VMP 420 Intro to antibiotics/immunology/vaccines ( may be on E1)
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
53 Terms
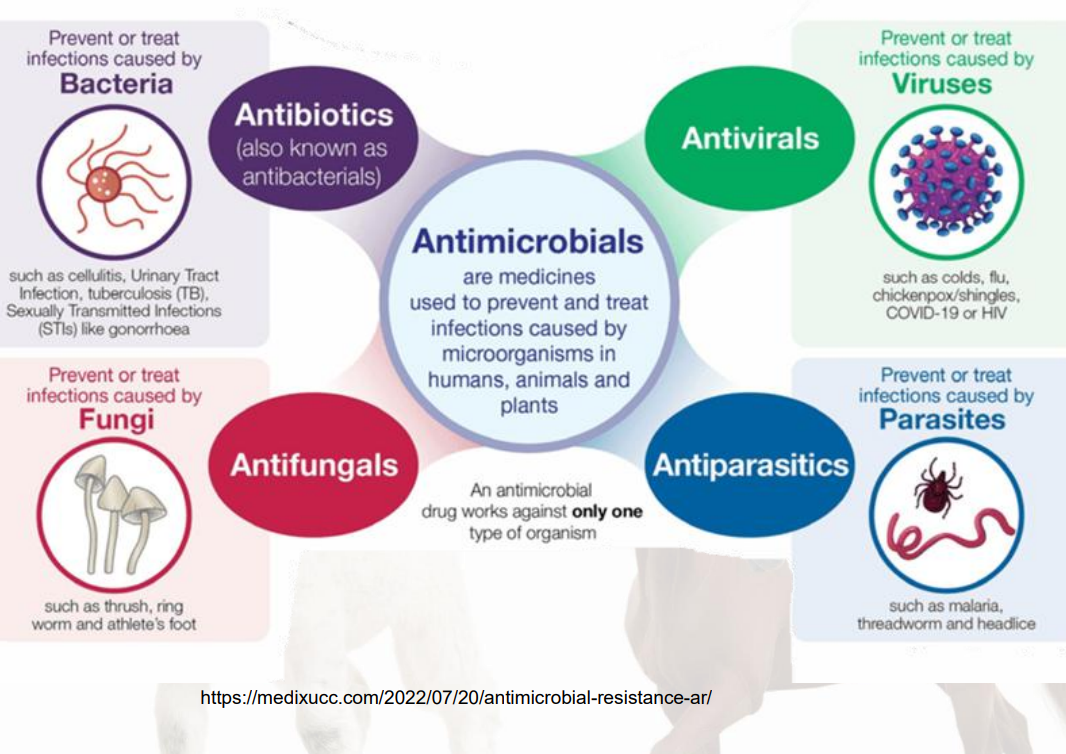
Antimicrobials
medicines used to prevent and treat infections caused by microorganisms in humans, animals and plants
Antimicrobial drugs works only against ONE type of organism
antibiotics( also known as antibacterials)
prevents/treats infections caused by bacteria ex: cellulitis, urinary tract infection, TB. STIs
antifungals
prevents/treats infections caused by fungi ex: thrush, ring worm, athletes foot
antivirals
prevent/treat infections caused by viruses ex: COVID, colds, flus, shingles/chickenpox
antiparasitic
prevent/treat infections caused by parasites ex: malaria, threadworm, and headlice
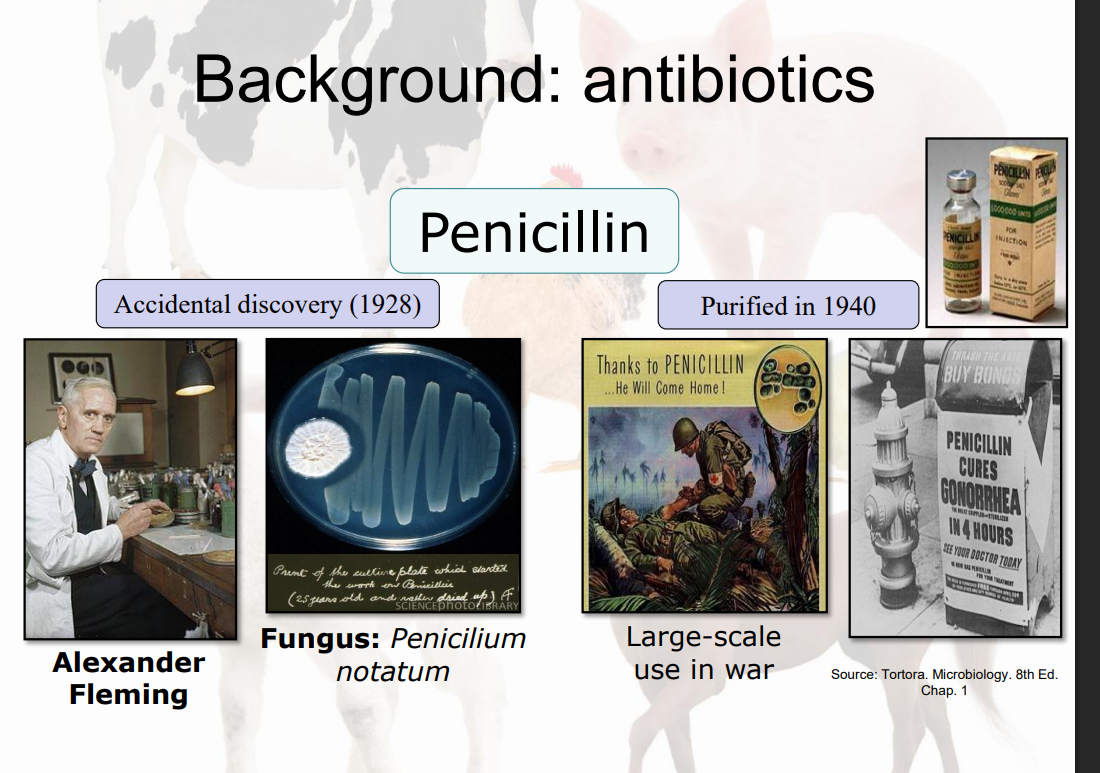
Quick history of antibiotics
6 Key Considerations in Antibiotics Use
Mechanism of action
Spectrum of activity
Dosage
Route of administration
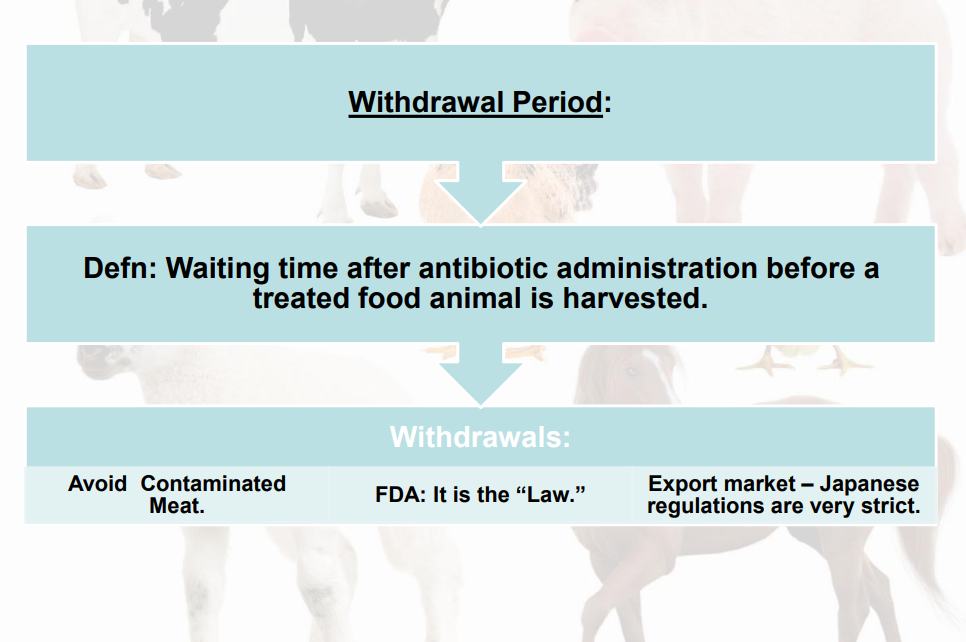
Meat quality
FDA legalities
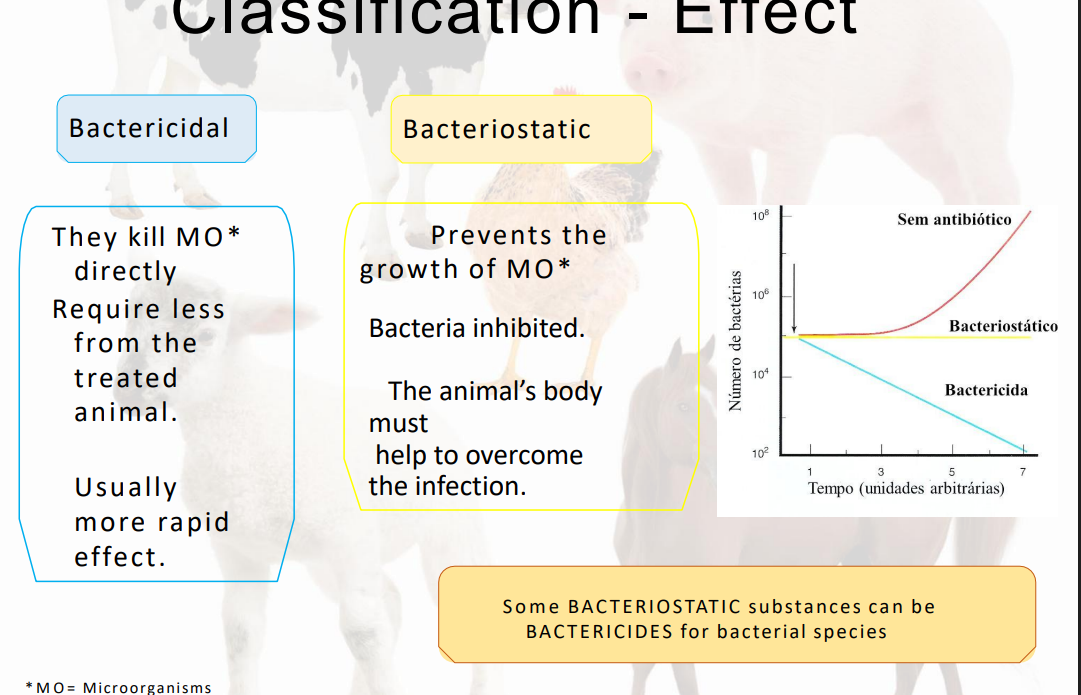
Classification-Effect
Bactericidal v bacteriostatic
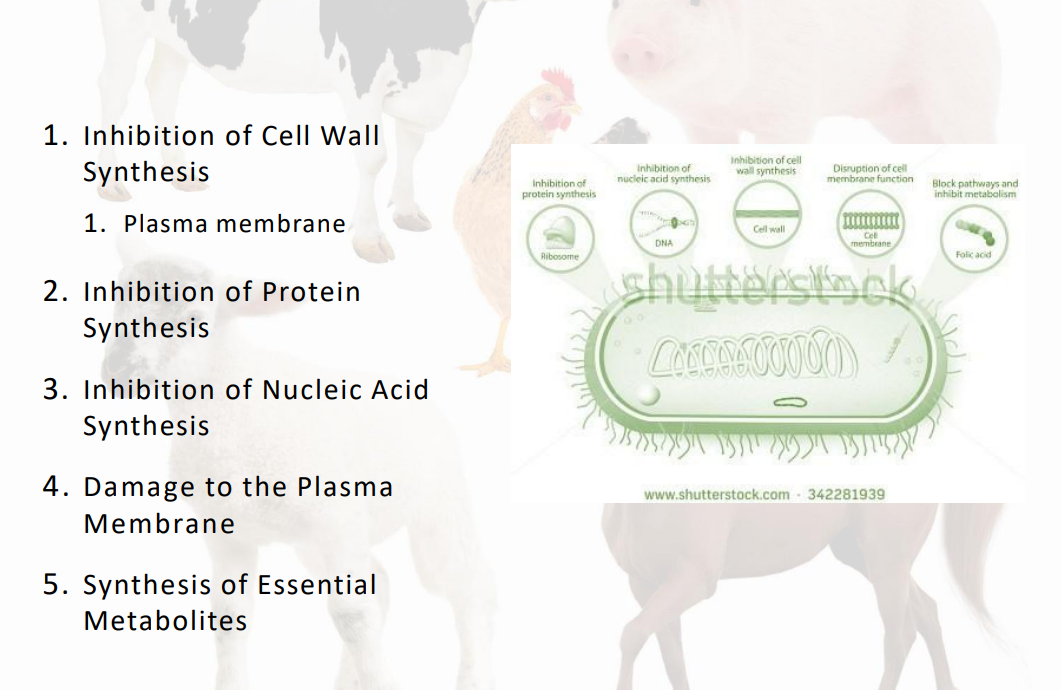
