GI Lecture 1: Control/Regulations, Blood Circulation, Motility, Secretion
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
the control mechanisms of the GI system regulates:
conditions of the lumen
versus internal control
the control mechanisms of the GI system are NOT governed by the nutritional status of the body but rather
by the volume and composition of luminal content
Luminal stimuli:
Distension of the wall by the volume of the luminal contents
Chyme osmolarity (total solute concentration)
Chyme acidity
Chyme concentrations of specific digestive products (aa, glucose,FA, peptides)
GI receptors are located where and are what type of receptors?
located on the wall of the tract
mechanoreceptors, osmoreceptors, chemoreceptors
what are the effectors of the GI tract?
muscle layer in the wall of the tract
Exocrine glands that secrete substances into the lumen
Neural control of the GI system
1) enteric system
-myenteric plexus
-submucosal plexus
2) ANS
3) sensory nerves
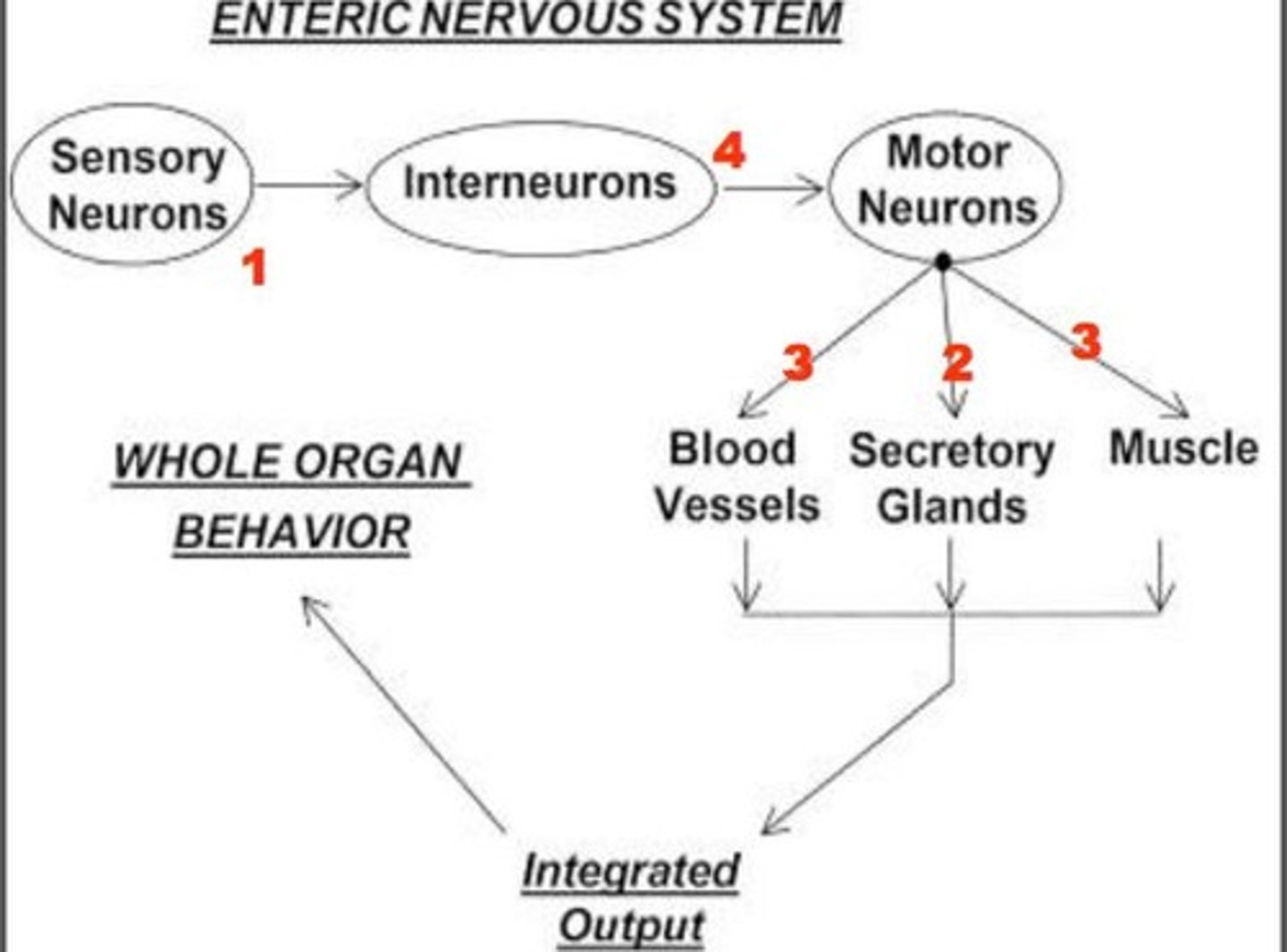
Describe the enteric system components and its functions
Lies entirely in the GI wall
Extends from esophagus to anus
Controls movement and secretion
May be excitatory OR inhibitory
Can function on its own or under ANS
Describe Myenteric plexus (Auerbach's plexus) location and control
Between longitudinal and circular muscle
Controls movement; excitatory and inhibitory
Extends all the way
Primarily controls:
Local and inter-regional motility activity through regulation of Circular and Longitudinal Muscle Layers
Blood Flow. However, overlapping and integrated control exists between the plexuses
Describe Submucosal plexus (Meissner's plexus) location and control
Submucosa
Controls local secretion and blood flow
Local
Primarily Controls:
Smooth muscle activity of the Muscularis Mucosae, affecting mucosal surface area
Secretion from mucosal endocrine and other secretory cells
What are the Neurotransmitters of the enteric system
ACh: excitatory
NE: inhibitory
What are the Effectors of the enteric system
Muscle cells
Exocrine glands
all have ducts, secrete into Lumen
Sensory Neurons of the Enteric system
-respond to various stimuli (stretch, food composition)
-mainly via receptors (mechano-, chemo-)
-located w/in mucosal epithelium of SM layers
-afferent fibers may RELAY SENSORY info to either enteric or extrinsic neurons which relay the appropriated efferent response
Secretory Neurons of the Enteric System
-innervate mucosal secretory cells
-regulate endocrine & exocrine functions of the mucosa
Motor Neurons of the Enteric System
-innervate smooth muscle layers
-control gut motility & mucosa surface area
-Blood vessel vasoconstriction & vasodilation are also affected
Interneurons of the Enteric System
-synapse with other neurons to relay information between
neurons within the same or adjacent plexus or between enteric
and extrinsic neurons
-This allows communication and integration of functions up and
down as well as outside the GI tract.
-Allows communications between enteric system and CNS
P-ANS connection with enteric system
-cranial through?
-sacral through?
cranial through the VAGUS nerve (CNX)
sacral through the PELVIC NERVE (PN)
P-ANS stimulation has an ______influence on the functions of the GI tract?
