Functional Outcome Measures
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
purpose of outcome measures
- objectively identify and measure a patient's deficits
- objectively measure progress over time
- write meaningful goals
challenges of outcome measures
- reimbursement requirements
- time
- productivity requirements
- documentation to support skilled care
- increased patient participation in their own health goals
benefits of outcome measures
- assist in determining patient's specific impairment
- patient education
- track functional progress objectively (tracks changes, motivates patients)
- common language between health care providers
- evidence based practice (valid, reliable)
APTA EDGE Taskforce recommendations
stroke, TBI, SCI, MS, Parkinson's, Vestibular
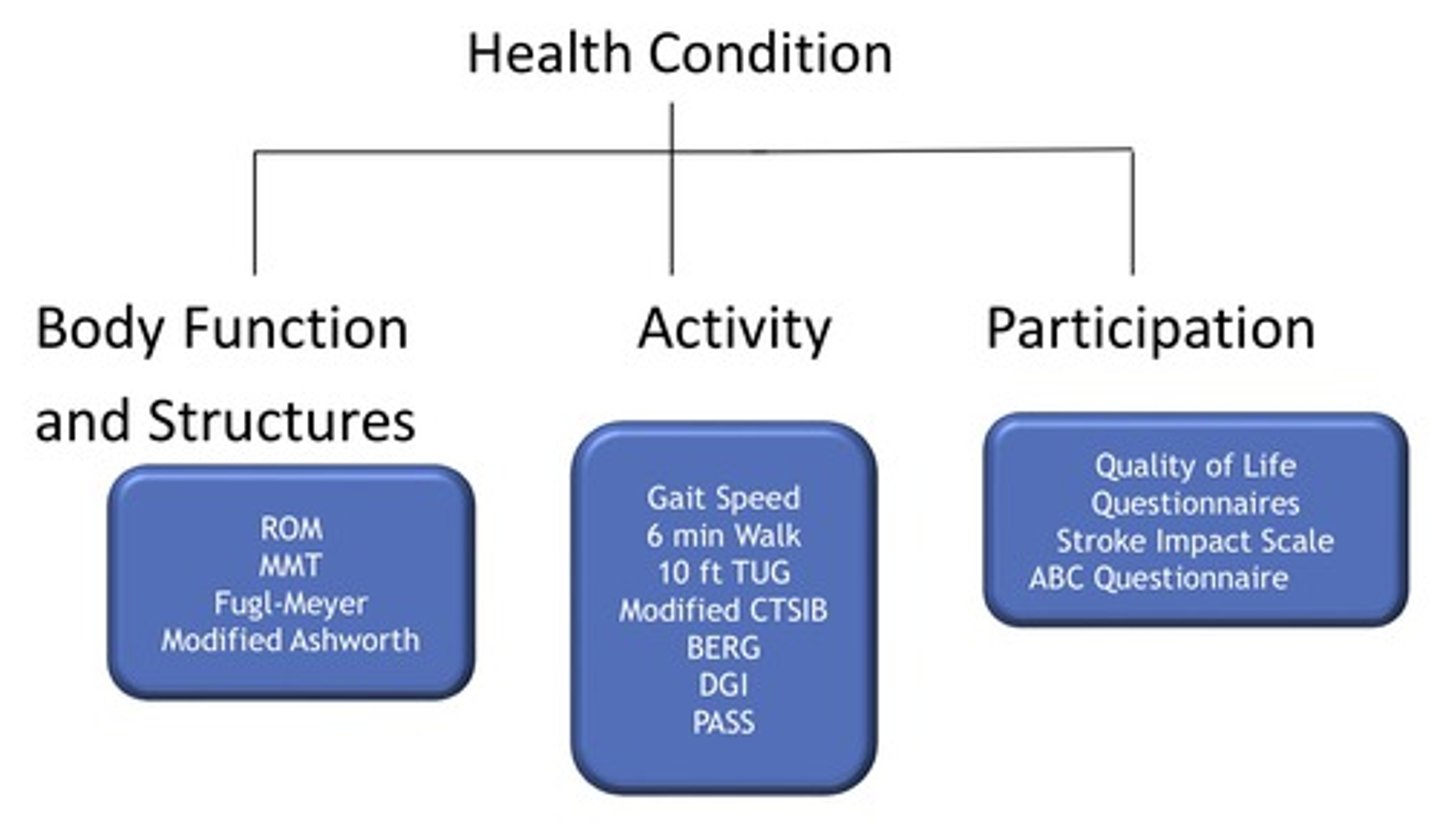
ICF WHO model
factors to consider when selecting an outcome measure
- purpose of measure (discriminative vs predictive vs evaluative)
- referral diagnosis
- clinic factors
- acuity level (acute, IPR, OP)
- observation (AD use, posture, movement quality and speed)
- patient's history
discriminative outcome measure
differentiates between patient groups and identifies meaningful differences in patients' abilities (no criteria reference)
predictive outcome measure
used to predict outcome (prognostic) or diagnosis (criteria referenced)
evaluative outcome measure
measures longitudinal change in an individual
minimal detectable change (MDC)
- smallest amount of change outside of error that reflects true change by a patient between two points in time (acuity, diagnosis specific)
- may not be meaningful
minimally clinically important difference (MCID)
- smallest amount of change in an outcome that a patient would perceive as clinically meaningful (acuity, diagnosis specific)
- meaningful change
cut-off scores
scores on an assessment that research has shown to have predictive value (fall risk, dysfunction)
normative data
what is usual in a defined population at a specific point or period of time (age, gender)
factors to consider when interpreting outcome measures
- scoring interpretation
- psychometric factors
reliability
consistency of the measure; repeatability
validity
is it testing what it is supposed to test; accuracy
specificity
how well a test can identify a true negative; rule in
sensitivity
how well a test can identify a true positive; rule out
ANPT core measures for all adults with neurologic disorders
- 6MWT
- 10 Meter Walk Test
- Berg Balance Scale
- Functional Gait Assessment
- Activities-Specific Balance Confidence Scale
- 5 Time Sit to Stand Test
neurological outcome measures
- gait measures
- balance measures
- tone measures
- cognitive screening assessments
- diagnosis specific
list the gait outcome measures
- 6MWT
- 10 meter walk test
- dynamic gait index
- functional gait assessment
- time up and go (TUG)
what do timed walk tests assess
aerobic capacity and gait
6MWT predictive value for patients with heart disease
<1000 ft in 6 minutes is a strong predictor of morbidity and mortality within 3-12 months
