anatomy of lungs and pleura
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
Cavities
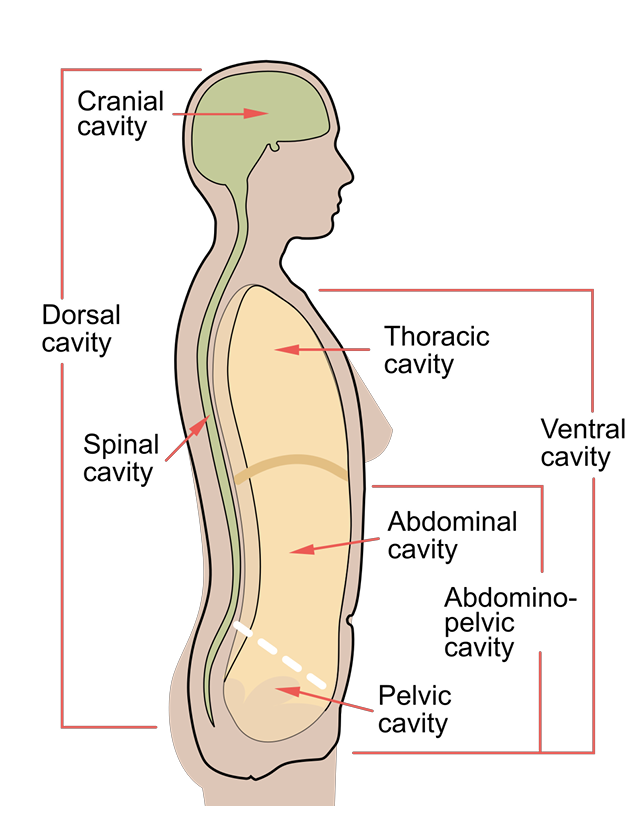
Thoracic cavity sub divisions
-Medially= mediastinum
-Laterally= pleural cavities
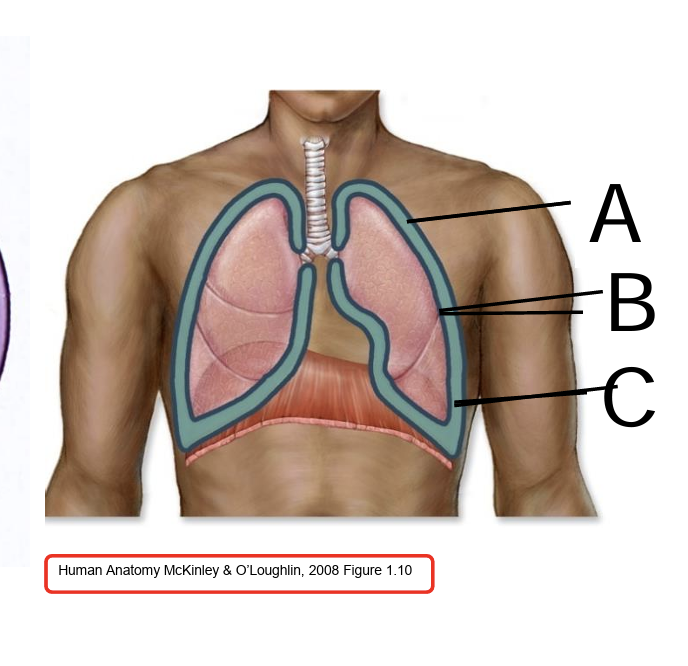
a= parietal pleura
b= visceral pleura
c= pleural cavity
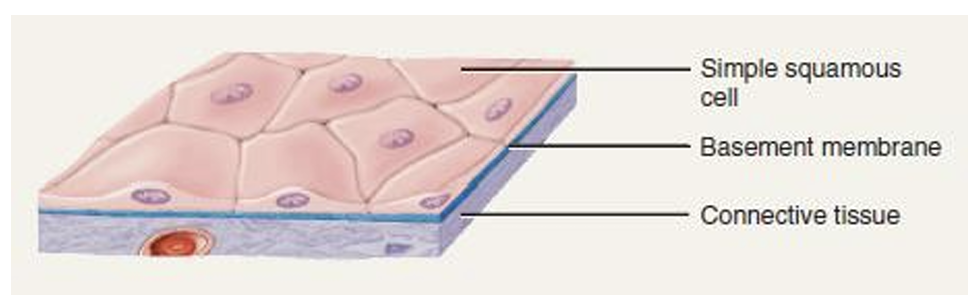
Histology of Pleura
Simple squamous epithelium
Subserous fascia (loose areolar CT)
which part of the pleura is pain sensitive
parietal pleura
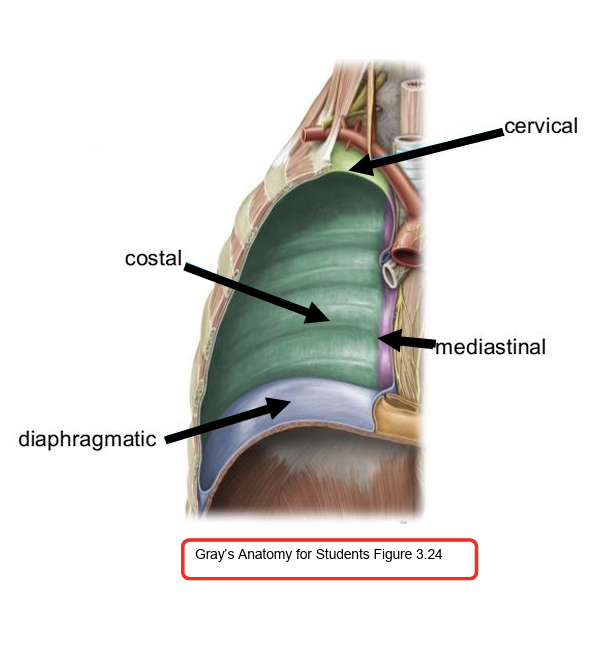
parietal pleura divisions
Cervical: Covers the apex of the lung in the neck region
Costal: Lines ribs and intercostal surfaces
Diaphragmatic: Lines thoracic surface of diaphragm
Mediastinal: Lines the mediastinum
phrenic nerve innervates
Mediastinal and central part of diaphragmatic pleura
Intercostal nerves innervates
Costal and peripheral part of diaphragmatic pleura
what is pleurisy
a condition where the pleura—the thin, double-layered membrane that surrounds the lungs and lines the chest cavity—becomes inflamed. This inflammation causes sharp chest pain, especially when breathing, coughing, or sneezing.
ignore