Excitatory
motor innervation of the vagus nerve
-tongue
-pharynx
-upper esophagus (swallowing)
Vagus nerve innervates what parts of the GI tract?
from tongue to transverse colon
Pelvic nerves innervates what parts of the GI tract?
Descending colon to rectum
motor innervation of the pelvic nerves
external anal sphincter (defecation)
S-ANS connection with Enteric System
-originates at?
-through what?
-Originates in T5 and L2
-Through the sympathetic chain
S-ANS stimulation generally has an ______influence on the functions of the GI tract?
Inhibitory
Sensory nerve endings in the GI epithelium and wall send AFFERENT fibers to
-Enteric plexus
-Sympathetic system
-Parasympathetic system
There is some motor VOLUNTARY innervations in the GI. For example
-Swallowing
-Defecation
Non neural control involves what molecules
hormones and GI peptides
GI regulatory peptides carry the non-neural control of GI functions and are classified according to
mechanism of delivery to target cell
-endocrine peptide: hormone
-paracrine peptides
-neruocrine peptides
GI regulatory peptides
-detected in lumen
-reach their target cells via circulation
-Exist in CNS and in GI plexus neurons where they function as neurotransmitters
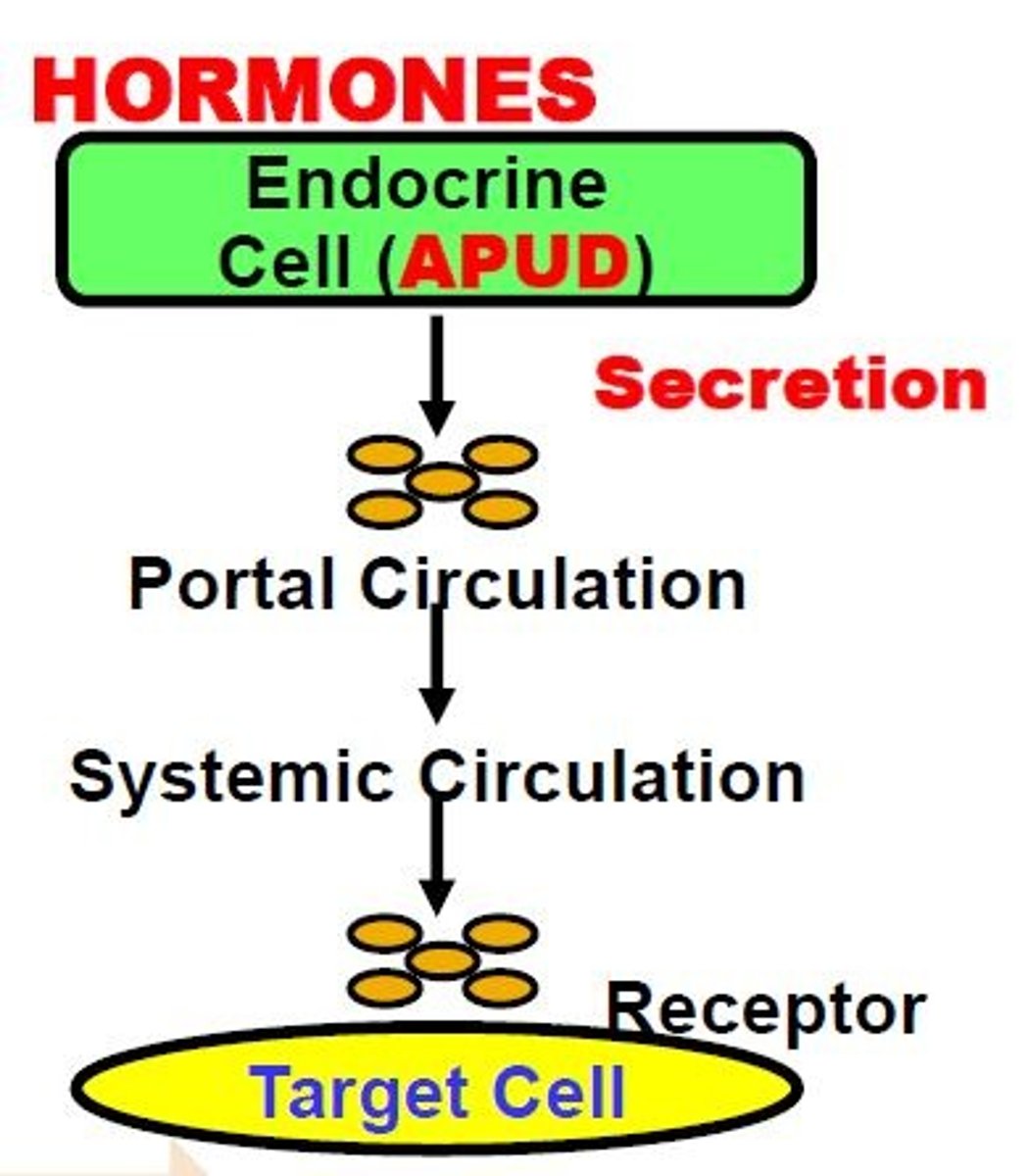
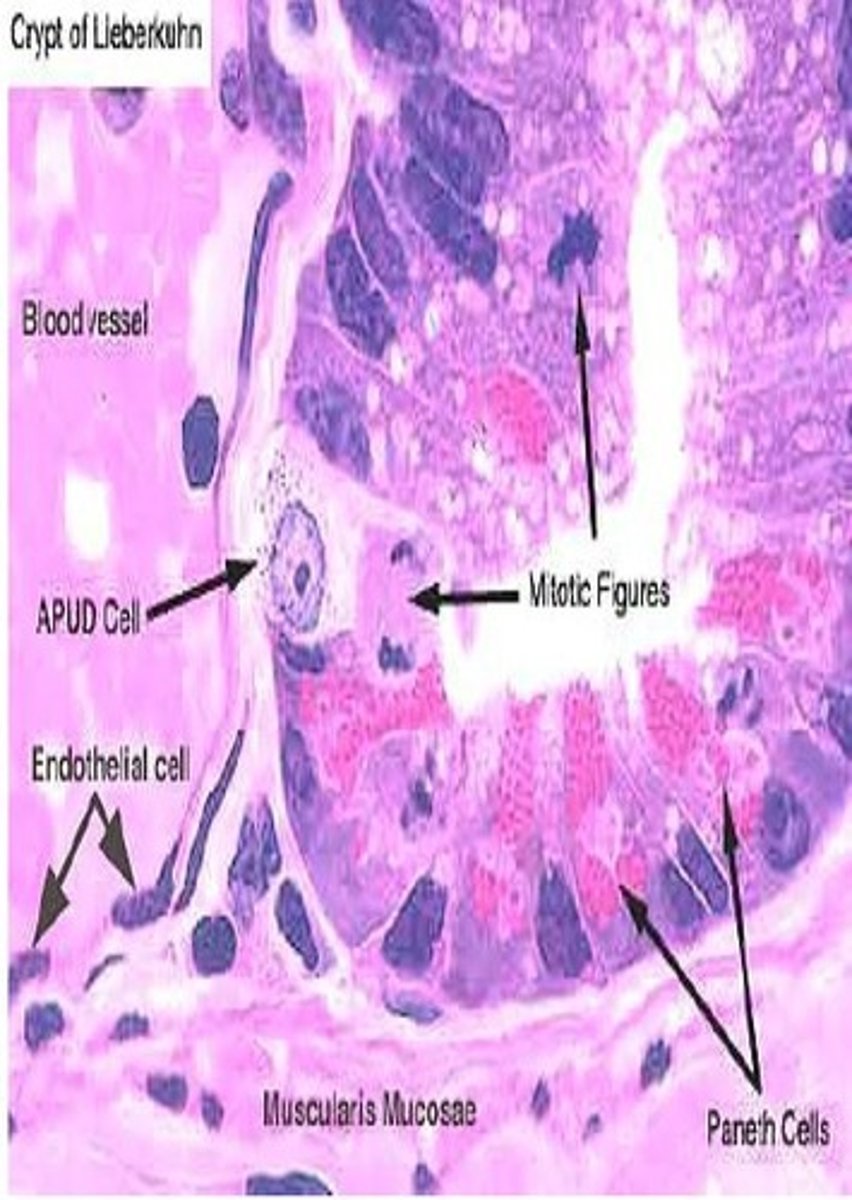
Endocrine Peptide Hormones
Released (Secretion) from specialized mucosal Endocrine Cells (APUD = Amine Precursor Uptake Decarboxylation) into the blood
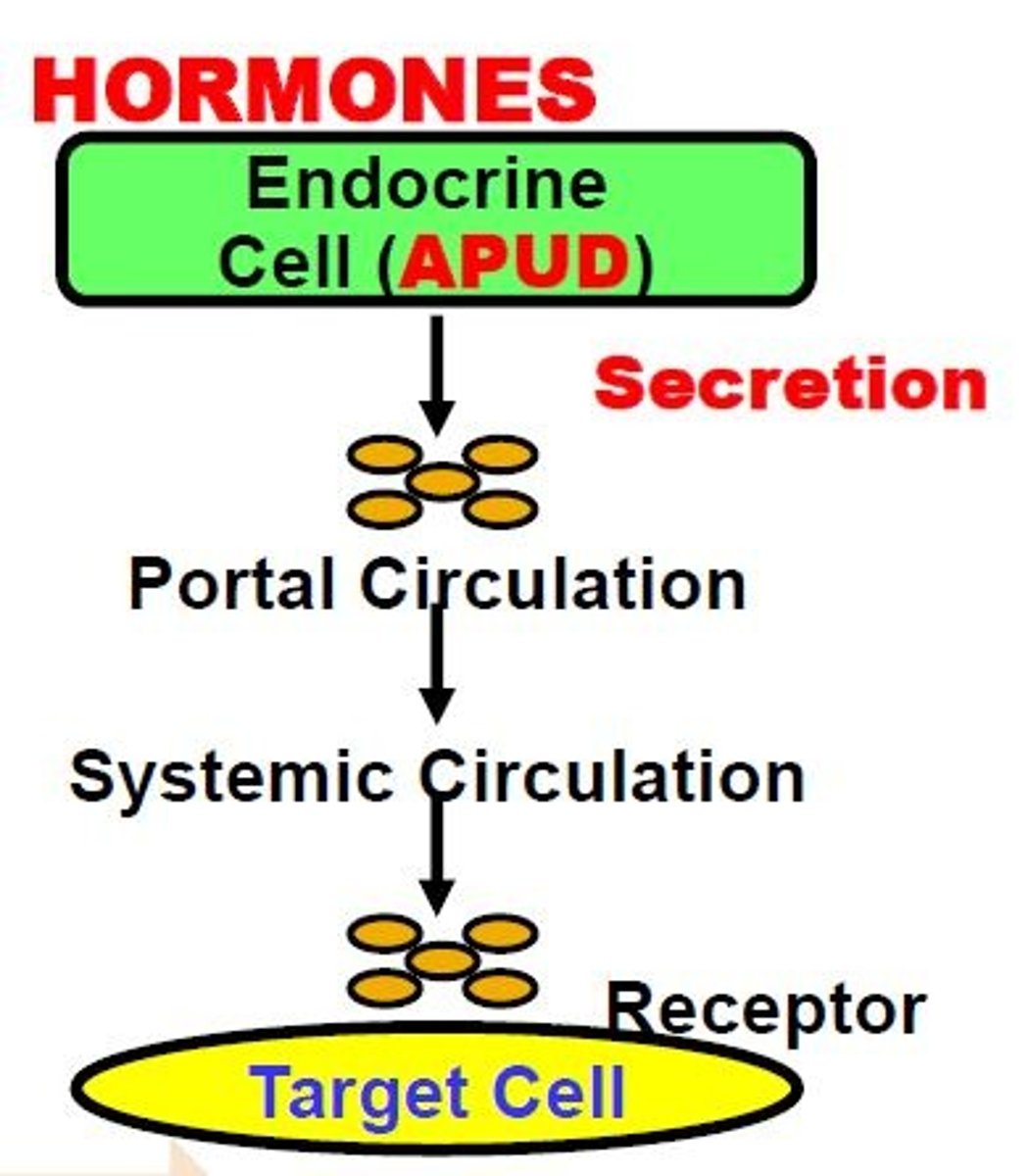
Endocrine Peptide Hormones act via what on target cells?