Mechanisms of action from antibiotics
inhibition of cell wall synthesis
inhibition of protein syn
inhibition of nucleic acid syn
damage to plasma membrane
synthesis of essential metabolites
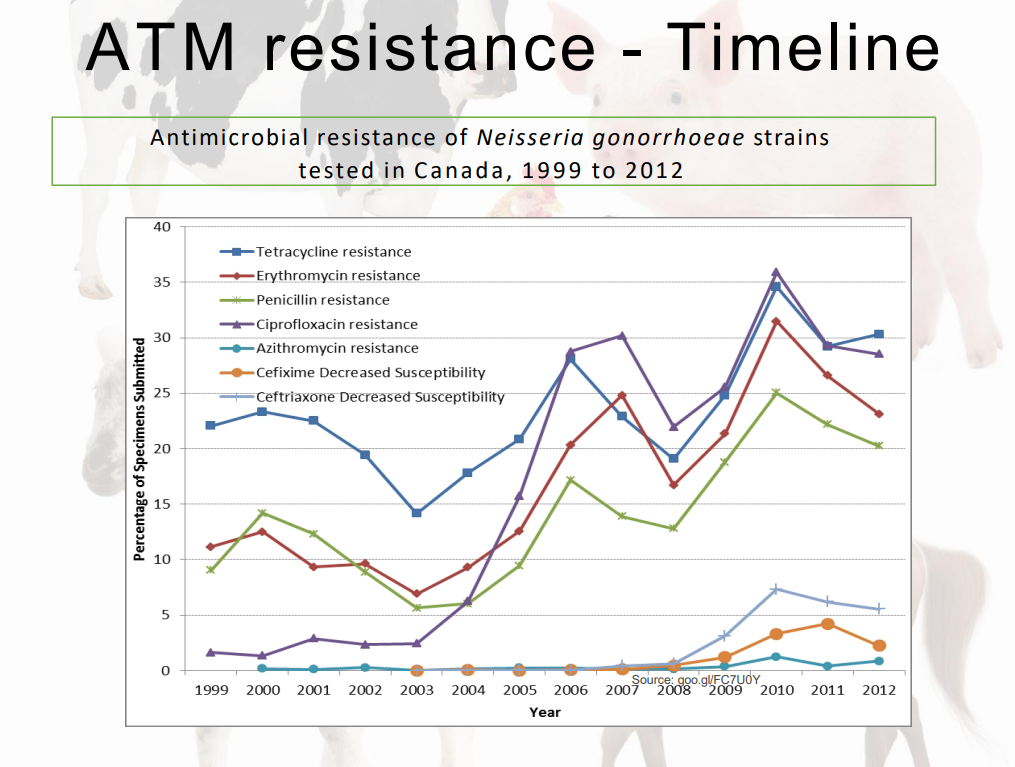
Antimicrobial Resistance
Specific bacteria have heritable traits that interfere with the mechanism of action of an antibiotic and render it ineffective.
AMR (antimicrobial resistance) - social and political issue.
What is resistance?
Parameter defined based on laboratory concepts.
In vitro X In vitro
MIC (Minimum Inhibitory Concentration) and MBC (Minimum Bactericidal Concentration)
Determining factors
ATB concentration at the infection site
Pharmacokinetics: Absorption, distribution, biotransformation and excretion •
Pharmacodynamics: concentration drug X antimicrobial activity
Host's own contribution against MOs
Time to start therapy
Choosing an Antibiotic Treatment
Susceptibility versus Resistance
Immediate assumption:
specific bacteria are susceptible
Lab confirmation in > 2 days:
Identify bacteria and sensitivity tested to multiple antibiotics
Spectrum of Activity
Broad Spectrum Antibiotic:
Few bacterial types can resist the antibiotic.