each 0.10 m/s (INCREASE/REDUCTION) in baseline walking speed over 1 year was associated with poorer health status, poorer physical functioning, more disabilities, additional rehab visits, longer hospital stays, and higher costs
reduction
each 0.10 m/s (INCREASE/REDUCTION) in baseline walking speed over 1 year resulted in improved health status, improved physical functioning, fewer basic disability and instrumental disabilities, fewer hospital stays, 2 fewer rehab visits, 3 fewer med-surg visits, and 1 year cost reduction of $1,188
increase
slow gait speed is the single best predictor of
functional decline and disability
older adults without impairments can increase walking speed from what percent over comfortable pace
22-56%
what gait speed is sufficient for most community mobility
0.5 m/s (1.1 mph)
what is the usual adult walking speed
1.2-1.3 m/s (2.67-2.9 mph)
gait speed of household ambulators (severe gait impairment)
0.23-0.27 m/s
gait speed of limited community ambulators (moderate gait impairments)
0.4-0.8 m/s
gait speed of full community ambulators (mild gait impairments)
>0.8 m/s
what gait speed requires intervention to reduce fall risk
<1 m/s
what percent of people who walked <0.6 m/s were hospitalized at least once
41%
what percent of intermediate walkers (0.6-1.0 m/s) were hospitalized
26%
what percent of fast walkers (>1.0 m/s_ were hospitalized
11%
what gait speed in acute stroke patients is indicative of the need for inpatient rehab
10 meter walk test measures the time it takes a patient to walk how many meters
6 meters (2 meter 'buffer' on each end)
dynamic gait index assesses
an individual's ability to modify balance while walking in the presence of external demands
dynamic gait index rundown
- uses 8 tasks of gait to assess a person's ability to accommodate to changes in gait speed, walking with head turns, stepping over obstacles, and changes in environment
- assessment may be performed with or without an AD
8 tasks included in dynamic gait index
1. gait level surface
2. change in gait speed
3. gait with horizontal head turns
4. gait with vertical head turns
5. gait and pivot turn
6. step over obstacle
7. step around obstacle
8. steps
0 on dynamic gait index
severe impairment
1 on dynamic gait index
moderate impairment
2 on dynamic gait index
mild impairment
3 on dynamic gait index
no gait dysfunction
what score does a patient automatically receive when using an AD on the dynamic gait index test
2
dynamic gait index cutoff score for fall risk
<19/24
functional gait assessment assesses
postural stability during walking tasks
functional gait assessment rundown
- modification of the DGI developed to improved reliability and decrease ceiling effect
- uses 10 items to assess gait (uses 7 items from DGI)
- max score of 30
- AD permitted where scoring indicates
10 tasks included in functional gait assessment
1. gait level surface
2. change in gait surface
3. gait with horizontal head turns
4. gait with vertical head turns
5. gait and pivot turn
6. step over obstacle
7. gait with narrow base of support
8. gait with eyes closed
9. ambulating backwards
10. steps (up and down)
0 on functional gait assessment
severe impairment
1 on functional gait assessment
moderate impairment
2 on functional gait assessment
