Topic 6: The Heart as a Pump & the Regulation of Cardiac Output
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
Contraction & ejection describes __, whereas relaxation & refilling describes __.
systole; diastole
Heart sounds correspond to __ of valves.
closure
What happens when the left ventricular pressure is greater than the aortic pressure?
the aortic valve is able to open and blood can be ejected
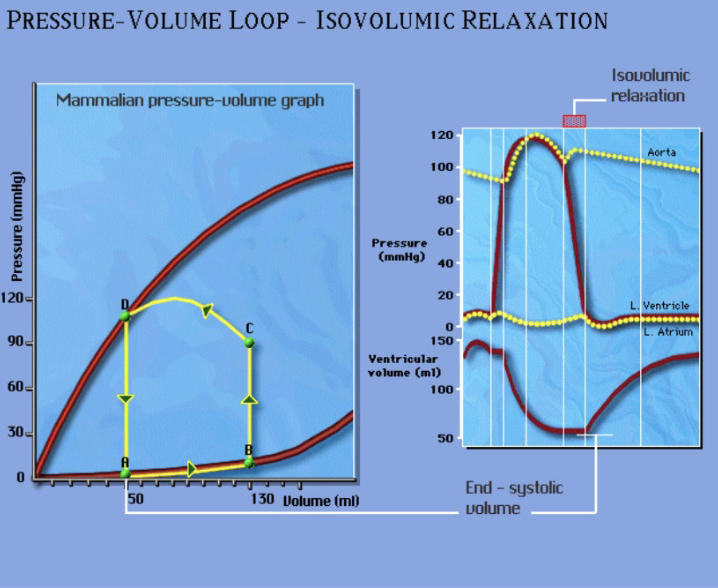
In this graph, describe what is happening from A —> B.
diastolic filling phase that determines the preload
point B = end diastolic volume
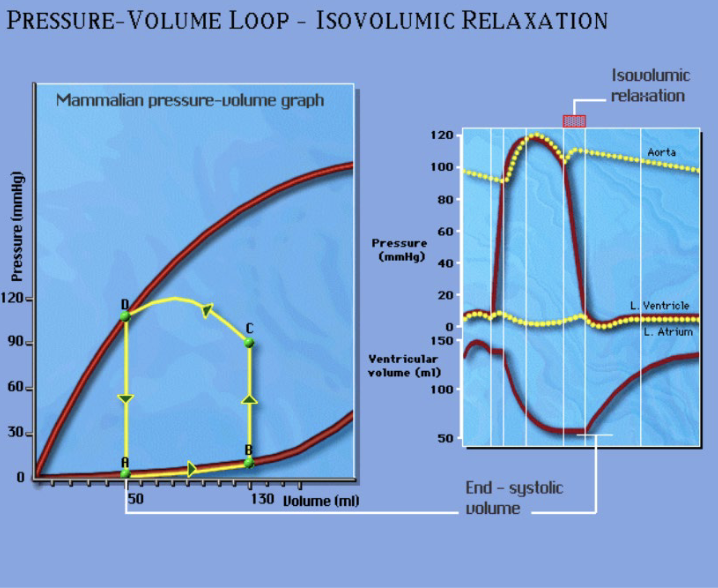
In this graph, describe what is happening from B —> C.
isovolumetric contraction: left ventricular pressure must overcome aortic pressure to initiate ejection
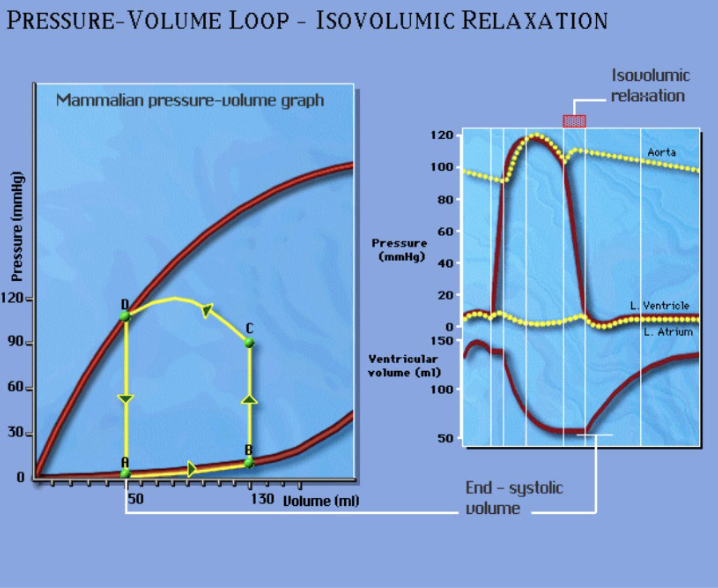
In this graph, describe what is happening from C—>D.