Broad Spectrum Antibiotics are usually more reliable when:
Resistance pattern unknown
Infection by multiple types of bacteria
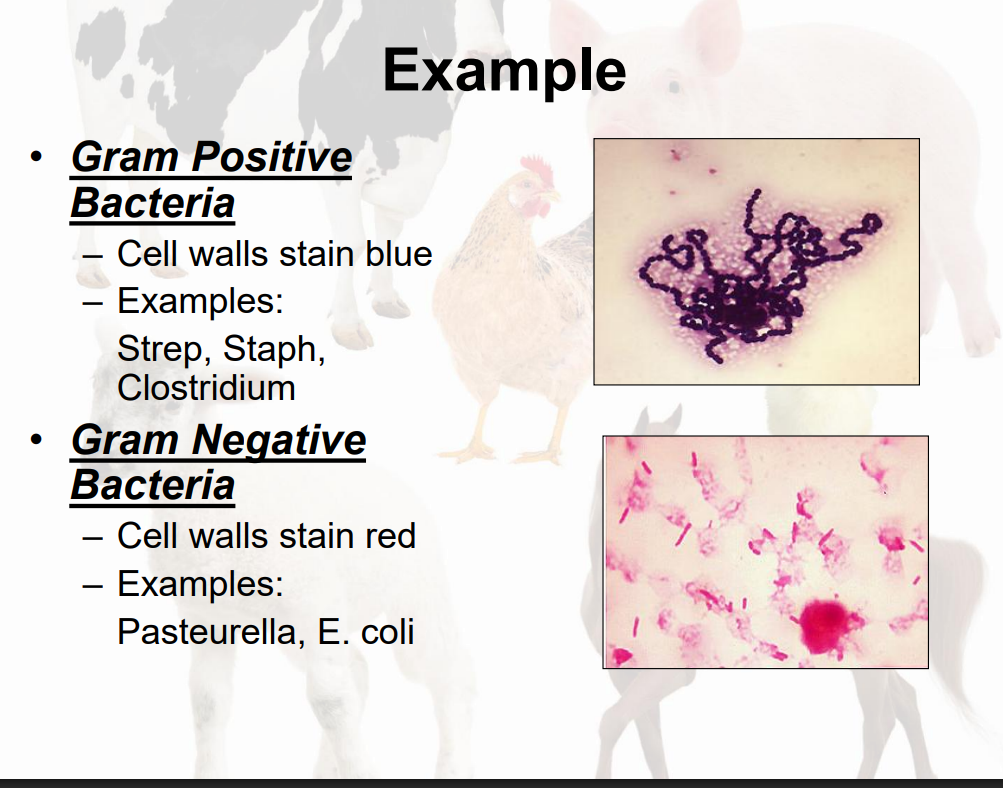
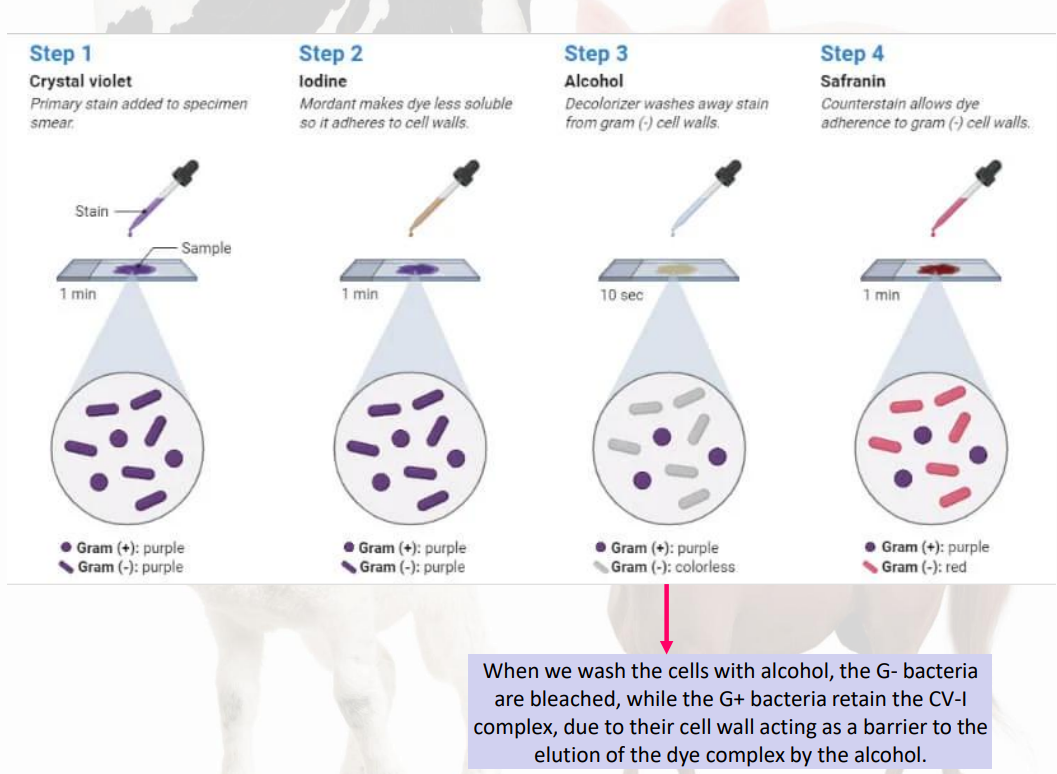
how to stain gran - / gram +
crystal violet
iodine
alcohol
safranin
Some antibiotics primarily affect gram positive bacteria
ex:
penicillin
tylosin
Some antibiotics primarily affect gram negative bacteria
ex:
gentamicin
neomycin
Some antibiotics affect gram - and gram +
ex: ceftiofur, tetracycline
Response: More reliable when bacterial type and resistance pattern is unknown.
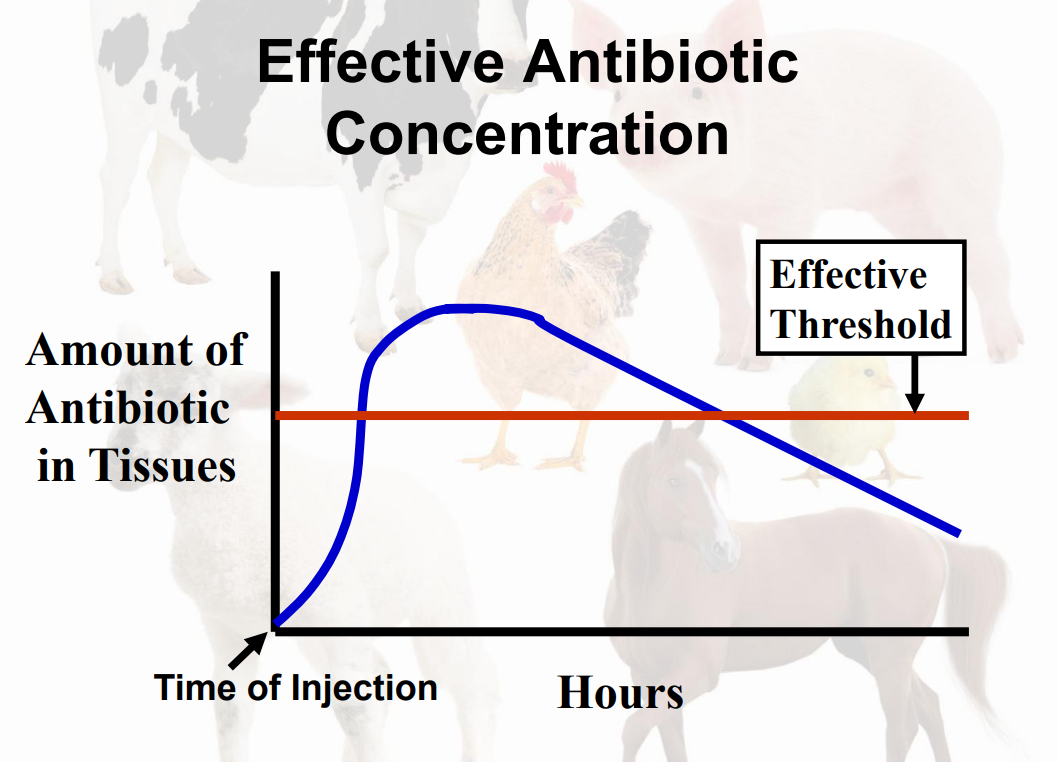
Dosage
Level of the Antibiotic Administered to Animals
How much (mg/lb, iu/lb, ml/lb)
How often (# doses/day)
How long (# days)
Route of administration (oral, subcutaneous, intramuscular, intravenous)
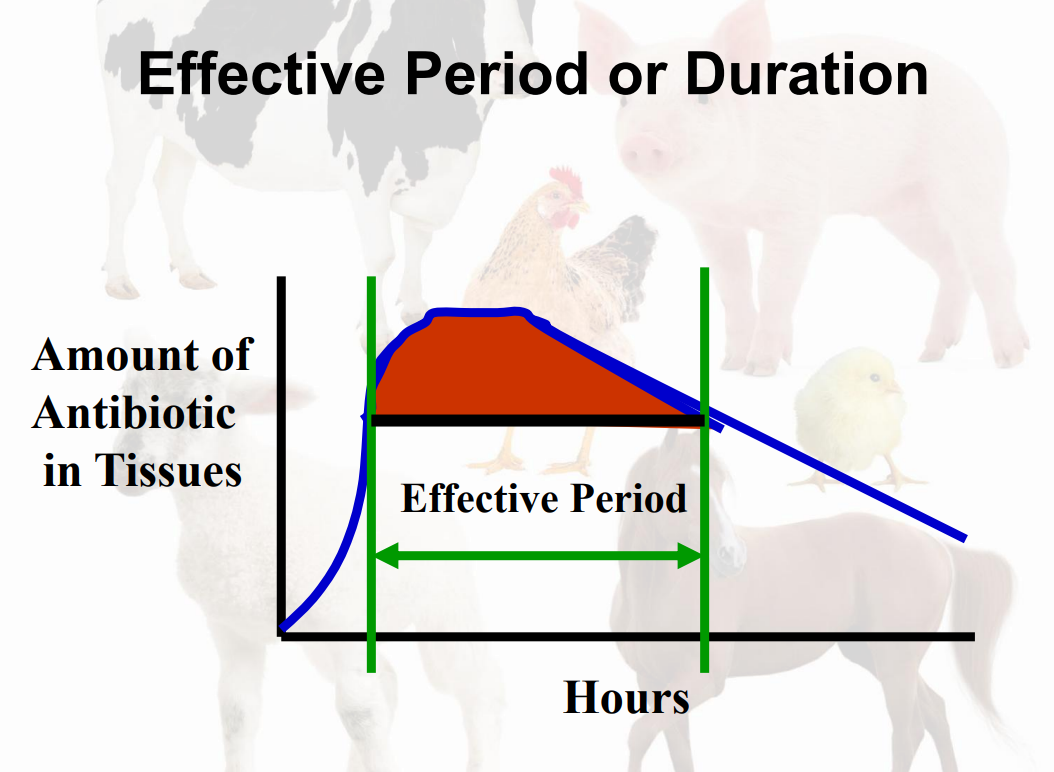
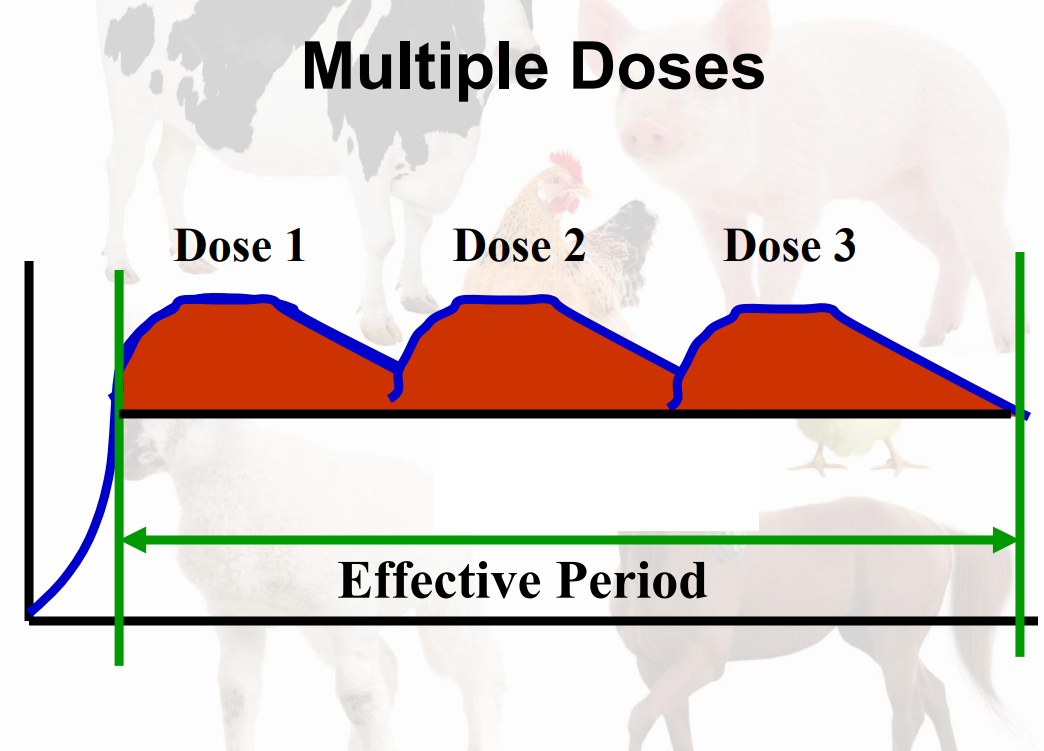
multiple doses effective period
long-acting antibiotics
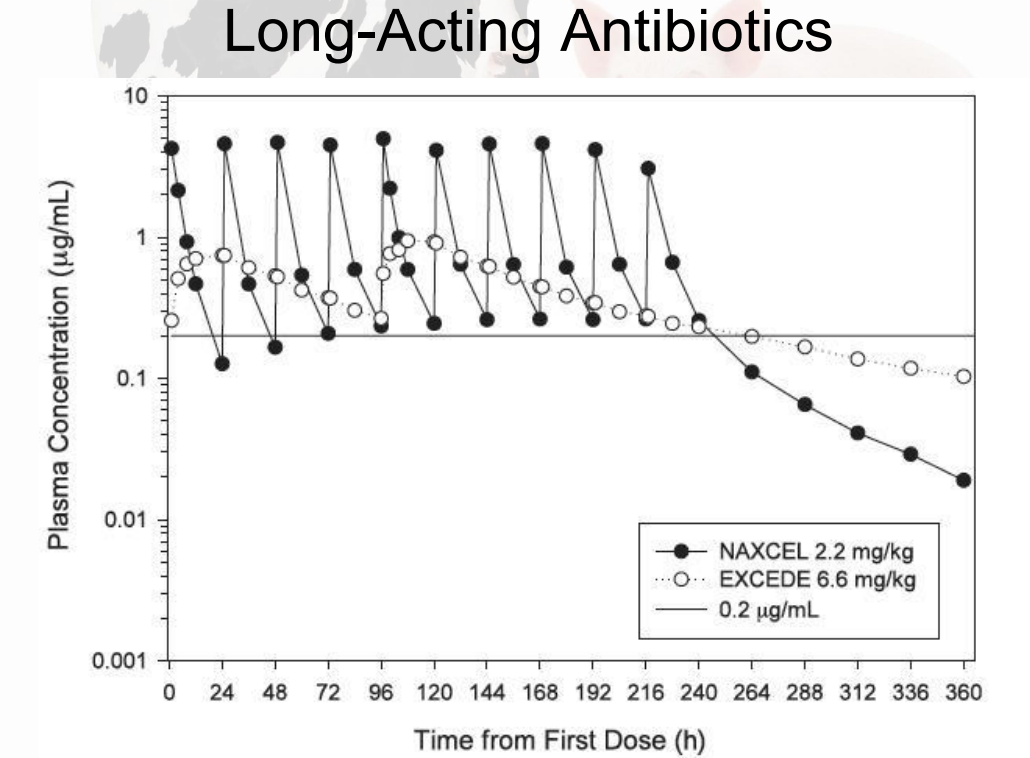
Dosage Requirements
Adequate Dose(s) Given
Doses Repeated Steadily
Adequate Duration
–Until Response: 5 Days - 2 Weeks
Absolute Minimum: 3 Days
Consider long-acting antibiotics.
Recurrence: Drastic Condition
Route of Administration
Topical Administration
Direct Application to Skin
Many daily applications
Individually contained animals: dairy cows, horse
Production Animals:
Unimportant route for most antibiotics
Parenteral Injection (Infuse into tissue via a needle)