Act via hormone-specific Receptors on Target Cells--all acting on smooth muscle of a gland
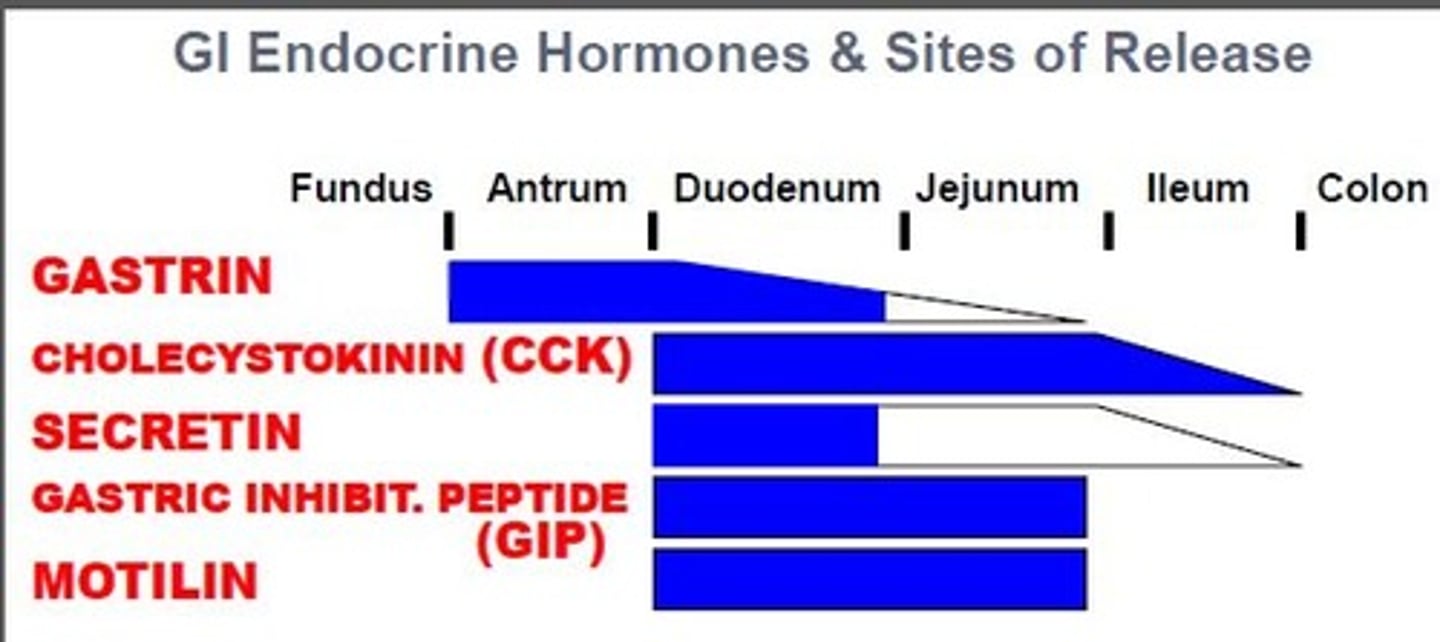
ex. of peptide hormones
o Cholecystokinin
o Gastrin
o Gastric inhibitory peptide
o Motilin
o Secretin
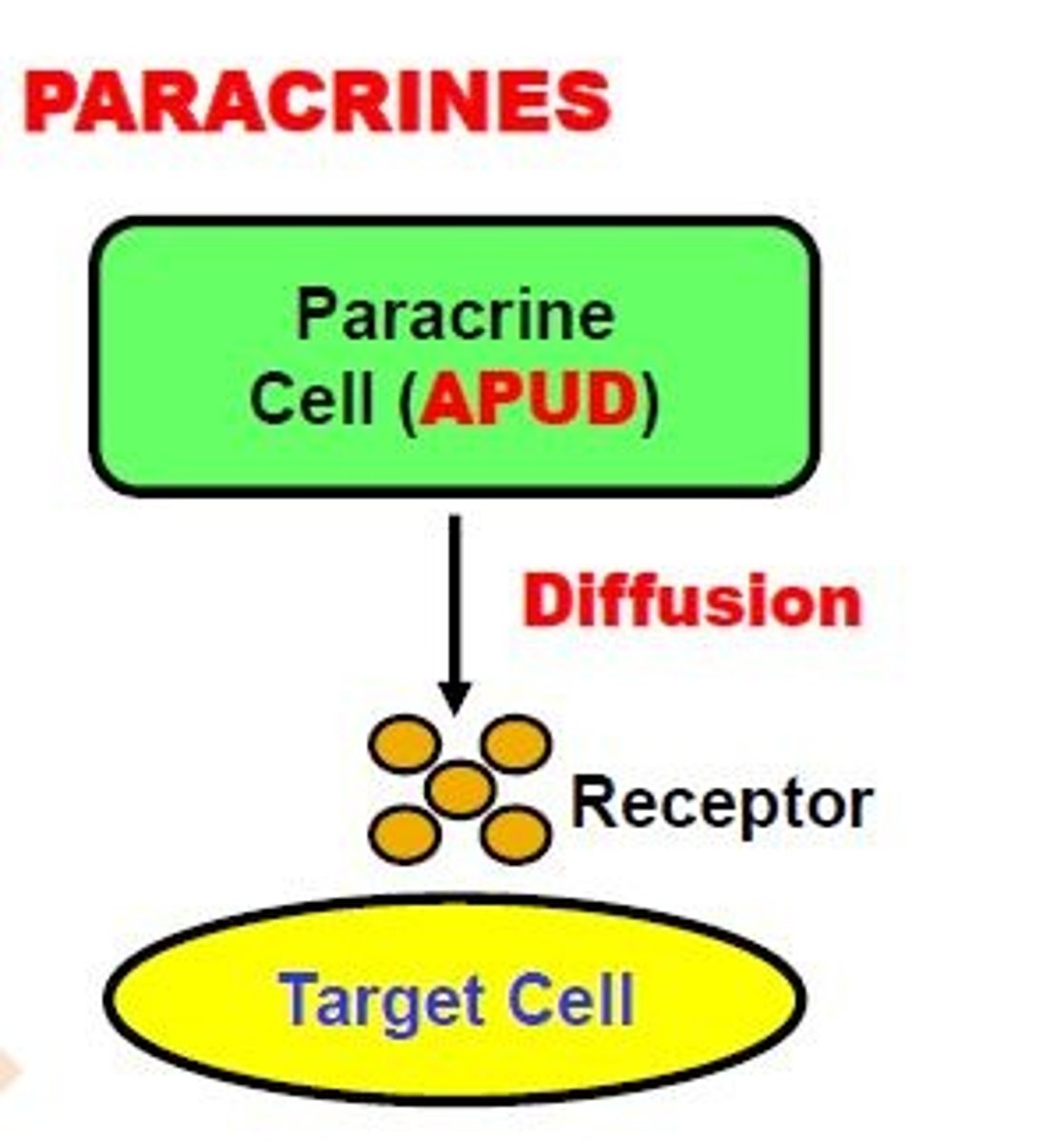
Paracrine peptides
-Released from APUD Cells
-Do NOT enter the circulation
-Delivered by DIFFUSION to closely neighboring Target Cells
ex. histamine
Neurocrines
-produced in neurons
-released from axon endings in response to an action potential
-act on target cells via synapses
ex.
-Vasoactive Intestinal Peptide (VIP)
-Gastrin Releasing Peptide (GRP)
-Enkephalins
Most GI endocrine hormones are secreted by?
