Unit 3 - Sources of Cardiac Muscle Dysfunction
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
138 Terms
Arrhythmia
any irregularity in the heart's normal rhythm, whether that rhythm is too fast, too slow, or simply out of sync
can arise spontaneously or in response to acute or chronic cardiac conditions
can also arise as a side effect of medications or as a consequence of other medical conditions, such as electrolyte imbalances
can originate from the atria or the ventricles
Atrial Arrhythmias
Structural Issues: coronary artery disease (CAD), hypertensive heart disease, valvular defects
Thyroid Dysfunction
Hyperthyroidism can increase excitability
Substance Use
Electrolyte Imbalances: K+, Mg2+
Ventricular Arrhythmias
Ischemic Heart Disease
Cardiac Remodeling: Dilated/hypertrophic myocardium
Cardiomyopathies: Hypertrophic, dilated types
Drug Effects: Antiarrhythmics, proarrhythmic drugs
Effective medical management of arrhythmias involves…
addressing underlying pathologies, adjusting lifestyle factors, and targeted pharmacotherapy
What is Atrial Flutter?
An atrial arrythmia characterized by rapid, regular atrial activity at a rate of 250-350 bpm
Atrial Flutter
The structural and functional changes to the atrial myocardium following an MI or other sources of myocardial injury (e.g., surgery) can alter normal electrical conduction paths and set up a reentrant circuit.
Can also occur in individuals with other preexisting heart conditions (e.g., valvular disease, pericarditis), have renal failure, hypertension, or chronic lung disease.
May be paroxysmal/transient, persistent (lasting days or weeks), or permanent
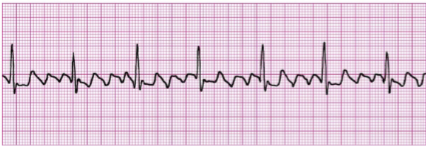
Atrial Flutter ECG
Because it is generally due to the regular depolarization of one area of the atria throughout each cycle (i.e., a single reentry circuit), the P waves appear identical to one another and give off a “sawtooth” appearance.
Many of the fast impulses that reach the AV node occur during its refractory period and do not conduct to the ventricles, resulting in a slower ventricular rate (e.g., 2:1 or 3:1 atrial:ventricular rate).
What is Atrial Fibrillation?
an erratic quivering or twitching of the atrial muscle that is caused by multiple ectopic foci and/or multiple reentry circuits
the most commonly encountered arrhythmia in medical practice and accounts for 1/3rd of cardiac hospitalizations

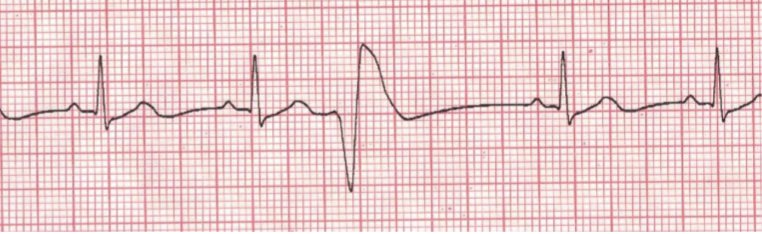
Atrial Fibrillation ECG
Since none of the ectopic foci actually depolarize the atria, no true P waves are found.
The AV node acts to control the most of the impulses that initiate a QRS complex; therefore, a totally irregularly irregular rhythm exists between the AV node pacemaker activity and random bouts of electrical activity in the atria that summate to depolarize the AV node
Conditions that increase atrial pressures in Atrial fibrillation
It is more common in enlarged atria with more space for dysfunctional circuitry. Following a myocardial infarction, inflammation and catecholamine release disrupt atrial electrophysiology and promote fibrosis, leading to structural changes like atrial dilation that exacerbate conditions favorable for the onset and persistence of atrial fibrillation.
Heart Failure
Hypertension
Pulmonary Disease
What to consider with atrial flutter and fibrillation?
are not, in and of themselves, considered immediately life-threatening, they can lead to serious and potentially life-threatening complications if not properly managed
Stroke risk due to blood stasis
Induce heart failure via tachycardia-induced cardiomyopathy
Symptoms of both atrial flutter and fibrillation…
will largely depend on underlying ventricular rate
Medical options for treating atrial flutter and fibrillation include:
Cardioversion: a medical procedure that aims to restore a normal heart rhythm
Medications:
Rate Control Medications: beta-blockers (e.g., metoprolol) and calcium channel blockers (e.g., diltiazem)
Rhythm Control Medications: Antiarrhythmic drugs (e.g., amiodarone) work by altering the electrical signals in the heart to maintain a normal rhythm
Anticoagulants (e.g., warfarin, apixaban): prevent the formation of blood clots in the heart
PTs can play a critical role in managing patients with atrial flutter & fibrillation by ensuring safe and effective rehabilitation strategies:
Activity Tolerance: fatigue, palpitations, shortness of breath, or chest pain can worsen with exertion.
Pulse Monitoring: Pulse oximeters may be inaccurate in AFib. Consider assessment of physical pulse for a full minute.
Use stethoscope for apical pulse if still unsure.
Consider using RPE for exercise.
RVR Concern: New-onset AFib with rapid ventricular response (RVR) >100 bpm at rest is concerning.
Premature Ventricular Contractions (PVC)
occur when an ectopic focus (or foci, in the case of multifocal PVCs) creates an impulse from somewhere in one of the ventricles. It occurs early in the cardiac cycle before the SA node actually fires
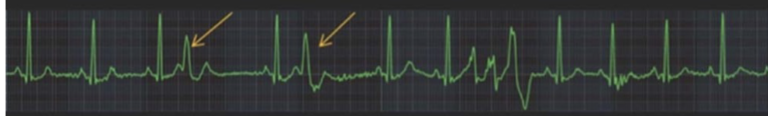
Premature Ventricular Contractions (PVC) ECG
The QRS complex is wide and bizarre and occurs earlier than normal sinus beat would have occurred.
It is wide because of slow cell-to-cell connections rather than through the normal rapidly conducting His-Purkinje system
**There are no P waves**
PVCs are…
common even among healthy people and are often asymptomatic and benign. In patients without heart disease, they usually pose no risk of life-threatening arrhythmias
PVCs can indicate…
underlying cardiac disorder and may suggest increased risk of serious ventricular arrhythmias, especially if frequent or multifocal
Serious PVCs
More than 10 per minute at rest
Occur consecutively
Multifocal origin
Physical exam note on PVCs
can be palpated as a skip or pause in the pulse. This may misleadingly suggest a lower HR during exercise when, in fact, arrhythmias have increased
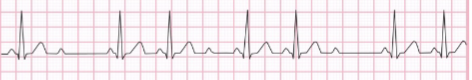
Trigeminy
every third beat is a PVC, with two normal beats in between