Intramuscular (IM)
Anatomical site is species specific.
Needle size – age, species, product specific
Intravenous (IV) – Typically jugular vein.
Subcutaneous (SQ)
Less Common:
intrarticular, intraperitioneal
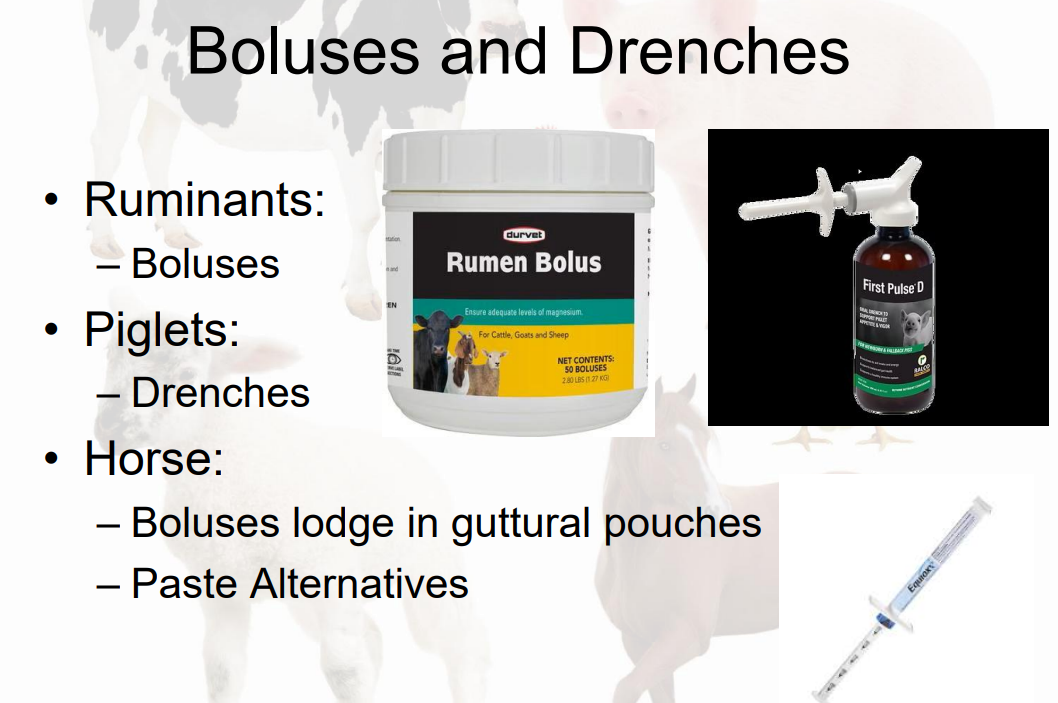
Oral Administration
Antibiotic Given Into the Mouth:
Treatment of individual animals
✓ Boluses (Large Pills)
✓ Drenches and Pumps
✓ Paste Syringes
Group Treatment of Animals:
Common:
✓ 65% of antibiotic expenditure
Methods: ✓ Water ✓ Feed
Boluses and Drenches
Group: Water Medication

Group: Feed Medication
medication put in groups feed
Regulations – Veterinary Feed Directive [VFD]
Advantages of group treatment over parenteral injections
Large Animals:
Difficult to restrain
reduced stress of administration
less labor
may be thousands to treat-population vs individuals
Advantages of parenteral injections over group treatment
Oral: Longer time to reach treatment level in tissues
Oral: Sick animals do not eat and drink well
Group Oral: Costly - every animal is treated
Antibiotics Absorbed After Oral Administration
Oral antibiotics must be absorbed by the gut in order to reach the lungs and other organs
Not Absorbed: Neomycin, Gentamycin, Spectinomycin
Antibiotic Characteristics For Water Medication
Water Soluble Antibiotics: Evenly disperse in water for accurate dosing
Suspensions: Treatment mixture must be stirred
Palatability: Imperative that animals continue to drink.
