Chapter 36: geriatric emergencies
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Venous stasis in an older patient creates problems such as superficial phlebitis and:
Deep vein thrombosis
which can lead to pulmonary embolism
Although more typically seen in children, ____________ can also cause serious illness in older people, especially those with lung disease or weakened immune systems.
RSV
Which interview technique should you use when addressing a geriatric patient?
Speak loudly and slowly.
Listen carefully to the answers the patient provides.
Refer to the patient by his or her first name.
Have both you and your partner ask questions.
The best thing you can do is listen carefully to the answers the patient provides.
You are assessing an 80-year-old patient who explains that he was awakened by a sudden feeling of suffocation and respiratory distress. These symptoms are characteristic of:
orthopnea.
exertional dyspnea.
intermittent sleep apnea.
paroxysmal nocturnal dyspnea.
paroxysmal nocturnal dyspnea.
Paroxysmal nocturnal dyspnea is a condition that is characterized by a sudden attack of respiratory distress that wakes the person at night when the patient is in a reclining position. The respiratory distress is caused by fluid accumulation in the lungs.
Which of the following is a noncontrollable risk factor for stroke?
Age
Atrial fibrillation
Hypertension
Obesity
Age
In arteriosclerosis, overproduction of abnormal collagen and decreased quantities of elastin lead to:
decreased coronary artery perfusion.
increased coronary artery perfusion.
narrowing pulse pressure.
hypotension.
Overproduction of abnormal collagen and decreased quantities of elastin lead to decreased coronary artery perfusion.
Which of the following statements is true regarding delirium?
It has a slow onset and leads to progressive disorientation.
Memory remains intact.
It is the result of an irreversible metabolic disorder.
It is rare in older hospitalized patients.
In delirium, memory generally remains intact.
You are working on a geriatric patient who reports severe abdominal pain radiating through her back and flank. She also reports discomfort in her right leg, and your assessment reveals a diminished pulse in this extremity. What should you suspect?
Abdominal aortic aneurysm
Peptic ulcer disease
Pulmonary embolism
Venous stasis
These signs are indicative of an abdominal aortic aneurysm (AAA).
Which of the following groups is most likely to commit suicide?
Teenage girls (any ethnicity)
African American women older than age 65
College-educated males ages 45 to 65
White males older than age 85
While males older than the age of 85
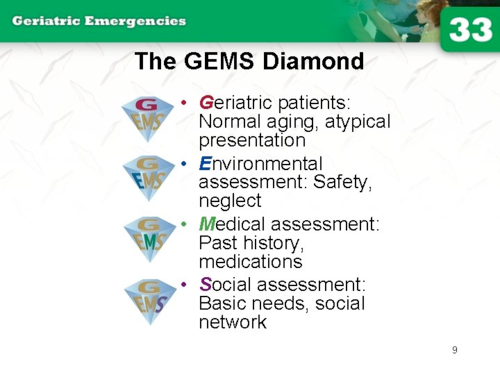
Which of the following would be part of the “S” part of the GEMS diamond?
Activities of daily living
Hazardous living conditions
Normal changes of aging
Polypharmacy
The “S” in the GEMS diamond stands for “social assessment.” Activities of daily living would fall under this category.

During auscultation of a patient’s lungs, you hear crackles. These lung sounds are caused by air passing through:
constricted airways.
thick secretions in the airways.
fluid in the alveoli.
an inflamed airway.
You will hear crackles when there is fluid in the lungs and alveoli.
Which of the following questions should you ask if you suspect a patient may have congestive heart failure?
“How many hours of sleep do you get each night?”
“In what position do you normally sleep?”
“How many pillows do you sleep on?”
“Do you take any medication to help you sleep at night?”
The need to sleep on several pillows suggests early congestive heart failure.
because lying flat can cause fluid to accumulate in the lungs. This symptom, called orthopnea, is a sign that the heart is not pumping blood effectively.

When assessing a geriatric patient who has possibly experienced an acute ischemic stroke, it is most important to:
administer 324 mg of aspirin as soon as possible.
determine the onset of the patient's symptoms.
ascertain about a history of atrial fibrillation.
determine if the patient has risk factors for a stroke.
determine the onset of the patient's symptoms.
A 69-year-old female was involved in a motor vehicle crash. She is semiconscious with a blood pressure of 80/50 mm Hg and a heart rate of 74 beats/min that is weak. Her daughter, who was uninjured in the crash, tells you that her mother has a history of hypertension and takes beta-blockers. Because this patient is probably in shock, what is the most likely explanation for the absence of tachycardia?