ejection phase; the curvature demonstrates a time-varying afterload highlight that this phase is auxotonic
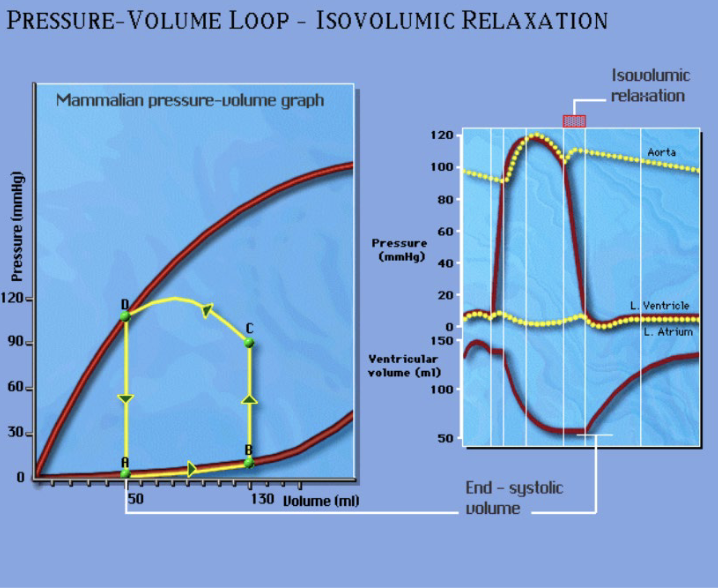
In the graph, describe what is happening from D—>A.
isovolumetric relaxation
point A = end systolic volume
What is the equation for cardiac output?
CO = HR x SV
Cardiac output is influenced by the amount of __ done by the heart.
work
The __ of the PV loop depicts the stroke work.
area
What is the equation for stroke work index?
stroke work/body surface area
The stroke work index reflects changes in: (5)
stroke volume, cardiac output, venous return, heart rate, blood pressure
What is the equation for cardiac index?
CO/body surface area
The Cardiac Cycle graph relates pressures in the __ atria, __ ventricle, and aorta to the __ ventricle volume, ECG, heart sounds, and valve function.
left; left; left
How does the cardiac cycle for the right ventricle and pulmonary artery compare to the cardiac cycle graph studied in the lecture?
it is analogous but at lower pressures
What are the intrinsic factors that affect cardiac output?
preload & starling pressure-volume relationship
What are the extrinsic factors that affect cardiac output?
contractility, afterload, chronotropic factors
Pacemaker cells spontaneously __ to initiate action potentials in __ & __ nodal cells.
depolarize; SA; AV
Describe the conduction pathway in the heart.
SA node initiates AP, which is detected by AV node —> passes to Bundle of His —> travels down and up the ventricles
Which cells are conducting cells?
Purkinje cells, Bundle of His
__ is the process in which the heart adjusts its heart rate to the body’s needs.
Chronotropic Regulation
When the SA node initiates a heart beat, __ modulates the rate of discharge.
chronotropic regulation
Chronotropic regulation is the primary __ factor utilized to modulate cardiac output.
extrinsic
In the parasympathetic nervous system, the NT __ is released and __ heart rate.
ACh, reduces
In the sympathetic nervous system, the NTs __ & __ are released, and they __ heart rate.
norepinephrine; epinephrine; increase
During sympathetic stimulation, depolarization is __, whereas during parasympathetic stimulation, depolarization is __.
