Hematology 1
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
75 Terms
Carotid arteries
Jugular veins
Arteries & Veins in the body
Head & Neck
Carotid Arteries (Common, Internal, External) – Supply oxygenated blood to the brain, face, and neck.
Jugular Veins (Internal & External) – Drain deoxygenated blood from the brain, face, and neck back to the heart
Aorta
subclavian arties
brachial artery
radial and ulnar arteries
pulonary arteries
Upper Body (Heart, Arms, Lungs)
Arteries:
Aorta – The largest artery, carries oxygenated blood from the heart to the entire body.
Subclavian Arteries – Supply blood to the arms and shoulders.
Brachial Artery – Runs along the upper arm, commonly used for blood pressure measurement.
Radial & Ulnar Arteries – Supply blood to the forearm and hand (radial artery is used for pulse check).
Pulmonary Arteries – Carry deoxygenated blood from the heart to the lungs (exception: an artery carrying deoxygenated blood).
Superior Vena Cava
Subclavian veins
Pulmonary veins
Veins:
Superior Vena Cava – Collects blood from the upper body and returns it to the heart.
Subclavian Veins – Drain blood from the arms into the superior vena cava.
Pulmonary Veins – Carry oxygenated blood from the lungs to the heart (exception: a vein carrying oxygenated blood).
Abdominal arota
renal arteries
lilac arteries
femoral artery
popliteal, tibial, and dorsalis pedis arteries
Abdomen & Lower Body
Arteries:
Abdominal Aorta – Supplies blood to organs like the stomach, liver, kidneys, and intestines.
Renal Arteries – Supply blood to the kidneys.
Iliac Arteries – Branch from the aorta to supply the pelvis and lower limbs.
Femoral Artery – Main artery supplying the thigh and leg.
Popliteal, Tibial, and Dorsalis Pedis Arteries – Supply blood to the knee, lower leg, and foot.
Inferior vena cava
hepatic vein
renal vein
iliac vein
femoral, popliteal, and tibial vein
Abdomen and lower body veins
Veins:
Inferior Vena Cava – Collects blood from the lower body and returns it to the heart.
Hepatic Veins – Drain blood from the liver.
Renal Veins – Drain blood from the kidneys.
Iliac Veins – Drain blood from the pelvis and legs.
Femoral, Popliteal, and Tibial Veins – Drain blood from the legs and feet back toward the heart
What is the human blood composition? (amount of blood in humans, and also what precent of each component is in the blood)
Blood composition - around 7% of body weight, equal to 5L in adults
Plasma dissolves all the cellular elements, 50-60% of blood is plasma and the rest is RBC’s
Plasma also contains: WBC’s, platelets, proteins, lipids, and
RBC formation, size, lifespan, and numbers
bone marrow
6-8 micrometers
100-120 days
4-8million/microlitre
WBC formation, size, lifespan, and numbers
bone marrow, lymphatic tissue
9-8 micrometers
24hrs-yrs
4.5k-11k/microlitre
Platelet (thrombocytes) formation, size lifespan, numbers
bone marrow
1-4 micrometers
8-12 days
150k-400k/microlitre
What is stem cell differentiation?
all blood cells originate from hematopoietic (rbc producing; HSCs) stem cells in the bone marrow
What are the two lines the HSCs can differentiate into?
Lineage Commitment – HSCs differentiate into either
Myeloid lineage (producing red blood cells, platelets, and some white blood cells)
Lymphoid lineage (producing lymphocyte; B cells, T cells, and natural killer cells
For RBCs (erythropoeisis);
what is the origin/ path?
where do they mature
final form
Red Blood Cells (Erythropoiesis)
Origin: Myeloid stem cells → Erythroblasts → Reticulocytes (teens)
Mature in: Bone marrow
Final form: Erythrocytes (RBCs), which carry oxygen.
For WBCs (leukopoeisis); granulocytes
what is the origin/ path?
where do they mature
final form
White Blood Cells (Leukopoiesis)
Granulocytes (Neutrophils, Eosinophils, Basophils) (have granules; tiny sacs with enzymes to attach intruders) - lobed nuclei to squeeze and have flexibility
Origin: Myeloid stem cells → Myeloblasts
Mature in: Bone marrow
Function: Fight infections and inflammation.