Deterioration of the cardiac conduction system
The effects of her antihypertensive medication
Failure of the parasympathetic nervous system
Intrathoracic bleeding and cardiac compression
The effects of her antihypertensive medication
When faced with a situation in which an older patient with a terminal illness is in cardiac arrest, but written documentation regarding the patient's wishes cannot be located, the EMT should:
allow the patient to die in peace.
contact medical control for advice.
try to locate the documentation.
attempt to resuscitate the patient.
attempt to resuscitate the patient.
You are dispatched to a residence for an 80-year-old female who fell. When you arrive, you find the patient conscious, lying in a recumbent position on the floor in her living room. In addition to providing the appropriate treatment, you should ask the patient if:
she became dizzy or fainted before falling.
she takes medications for Alzheimer disease.
she attempted to catch herself before falling.
a family member regularly checks up on her.
she became dizzy or fainted before falling.
Talking about an elderly patient in front of him or her to other members of the family:
will anger the patient and result in his or her refusal to accept care or transport.
is usually beneficial because the patient's cognitive skills are typically impaired.
might cause the patient to think that he or she has no say in making decisions.
often causes the patient to become paranoid and untrusting of your help.
might cause the patient to think that he or she has no say in making decisions.
Which of the following statements regarding communications with the elderly is correct?
Explain the justification for a procedure after it has been completed.
Older patients have difficulty understanding when they are stressed.
Attempt to calm the elderly patient by using his or her first name.
The majority of elderly patients are hearing or visually impaired.
Older patients have difficulty understanding when they are stressed.
When an elderly patient presents you with multiple over-the-counter medications that he or she is taking, it is most important to:
ask the patient to explain what each medication is used for.
recall that the patient is at risk for negative medication interactions.
contact each of the physicians whose names are on the medications.
look up all of the medications before providing care to the patient.
recall that the patient is at risk for negative medication interactions.
EMTs are dispatched to a residence for an 80-year-old woman who is ill. The patient's daughter states that her mother almost fainted after going to the bathroom and that her pulse was very slow. The patient's pulse rate is 80 beats/min and irregular, and she is conscious and alert. The EMTs should suspect that the patient:
took too much of her medication.
has an abdominal aortic aneurysm.
experienced a vasovagal response.
has a gastrointestinal hemorrhage.
experienced a vasovagal response.
an overreaction of the nervous system to a trigger, causing a temporary drop in heart rate and blood pressure, which can lead to fainting.
Blood levels of medications might rise in the elderly, sometimes to toxic levels. This is most likely due to:
pancreatic failure.
intentional overdose.
splenic dysfunction.
renal insufficiency.
renal insufficiency.
When explaining the need for a particular procedure to an elderly patient, you should:
use plain language and simple terms.
use the appropriate medical terminology.
realize that he or she will not understand you.
be complex so the patient fully understands.
use plain language and simple terms.
In contrast to younger patients, older patients are more prone to a decrease in blood pressure (BP) upon standing because:
any change in position causes blood to be shunted to the brain.
their red blood cells are destroyed at a faster than normal rate.
the body is less able to adapt the BP to rapid postural changes.
the aging process results in an overall increase in blood volume.
the body is less able to adapt the BP to rapid postural changes.
Common causes of syncope in older patients include all of the following, except:
blood volume loss.
venous pooling.
acute hypotension.
vasoconstriction.
vasoconstriction.
An older woman with osteoporosis presents with pain and deformity to her left hip after she shifted her weight onto her other foot. She has most likely experienced a(n):
compression fracture.
comminuted fracture.
idiopathic fracture.
pathologic fracture.
pathologic fracture.
Findings during the social assessment of an older patient include all of the following, except:
outdated medications.
daily activity assistance.
delays in obtaining meals.
interaction with others.
outdated medications.
When documenting a case of suspected elder abuse, it is most important for the EMT to:
document his or her perceptions of the event.
theorize as to why the patient was abused.
list the names of all of the suspected abusers.
avoid documenting any unsupported opinions.
avoid documenting any unsupported opinions.
Which of the following observations or statements represents the "E" in the GEMS diamond?
Elderly patients present atypically and deserve your respect.
A patient is assisted with his or her activities of daily living.
The patient's residence is cold due to a malfunctioning heater.
The patient's medications have not been filled in 2 months.
The patient's residence is cold due to a malfunctioning heater.
Which of the following is the most common mechanism of injury in older patients?
