Inflammation, Macrophages, & Neutrophils
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
107 Terms
Inflammation
A concerted action between various mediators, inflammatory enzymes and vascular response mechanisms
Defensive cells
Once sentinel cells recognize invaders, signals are generated that activate and attract ____ cells to the site of invasion
Dendritic cells, mast cells, eosinophils, neutrophils, macrophages and lymphocytes
Cell types involved in inflammation
Innate immunity
Type of immunity where there are molecules and cells that distinguish host from infectious agents by recognizing conserved motifs
Adaptive immunity
Type of immunity where there are cells with exquisitely specific receptors for a potentially unlimited number of targets
Macrophages, neutrophils and dendritic cells
Which cells are known as the phagocytes of innate immunity?
Eosinophils, basophils, mast cells and natural killer cells
Which cells are known as the granulocytes of innate immunity?
B and T cells
Adaptive immunity cell types
Damage associated molecular patterns; these are used internally to recognize invaders
What does DAMPS stand for and what do they do?
Pathogen associated molecular patterns; these are used externally to recognize microbial invaders
What does PAMPS stand for and what do they do?
-Immunological reactions
-Nutritional imbalances
-Genetic defects
-Hypoxia
-Microorganisms
-Chemical agents
-Physical agents
What are some things that DAMPS are involved in?
T
T/F - All PAMPS are DAMPS but not all DAMPS are PAMPS
F; they are essential to survival of the microorganism though
T/F - PAMPS are found on normal host animal tissue
Nonspecific (these receptors are called Toll-like receptors)
Are PAMPS receptors specific or nonspecific?
T; this ensures that the correct response is elicited to fight that pathogen
T/F - Stimulation and triggering of different TLRs will lead to different signal transduction pathways depending on the nature of the PAMP causing the response
1) Receptor binding triggers signal transduction pathways
2) This leads to new gene activation
3) This in turn leads to inflammatory cytokine production and release
What are the following steps after something binds to a TLR (toll like receptor)?
Sentinel cells
Cells of inflammation that detect invaders or tissue damage
Cytokines and other substances that cause necessary vascular changes and attract and activate phagocytic cells
What do sentinel cells release?
Vasodilation (THINK: this is why you see redness, warmth and swelling with acute inflammation - due to the increase in blood flow to the area)
Vaso____ is the hallmark of acute inflammation
Neutrophils and then the second ones to arrive are macrophages
Which cells are the first cells to arrive to inflamed areas?
1) Macrophages
2) Dendritic cells
3) Mast cells
What are the three types of sentinel cells that are also known as being part of the mononuclear macrophage system?
Cytokines
What do mast cells produce?
TNFa and IL-1
Which cytokines activate endothelial cells?
IL-6
Which cytokine activates acute phase protein synthesis by the liver?
Chemokines
Which cytokine regulates cell movement?
TNFa, IL-1, IL-6 and chemokines
Which specific cytokines are made from the macrophages?
IL-1, IL-6 and chemokines
Which specific cytokines are made from endothelial cells?
Macrophages, NK cells and T cells
What is the source of TNFa?
TNFa, IL-1 and IL-6
Which cytokines are known as the pro-inflammatory cytokines?
Systemic effects
Inflammatory cytokines have ____ effects
Fever (pyogen)
Inflammatory cytokines stimulate the hypothalamus to produce prostagaldins into what?
acute-phase proteins
Inflammatory cytokines stimulate the liver to produce ____
T; this can include septic shock and cachexia. They can also cause sickness behavior such as loss of appetite, lethargy and protein catabolism (muscle wasting)
T/F - Inflammatory cytokines are responsible for clinical illnesses
-Promotes inflammation
-Activates cells
-Enhances collagen synthesis, bone resorption and fibroblast growth
-Toxic effects such as killing tumor cells, septic shock, sickness behavior and altered lipid metabolism
How does TNF alpha affect the body?
-Affects metabolism
-Affects blood flow
-Affects cell growth
-Affects leukocytes
-Kills cells
-Promotes inflammation
-Affects the brain
How does IL-1 affect the body?
-IL-6
-IL-1
-TNFa
Which factors are responsible for acute-phase response?
IL-1
Interleukin that is a co-stimulator of Th2 cells
IL-6
Interleukin that promotes B cell differentiation
TNFa
Cytokine that stimulates T cell growth
It stimulates hepatocytes to produce acute-phase proteins
How do IL-1, IL-6 and TNFa affect the liver?
When there is a response to severe infections or massive tissue damage where there are very large amounts of cytokines and oxidants escaping into the blood stream causing a lethal form of shock
What is systemic inflammatory response syndrome (SIRS)?
Activated macrophages, endothelial cells and other types of cells
What are the sources of chemokines?