faster; slower
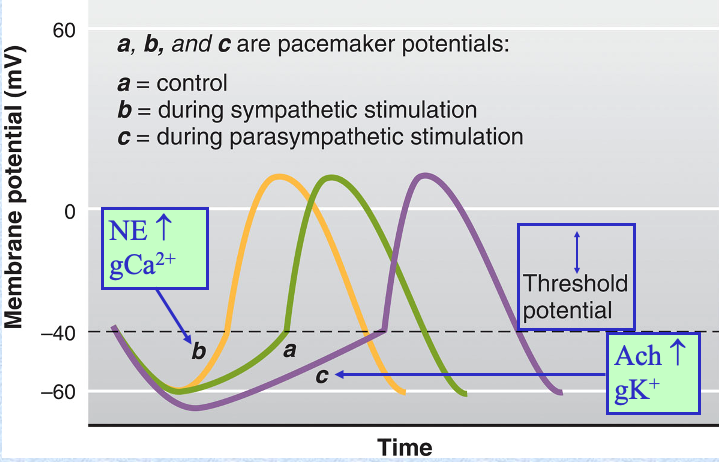
Chronotropic regulation depends on: (3)
activity of sympathetic nerves
plasma epinephrine (goes from blood vessels to ventricles)
activity of parasympathetic nerves
What are the 3 factors that modulate stroke volume?
preload, afterload, contractility
Increases in __ and __ increase the force of contraction by separate mechanisms, but both __ SV.
preload; contractility; increase
Increases in __ oppose contraction and thus __ SV.
afterload; reduces
End-diastolic ventricular volume is related to __.
preload
Increased venous return (refilling) increases __, which increases __.
EDV; preload
Stroke volume is the amount of blood __ from the ventricle each cardiac cycle.
ejected
How will a larger preload affect EDV, SV, stroke work?
it will give a larger EDV and thus a larger SV. Stroke work will also increase as a result.

How does a larger preload affect crossbridges? How does this affect cardiac output and end-systolic volume?
It allows more crossbridges to contribute to contraction. (preload is associated with how much the muscle is stretched, and when stretched, thick and thin filaments are closer together to enable more crossbridge attachment) Therefore, a larger contraction will allow for a larger stroke volume and thus cardiac output, bringing the end-systolic volume back to normal.
The Frank-Starling preload mechanism is important to prevent __.
overfilling in the heart
When the ventricle fills to a greater volume, the sarcomere length __. How does this affect the active force at the plateau and ultimately the Starling curve?
increases; it will elicit a greater active force at the plateau and move up the ascending limb of the Starling curve.
How does a stretched sarcomere allow for contraction? (4)
thick and thin filaments are closer together —> inc likelihood of crossbridge attachment
increased TnC Ca sensitivity with stretch
less double overlap of thin filaments
thick filaments are in a more relaxed state, where crossbridge and binding is more readily available (via titin and MyBP-C regulation)
__ is the force that opposes LV contraction and reduces stroke volume and the ejection of blood.
afterload
What is the systolic wall stress/arterial pressure during contraction?
afterload
An increased afterload __ the isovolumetric contraction phase and __ the time for ejection.
prolongs; reduces
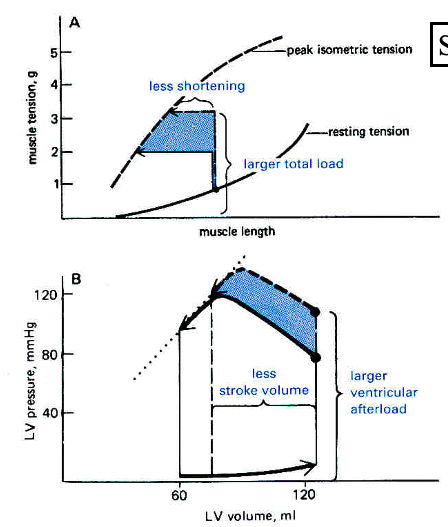
How does an afterload affect contraction and SV?
There is less shortening and reduced SV
this is because it takes longer to reach the ejection phase, as the ventricular pressure takes time to overcome the afterload/arterial pressure. this reduces the time for the ejection phase, reducing the SV.
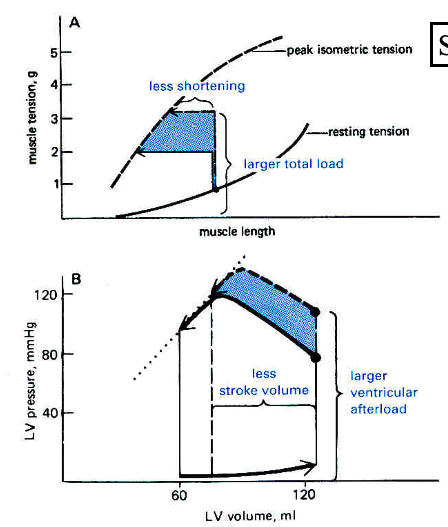
Work from __ is greater than work from SV.
pressure
LV pressure (afterload) is constantly changing during __.
ejection
The __ is a reasonable index of afterload during ejection.