Duodenum & Jejunum
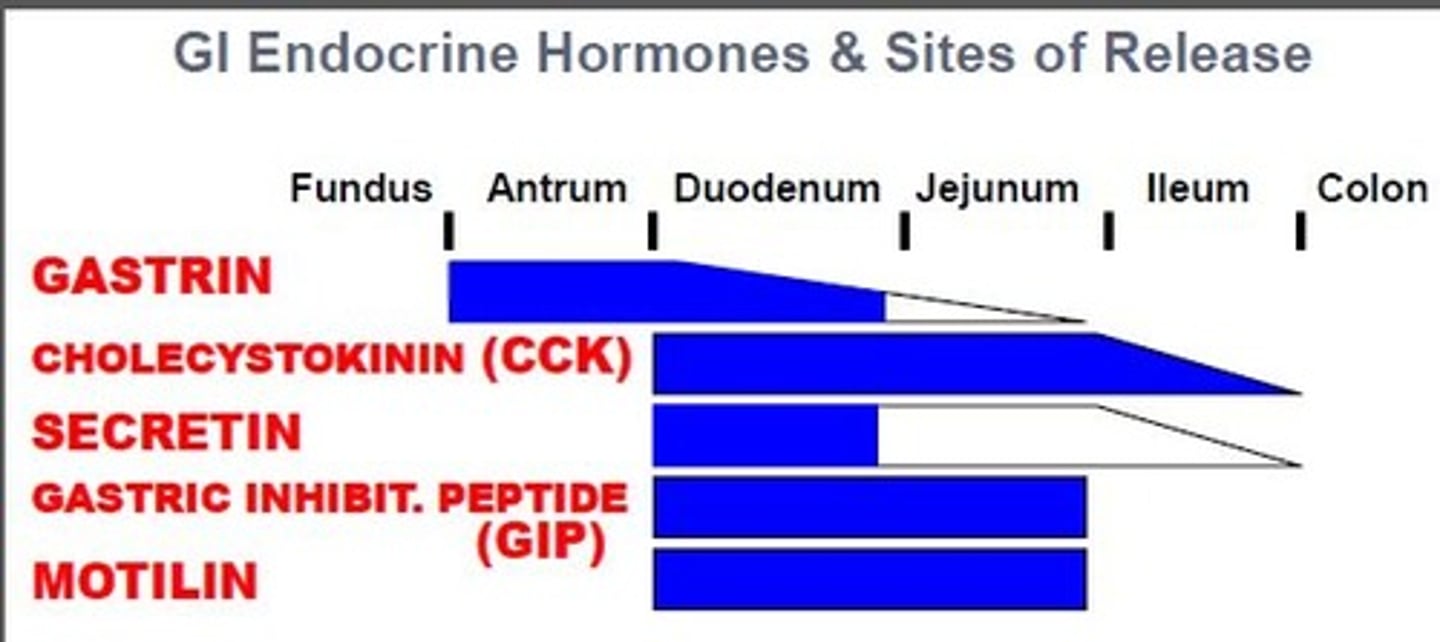
Only hormone secreted by stomach
Gastrin
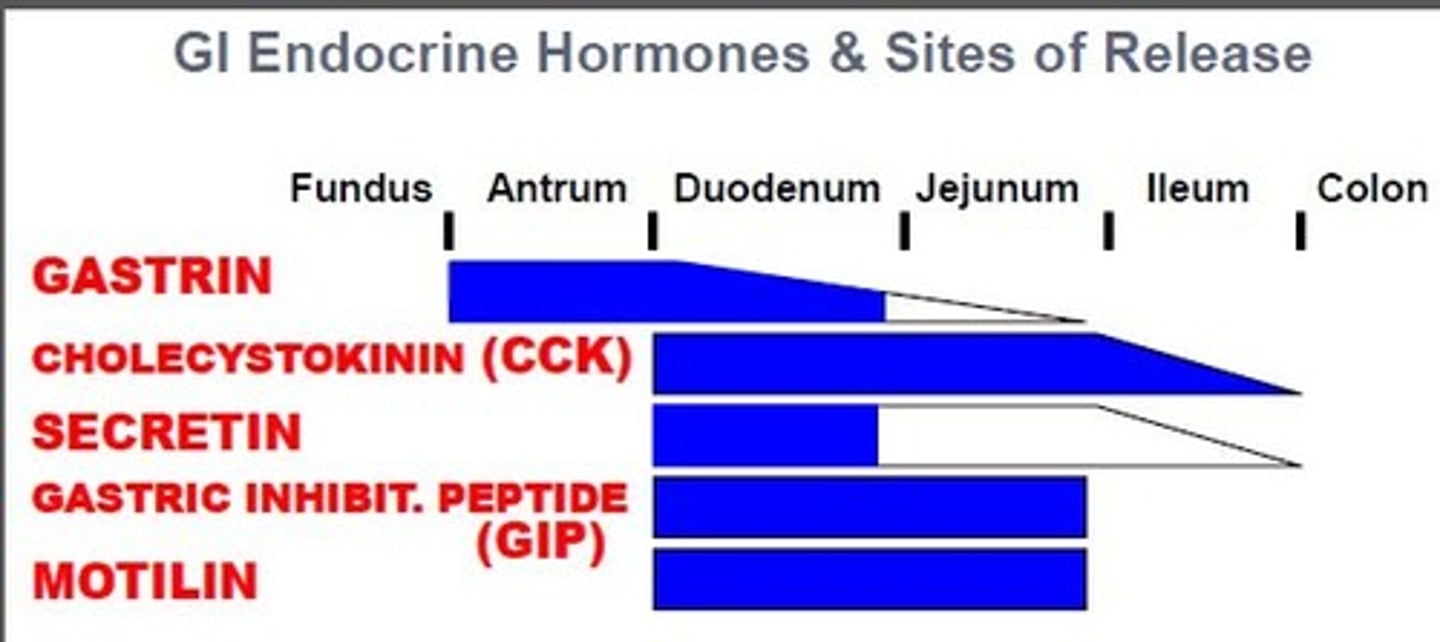
Hormones released from colon
None
Basic principles of GI regulatory peptides
-each hormone participates in a feedback control mechanism that regulates some aspect of the GI luminal environment
-each hormone affects more than 1 type of target cell
FA and AA trigger what?
Trigger CCK secretion from cells in small intestine into blood
CCK stimulates what?
Stimulates the pancreas and gall bladder
When FA and AAs are absorbed what happens to the stimuli for CCK
The stimuli for CCK is removed (feedback)
A single GI effector cell contains
-Receptors for more than one hormone
-Receptors for more than one neurotransmitter
-Receptors for more than one paracrine agent
Potentiation
Occurs when one hormone effects amplifies the response of another, e.g., secretin and CCK
Arterial blood is carried to the GI tract through
1. Superior mesenteric artery
2. Inferior mesenteric artery
3. Celiac trunk
From the GI tract, spleen and pancreas blood is carried to the liver through ________
The portal vein
In the liver blood flow through large ______ along which specialized cells remove bacteria and particulate matter
Sinusoids
The liver cells also detoxify the blood from the GI tract. From the liver, blood returns to circulation through _______
Hepatic Vein
Hepatic Portal System: 4 basic steps
1) small intestine absorbs products of digestion
2) Nutrient molecules travel in hepatic portal vein to liver
3) liver monitor blood content
4) blood enters general circulation by way of hepatic vein
The Splanchnic circulation is blood flow through GI tract, the spleen, pancreas, and liver
What 3 arteries are involved?