mild impairment
3 on functional gait assessment
normal
functional gait assessment cutoff score for fall risk
<23/30
TUG assesses
mobility, balance, walking ability, and fall risk in older adults
TUG rundown
- on the command "go" the patient rises from the chair, walks 3 meters at a comfortable safe pace, turns, walks back to the chair and sits down
- patient needs to start with their back against the chair
- one practice trial
- be consistent with AD used
- standard chair height 46 cm (not supported against wall)
- no physical assistance
TUG cutoff score for fall risk
>13.5 seconds
30-50 year old TUG norm
4.4-4.9 sec
60 year old TUG norm
5.6 sec
70 year old TUG norm
6.7 sec
80 year old TUG norm
7.8 sec
TUG score indicative of impaired functional mobility
>20 sec
TUG score indicative of need for assistance with transfers and inability to climb stairs
>30 sec
the slower the TUG, the (MORE/LESS) variability with times
more
cognitive dual-task TUG
patients will complete the test while counting backward by 3s from a randomly selected number 20-100
manual dual-task TUG
patients will complete the test while carrying a full cup of water (filled 5 cm from the top)
cognitive dual task TUG cutoff score for fall risk
>15 sec
list the balance outcome measures
- functional reach test
- berg balance scale
- mini BESTest
- 5 rep sit to stand
- 4 square step test
- ABC scale
- modified CTSIB
purpose of functional reach test
measure maximum forward reach in standing
what functional reach test score indicates a significant increased risk for falls
6 or less
what functional reach test score indicates a moderate risk for falls
6-10
purpose of berg balance scale
assess static balance and fall risk
berg balance scale rundown
- can be used in all settings
- takes about 15-20 minutes
- max score of 56
- patient cannot use AD for this test but is allowed to wear AFO
- items should be graded on the first attempt
berg balance test cutoff score for fall risk
<45/56
purpose of BESTest test (balance evaluation systems test)
assesses balance impairments across different contexts
mini-BESTest rundown
- balance evaluation systems test
- best all inclusive test of functional measure
contexts included in mini-BESTest test
- anticipatory postural adjustments
- reactive postural control
- sensory orientation
- dynamic gait
- dual tasking
mini BESTest cutoff score for fall risk
<21/32
purpose of modified clinical test of sensory integration and balance (MCTSIB)
quantify postural control under various sensory conditions
MCTSIB rundown
- patient stands on 4" foam (memory foam best) in a corner for safety
- stand 30 seconds, feet together, arms crossed
- if 30 seconds is not achieved on 1st trial, perform 3 trials and average scores
- useful in determining treatment strategies
MCTSIB sensory conditions
- eyes open, firm surface
- eyes closed, firm surface
- eyes open, compliant surface
- eyes closed, compliant surface
Activities-Specific Balance Confidence (ABC) Scale rundown
- subjective measure in which a patient rates their confidence in performing 16 different activities ("how confident are you that you will not lose your balance and become unsteady when you...")