Costal pleura: Local dermatomal pain through intercostal nerves
Mediastinal pleura: Referred pain through phrenic nerve (C3-5)
-Diaphragmatic pleura (central):
Costal pleura pain
Innervation: Intercostal nerves
Pain pattern: Sharp, localized dermatomal pain along the chest wall
Mediastinal pleura pain
Innervation: Phrenic nerve (C3–C5)
Pain pattern: Referred to shoulder and neck
central Diaphragmatic pleura
Phrenic nerve (C3–C5) → referred pain to the shoulder and neck
peripheral diaphragmatic pain
Intercostal nerves → localized pain
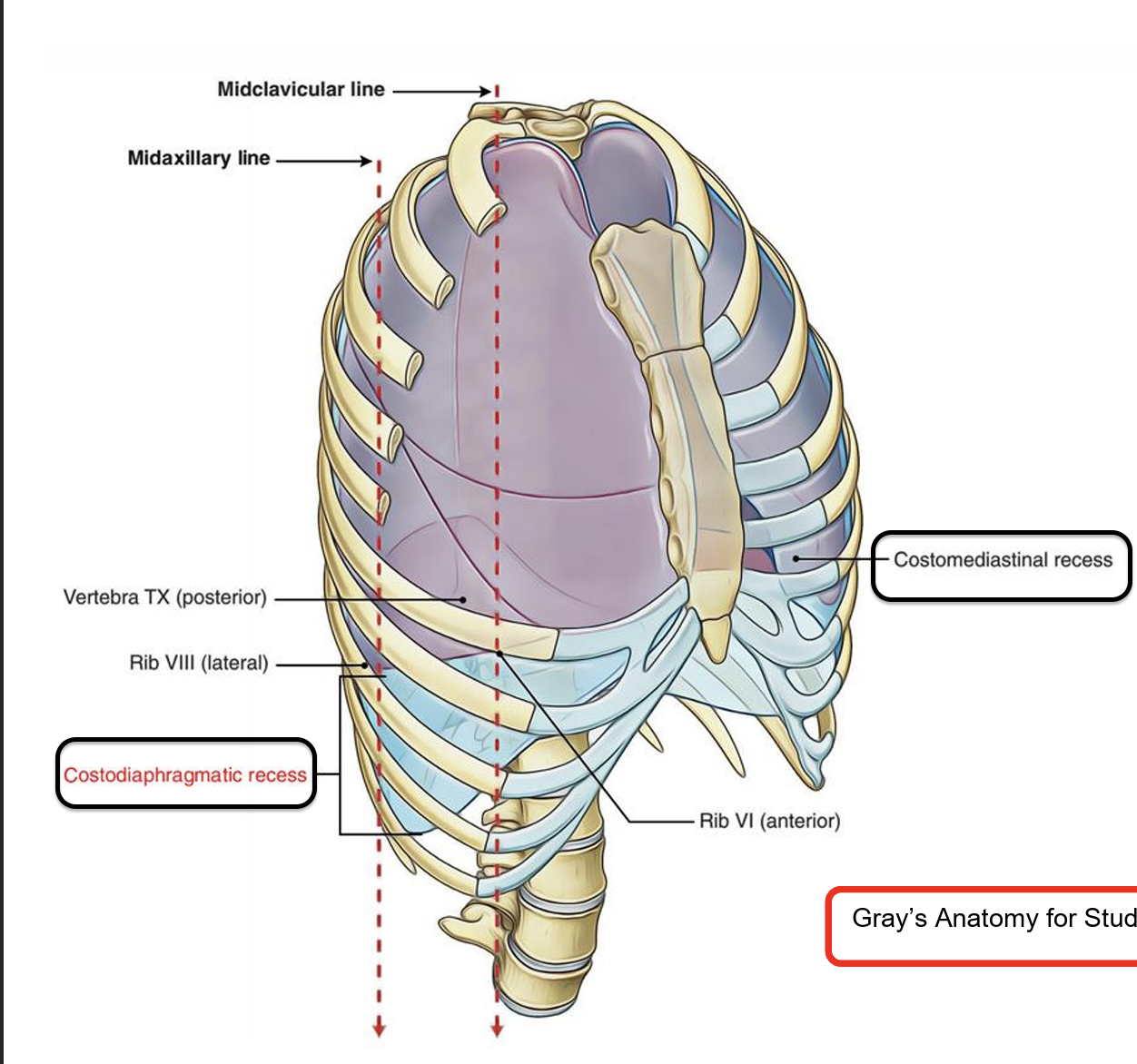
what are Pleural Recesses
Potential spaces for lung expansion during forced inspiration and fluid collection and spaces from which fluid can be aspirated
what are the 2 pleural recesses
Costodiaphragmatic recesses: Found between costal and diaphragmatic pleura
Costomediastinal recess: Located between costal and mediastinal pleura (large on the left side)

pleural effusion
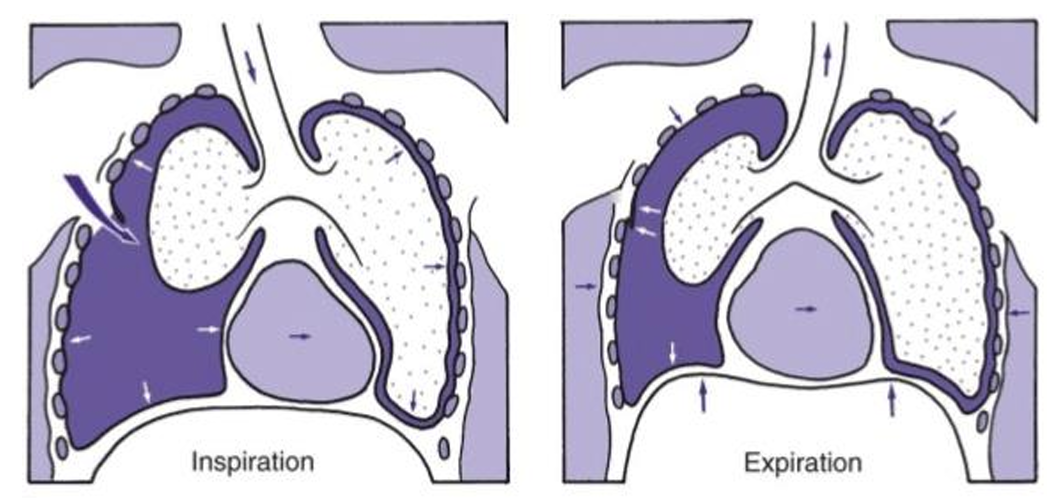
pneumothorax
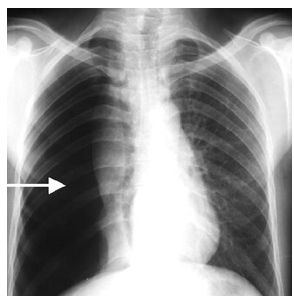
Pleural Effusion
A pleural effusion is the accumulation of excess fluid in the pleural space, the area between the visceral and parietal pleura.
