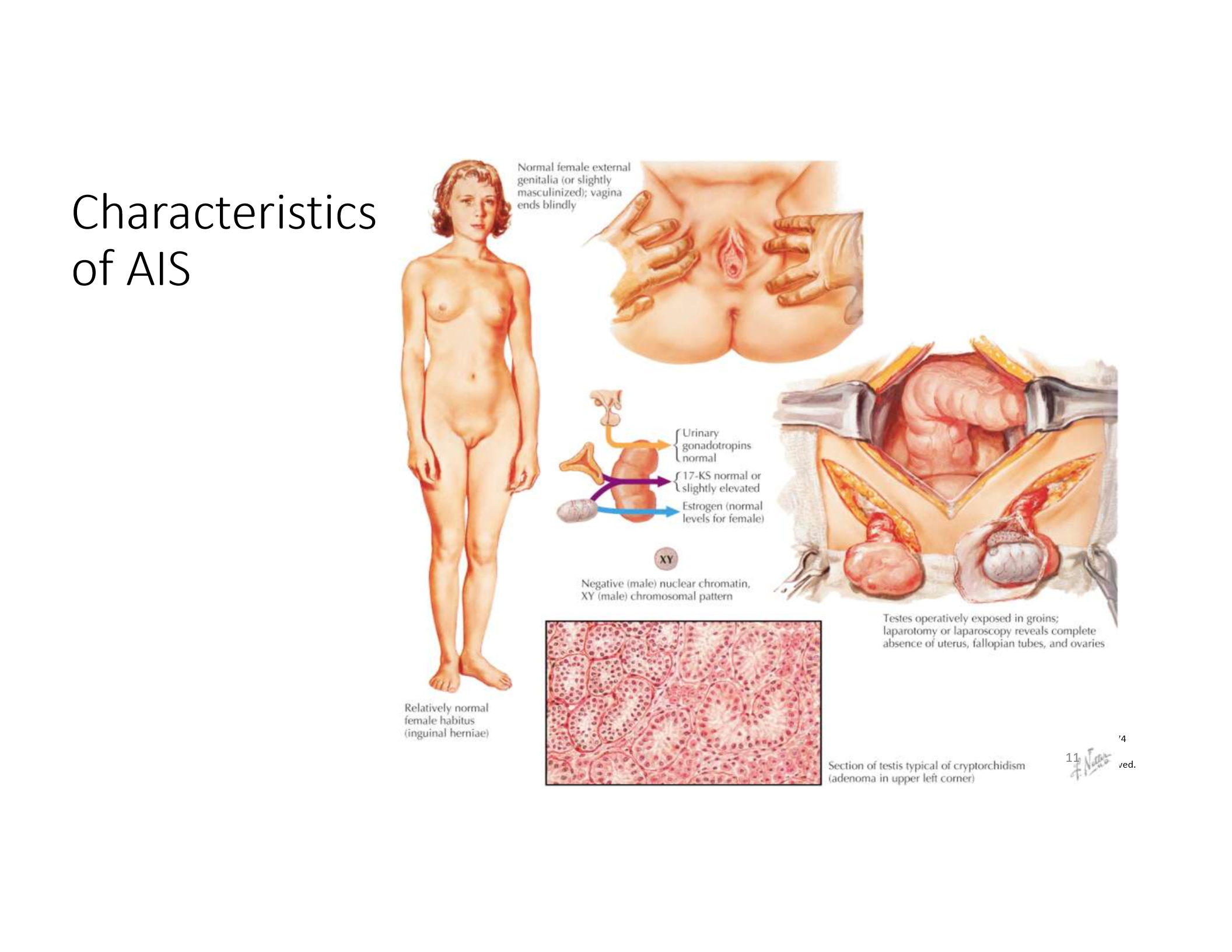
Clinical features of complete AIS?
Normal breast development, absent uterus/upper vagina, scant pubic/axillary hair, elevated testosterone and LH.
What is 5α-reductase deficiency?
Inability to convert testosterone to DHT → ambiguous or female external genitalia at birth, virilization at puberty.
A 46,XY individual presents with female external genitalia, no uterus, and intra-abdominal testes. What is the most likely diagnosis?
Androgen Insensitivity Syndrome (AIS). Explanation: Despite having XY chromosomes and normal testes, the body's cells can't respond to androgens due to defective androgen receptors. As a result, external genitalia are female, but there are no internal female structures (due to AMH from Sertoli cells). Testes remain undescended.
A male patient taking anabolic steroids has low sperm count, small testes, and normal or high total testosterone. What is the mechanism?
Exogenous testosterone suppresses GnRH → ↓ LH/FSH → ↓ intratesticular testosterone → ↓ spermatogenesis. Explanation: Exogenous androgens inhibit the HPG axis, reducing LH/FSH production. Without LH, Leydig cells stop making intratesticular testosterone, which is critical for spermatogenesis. Sertoli cells lose testosterone support → infertility.
A newborn with ambiguous genitalia, normal male internal reproductive structures, and low DHT levels. Diagnosis?
5α-reductase deficiency. Explanation: Testosterone is normal (so Wolffian structures develop), but the enzyme that converts testosterone to DHT is deficient, preventing male external genitalia development. At puberty, testosterone rises and may cause partial masculinization.
A male has low testosterone, high LH and FSH. What type of hypogonadism is this and what is a likely cause?
Primary hypogonadism (testicular failure); possible cause: Klinefelter syndrome. Explanation: The testes fail to produce testosterone despite LH/FSH stimulation, leading to compensatory rise in these pituitary hormones. Common causes include genetic abnormalities like 47,XXY (Klinefelter), mumps orchitis, or radiation.
A male has low testosterone, low LH and FSH. What type of hypogonadism is this and what is a likely cause?
Secondary hypogonadism (hypothalamic/pituitary issue); possible cause: Kallmann syndrome or pituitary tumor. Explanation: Defects in GnRH production (e.g., Kallmann syndrome) or pituitary damage reduce LH/FSH output → low testosterone. Often associated with delayed puberty and anosmia in Kallmann.
Why does obesity contribute to male infertility?
Increased aromatase activity in adipose tissue converts testosterone to estradiol → ↓ GnRH/LH/FSH → ↓ intratesticular testosterone → ↓ spermatogenesis. Explanation: High estradiol from fat cells negatively feeds back on the HPG axis, leading to lower gonadotropins and suppressed spermatogenesis. This also explains low libido and erectile dysfunction in obese men.