For Monocytes; (mega munchers)
what is the origin/ path?
where do they mature
final form
Monocytes (Macrophages & Dendritic Cells) (mega munchers)
Origin: Myeloid stem cells → Monoblasts
Mature in: Blood (monocytes) → Tissues (macrophages/eaters & dendritic cells/messengers, snitches)
Function: Engulf bacteria and present antigens
For lymphocytes;
what is the origin/ path?
where do they mature
final form
Lymphocytes (T cells, B cells, NK cells) (long term defence)
Origin: Lymphoid stem cells → Lymphoblasts
Mature in:
T cells → Thymus (immunity)
B cells → Bone marrow (antibody production)
Natural Killer (NK) cells → Bone marrow (attack infected cells)
For platelets (thrombopoiesis)
what is the origin/ path?
where do they mature
final form
Platelets (Thrombopoiesis)
Origin: Myeloid stem cells → Megakaryoblasts
Mature in: Bone marrow
Final form: Platelets (Thrombocytes), which help in blood clotting
What are some growth factors?
Erythropoietin
Thrombopoietin
Colony- Stimulating Factors (think army)
Growth factors:
Erythropoietin (EPO) – Helps make red blood cells (RBCs), which carry oxygen
Thrombopoietin (TPO) – Helps make platelets, which stop bleeding by forming clots
Colony-Stimulating Factors (CSFs) – Help make white blood cells (WBCs), which fight infections
Define each RBC disorder
anemia
hyperslenism
sickle cell disease
polycthemic vera (hint; POLY)
Red Blood Cell Disorders
Anemia – Low red blood cell count, leading to fatigue and weakness
Hypersplenism - spleen is overactive in blood cell removal
Sickle Cell Disease – Abnormally shaped red blood cells that block blood flow = pain
Polycythemia Vera – Too many red blood cells, making the blood thick, increase clot risk
What does hematological disease effect?
blood, bone marrow, and lymphatic system
Define each WBC disorder
leukemia
lymphoma - give a name too (hint; Hod)
neutropenia
White Blood Cell Disorders
Leukemia – Cancer of white blood cells (grow uncontrollably), affecting immune function
Lymphoma – Cancer of the lymphatic system (eg; Hodgkin’s and non-Hodgkin’s lymphoma)
Neutropenia – Low neutrophil count, increasing infection risk
Define each platelet disorder
thrombocytopenia
thrombocythemia
Platelet Disorders
Thrombocytopenia – Low platelet count, causing excessive bleeding.
Thrombocythemia – Too many platelets, leading to clotting issues.
Define each plasma disorder
hemophilia A & B
Von Willebrand Disease
Multiple Myeloma
Plasma Disorders
Hemophilia – A bleeding disorder due to missing clotting factors; Factor VIII (Hemophilia A) or Factor IX (Hemophilia B)
Von Willebrand Disease – A genetic disorder caused by a missing/defective protein (von willebrand factor), affecting blood clotting
Multiple Myeloma – Cancer of plasma cells in the bone marrow (abnormal plasma cells grow uncontrollably, leads to faulty antibodies), weakens bones and reduces immunity
what are inherited and acquired disorders?
Inherited
Eg; hemophilia; bleeding problems from defective coagulation factors
Acquired
Eg: viral infections, medication, radiation, heart conditions
How is specimen picked for hematology lab testing?
Specimen - capillary and venous blood samples, choice made is based on volume needed and specific biomarkers measured
What is a CBC?
Complete blood count (CBC) - common test, analyzes numerous markers; cell counts, hemoglobin, hematocrit, platelets, blood cell morphology
What is hemoglobin?
What % of RBC protein content does hemoglobin make up, and what is the structure of it
Hemoglobin is an iron-rich protein in red blood cells that transports oxygen from the lungs to the body's tissues and carries carbon dioxide from the tissues back to the lungs.
Hemoglobin characteristics - make up 98% of RBC protein content and provides red colour
Structure: heme and globin groups
Globin = quaternary structure of 4 protein chains linked together
Heme = iron that allows the binding of oxygen
Hemoglobin reference ranges for
newborn
children
adult males
adult females
age/gender | g/dl (grams per deciliter/tenth of a L) | Conversion factor | g/l (SI units) |
Newborn | 16-23 | x10 | 160-230 |
Children | 10-14 | x10 | 100-140 |
Adult males | 13-17 | x10 | 130-170 |
Adult females | 12-16 | x10 | 120-160 |
How does the specific gravity technique for hemoglobin measurement work?