pneumothorax
A pneumothorax is the presence of air in the pleural space, causing partial or complete lung collapse.
tension pneumothorax
A tension pneumothorax occurs when air enters the pleural space during inspiration but cannot escape during expiration, leading to progressive pressure build-up.
This pressure compresses the lung, shifts the mediastinum, and obstructs venous return to the heart → can lead to cardiac arrest if untreated.
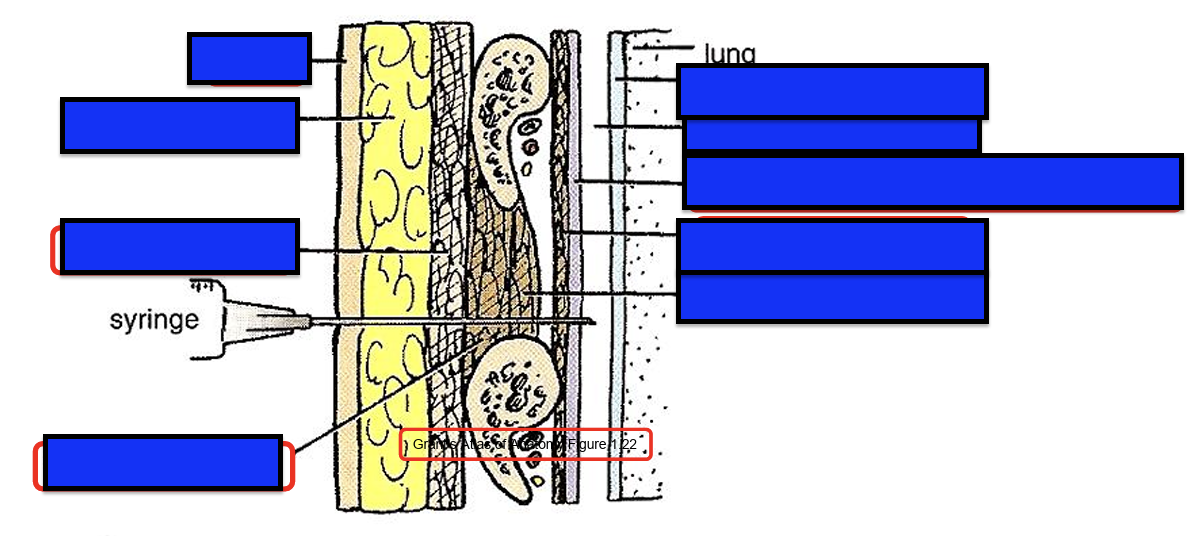
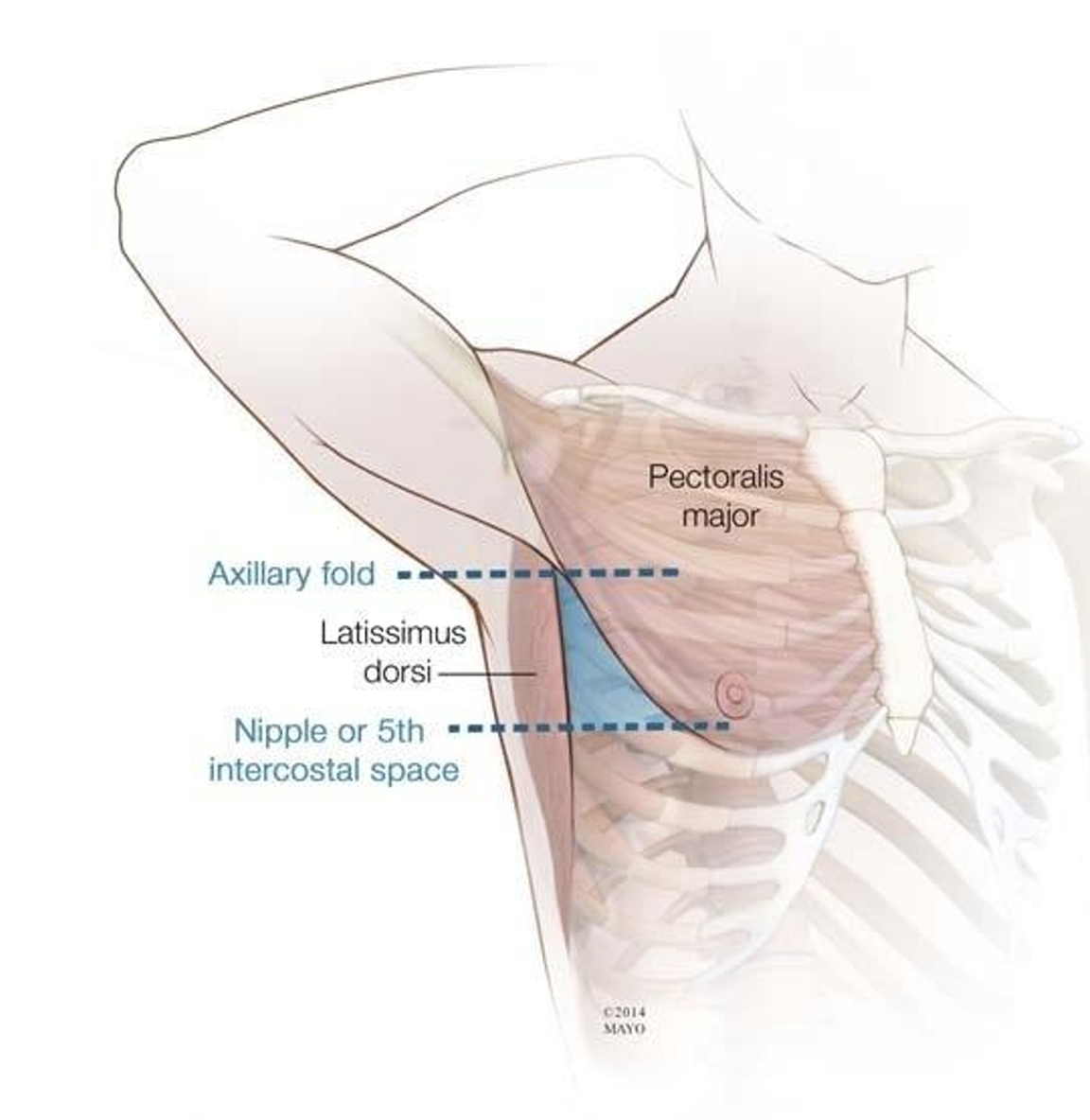
Thoracentesis
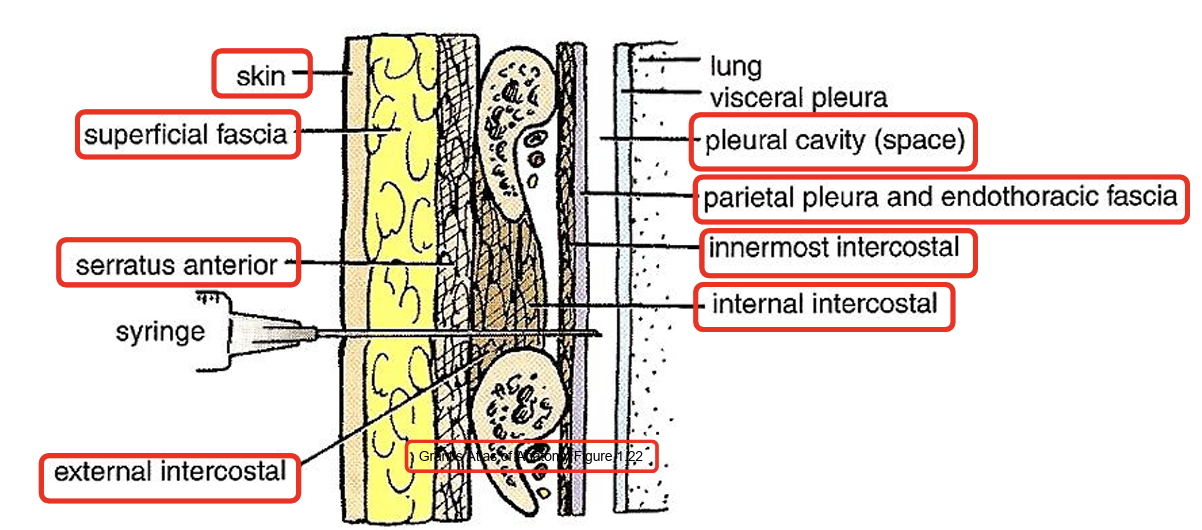
Safe triangle for needle in lung
Anterior | Lateral border of the pectoralis major |
Posterior | Lateral border of the latissimus dorsi |
Inferior | Line at the level of the nipple (5th intercostal space) |
Superior | Base of the axilla (apex of triangle) |
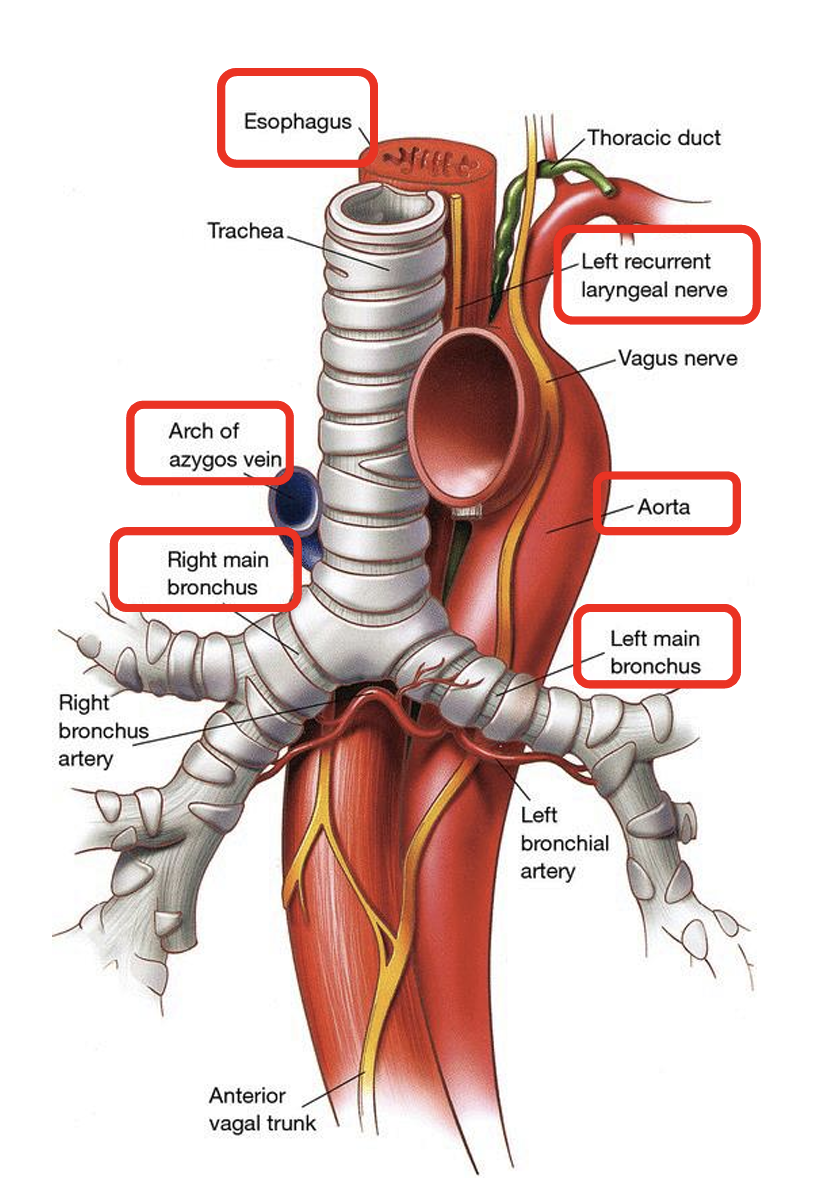
trachea position
Fibrocartilaginous tube from C6 to T4/T5
In deep inspiration, reaches the level of T6
Anterolateral of trachea
U-shaped bars of hyaline cartilage
posterior part of trachea
Smooth muscle (trachealis)
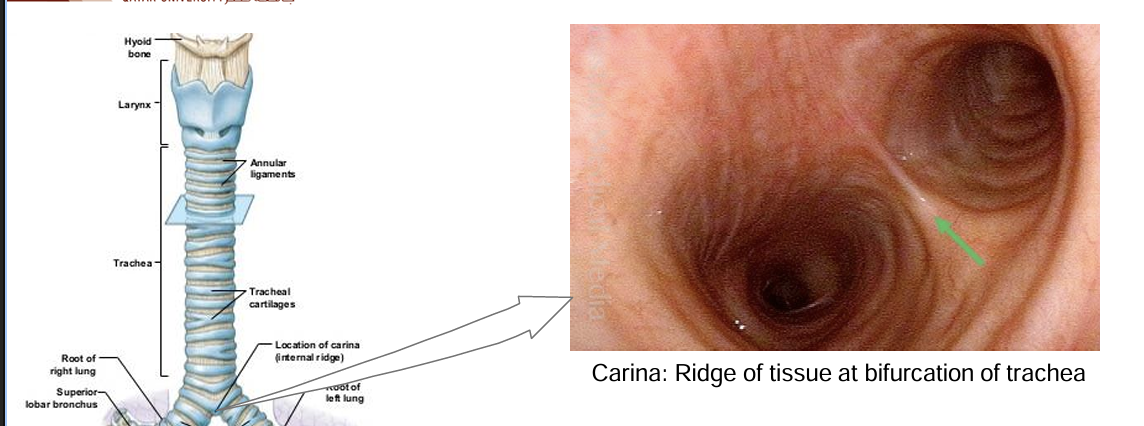