Falls
Suicide
Abuse
Burns
Falls
You receive a call for a sick person. When you arrive, you find the patient, a 75-year-old male, lying unresponsive in his bed. His respirations are slow and irregular, and his pulse is slow and weak. His daughter tells you that he fell the day before but refused to allow her to call 9-1-1. His past medical history is significant for hypothyroidism, deep vein thrombosis, heavy alcohol use, and liver cirrhosis. His medications include blood thinners and vitamins. You should be most suspicious that this patient is experiencing:
acute hyperglycemia.
a subdural hematoma.
diabetic ketoacidosis.
acute ischemic stroke.
a subdural hematoma.
the patient fell the day prior. Subdural hematomas are more common in older adults, even after a minor head injury, because brain shrinkage stretches and weakens bridging veins.
When assessing a 78-year-old female who complains of shortness of breath, the EMT should:
conclude that the patient is experiencing a heart attack.
determine the position in which the patient normally sleeps.
place the patient supine to see if the problem worsens.
give oxygen only if the patient has labored breathing.
determine the position in which the patient normally sleeps.
Heart failure is a common cause of dyspnea in the elderly
Orthopnea: A patient who needs to sleep propped up on pillows or in a chair to breathe comfortably is likely experiencing orthopnea, a classic sign of congestive heart failure (CHF).
Which of the following statements regarding suicide in the older patient is correct?
Older females have a higher rate of suicide than any other group.
Most suicidal patients readily seek care and do not deny the problem.
Depression and hopeless feelings are often not predisposing factors.
Older patients tend to use more lethal means than younger patients.
Older patients tend to use more lethal means than younger patients.
You are assessing a 70-year-old female who complains of intense thirst, frequent urination, and dizziness. She has a history of type 2 diabetes, heart disease, rheumatoid arthritis, and gout. Her blood glucose reads "high." She is conscious but confused. Her blood pressure is 92/52 mm Hg, her pulse rate is 130 beats/min and weak, and her respirations are 22 breaths/min and shallow. This patient's clinical presentation is most consistent with:
acute renal failure with associated hyperglycemia.
hyperglycemia with moderate dehydration.
diabetic ketoacidosis.
hyperosmolar hyperglycemic nonketotic syndrome.
hyperosmolar hyperglycemic nonketotic syndrome.
The patient is a 70-year-old female with type 2 diabetes presenting with polyuria, polydipsia, altered mental status, and severe dehydration (hypotension, tachycardia, weak pulse). These are hallmark signs of hyperosmolar hyperglycemic nonketotic syndrome (HHNS)
Which of the following statements regarding the aging process is correct?
Because he or she is younger and healthier, a 35-year-old person ages slower than a 75-year-old person.
The older a person gets, the slower the decline in the function of vital organs, such as the kidneys and liver.
The process of aging is gradual, and the rate at which a person loses functions does not increase with age.
Human growth and development peaks in the late 40s or early 50s, at which point the aging process sets in.
The process of aging is gradual, and the rate at which a person loses functions does not increase with age.
When assessing an older patient who has multiple bruises in various stages of healing, the EMT should do all of the following, except:
accuse a caregiver of physical abuse.
factually document all findings.
review the patient's activities of daily living.
ask the patient how the bruises occurred.
accuse a caregiver of physical abuse.
Upon arriving at the residence of an elderly female who apparently fainted, you find the patient lying supine on her living room floor. She is not moving, and her eyes are closed. A neighbor tells you that she found the patient this way but did not move her. When you gently tap the patient, she does not respond. You should:
direct your partner to manually stabilize her head while you quickly visualize her chest for signs of breathing.
begin assisting her ventilations with a bag-valve mask while your partner auscultates her lung sounds to ensure adequate positive-pressure ventilation.
open her airway with the head tilt-chin lift maneuver, insert an oral or nasal airway, and assess her blood glucose level to rule out hypoglycemia.
suction her airway, apply a cervical collar, administer high-flow oxygen via a nonrebreathing mask, and perform a rapid assessment.
direct your partner to manually stabilize her head while you quickly visualize her chest for signs of breathing.
Which of the following patients is at highest risk for a pulmonary embolism?
71-year-old male with recent surgery to a lower extremity
59-year-old male who is recovering from pneumonia
66-year-old active female with a history of hypertension
78-year-old female who takes blood-thinning medications
71-year-old male with recent surgery to a lower extremity
Recent surgery, especially orthopedic surgery on a lower limb, is one of the most significant risk factors for developing a deep vein thrombosis (DVT), which is the most common cause of a pulmonary embolism (PE). The risk is highest in the first few months after the surgery.
Venous stasis (slowed blood flow) is a key factor in clot formation. After surgery, especially involving the lower extremities, a patient's immobility or prolonged bed rest leads to this venous stasis.