Specific gravity technique (approximation)
Involves copper sulfate solution w/specific gravity of 1.052 (approx the same as blood with a low hemoglobin concentration)
If a drop of blood falls through = healthy hemoglobin count
If a drop floats = low hemoglobin count
How does the clinical method, or cyanmethemoglobin measurement work for hemoglobin?
Chemical methods (cyanmethemoglobin measurement)
Blood is reacted w/Drabkin’s solution, then reacts w/hemoglobin to form cyanmethemoglobin
Changes the colour of the solution, then is photometrically analyzed to determine the hemoglobin concentration
Photometrically = light measurement, how much light the sample absorbs at a specific wavelength
How does the hematocrit test measurement work for hemoglobin?
Hematocrit - test used to determine volume of patient’s RBC volume (oxygen carrying capacity)
Microhematocrit - test involving centrifuging a small sample of blood
Components of blood will separate by specific gravity
After centrifuging - bottom of tube = RBCs, top will have WBCs, buffy coat, platelets, and plasma (order is called packed cell column)
Specific gravity = ratio of density of a substance to the density of a reference substance (usually water at at 4°C, where water has its maximum density of 1 g/cm³)
Formula = Density of Substance/Density of Water (1 g/cm3)
What are the hematocrit reference values affected by?
Hematocrit reference values - affected by physiological and pathological factors
Normal values vary by age and sex
anemia/bleeding = lower levels
dehydration = higher values (bc when water loss, volume of plasma decreases (liquid part of blood), but the number of RBCs stay the same = higher concentration)
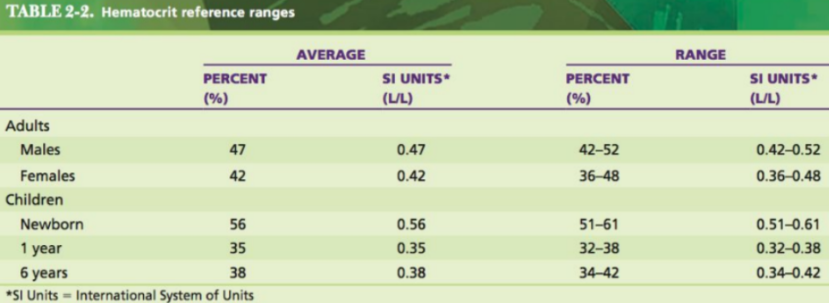
What are the hematocrit reference values for
adult male
adult female
children
newborn
1yr
6yrs
What can the appearance of packed cell colulmn indicate?
Appearance of packed cell column can indicate conditions
Eg; opaque plasma = high fat levels
What are the 3 steps to performing microhematocrit tests
Performing microhematocrit tests
Collecting specimen
Sample is obtained from a capillary puncture or from venus blood (w/anticoagulant)
Blood samples should be drawn into capillary tubes through capillary action
Centrifuging
Capillary tubes must be balanced
Generally spun at 10,000 RPM for 2-4 minutes
Reading test values
Microhematocrit readers are used to determine test values
RBC portion of tube is measured and a value is produced
What is hematocrit and microhematocrit?
Hematocrit is a measure of the proportion of your blood that is made up of red blood cells. It's expressed as a percentage and indicates how much of your blood's volume is red blood cells compared to the liquid plasma, white blood cells, and platelets. A low hematocrit can signal anemia (not enough red blood cells), while a high hematocrit can indicate conditions like dehydration or too many red blood cells (polycythemia)
Microhematocrit is a laboratory procedure that measures the volume percentage of red blood cells in a blood sample.
What is a hemocytometer?
Hemocytometer & blood cell counting
Blood count - automated counters and hemocytometer (microscopically)
Hemocytometer - precision made microscope slide that includes a counting chamber
Allows manual counting of blood cells in a sample
Typically glass slide w/2 counting chambers
Coverglass is needed on top of the slide to confine blood sample for microscopy
What does a moat do?
prevents overflowing
How is the hematocrit test divided?
Counting chambers - 2 on a hemocytometer, each divided into 9 squares
Each square is divided into further segments; corners are split into 16 squares and the center is split into 625 squares
4 corners are for counting WBCs (larger), center used for RBCs (smaller)
What is a hemocytometer and how do u count it?
Hemocytometer - manually count cells under a microscope
Preparing sample
Must be diluted depending on cell type
RBCs - 1:200 dilution
WBCs & platelets - 1:100 or 1:20 dilution
Employees must be trained on donning PPE and items
Loading hemocytometer - micropipette around 10uL of blood into counting chamber in a smooth unbroken stream
Cell counting pattern
count upper or left in a left→ right squiggle down alternating
What is the formula for calculating cell counts?