Carina
Right vs left primary bronchi
Right bronchus: Wider, shorter and more vertical
Left bronchus: Narrower, longer and more horizontal
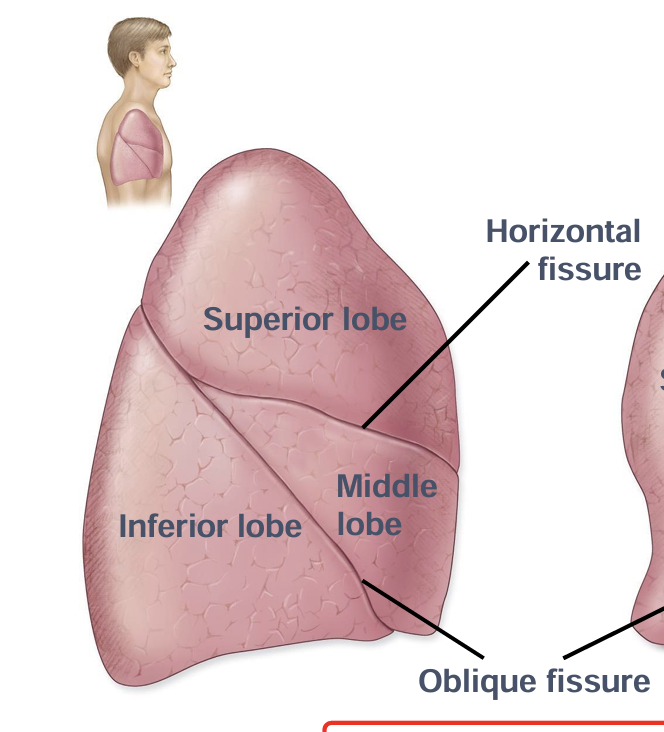
Secondary bronchi right vs left
Right: Superior, middle and inferior
Left: Superior and inferior
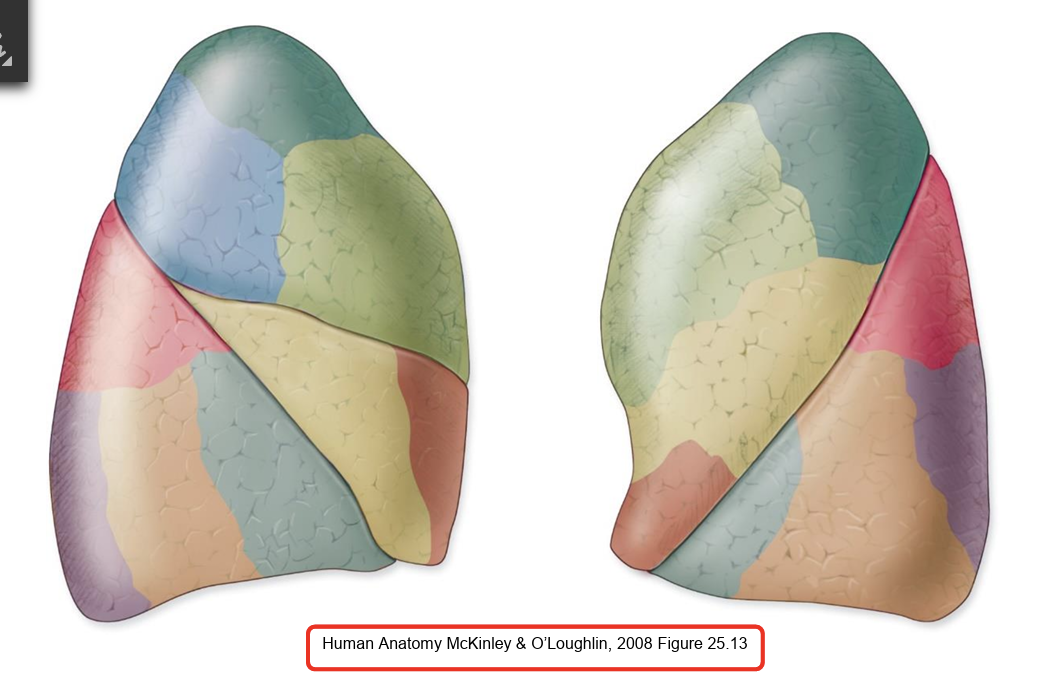
right lung lobes and fissures
3 lobes
2 fissures: oblique and horizontal
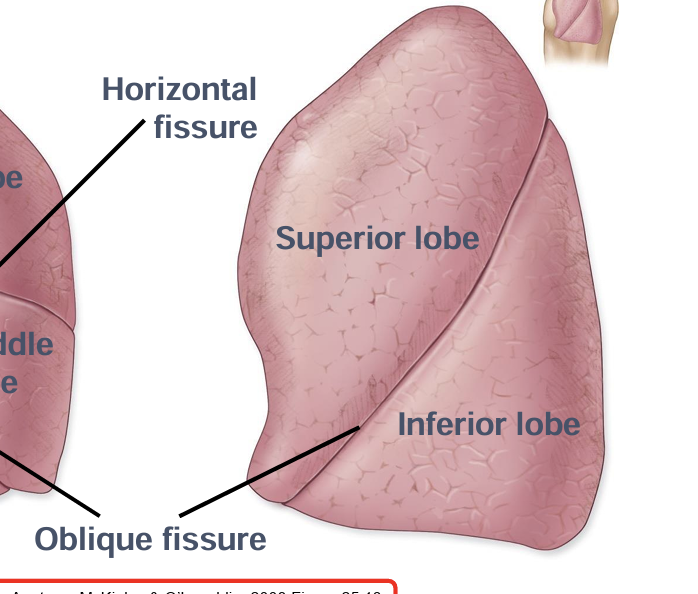
left lung lobes and fissures
2 lobes
1 oblique fissure
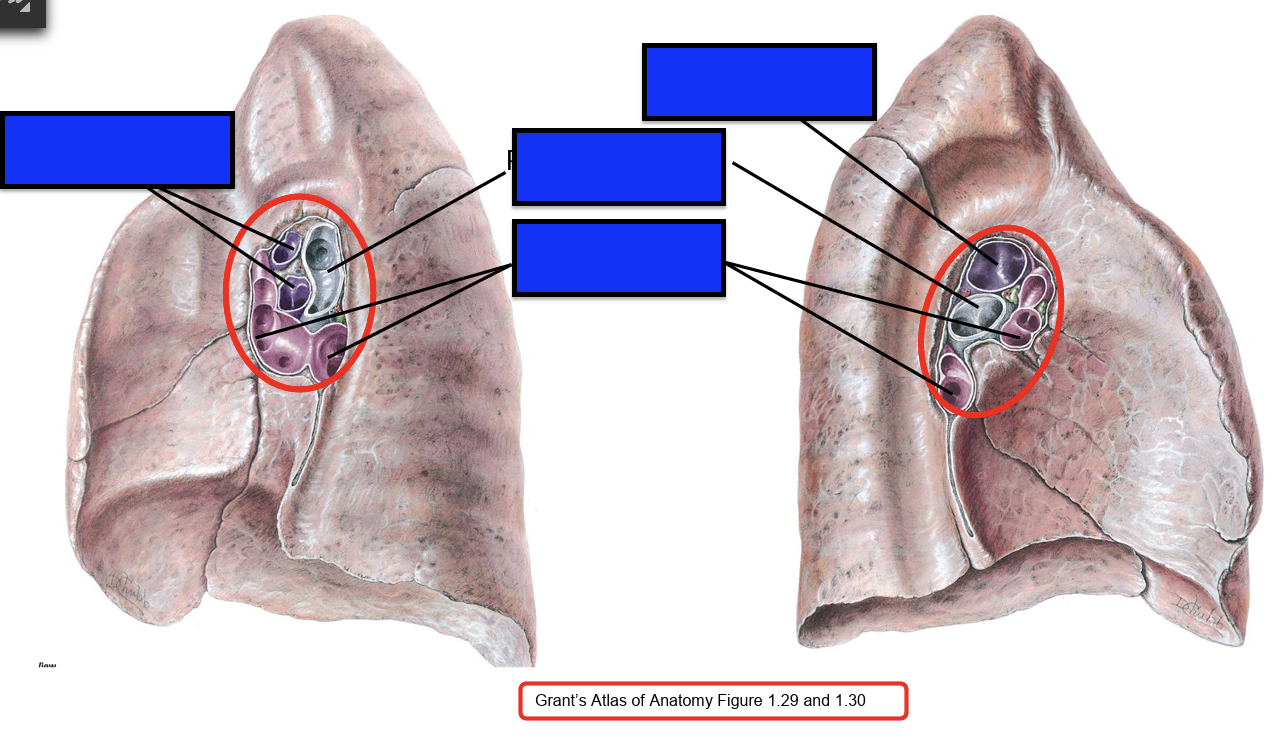
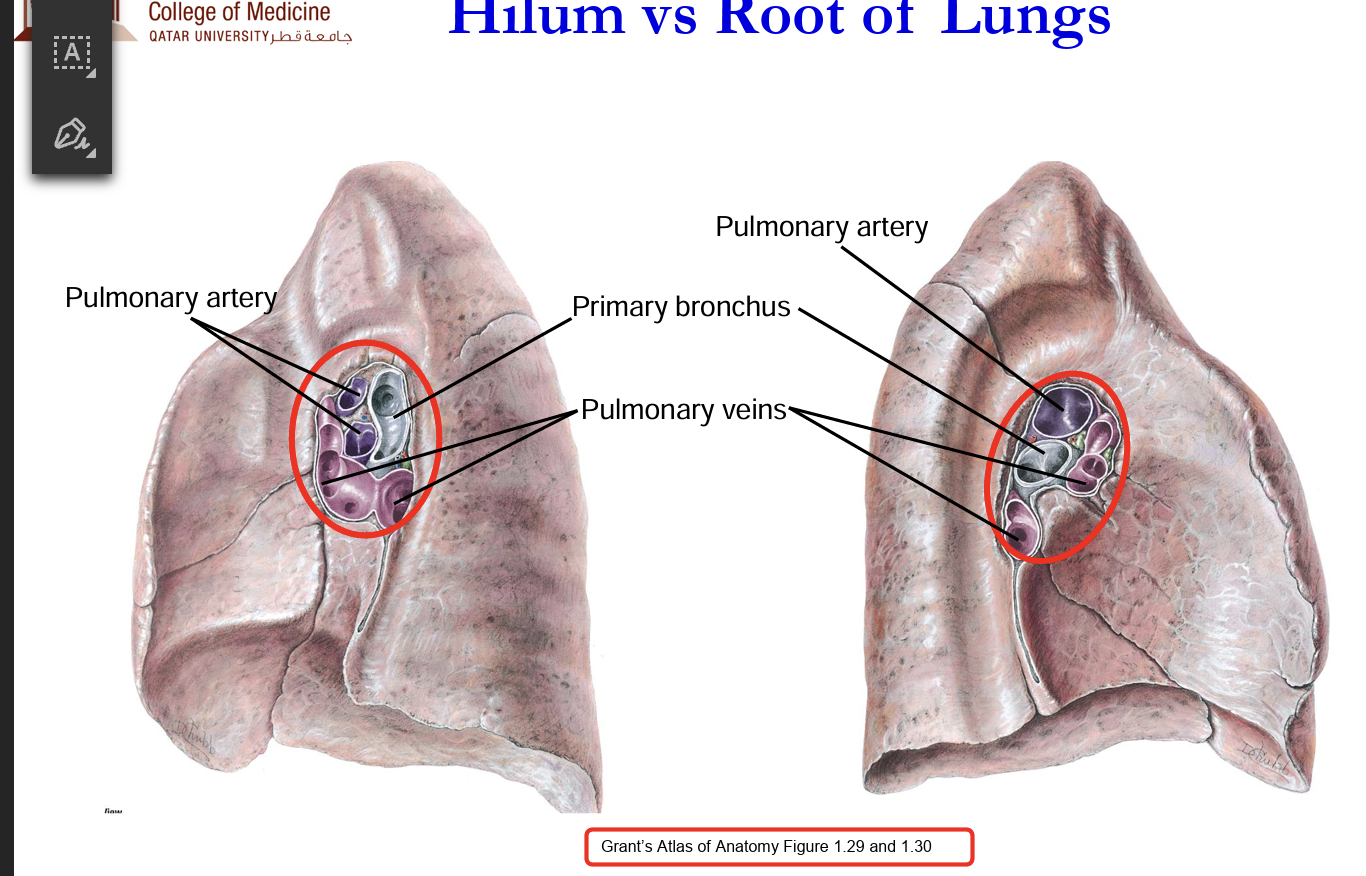
hilum and root of lung structures
horizontal fissure location
Follows curvature of 4th rib (only in right lung)
oblique fissure location
From 5th intercostal space at the midclavicular line (MCL) → curves along the 6th rib anteriorly toward the midaxillary line and posteriorly
Right Lung lobe location
Superior lobe: Located above the 4th rib, anteriorly
Middle lobe: Lies between the 4th and 6th ribs, anteriorly
Inferior lobe: Lies below the 6th rib, posteriorly
Posteriorly, both lungs are mostly inferior lobes—important when auscultating for basal pneumonia or effusions.