Bigeminy
every other beat is a PVC, creating an alternating pattern between a normal beat and a PVC.
Because it has a higher PVC frequency, it is generally more concerning

Couplet
two PVCs occur consecutively
suggest heightened ventricular ectopy, their clinical significance depends on the underlying cardiac condition
may indicate increased ventricular irritability and a higher risk of progressing to sustained arrhythmias, such as ventricular tachycardia

Triplet
three PVCs occur consecutively
considered a brief run of what is called non-sustained ventricular tachycardia if they occur at a rate of 100 beats per minute or higher

Multifocal PVC
originate from multiple ventricular foci from different areas of the ventricles
clinically more concerning than unifocal PVCs because they suggest greater ventricular irritability, increasing the risk of more serious arrhythmias, particularly in patients with underlying heart disease
considered a red flag in clinical practice
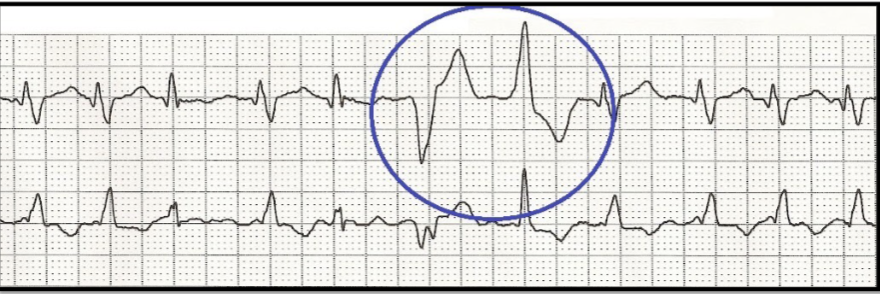
Ventricular Tachycardia (V-Tach)
a life-threatening arrhythmia defined as three or more consecutive PVCs at a rate exceeding 100 beats per minute, often reaching between 150 and 250 beats per minute
indicates extreme electrical instability in the ventricles and is often a precursor to even more lethal arrhythmias, like ventricular fibrillation
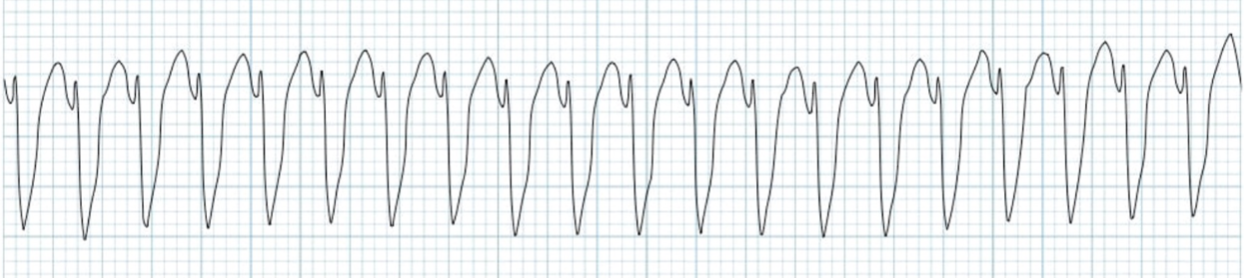
The rapid heart rate Ventricular Tachycardia (V-Tach)…
shortens ventricular filling time and leads to inefficient, uncoordinated contractions, drastically reducing cardiac output
This results in a significant drop in blood pressure, hemodynamic instability, and, without intervention, rapid progression to loss of consciousness, cardiac arrest, or sudden death
V-tach symptoms
lightheadedness and syncope, as reduced cardiac output can impair perfusion to vital organs
Ventricular Fibrillation (V-Fib)
chaotic, uncoordinated electrical activity in the ventricles, causing the heart to, essentially, just quiver rather than pump blood
results in virtually no cardiac output, depriving vital organs of blood flow
Without immediate intervention, it is fatal within minutes
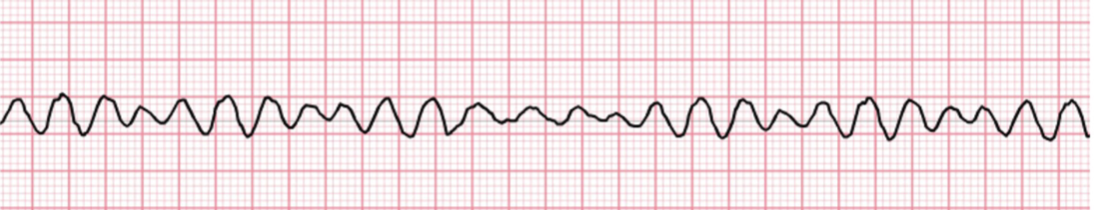
Ventricular Fibrillation (V-Fib) ECG
a rapid, erratic waveform with no recognizable QRS complexes, P-waves, or T-waves
Asystole
the most severe form of cardiac arrest, characterized by complete absence of electrical activity in the heart
indicates that the heart is no longer generating impulses, resulting in no cardiac output and no blood flow to the body
non-shockable, meaning defibrillation is ineffective
treatment focuses on immediate CPR to manually circulate blood and administration of emergency medications, such as epinephrine, to stimulate the heart and restore electrical activity
AV heart blocks
conduction disorders caused by delays or interruptions in the heart's electrical system, disrupting the coordination between the atria and ventricles
vary in severity based on the exact location and extent of conduction impairment
first-degree, second-degree, third-degree
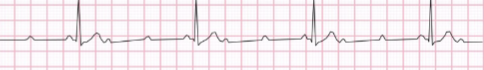
First-degree AV block
PR interval > 200 ms; delay at the AV node