Calculating cell counts
Formula:
cells/uL = # counted cells (DF) / a(mm2)x0.1
DF = dilution reciprocal
What is the purpose of blood smears?
Blood smears - staining and observing RBCs, WBCs and platelets microscopically
Altered cell morphology can inform physicians about diseases; IM, sickle cell anemia, malaria
What specimen should you collect for blood smears?
Preparing blood smears
Specimen collection
Capillary blood is recommended
Venous blood can be used w/coagulant
How do u make, preserve, and qualities of a good smear
Making the smear
Two-slide method:
Drop of blood placed on 1 end of the slide
Another slide edge is placed at an angle to specimen slide
Edge is moved into a blood sample & when the specimen spreads along the edge, quickly push the slide forward to distribute the blood
Preserving the smear - immerse in methanol for 30-60 seconds
Methanol is a fixative that prevents deterioration of cellular components
Qualities of a good smear
Should cover ¾ of the slide and have gradual transition from heavy to light
No holes/ridges
Cells should be evenly distributed under microscope w/o overlapping RBCs in the thin section
What does staining the smear do? Explain wrights stain procedure
Wright’s stain procedure:
Quickstain - dip blood smear slide into Wright’s stain, creates adequate results in 2-5 minutes
Two step method - smear slides placed on a staining rack and are flooded with Wright’s stain
Then flooded w/buffer that accentuates the stain colours
Automatic stainer - staining machines, provide better results
What are common buffers in blood staining (resists ph change)
Common Buffers in Blood Staining: (proper pH 6.8-7.2)
Phosphate buffer (pH 6.8–7.2) – Used in Wright's, Giemsa, and Romanowsky stains
Sørensen’s buffer – A phosphate buffer used in hematology
What are different types of blood parts used for and why?
whole blood
plasma
serum
capillary
venous
arterial
Blood Type | Used For | Why |
Whole Blood | CBC, blood cultures, immunology tests | Contains all components (RBCs, WBCs, platelets, plasma). |
Plasma | Coagulation tests (e.g., PT, aPTT), electrolytes, hormones | Liquid part of blood contains proteins, hormones, nutrients, and waste. |
Serum | Blood chemistry, liver enzymes, antibody testing | Blood after clotting, ideal for assessing electrolytes and antibodies |
Capillary Blood | Blood glucose monitoring, newborn screening | Convenient for quick results, especially for glucose tests. |
Venous Blood - most popualr | Routine tests (CBC, liver/kidney function, cholesterol) | Standard source for most blood tests, easy to collect in larger volumes. |
Arterial Blood | Arterial blood gas (ABG) analysis | Provides accurate oxygen, carbon dioxide levels for respiratory and metabolic function. |
What is normal RBC morphology?
shape, size, color, nucleus, function
Red Blood Cells (RBCs):
Shape: Biconcave discs (donut-shaped, but without a hole in the center).
Size: About 7-8 micrometers in diameter.
Color: Pinkish due to hemoglobin content.
Nucleus: None, do not have a nucleus in their mature form.
Function: Carry oxygen and carbon dioxide.
What is normal platelet morphology?
shape, size, color, nucleus, function
Platelets:
Shape: Disc-shaped with a slightly irregular outline.
Size: About 2-3 micrometers in diameter.
Nucleus: None, as they are fragments of larger cells called megakaryocytes (large bone marrow cells)
Function: Play a key role in blood clotting by forming plugs in response to injury
What is normal neutrophil morphology?
shape, size, color, nucleus, function
White Blood Cells (WBCs):
Lobed: allows easier movement and performing specialized immune functions, eg squeezing through tiny blood vessels or engulfing pathogens
Granules: attack stuff and do the function
Neutrophils:
Shape: Multi-lobed nucleus (3-5 lobes).
Size: About 12-15 micrometers
Color: Pale cytoplasm with fine granules.
Function: First responders to infections, especially bacterial.
what is normal lymphocytes morphology?
shape, size, color, nucleus, function
Shape: Large round nucleus with a thin rim of cytoplasm.
Size: About 7-10 micrometers.
Color: Dark blue nucleus with a light blue cytoplasm.
Function: Important for adaptive immunity, producing antibodies (B cells) and attacking infected cells (T cells)
What is normal monocyte morphology?
shape, size, color, nucleus, function
Monocytes: EATERS AND SNITCHES
Shape: Kidney-shaped or horseshoe-shaped nucleus.