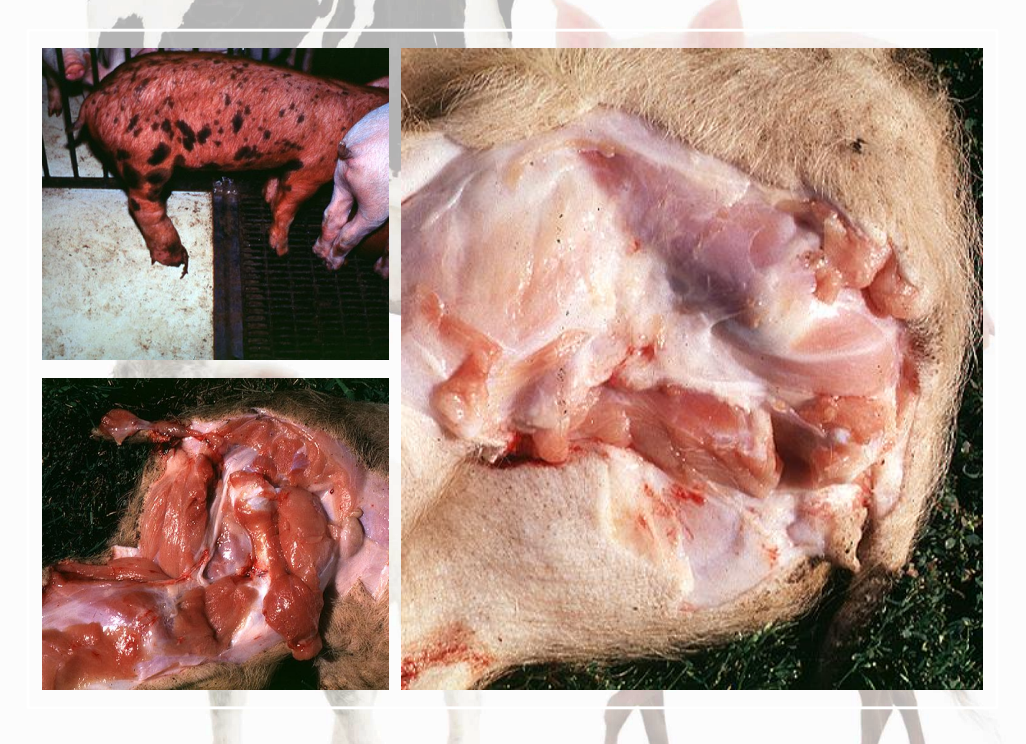
Injection Site Damage
Meat: Injection Site Blemishes
Animals: Blemishes are related to discomfort.
Parenteral Carriers: Injectable Solvents
Aqueous Carriers:
Antibiotics that are water soluble or suspend in water.
Soluble: Clear Solution
Suspension: Precipitate
Oil Carriers:
Polypropylene Glycol (PPG)
Carrier Irritation
Aqueous - Little tissue irritation.
PPG Carriers - Very Irritating
Painful at injection site
swollen tissue
complication= abscess =/- scar
ex in pic pigs lost sciatic nerve due to damage from injection to sciatic nerve
Reducing Injection Site Irritation
Limit volume injected.
Base volume on animal size and caustic property of product.
Cattle (>500#)- 10 ml per site
Hogs (100#-250#)- 5 ml per site
Consider SubQ route.
cattle and other ruminants
use subq route if label directions advise

Reasons for Antibiotic Failure
Misdiagnosis: viral, animal flow, environmental, nutritional, PPM
Improper Dosing: Bacteria resistant to selected antibiotic
Irreversible Damage: too late, impossible
Residue Avoidance
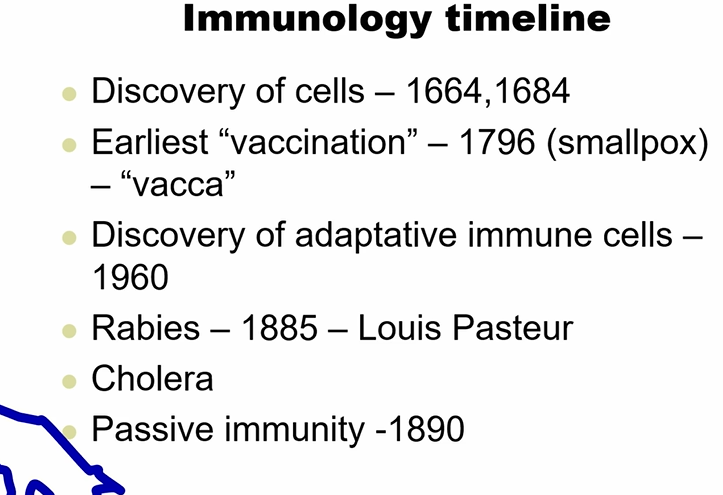
Immunology timeline
Concepts
Immunity •
Ability to resist infection.
Immunology
Study of all aspects of host defense against infection and of the adverse consequences of the immune response.
⚫ Pathogen