Bronchopulmonary Segment
Segment of the lung supplied by a tertiary bronchus
Respiratory bronchioles:
Lead to individual pulmonary lobule
Branch as alveolar ducts to alveolar sacs, alveoli
Branches of pulmonary arteries and pulmonary veins form capillary bedsaround alveoli for gas exchange
Elastic fibressurround alveoli, assist in expiration
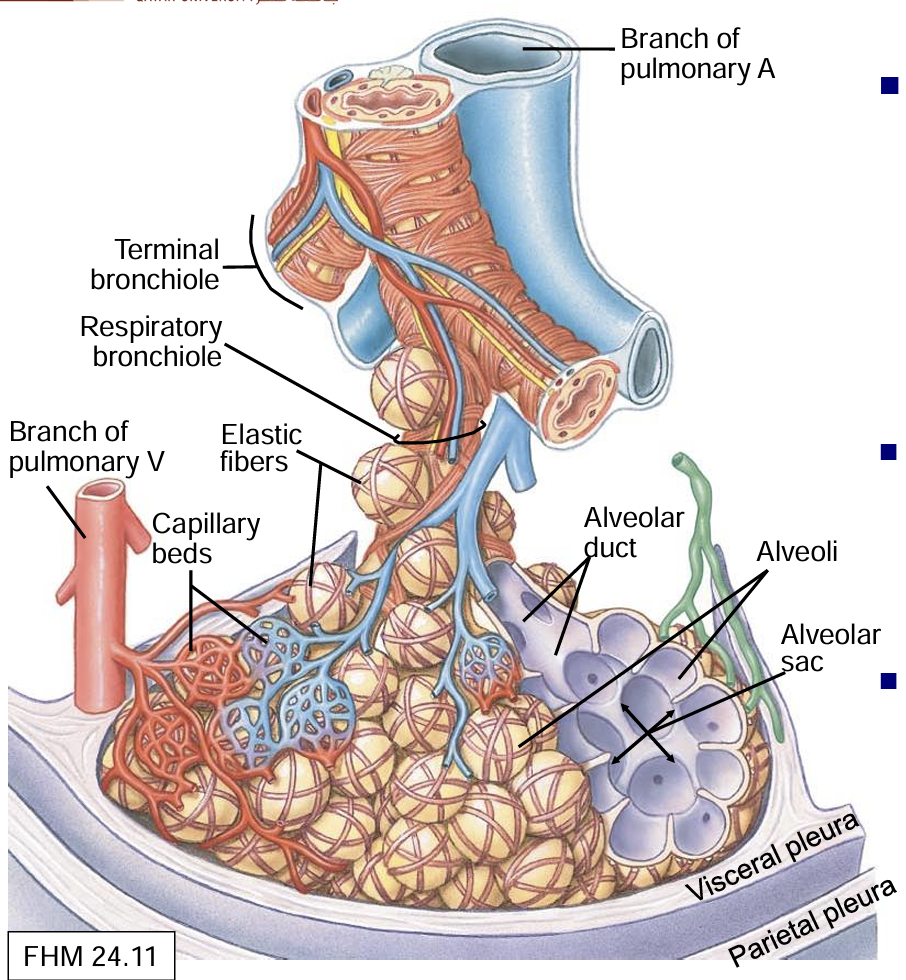
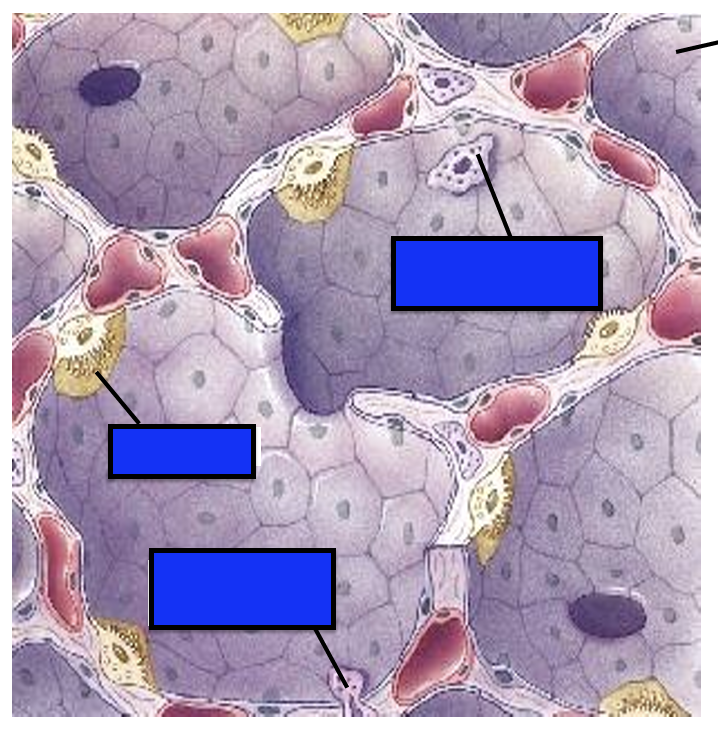
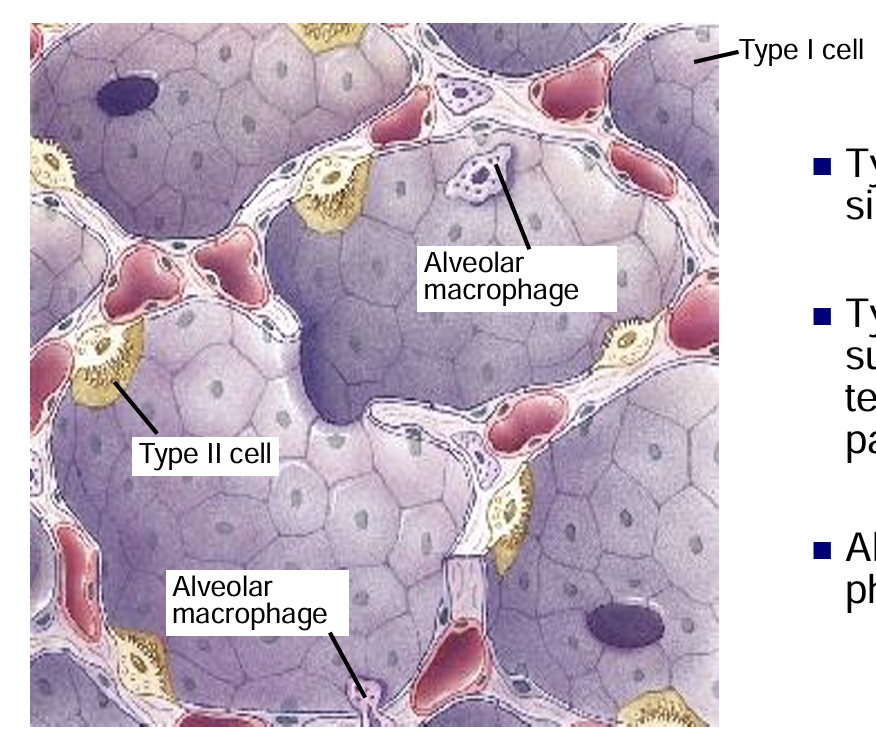
Type I pneumocytes
form a simple squamous epithelium
Type II pneumocytes
secrete surfactant decrease surface tension, maintains alveolar patency
stem cells for regeneration