Superior mesenteric artery
Inferior mesenteric artery
Celiac artery
Main takeaway: bring blood from the AORTA to the wall of the gut
Splanchnic circulation: The circling arteries penetrate the wall and branch into smaller arteries within __________
the muscle, mucosa and submucosa
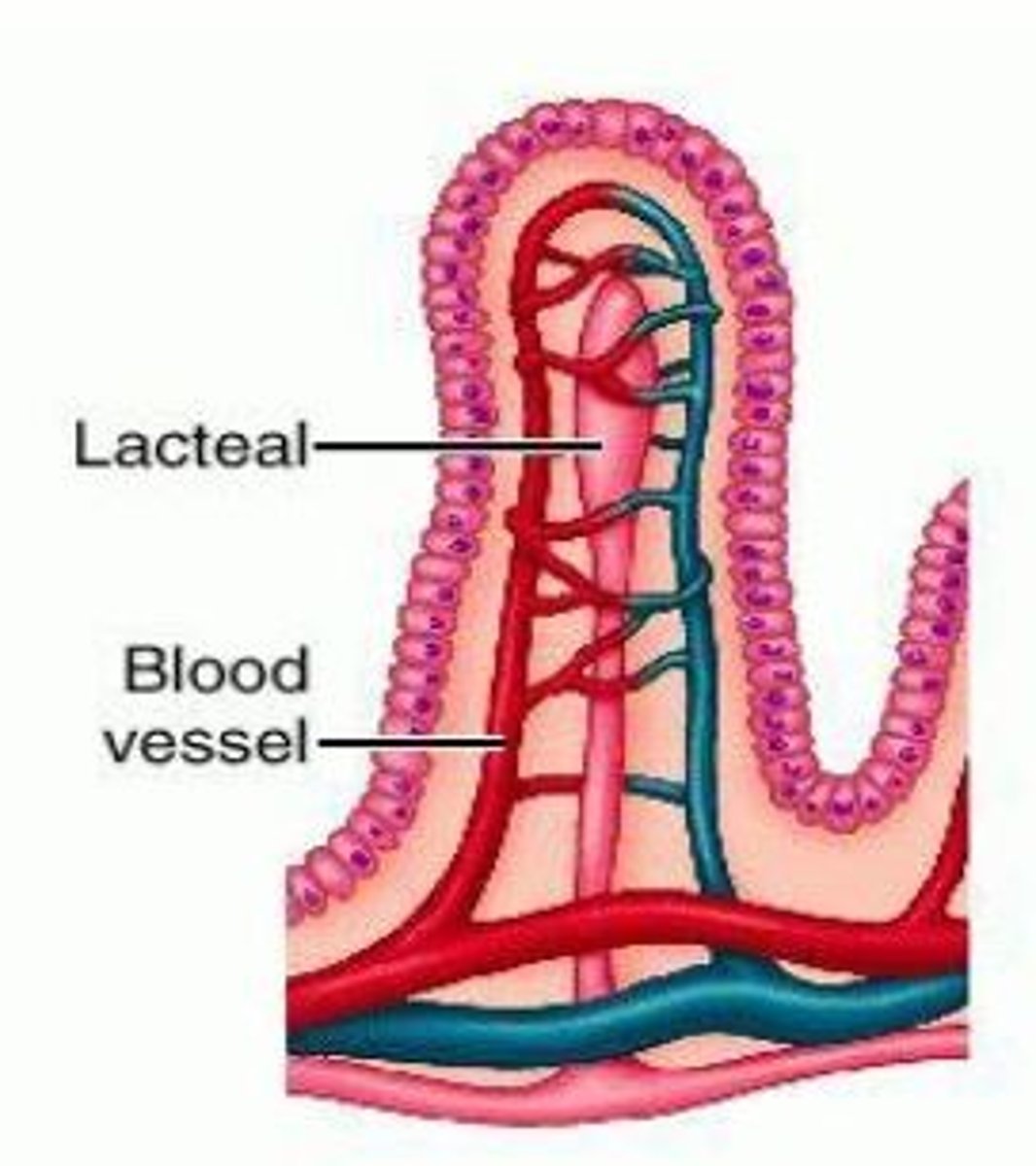
Mechanics of the special arrangement of smaller arteries within the villi of the small intestine
-the arterial and venous blood flow in the villi are in OPPOSITE DIRECTION
-Blood oxygen diffuses directly from the capillaries into the venules WITHOUT the NEED TO REACH THE TIP OF THE VILLI
Liver cells _____ the blood and use nutrients absorbed from the GI
Detoxify
Blood then enters the _______ (2) which empties into the _______
Central Vein, Hepatic Vein
The types of GI motility
1) propulsive movement
2) mixing movement
What is propulsive movement: peristalsis
A series of alternating contractions and relaxations of smooth muscle that lines the walls of the digestive organs and that forces food to move forward
An inherent property of smooth muscle
stimulation of propulsive movement (peristalsis)
Distension, Chemical, physical
Effectual peristalsis requires an active what?
Active Myenteric Plexus
Contractile ring in circular muscle behind the point of distension
Absence of myenteric plexus
-Congenital megacolon
-Atropine
Congenital megacolon
Congenital disorder of peristalsis of distal bowel caused by absence of parasympathetic ganglion cells in the myenteric plexuses
Atropine
Paralyzed cholinergic nerves
Peristalsis results from the initiation of
A unidirectional Spreading Contraction of the Circular Muscle
This typically forms behind a food bolus and serves to move the bolus in the aborad (away from the mouth) direction
Physiologically, peristalsis mainly results in a Propulsive Action on GI contents which causes net movement. Some mixing of content also occurs
Mixing movement: segmentation results from:
A Focal Contraction of the primarily Circular Muscle layer that constricts the lumen and compresses GI contents at the site
This action is coordinated with Longitudinal Muscle layer contraction and circular muscle layer relaxation on either side of the constricted site
Physiologically, segmentations primarily results in a mixing action that reduces food particle size, homogenize particles with digestive enzymes and other secretions, and exposes contents to the mucosal surface
Segmentations does NOT typically results in significant net movement (propulsion) of material along the tract
Peristalsis is PRIMARILY PROPULSION + Mixing, while segmentation is
Mixing only
transit time through segments of GI tract:
-esophagus
-stomach
-small intestine
-large intestine and colon
-total
esophagus: 5-15 sec
stomach: last: 3-5 hrs, first= 1-5 min
small intestine: 2-4 hrs
large intestine and colon: 36-48 hrs
total: 48 hrs
relaxation of SM sphincters = _________ GI propulsion
constriction of SM sphincters =_________GI propulsion
relaxation of SM sphincters = increase GI propulsion
constriction of SM sphincters = decreased GI propulsion
Extrinsic Autonomic Control
Increased Parasympathetic = Increased propulsion and mixing
Increased Sympathetic = Decreased propulsion and mixing
Enteric Autonomic Control
Primarily Myenteric Plexus (Muscularis Externa)
integrates with Extrinsic Controls
Allows fine local control
Coordinates interregional propulsive/mixing movements
Voluntary and GI Peptide Control:
Overall minor roll
Voluntary - Swallowing reflex and defecation control
GI Hormones - Motilin: stomach motility action
Intrinsic Basal Tone
Some Smooth Muscle regions of the GI tract (e.g. Lower Esophageal Sphincter) are under almost constant Tonic Contraction
The “natural” state of the muscle without any extrinsic influences is the contracted state
This basal contractile tone is distinguished because it is initiated without apparent extrinsic input from nerves or hormonal factors
Tone is generated intrinsically by the smooth muscle cells themselves
→ Regions displaying basal muscle tone are said to be under Intrinsic Myogenic Control
Tonic Contractions can be __________ physiologically by certain extrinsic factors such as
autonomic neural input or
hormones
other regulatory peptides.