Size: About 15-20 micrometers.
Color: Pale blue cytoplasm.
Function: Differentiate into macrophages or dendritic cells (snitches) to fight infection and clear debris.
What is normal eosinophil morphology?
shape, size, color, nucleus, function
Eosinophils:
Shape: Bi-lobed nucleus (often resembling a figure 8).
Size: About 12-17 micrometers.
-orange granules in cytoplasm.
Function: Involved in allergic reactions and combating parasitic infections
What is normal basophil morphology?
shape, size, color, nucleus, function
Basophils:
Shape: Bi-lobed nucleus, often obscured by granules.
Size: About 10-15 micrometers.
Color: Dark purple granules in the cytoplasm.
Function: Release histamine during allergic reactions and inflammation
What does histamine do?
Histamine - causes blood vessels to expand and become more permeable (allowed substances to pass through)
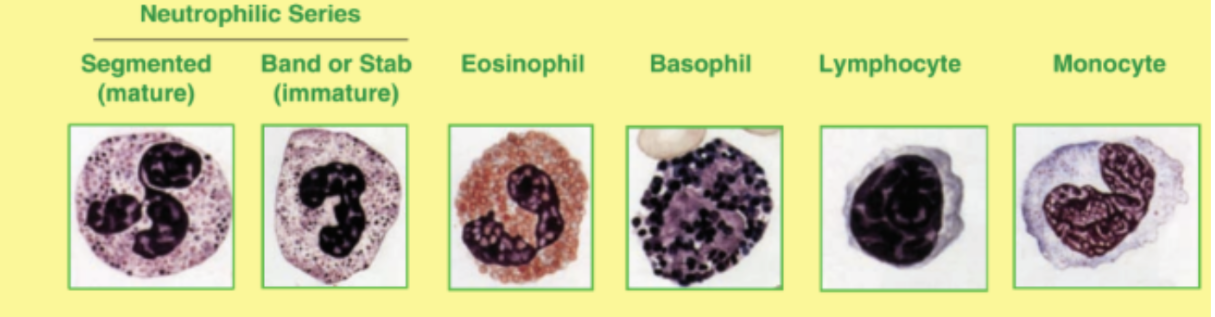
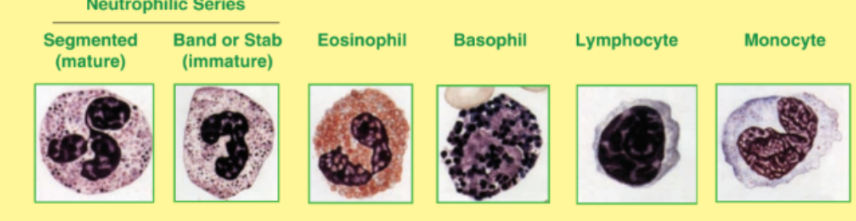
Image of all wbcs
What is Anisocytosis?
Anisocytosis - mix of RBC sizes in blood
What are microcytic and macrocytic rbcs caused by?
Anisocytosis - mix of RBC sizes in blood
Microcytic RBCs = smaller
caused by iron deficiency anemia, thalassemia (genetic blood disorder; lack of hemoglobin)
Macrocytic RBCs = larger
Caused by vitamin B12 deficiency, alcoholism, liver disease, folic acid deficiency (type of vitamin B9)
What is Poikilocytosis and what conditions is it seen in?
Poikilocytosis (genetic abnormalities in morphology)
Seen in anemia, liver disease genetic blood disorders
What are drepanocytes? (cause and effect)
Sickle Cells (drepanocytes):
Shape: Crescent or sickle-shaped (in low oxygen conditions)
Cause: Due to sickle cell anemia, where the hemoglobin in RBCs is abnormal
Effect: RBCs become rigid and sticky, blocking blood flow, insufficient oxygen supply for organs, and causing pain
What are spherocytes? cause and effect
Spherocytes:
Shape: Spherical (round)
Cause: Seen in conditions like hereditary spherocytosis or autoimmune hemolytic anemia (destroyed by spleen when they get trapped)
Effect: These cells are more prone to destruction in the spleen, leading to anemia
What are elliptocytes? cause and effect
Elliptocytes (ovalocytes):
Shape: Oval or elliptical
Cause: Often seen in hereditary elliptocytosis (destroyed by spleen)
Effect: These cells are less flexible, which may lead to mild hemolysis (destruction of RBCs) and anemia.