Alveolar macrophages
phagocytose pathogens
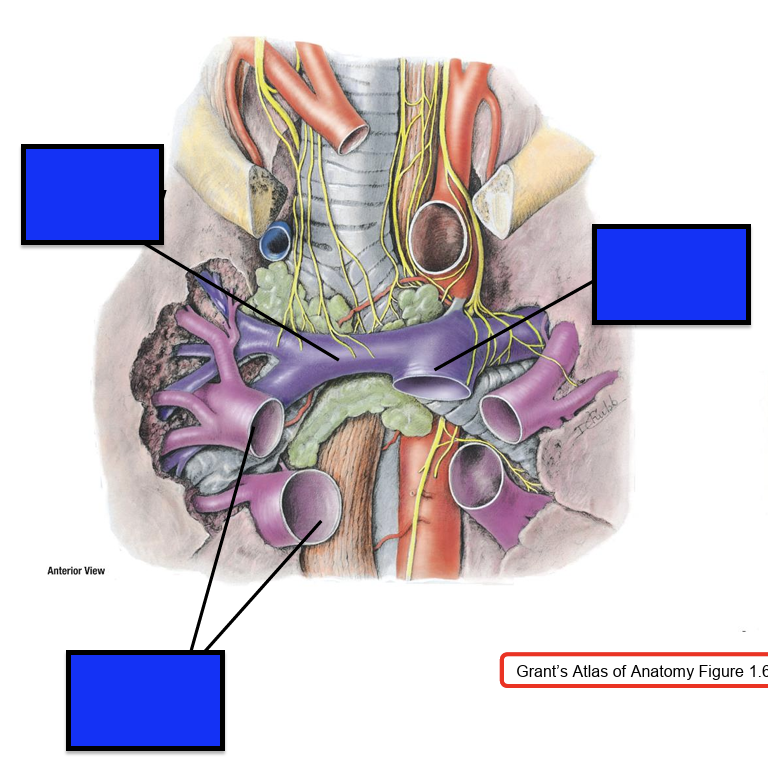
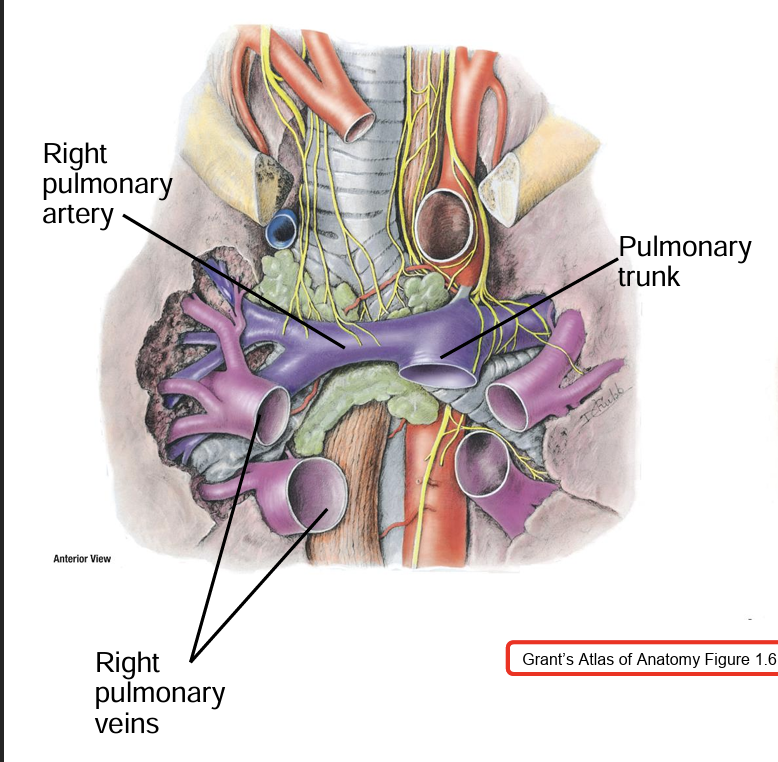
Pulmonary Circulation
Pulmonary trunk divides into R and L pulmonary arteries, carry deoxygenated blood to alveoli Arteriole
Pulmonary veins (four) drain oxygenated blood from alveoli
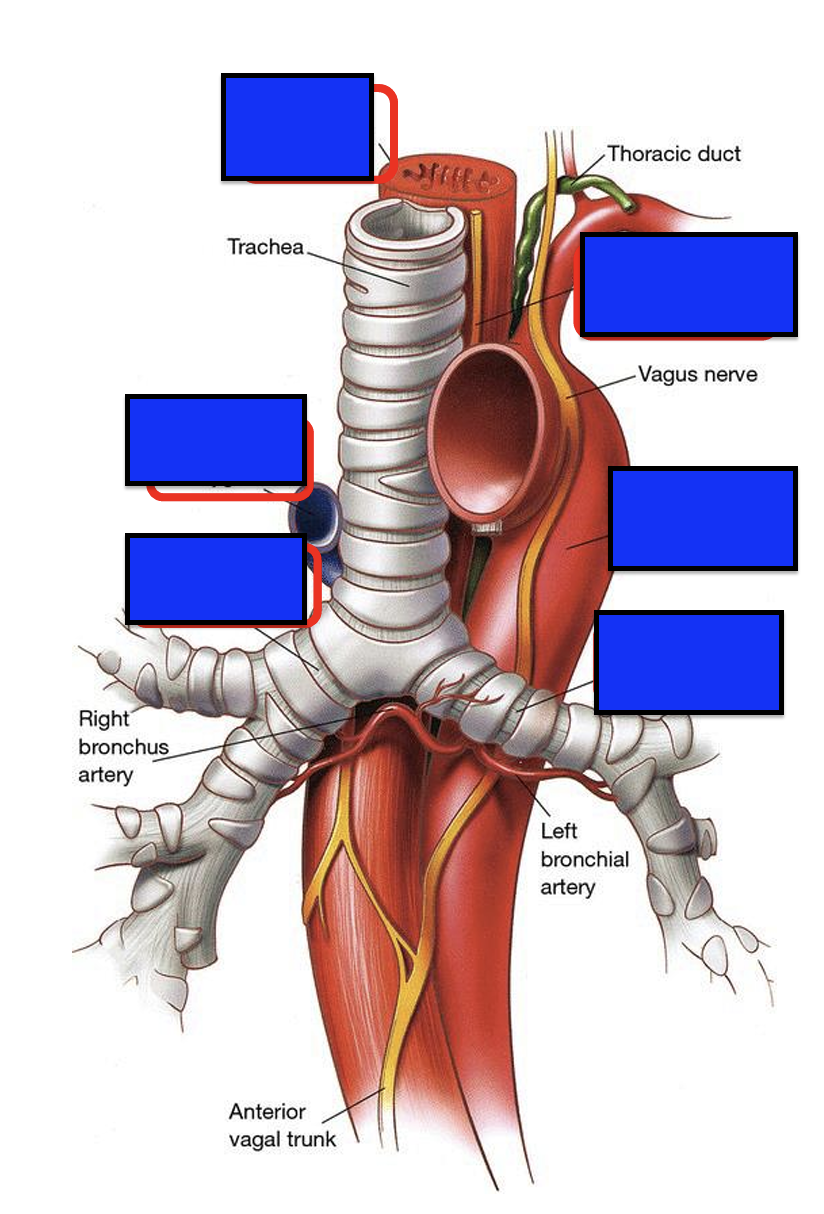
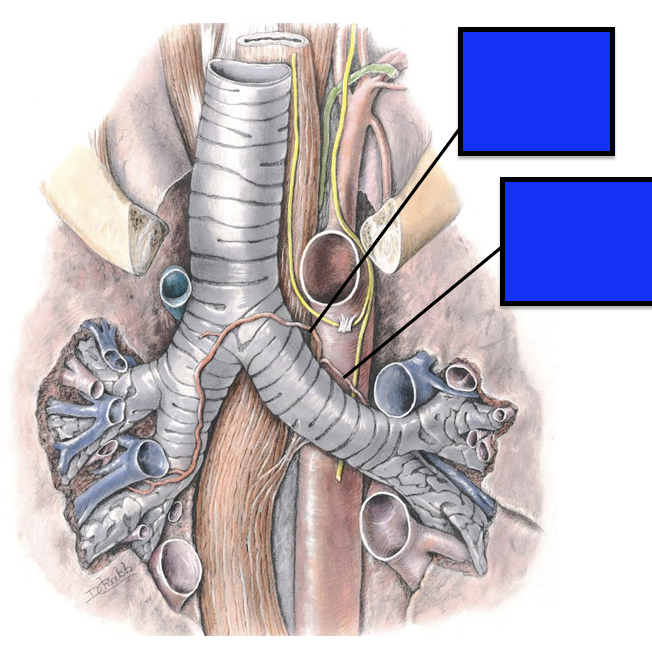
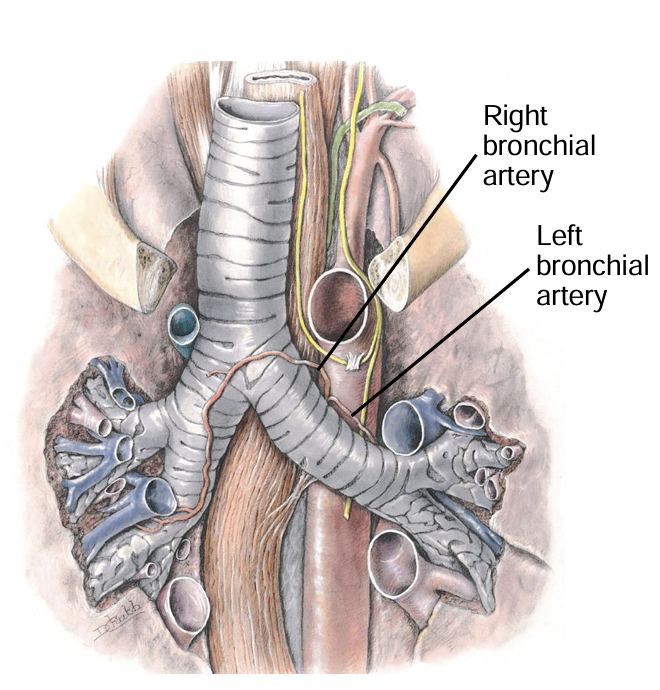
Bronchial arteries
branches of thoracic aorta supply lung parenchyma, pleura and alveoli
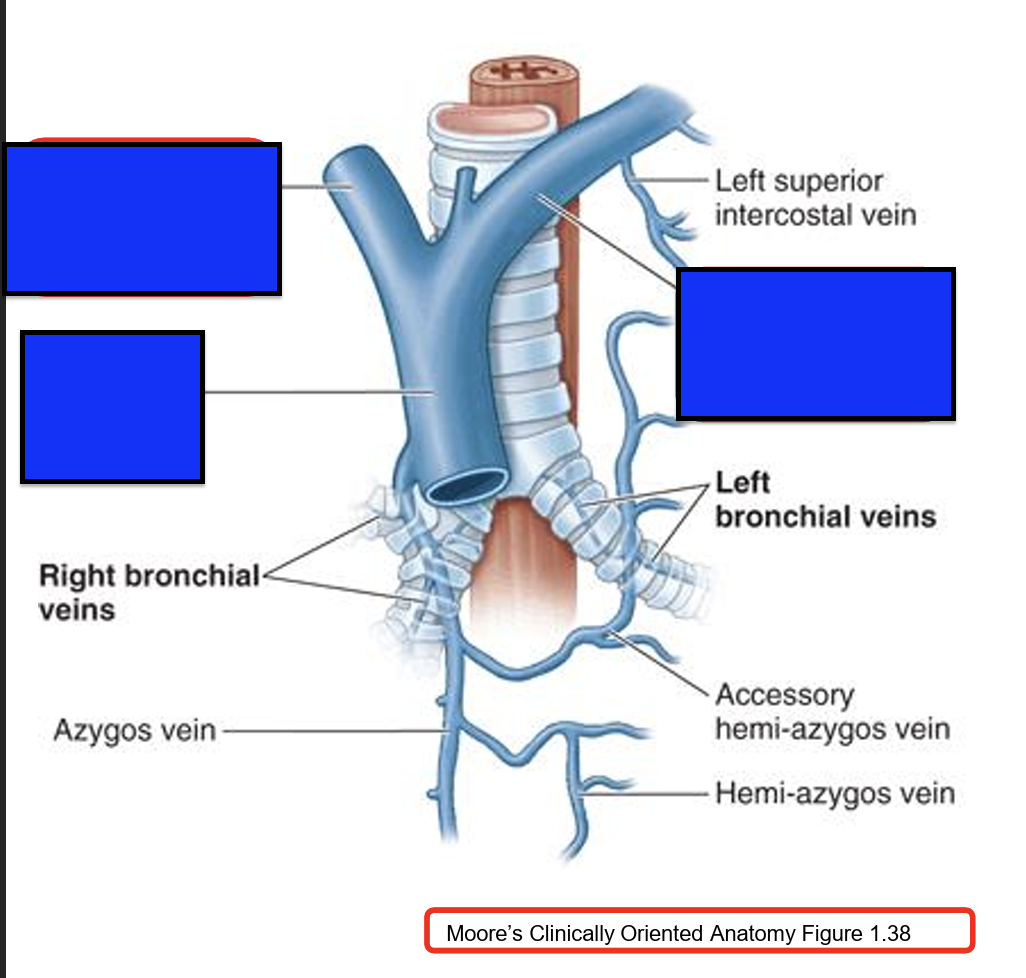
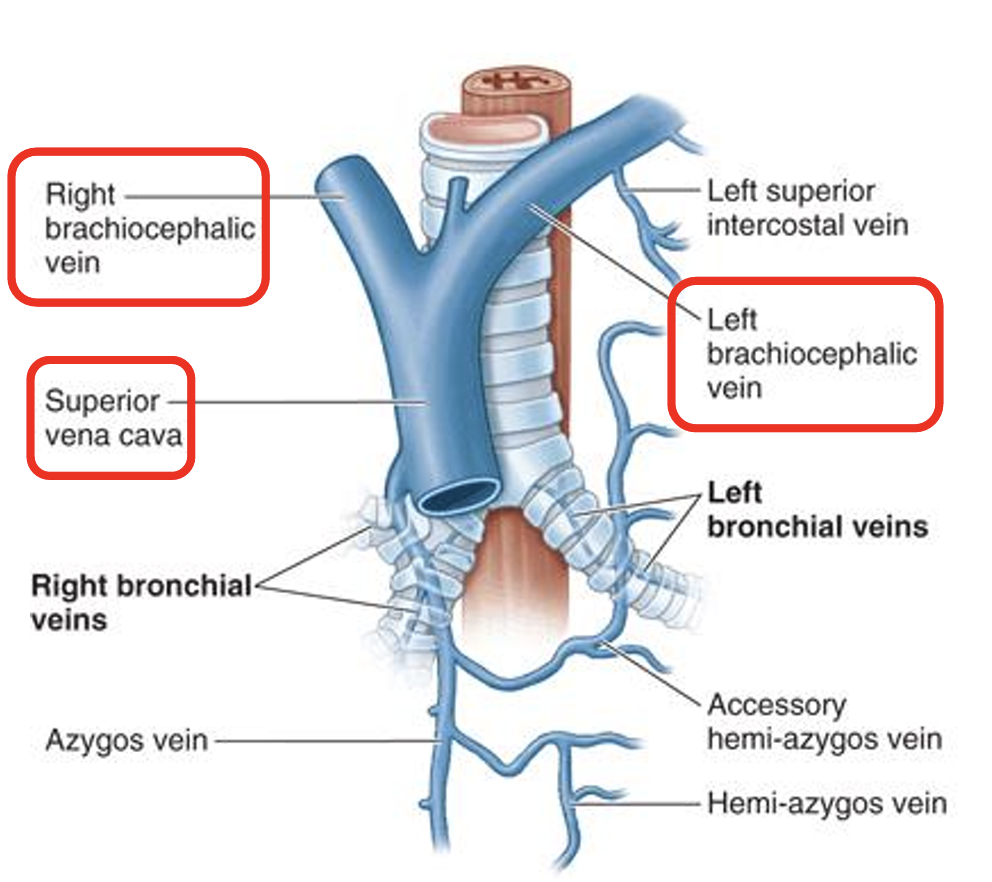
bronchial veins
Drain into the azygous system