Transiently Modulated
GI secretion refers to the ______ and ______ of fluids and substances into the lumen of the GI tract by mucosal cells and/or accessory GI organs
Production; Release
__ L of fluid is secreted into the GI tract each day, not including approximately 2 L of daily fluid intake in the diet .
>7 L
Secretions along the GI tract are _______ in Composition, depending on
Highly Variable
-Mucosal Cell Type (APUD, Parietal, Chief, Goblet, etc.) within the segment
-Accessory Organs (e.g. Salivary Gland, Pancreas, Liver).
Compostion of GI secretions
-water
-mucus
-ions
-enzymes
-hormones
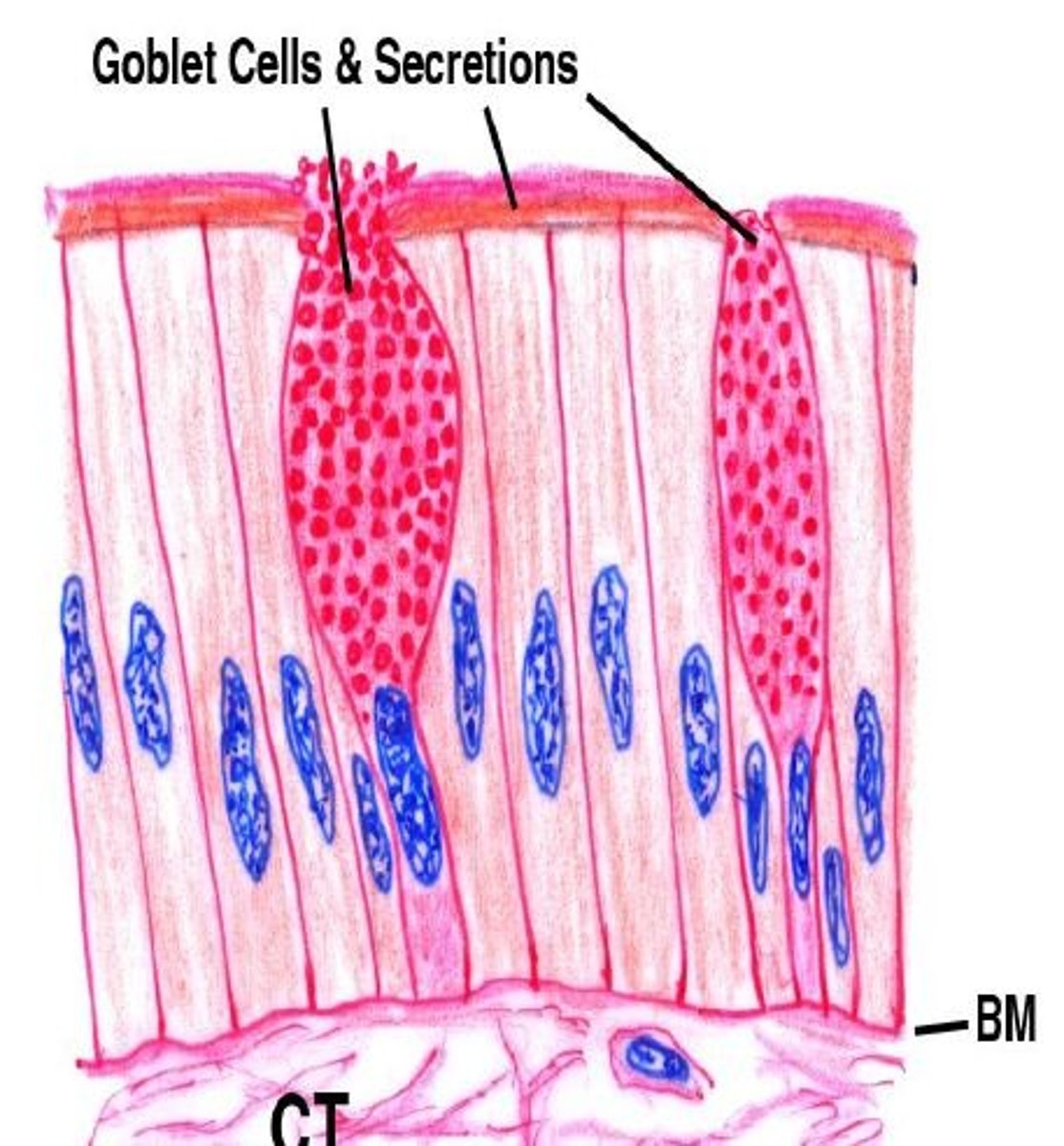
Goblet cells
-single-celled glands lining the GI mucosa (most in large intestine/colon)
-secretes MUCUS onto the the mucosa to lubricate and protect the surface from abrasion and chemical digestion
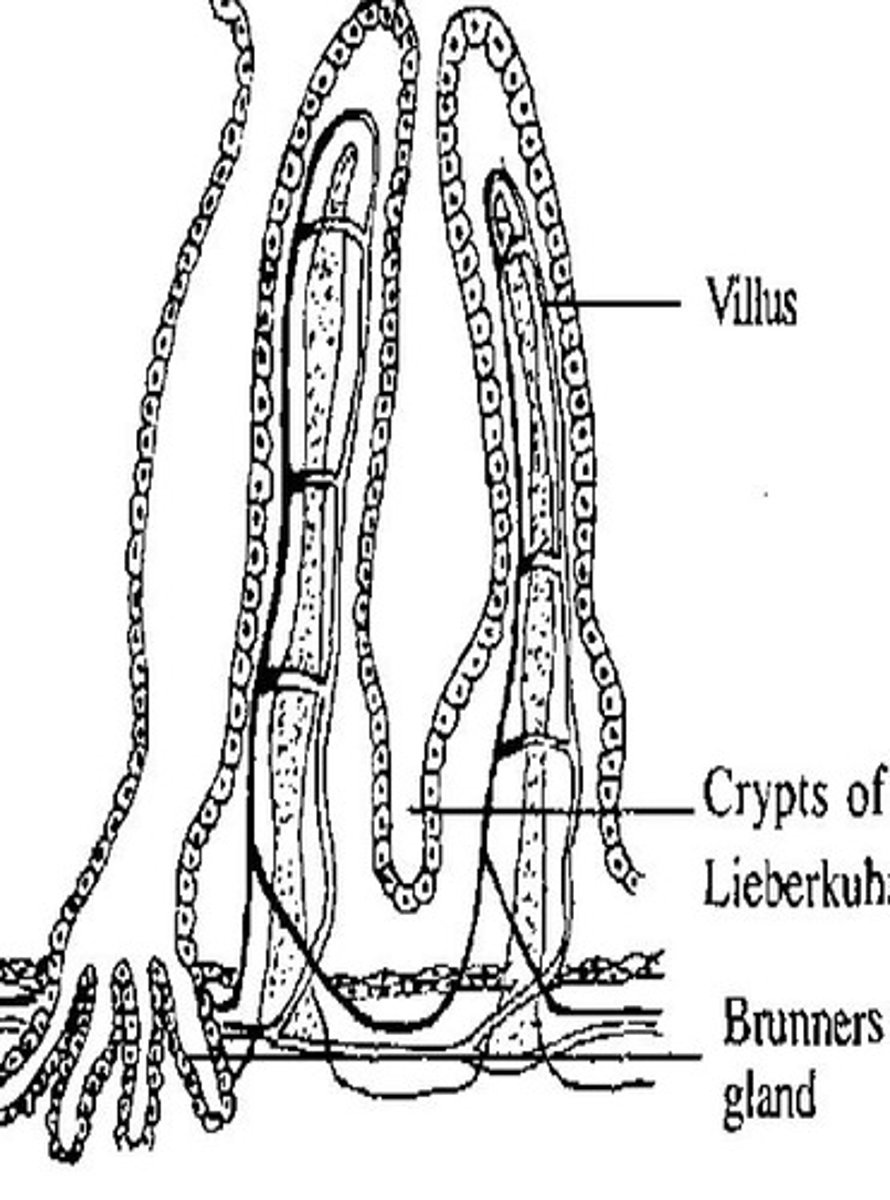
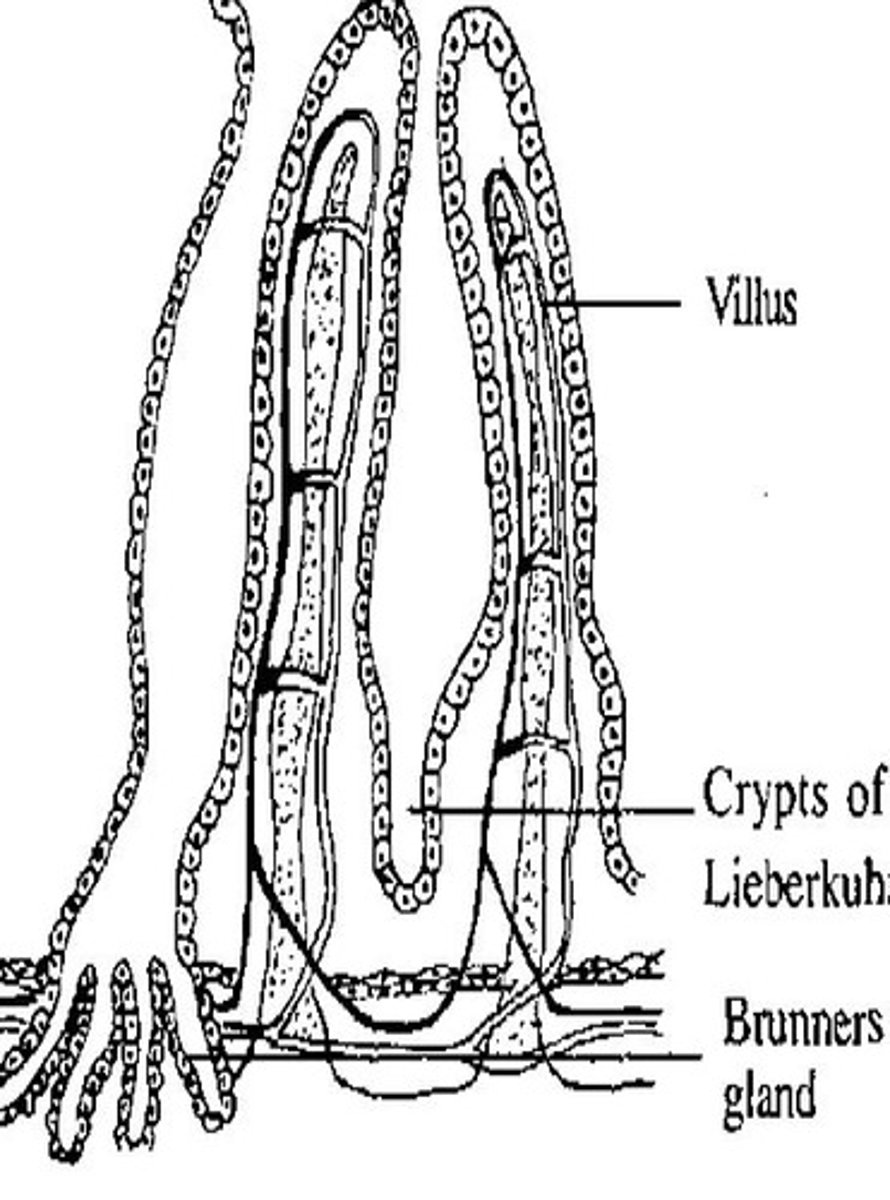
Brunner's Glands
-compound glands near the proximal duodenum
-secrete alkaline mucus that neutralizes gastric acid
Tubular Glands
-stomach and duodenum
-parietal cells (secretes acids)
-chief cells (secretes pepsinogen)
Crypts of Lieberkuhn
-deep pits formed by mucosal folds
-mainly small intestine
-contain several types of secretory cells including: goblet cells and enterocytes that secrete:
digestive enzymes
H2O
ions that facilitate digestion and absorption
APUD cells
-single-cell mucosal endocrine glands
-mainly small intestine
-secrete various GI hormones involved in endocrine regulation of GI functions
Accessory Glands
-salivary glands
-pancreas
-liver
-secrete saliva, HCO3-, enzymes, & bile) for Lubrication, Acid Neutralization, Digestion & Absorption.
Basic Mechanics of Stimulation of Secretion
Contact of food
direct stimulation of glandular epithelium
activation of enteric nervous system
Autonomic stimulation
Parasympathetic
Hormonal Regulation