MAP (mean arterial pressure)
Contractility is directly related to the amount of __ available to bind troponin and permit crossbridge binding.
Ca
Contractility is the extent to which __ are activated to generate force.
crossbridges
Contractility is independent of __ and initial __.
preload; afterload
__ stimulation increases contractility.
sympathetic
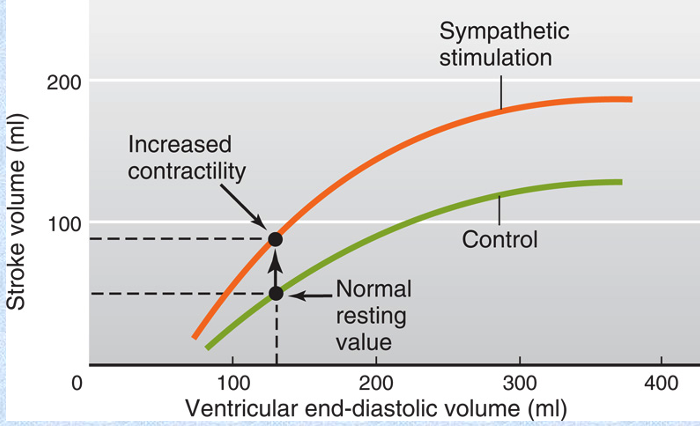
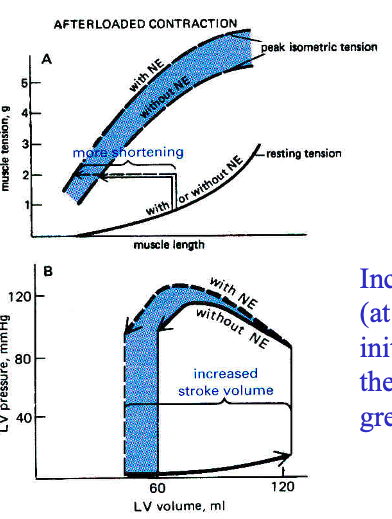
Increased contractility reduces the __, which allows for a greater __.
ESV; SV
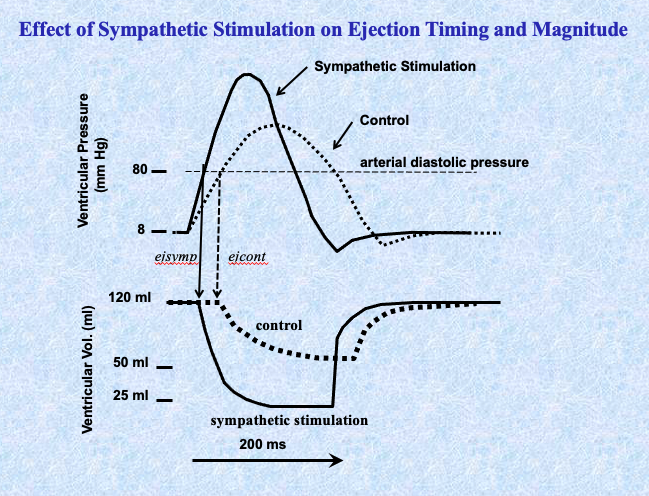
with sympathetic stimulation (like NE), there is an increase in pressure that ends at a lower ESV, allowing for a greater SV
Contractility is an __ mechanism that sends NT to increase CO to match the needs of the __.
extrinsic; peripheral organs
Norepinephrine and epinephrine bind to a GCPR that activates a cAMP that will trigger 5 reactions to increase contractility. What are these 5 reactions?