Attract leukocytes to sites of infection, stimulates actin polymerization/depolymerization and increase expression of adhesion molecules (B-integrins) on leukocytes
What are the actions of chemokines?
-Loss of appetite
-Fever
-Depression
-Neutrophilia
-Acute phase protein response
What are the systemic effects of chemokines?
T
T/F - illness is part of the response of the body to inflammatory stimulus
-Mast cells
-Macrophages
-Dendritic cells
Which cells secrete IL-1, IL-6, TNFa and HMGB-1?
Stimulates neutrophil production from bone marrow
How do cytokines affect the bone marrow?
-Activation of immune system (innate and specific immunity)
-Increased liver function
-Active excretion of toxins
-Bacteriostatic and bactericidal effects
What are the positive things associated with a fever?
-Functional overload of organs (lungs, heart, endocrine glands)
-Hypohydration and blood hemolysis may lead to disturbances of blood clotting
-Disturbances of GIT function due to increased level of toxic substances
What are negative things associated with a fever?
Increase in a1, a2 and B serum protein fractions
What is the lab diagnosis of inflammation?
Produced by the liver and it rises when there is inflammation throughout the body (*indicator of inflammation) (Binds to surface of dying cells and activates the complement system, promoting phagocytosis by macrophages which clears necrotic and apoptotic cells and bacteria)
What is C-reactive protein (CPR) and when does it rise?
-TGFb
-IL-10
What are the anti-inflammatory cytokines?
-TNFa
-IL-1
-IL-6
-chemokines
What are the pro-inflammatory cytokines?
1) Arterioles dilate, increasing blood flow to the affected area
2) Capillaries become more permeable, allowing extra fluid plus large serum proteins to escape the blood
3) Leukocytes migrate through venule walls into extravascular tissue (exudate)
What are the 3 vascular changes due to inflammation of the small blood vessels in the area of infection?
1) Pain
2) Redness and Heat
3) Swelling
4) Loss of function
What are some signs associated with inflammation?
Vasodilation and therefore inflammation
What do prostaglandins promote?
Phospholipases (enzymes that breakdown the cell membrane)
What do steroids inhibit in the arachidonic acid cascade?
1. Margination
2. Rolling
3. Integrin activation by chemokines
4. Stable adhesion
5. Migration through endothelium
What are the steps of the leukocyte adhesion cascade?
Cytokines such as TNF and IL-1, macrophages
In the leukocyte adhesion cascade, margination is facilitated by what chemical messenger? What produces these chemical messengers?
Rolling
Glycoproteins of leukocytes interact with selectins
Integrin activation by chemokines
Integrins change to a high affinity state
Stable adhesion
The integrin ligands stop the leukocytes at the site of injury
CD31
What modulates the leukocyte's migration through the endothelium?
Neutrophils
What WBC is the most abundant in most species?
Neutrophils