Microorganisms that can cause disease when they infect a host.
⚫ Antigen/Immunogens •
Recognized by the body as non-self and stimulates an acquired immune response.
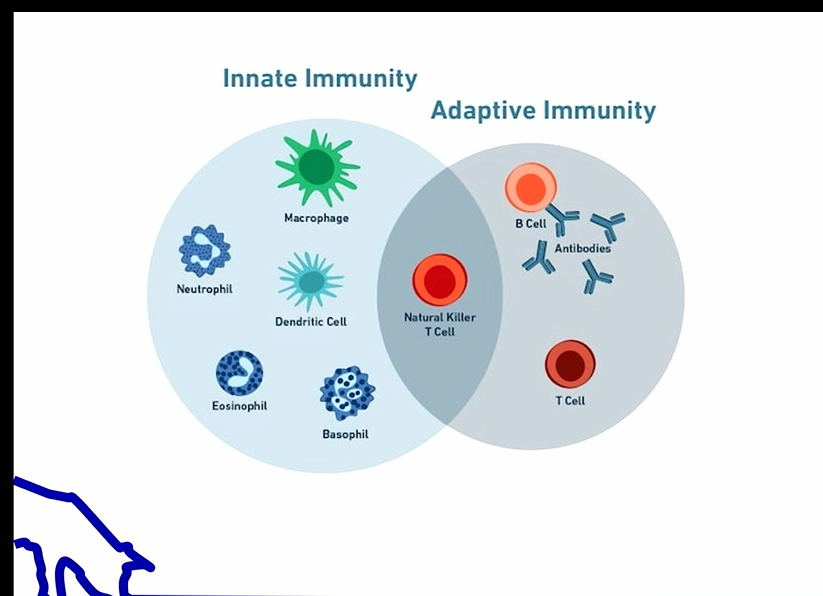
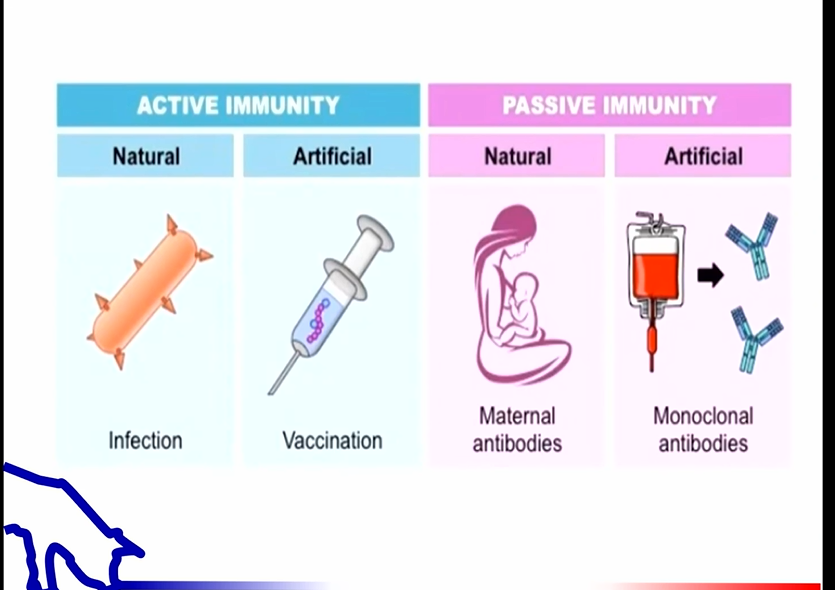
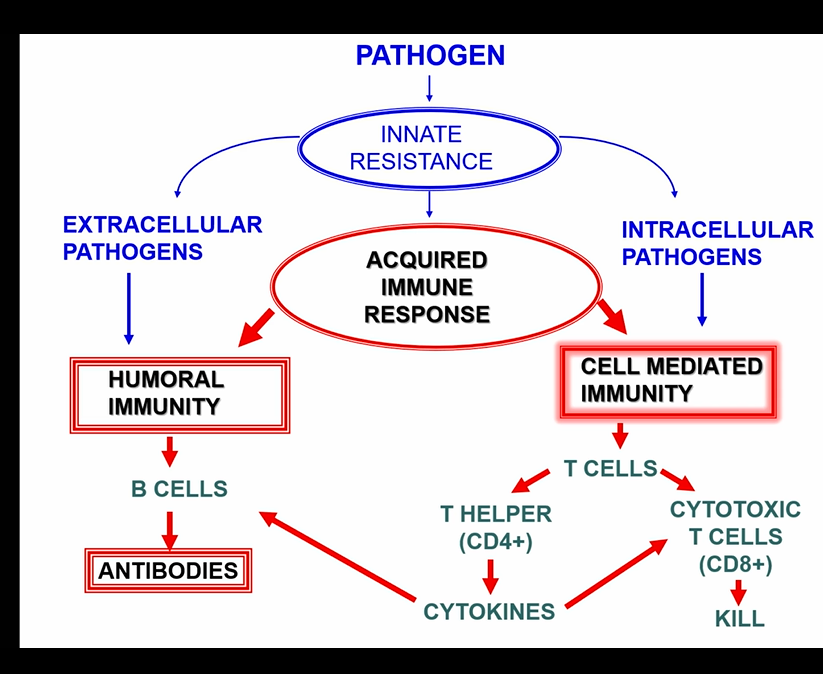
types of immunity
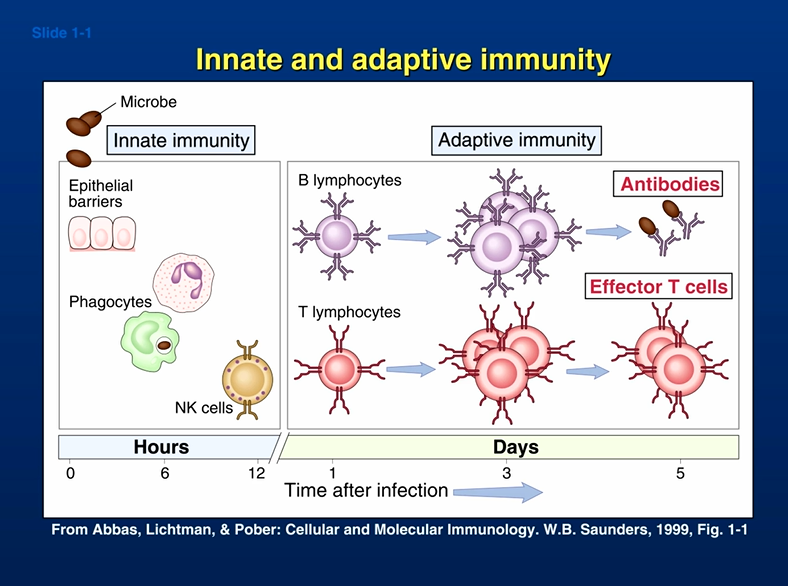
innate immunity
acquired (adaptive) immunity
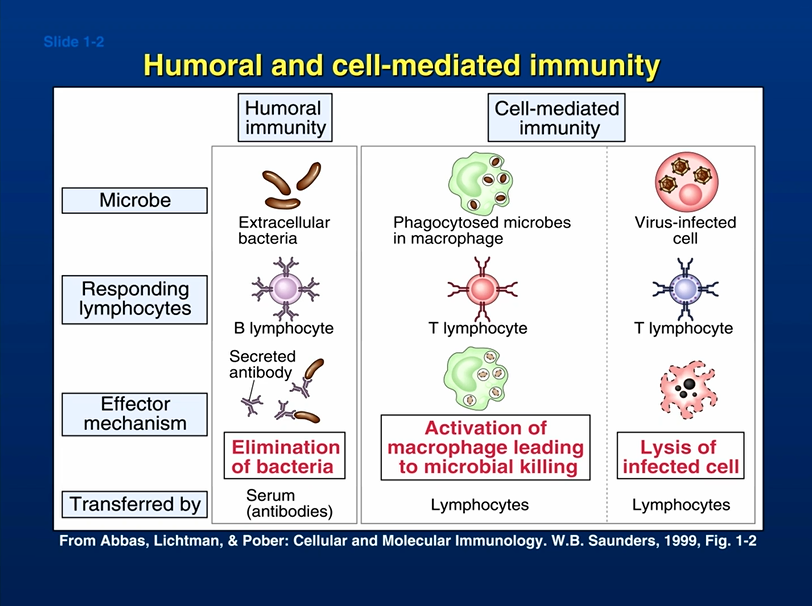
humoral immunity
cell-mediated immunity
naturally acquired immunity
artificially acquired immunity
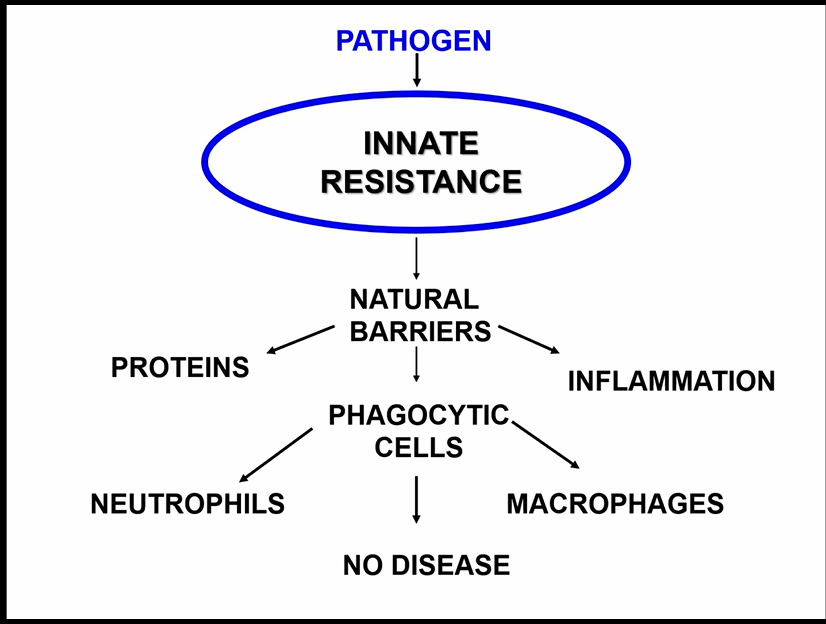
innate immunity
antigen-nonspecific defense mechanisms
very rapid response to almost any antigen
born w it
initial response to eliminate microbes and prevent infection
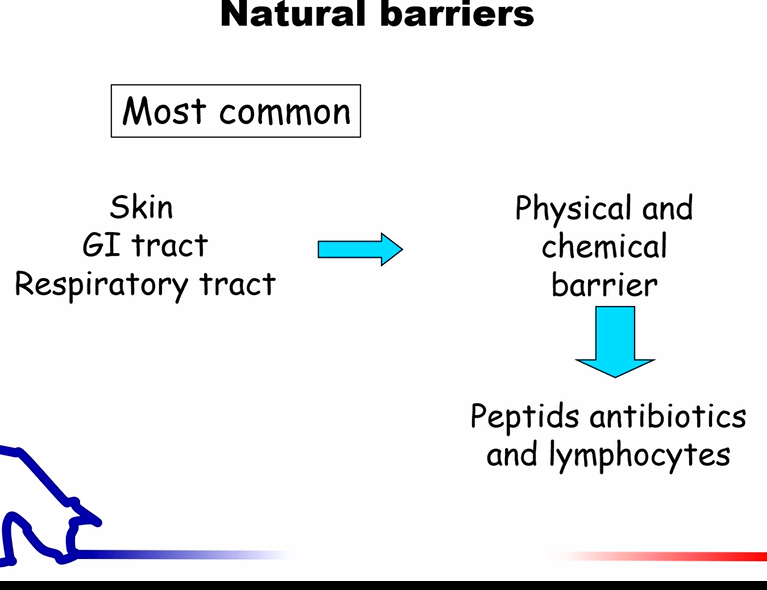
examples: anatomical barriers (skin), mechanical removal (saliva, mucus), antigen-nonspecific defense chemicals
acquired immunity
antigen-specific
takes several days to become protective
develops through life
reacts w and removes specific antigen
natural barriers
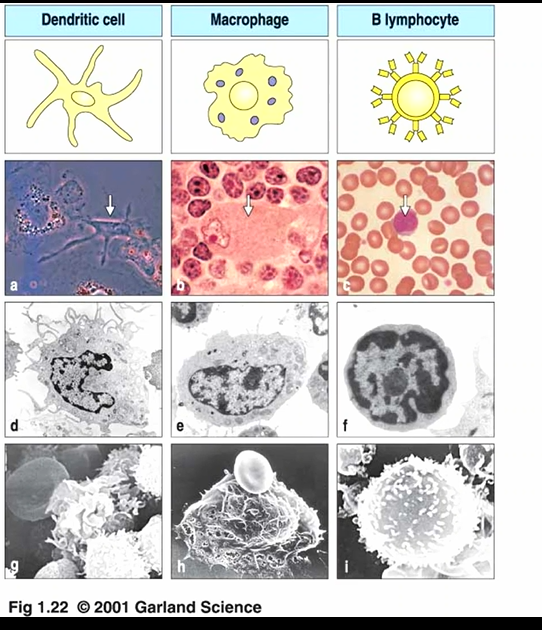
APCs (antigen-presenting cells)
dendrit cells
macrophages
B cells
2 types of acquired immunity
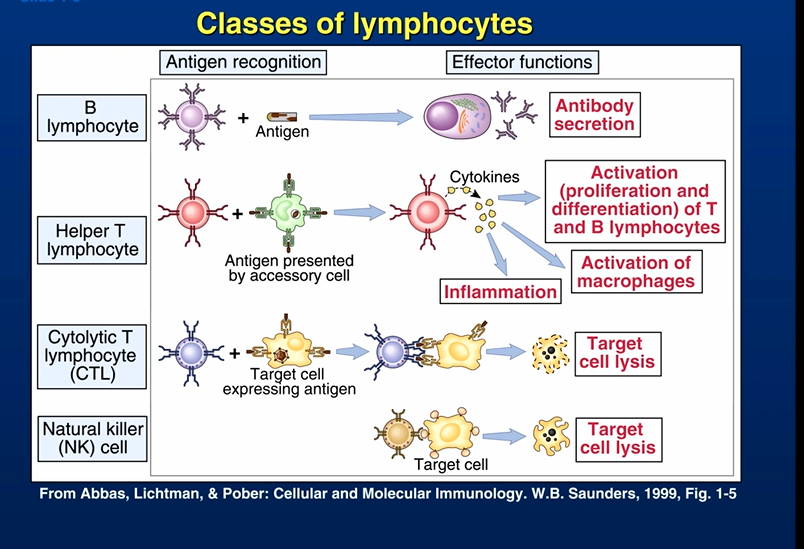
humoral immunity
involves production of antibody molecules in response to an antigen and is mediated by B-lymphocytes