What are stomatocytes? cause+effect
Stomatocytes:
Shape: Oval with a central slit-like area (mouth-shaped)
Cause: Associated with hereditary stomatocytosis or liver disease
Effect: Can lead to membrane instability and impaired oxygen transport.
What are target cells? cause+ effect
Target Cells:
Shape: RBCs with a central area of hemoglobin surrounded by a clear ring (like a target)
Cause: Found in conditions like thalassemia, liver disease, and iron deficiency anemia
Effect: RBCs may have reduced oxygen-carrying ability
What are keratocytes? cause+effect
Keratocytes:
Shape: RBCs with blister-like vesicles or spiky projections
Cause: Often a sign of mechanical damage to RBCs (burns, movement through artificial heart valve, cut by fibrin strand) or conditions like microangiopathic hemolytic anemia
Effect: These cells are fragile and may be destroyed prematurely
What are crenated cells?
Crenated Cells: improper blood smear procedure
Shape: RBCs with spiny projections or irregular edges
Cause: Can result from dehydration, where the cell loses water and shrinks or prolonged exposure to anticoagulant
Effect: These cells are less flexible and can have impaired circulation
What are nonchromic, hypochromic, and hyperchromic cells
Normochromic cells - RBCs w/correct hemoglobin amount
Hypochromic = lower hemoglobin content, very thin outer rim
Hyperchromic = higher hemoglobin content, no central divot that normal RBC’s have
What are rbc inclusions? and what are they caused by
RBC Inclusions - abnormal structures/structures inside RBC’s
Diseases caused by toxicity, hemolytic anemia, vitamin deficiency
What is the appearance, cause, conditions, and effect of basophilic stippling?
1. Basophilic Stippling:
Appearance: Small, blue granules seen in the cytoplasm of red blood cells
Cause: granules are remnants of ribosomal RNA (or ribosomes) that are not removed during cell maturation
Associated Conditions: Lead poisoning, thalassemia, sideroblastic anemia (can't properly use iron to make hemoglobin), chronic liver disease
Effect: often a sign of impaired RBC maturation or a disturbance in hemoglobin production
What is the appearance, cause, conditions, and effect of Howell-jolly bodies?
Howell-Jolly Bodies:
Appearance: Small, round, purple or dark blue inclusions in the RBCs, representing nuclear remnants.
Cause: These bodies are left over from the nucleus when RBCs lose it during maturation
Associated Conditions: Splenectomy (removal of the spleen), hemolytic anemia, megaloblastic anemia (due to vitamin B12 or folate deficiency)
Effect: The spleen normally removes these remnants, so their presence suggests the spleen is not functioning or absent
What is the appearance, cause, conditions, and effect of cabot rings?
. Cabot Rings:
Appearance: Ring-shaped or figure-eight structures in the cytoplasm of RBCs, often purple.
Cause: They are believed to be remnants of the mitotic spindle or nuclear material
Associated Conditions: Severe anemia (eg megaloblastic anemia; abnormally large RBCs that don't work properly), lead poisoning, myelodysplastic syndromes (group of bone marrow disorders)
Effect: These are rare but indicate disrupted cell maturation or abnormalities in RBC production
What is the appearance, cause, conditions, and effect of nucleated rbcs?
. Nucleated RBCs:
Appearance: RBCs that still contain a nucleus
Cause: immature RBCs are being released into the bloodstream prematurely, happens when the bone marrow is under stress or producing RBCs rapidly
Associated Conditions: Severe anemia, bone marrow disorders, hemorrhage (bleeding), hypoxia (insufficient oxygen supply to body tissues)
Effect: Normally, RBCs lose their nucleus in the bone marrow before entering circulation, presence in the blood suggests abnormal bone marrow function or increased RBC production
What is leukopenia and the cause?
Leukopenia - low WBC count
Causes: infections, antibiotics, chemotherapy, radiation
Bone marrow disorders - leukemia, aplastic anemia, myelodysplastic syndrome
What is leukocytosis and the cause?
Leukocytosis - high WBC count
Causes: infections, exercise, anxiety, medications, steroids
what is leukemias?
Leukemias - unrestrained production of leukocytes in bone marrow
Inhibits growth of other cells, leading to anemia
What is cause of thrombocytopenia and thrombocytosis?
Thrombocytopenia - low levels caused by radiation, certain drugs, alcoholism, leukemia
Thrombocytosis - high levels caused by inflammatory conditions, reaction to other blood disorders