- patient rates each item 0-100% confidence
- total ratings and divide by number of items completed
- 12/16 items must be answered to get a score
ABC Scale normative value for community dwelling older adults
79.89%
purpose of 5 time sit to stand test
- measure functional LE muscle strength (particularly quads)
- also useful in quantifying functional change of transitional movements
- correlates better to walking independence than MMT or handheld dynamometry
5 time sit to stand test rundown
- consistent chair height (17-18") that is unsecured (not up agaisnt a wall)
- patient sits with arms folded across chest
- patient trials 1-2 reps before being tested
- timing starts when you say go, stop timer when patient's buttocks hit the seat on the 5th repetition
sit to stand variations
- 10x STS
- single leg
- 30 second
- 60 second
5 time sit to stand cutoff score for fall risk
>12-15 seconds (dependent on source/dx)
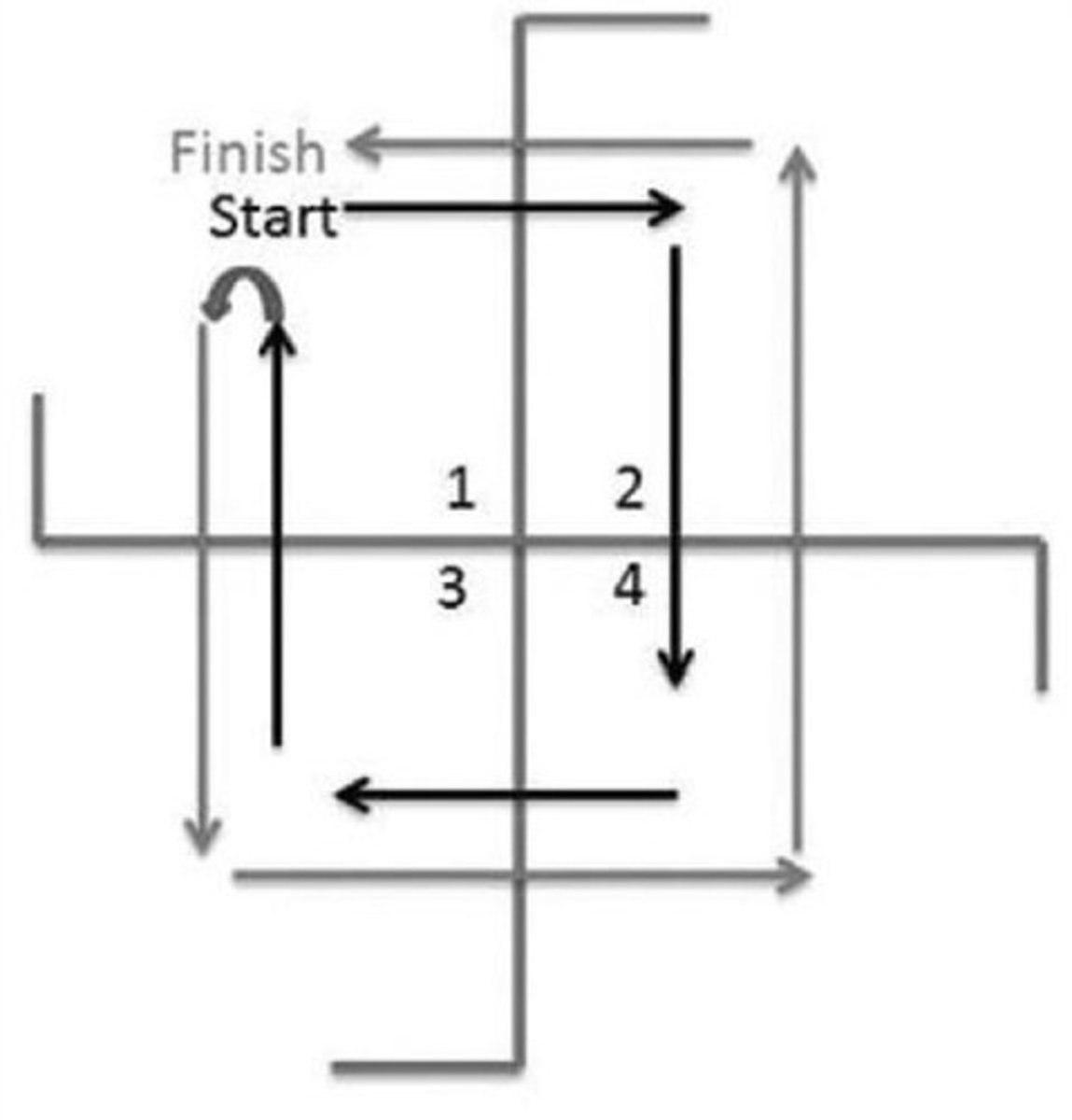
purpose of four square step test
assesses a person's ability to step over objects in different directions
four square step test rundown
- both feet must make contact with the floor in each square
- patient stays facing forward
- timing starts when the right foot contact the floor in square 2
- PT demonstrates
- patient has 2 timed trails, best time is demonstrated
scales used to measure tone/spasticity
- modified ashworth scale
- tardieu scale
purpose of modified ashworth scale
measures spasticity in patients with CNS lesions
0 on modified ashworth scale
no increase in muscle tone
1 on modified ashworth scale
slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of ROM when the affected part(s) is moved in flexion or extension
1+ on modified ashworth scale
slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout less than half of the ROM
2 on modified ashworth scale
more marked increase in muscle tone throughout most ROM, but affected part(s) easily moved
3 on modified ashworth scale
considerable increase in muscle tone, passive movement difficult
4 on modified ashworth scale
affected part(s) rigid in flexion or extension
purpose of Tardieu Scale
measures spasticity in patients with CNS lesion at different velocities
V1 speed on Tardieu Scale
as slow as possible (minimizing stretch reflex)