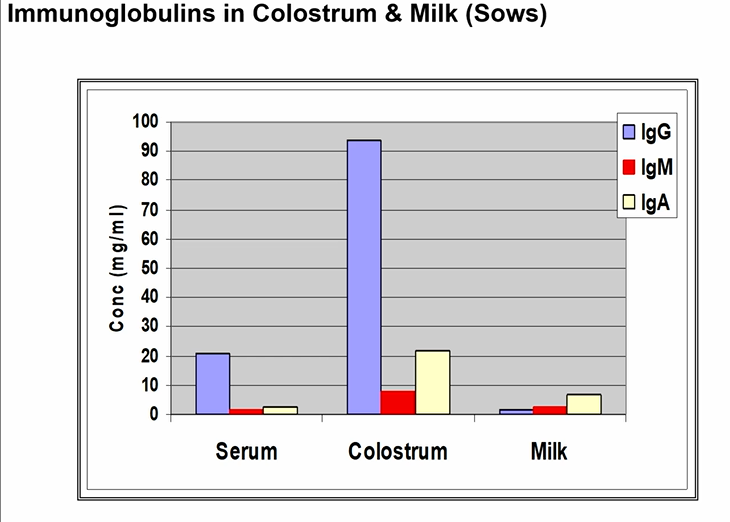
antibodies or immunoglobins are produced by B-lymphocytes and plasma cells in response to specific antigen
antibodies circulate in blood and enter tissue via inflammation
effective against bacteria, bacterial toxins, and viruses prior to these agents entering cells
there are 5 classes antibodies: IgG, IgM, IgA, IgD, and IgE
cell-mediated immunity
involves production of cytotoxic T-lymphocytes, activated macrophages, activated NK cells, and cytokines in response to an antigen and is mediated by T-lymphocytes
2 types of naturally acquired immunities
ACTIVE naturally acquired immunity
natural exposure to an infectious agent or other antigen
body responds by making its own antibodies
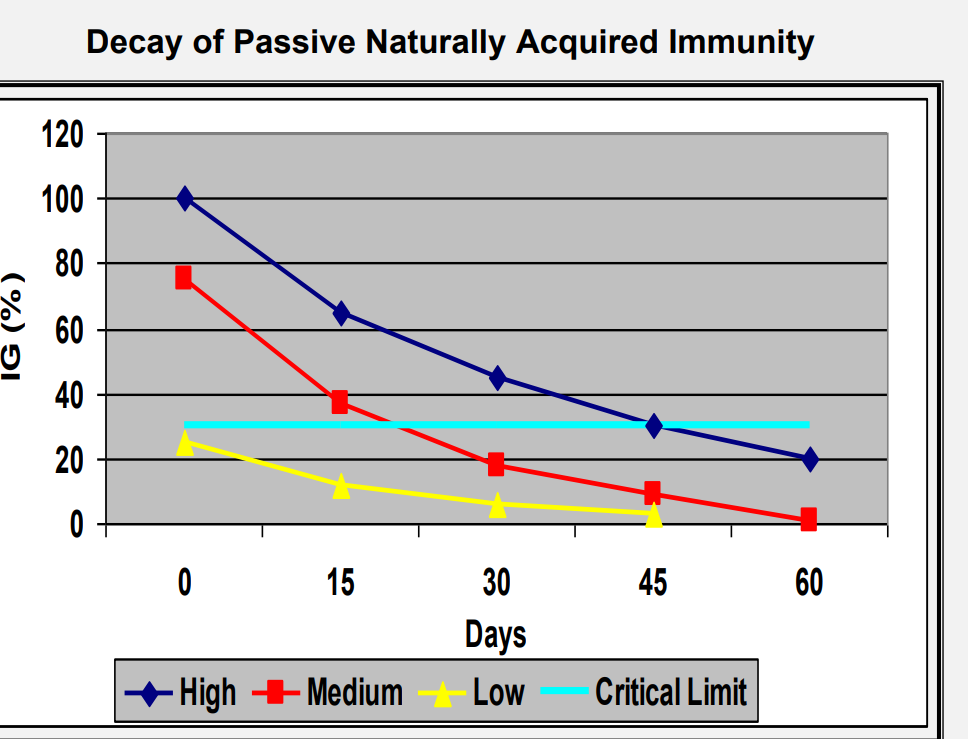
PASSIVE naturally acquired immunity
ex: placental transfer of antibodies from mother to fetus during pregnancy
antibodies( IgA, IgG) found in colostrum and milk
ACTIVE ARTIFICIALLY acquired immunity
Any immunization with an antigen.
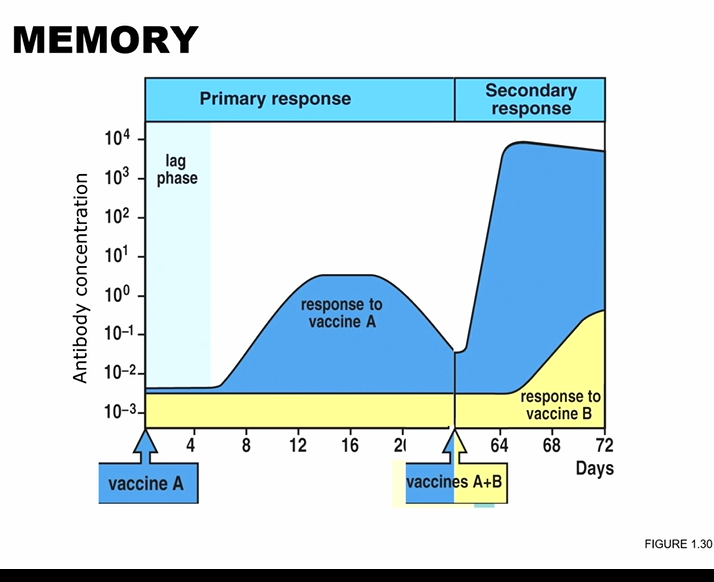
The body will produce its own ANTIBODIES and develop circulating, long-lived B-memory cells.
If the body is again exposed to that same antigen, the memory cells will cause immediate and rapid production of the appropriate antibodies for protection.