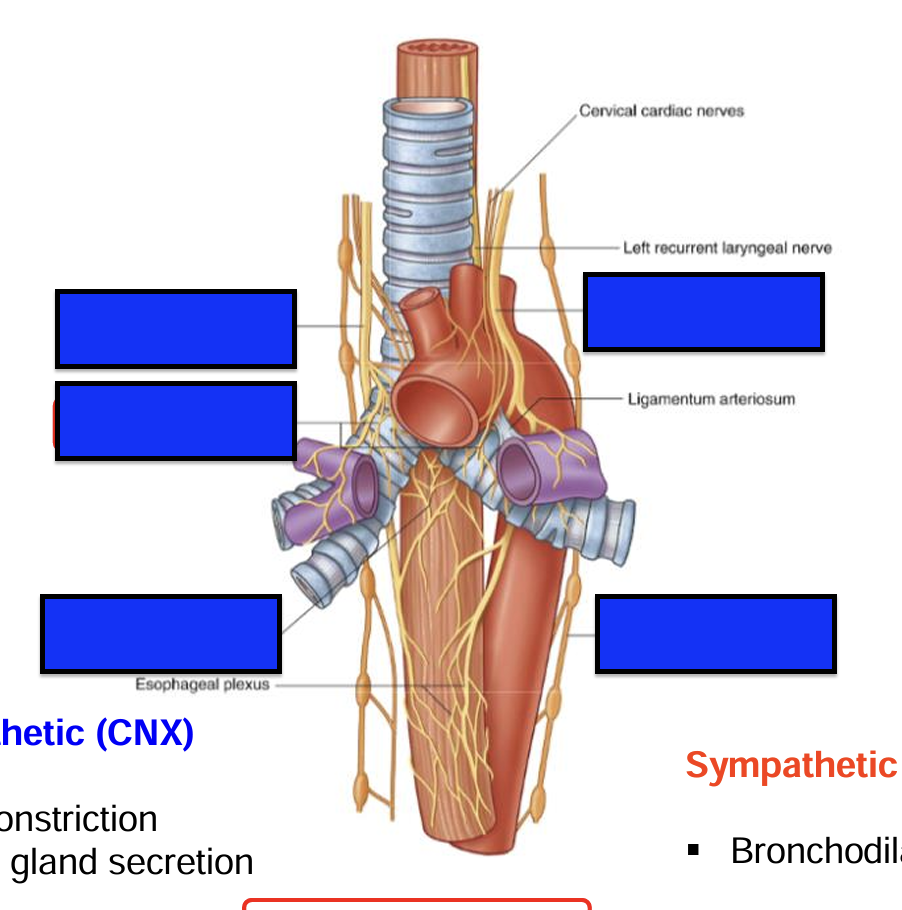
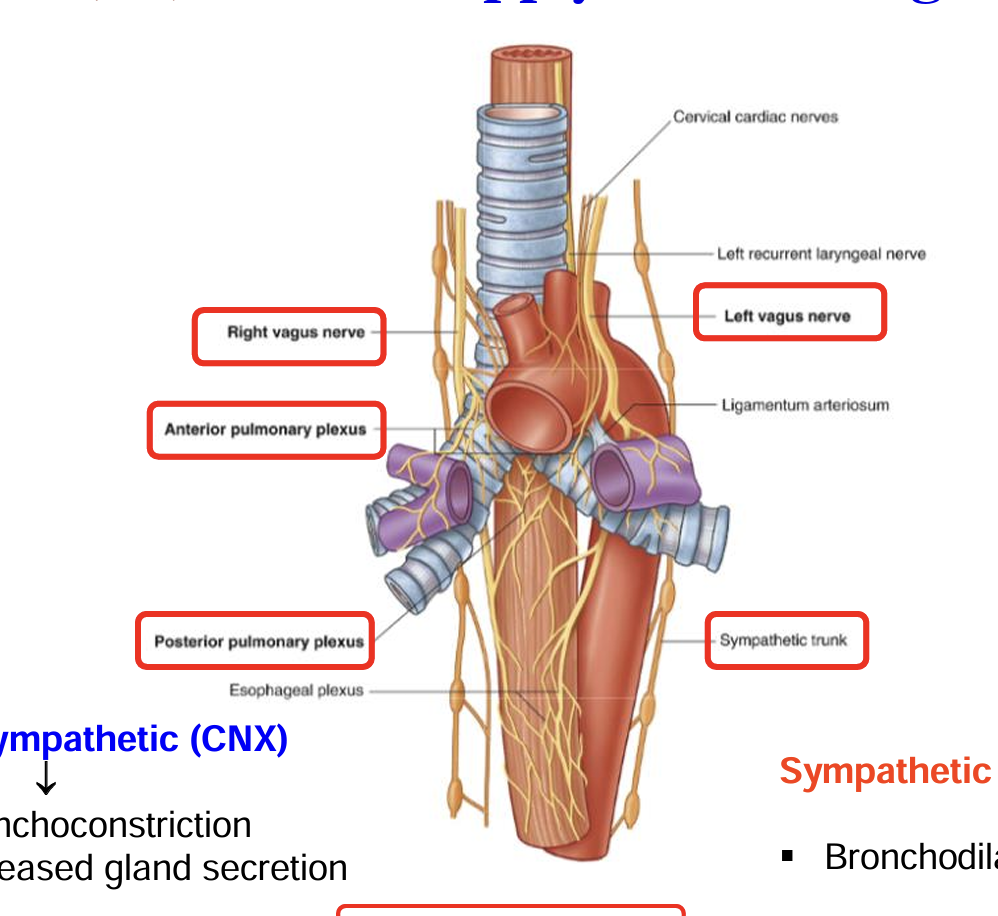
Parasympathetic Supply of lungs
Vagus nerve (CN X)
Parasympathetic action
Bronchoconstriction 🫁
Vasodilation (pulmonary vessels)
Increased mucus secretion
Sympathetic Supply
Sympathetic trunk (T1–T5 spinal levels)
sympathetic effects
Bronchodilation 🫁
Vasoconstriction
Decreased glandular secretion
Pulmonary Plexus
The pulmonary plexus is a network of nerves that provides autonomic (involuntary) innervation to the lungs and bronchi. It’s formed by sympathetic and parasympathetic fibers and is located around the main bronchi at the hilum of the lungs.