_____________ are the first cells to arrive and they deal with most if not all of the invading organisms
Macrophages
_____________ follow neutrophils and deal with the remaining invaders and also clean up the mess
Neutrophil NETs
Neutrophils release histones concentrated with proteolytic enzymes that surround an antigen and kill it
NETosis
Slow cell death of neutrophil when producing NETs
Non-lytic NETosis
Rapid release of NETs from live cells
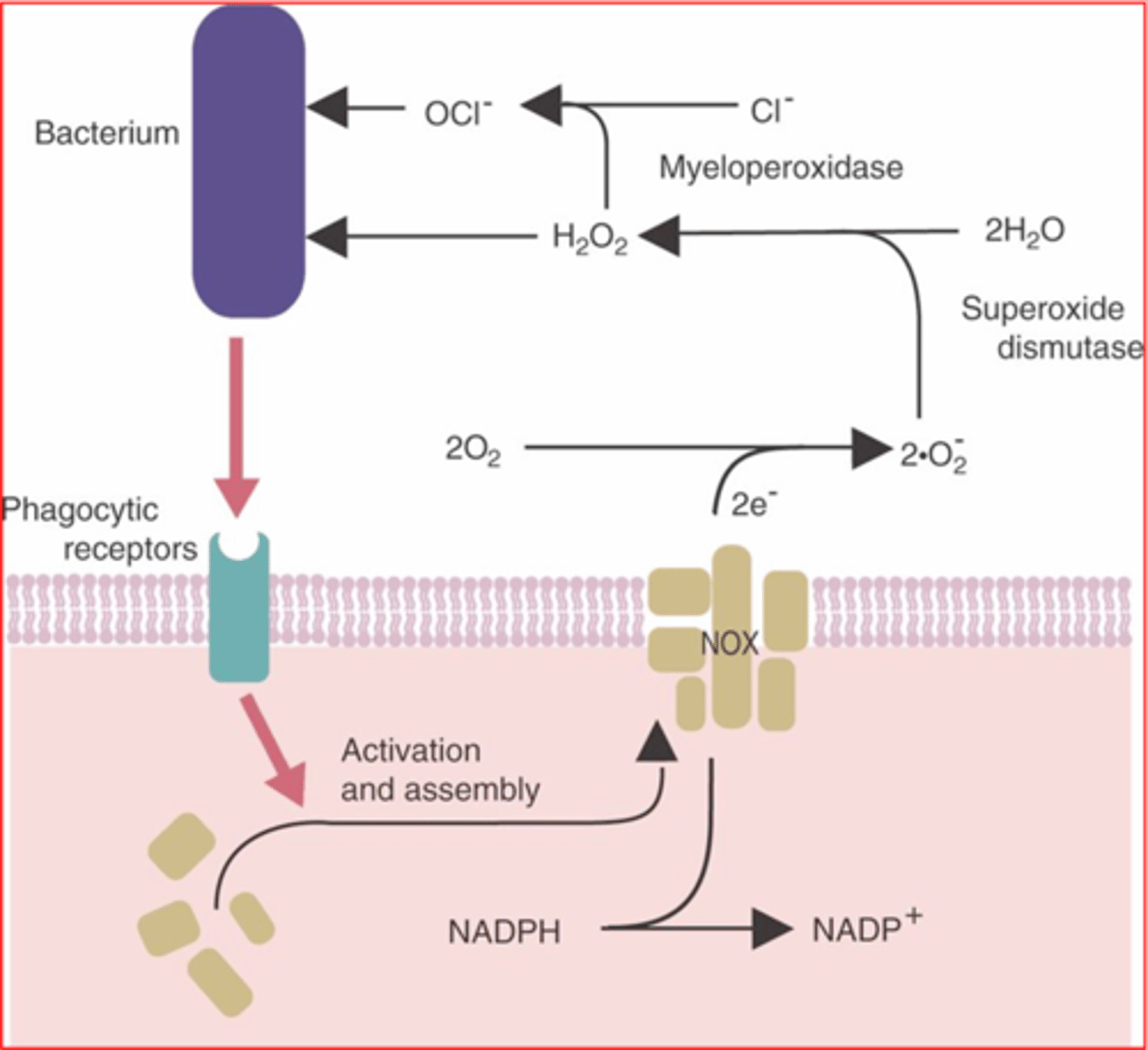
1. NADPH to NADP+
2. Nitrogen oxides used to convert oxygen to superoxide anion
3. Superoxide dismustase converts to hydrogen peroxide
4. Myeloperoxidase converts chlorine to hypochlorite (which kills microbes)
What are the steps of respiratory burst in neutrophils?
T
T or F: Neutrophils contain both primary and secondary granules
T
T or F: Neutrophils can only phagocytose once and then they have to be removed by a macrophage
F
T or F: Macrophages can only phagocytose once
Bone marrow
Where are macrophages produced?
Myeloid stem cell
Macrophages arise from what?
Monocytes
Before macrophages are macrophages, what are they in the blood?
Microglia
Macrophages in brain
Histiocyte
Macrophage in connective tissue
Dendritic cell
Specialized type of monocyte that displays antigens on its cell surface and presents them to components of the immune system
Osteoclast
Macrophage in bone
Kupffer cell
Macrophage in liver
Alveolar macrophage
Macrophage in lung
Acute phase responses (fever and pain)
IL-1 produced by macrophages is involved in stimulating what?
1. Stimulates T cell growth (part of adaptive immunity)
2. Stimulates acute phase response
3. Triggers inflammation
TNFA produced by macrophages has what actions?
Cytokines
All resting macrophages are activated by what?
Killing
M1 macrophages function
Repairing
M2 macrophages function
IFN-y (gamma)
What causes classical activation of a macrophage to an M1 cell?
IL-4, IL-13, and IL-10
What causes alternate activation of a macrophage to an M2 cell?
1. Chemotaxis
2. Adherence
3. Ingestion
4. Digestion
Steps of phagocytosis
Find-me signals
LPC is an example of what?
Monocytes, tissue macrophages, other phagocytes
Find-me signals recruit what cells?
Phagocytosis
___________ is triggered by the binding of a pathogen to receptors on the surface of the phagocyte
T
T or F: More than one receptor must be triggered in order to initiate the phagocytic response
Opsonization
Binding of antibodies or complements to bacteria that make them susceptible to phagocytosis
Opsonins
Antibodies and complement molecules that tag particles to be ingested
FC receptors
Receptors on the phagocyte's surface that specifically bind to antibodies
Phagosome
Intracellular vesicle containing antigen taken up by phagocytosis
Phagolysosome
Intracellular vesicle formed by fusion of a phagosome with a lysosome, in which the phagocytosed material is broken down by degradative lysosomal enzymes
Phagolysosome
If this structure does not form, the microbe will not die even if it has been phagocytosed