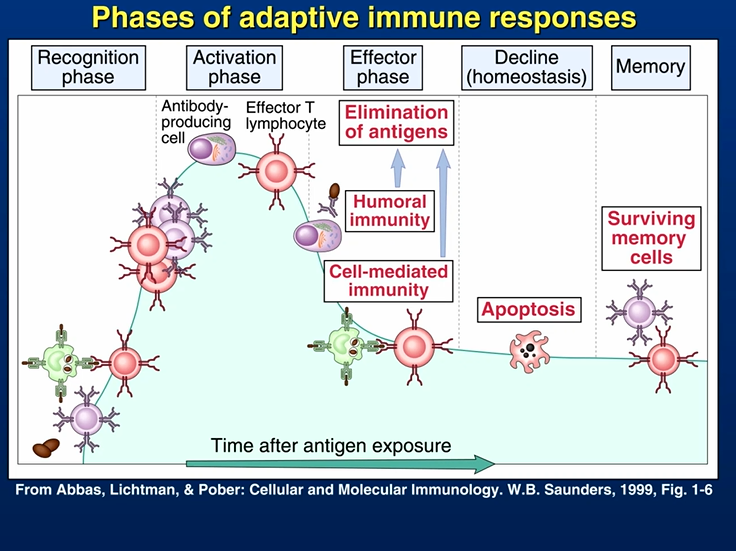
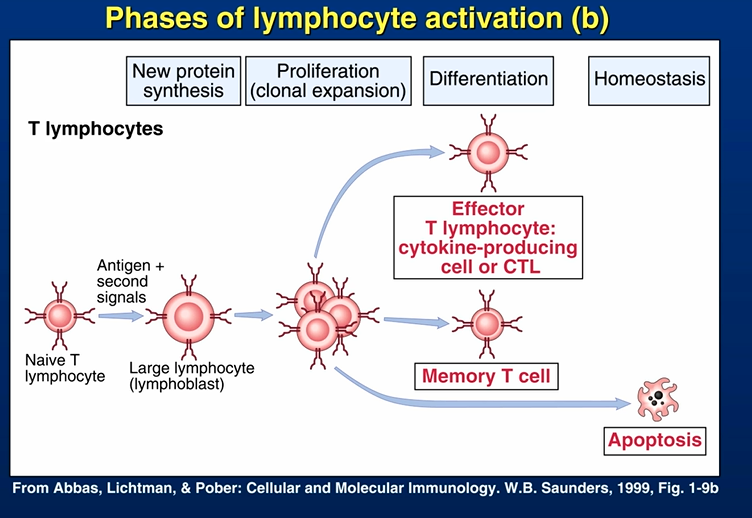
phases of adaptive immune responses
classes of lymphocytes
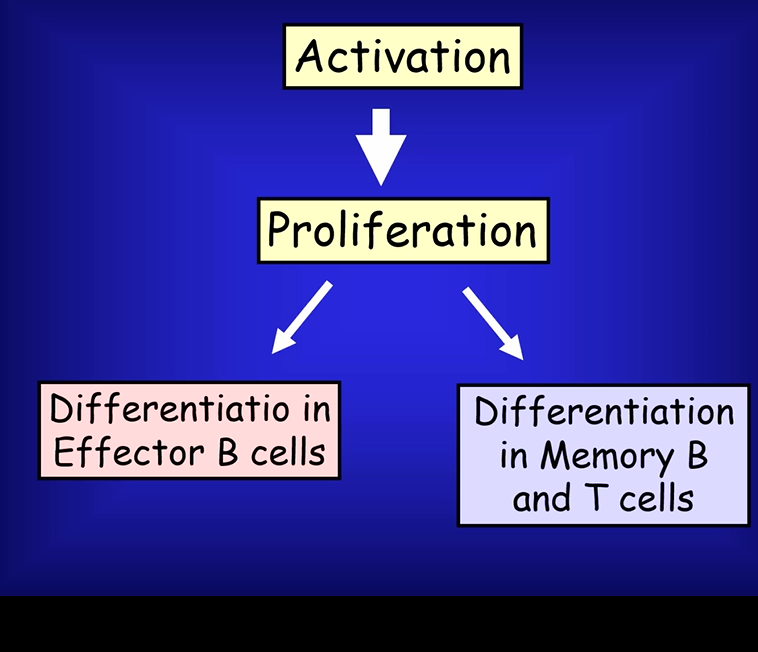
pathways
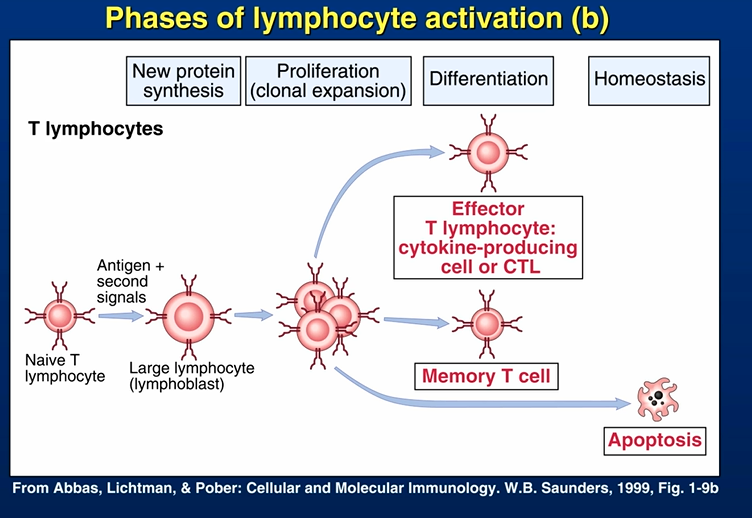
phases of lymphocyte activation (a)
phases of lymphocyte activation (b)
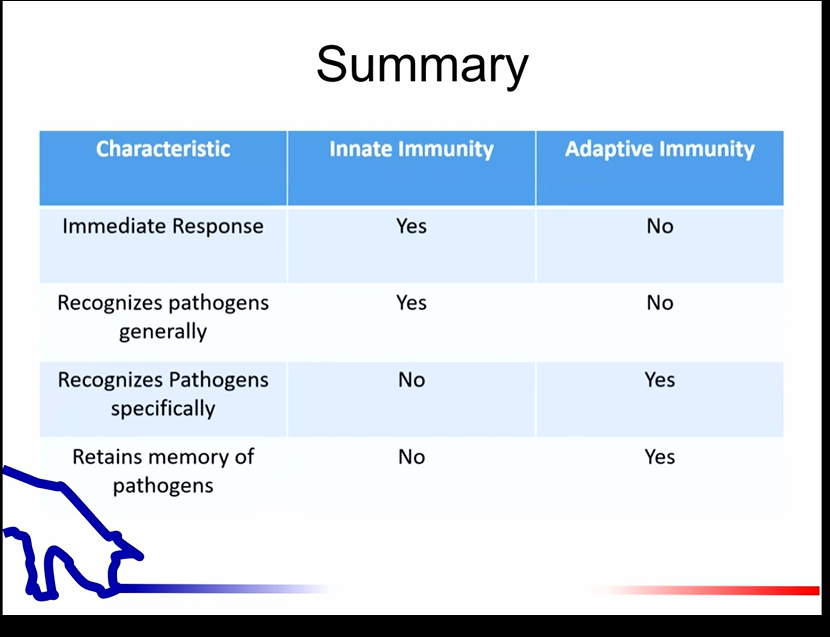
summary of innate vs adaptive
vaccination
not treatment for disease it is to PREVENT
why important?
protects individuals/ animals- effective
eradication
clinical signs/ shedding
important Concepts
ACTIVE IMMUNITY IS NOT ABSOLUTE
animal can become diseases
high levels of virus/bacteria
animal in poor health/condition
stressful environment
animal can still become infected
may not show disease
Passive immunity can block active immunity
types of vaccines- VIRUSES
live viruses
rarely used
feedback programs in pigs
modified live viruses
common, PRRSV in pigs, IBR in cattle
can be pathogenic to fetuses, sick animals, or other species
types of vaccines- bacteria
modified live bacteria
becoming more common
salmonella, erysipelas, ileitis in pigs
caution: do not use antibiotics at time of vaccination
killed
safety improved over modified live
immunity may be incomplete
types of vaccines-others
toxoids
inactivated toxins
animal produces antibpody response
ex: tetanus toxoid in horses, clostridial toxoids for sheep and pigs
antisera
antibodies in serum from another animal
does not stimulate active immunity
ex: tetaus antitoxin
new genetically engineered vaccines
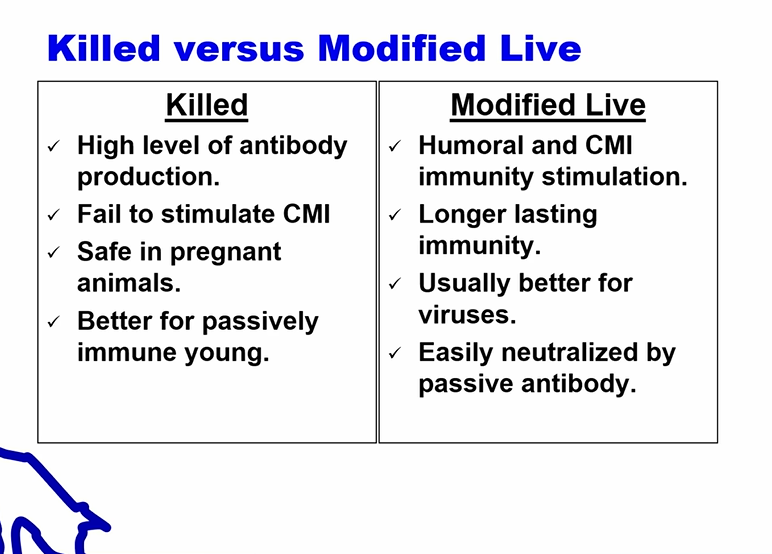
killed vs modified live
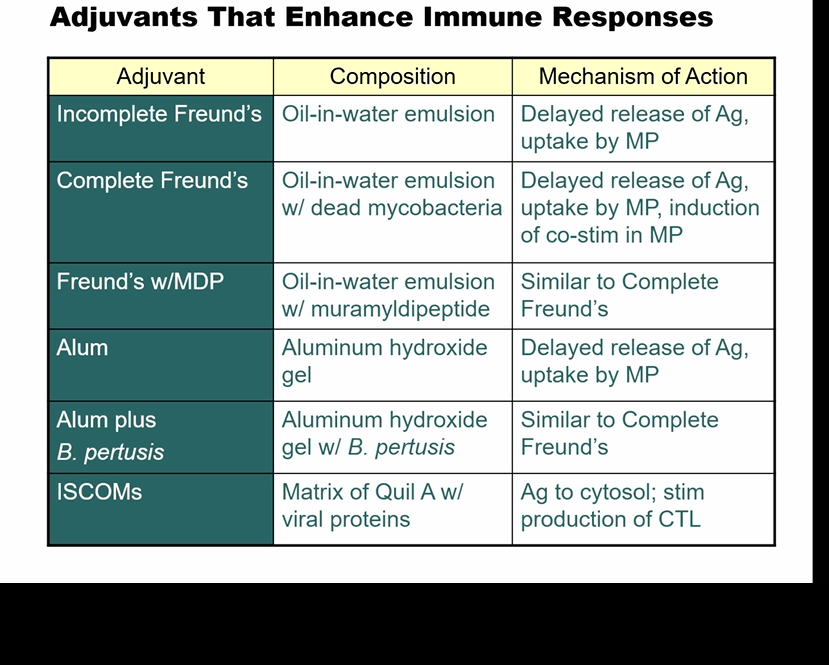
adjuvants that enhance immune responses
handling vaccines
remember- made from living organisms
keep in fridge (unless instructed otherwise)
opened bottles of killed virus/bacteria can be stored and reused
opened bottles of MLV or bacteria should be discarded
keep vaccines away from heat and sunlight
do not mix vaccines in same syringe
formalin in bacterins will kill MLV
caution: disinfectants for cleaning syringes will kill MLV vaccines
use appropriate routes of administration- IM vs SubQ vs oral
use appropriate needle length