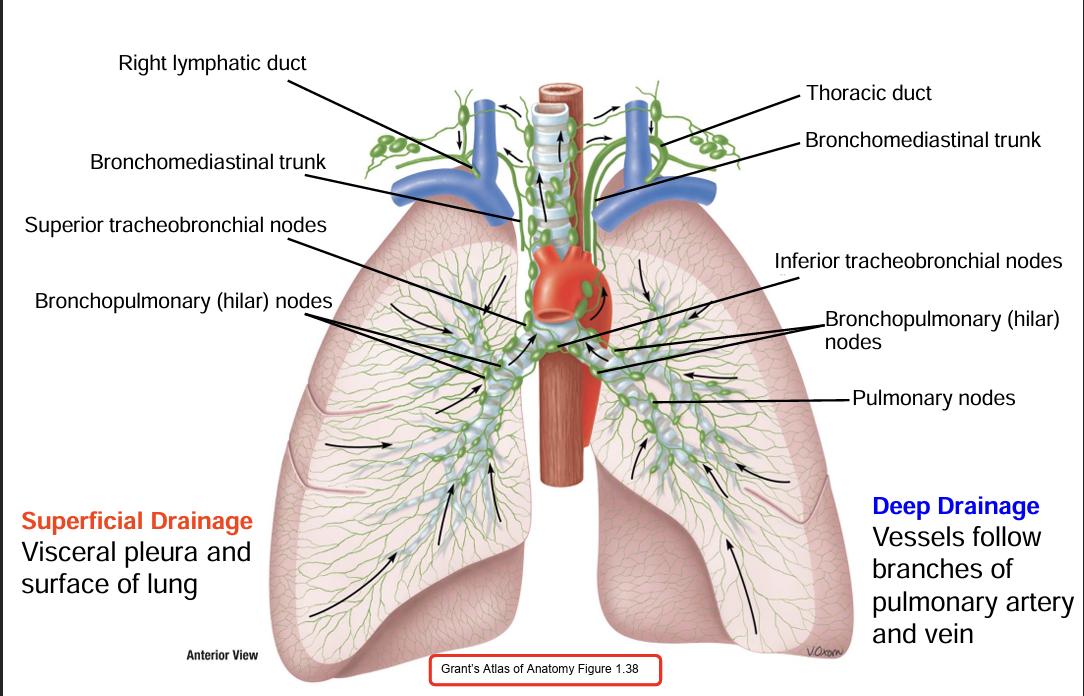
lymph drainage of lungs
Pulmonary Lymph Nodes —> Hilar Lymph Nodes —> Mediastinal Lymph Nodes —> right lymphatic duct or thoracic duct (left lung) —> right and left subclavian
-subcarinal lymph nodes that drain from both lungs
boundaries of inferior mediastinum
superior: sternal angle (T5 vertebrae)
inferior: diaphragm
anterior: sternum body
posterior: T5- T12
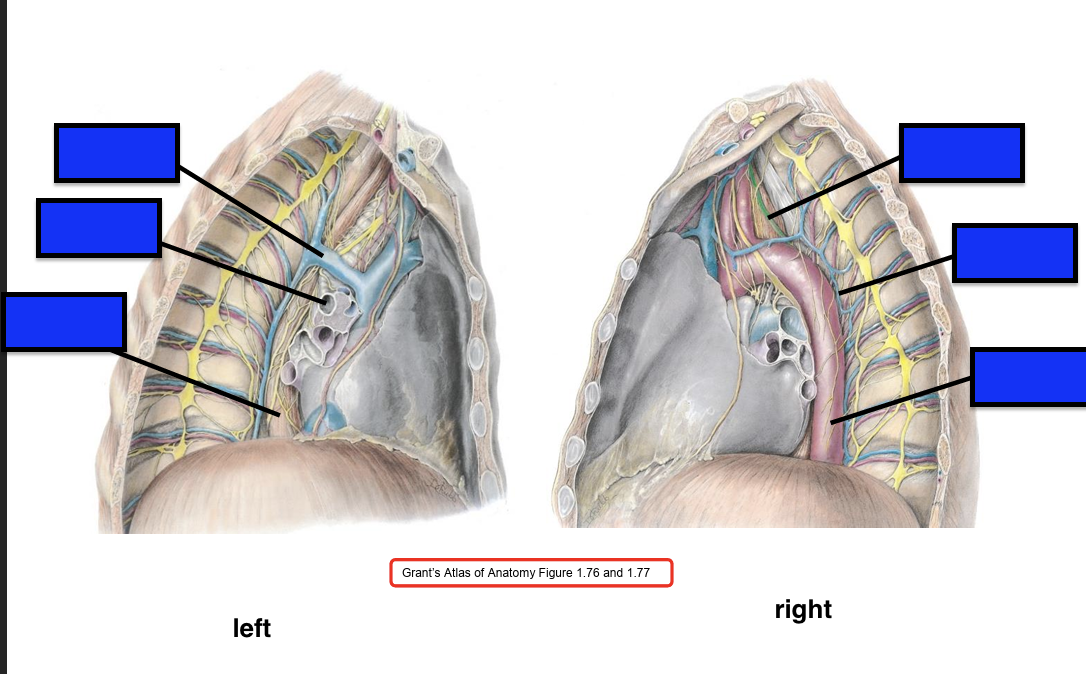
switch left and right
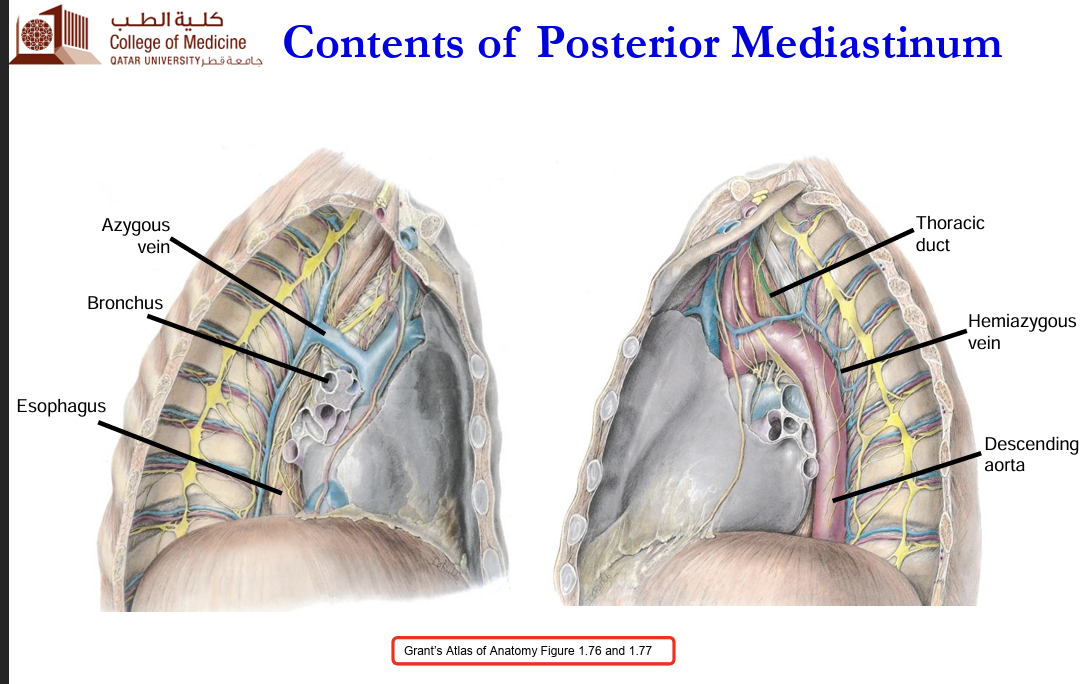
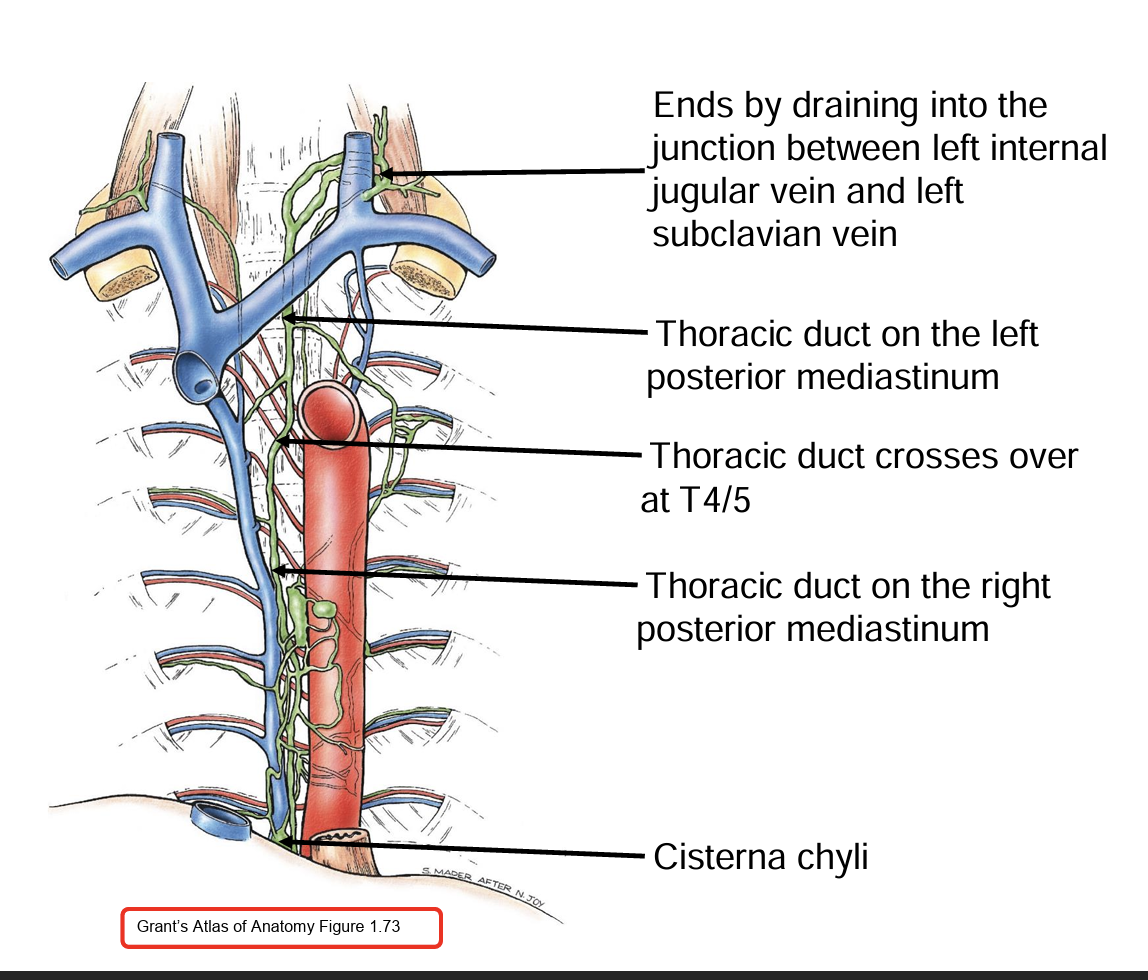
Course of the Thoracic Duct
Origin: The thoracic duct begins at the cisterna chyli (a dilated sac) at the level of L1-L2 in the abdomen.
Abdominal Course: It ascends along the right side of the aorta in the abdomen, passing through the diaphragm at the aortic hiatus at T12.
Thoracic Course: In the thoracic cavity, it initially runs along the right side of the vertebral column, then crosses to the left side around T5-T6.
Termination: The duct empties into the left venous angle, where the left internal jugular vein meets the left subclavian vein.