activates receptor that allows Ca into the cell (inc Ca)
binds to receptors on SR to allow Ca into cytosol (inc Ca)
enhances thin filament activation (binding of Ca to troponin)
enhances crossbridge cycling (faster crossbridge cycling)
binds to a receptor that will reuptake Ca into the SR to recycle Ca (steady flow of Ca available)
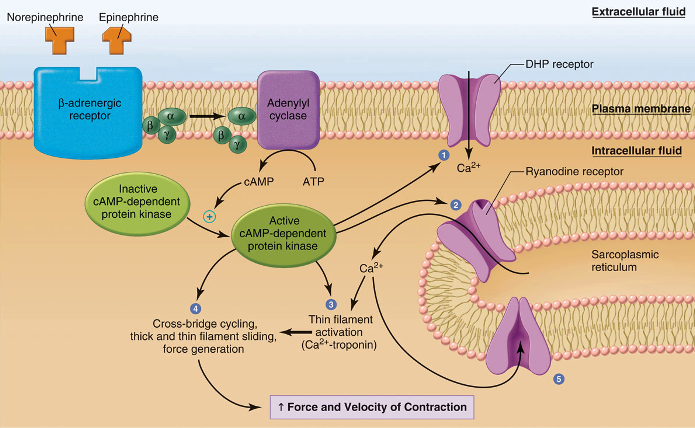
In increasing contractility, the __ is faster due to __ crossbridge cycling.
shortening velocity; faster
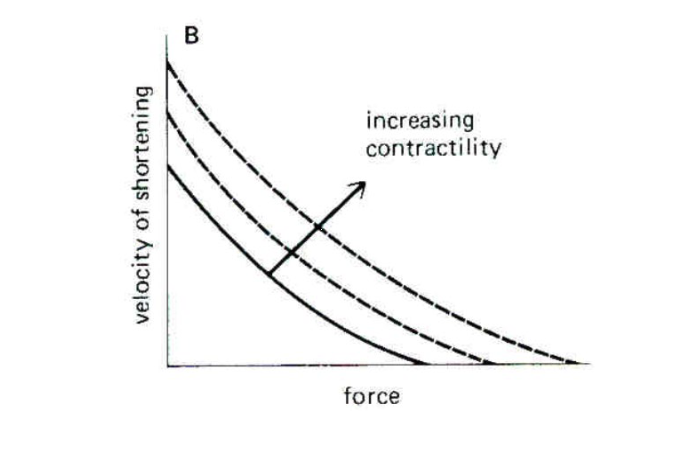
Enhanced Ca availability and binding to TnC gives a __ developed force during increasing contractility.
greater
What agents (like NE) that increase contractility called?
Positive Inotropic Agents
Increasing contractility will __ wall stress (pressure).
increase
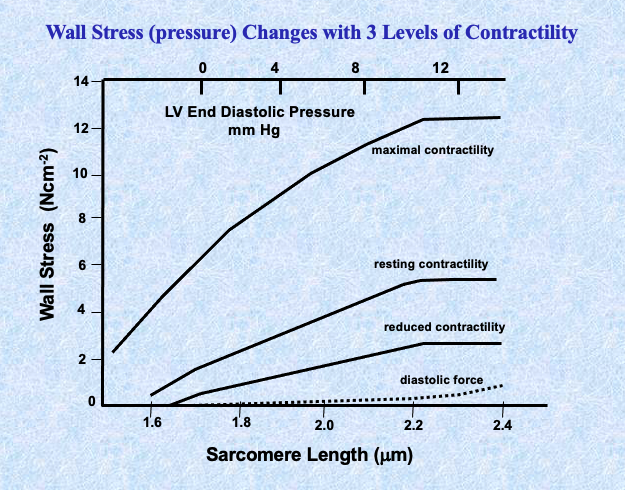
Sympathetic stimulation will __ shortening velocity, ventricular pressure, and SV.
increase
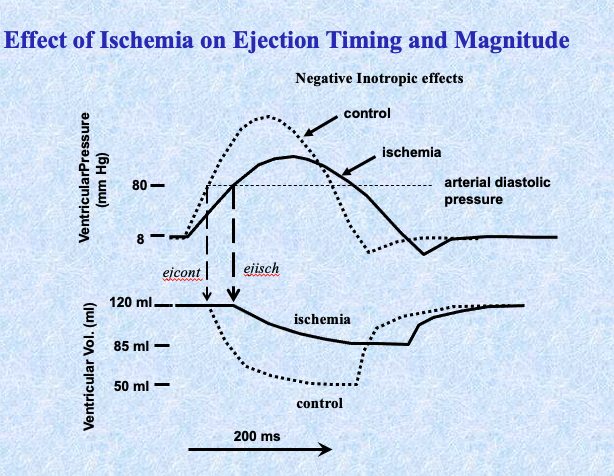
Ischemia will __ ventricular pressure, shortening velocity, and SV.
decrease
Contractility and the increased force of contraction due to preload and the Starling Relationship are __.
different mechanisms