Second-degree AV block
Mobitz Type 1 (Wenckebach): Progressive PR lengthening until a beat is dropped (P wave not conducted).

Mobitz Type 2: Fixed PR interval; intermittent non-conduction of P waves. Often involves a bundle branch block
Third-degree AV block
Complete block
No AV conduction; atrial and ventricular rhythms are independent
Cardiac rhythm assessment is used to…
identify and understand common to life-threatening arrhythmias. A regular rhythm expected during exercise; changes in arrhythmia with activity require careful evaluation
Considerations for clinical decision-making
Is the arrhythmia new or changing in character with increased activity?
Is the arrythmia benign or life-threatening?
Is the arrhythmia producing new or worsening symptoms?
Clinical tips
Individuals experiencing intermittent arrhythmias might not exhibit arrhythmic events during every bout of increased activity.
Arrhythmias that are effectively managed with medication while at rest can sometimes become less controlled or more pronounced during physical exertion
Hypertensive Heart Disease
Left Ventricular Hypertrophy (LVH)
Thickening of the left ventricle wall to counteract increased vascular resistance; stiffens myocardial structures
creates a continuous afterload challenge
Hypertensive Heart Disease Results
Decreased Compliance & Diastolic Dysfunction:
Impaired ventricular filling and relaxation, reducing preload and stroke volume, particularly during exertion.
Impaired Coronary Reserve:
Limited oxygen supply during exercise heightens the risk of myocardial ischemia, atrial fibrillation, and ventricular dysrhythmias.
Reduced Cardiac Output:
Symptoms include lightheadedness, dizziness, dyspnea, and decreased exercise tolerance
Valvular dysfunction can…
develop acutely (e.g., valvular rupture) or chronically (e.g., due to atherosclerotic changes)
Valvular dysfunction can lead to…
Stenosis:
Narrowing of the valve opening, increasing pressure gradients and leading to ventricular hypertrophy.
Regurgitation:
Valve fails to close properly, causing backflow, volume overload, and potential dilation of chambers.
Prolapse:
Valve leaflets bulge backward, disrupting the seal, often seen in the mitral valve.
Chronic pressure or volume overload can lead to structural changes in the heart that can cause issues in both systole and diastole
Acute Valvular Dysfunction
Sudden cardiac output impairment; requires immediate surgical intervention.
Acute Valvular Dysfunction: Clinical Presentation
Sudden heart failure, severe dyspnea, chest pain, hypotension.
Example: Acute mitral regurgitation → volume overload → cardiogenic shock.
Acute Valvular Dysfunction: Management
Emergency valve repair/replacement
Chronic Valvular Diseases
Gradual onset due to degeneration, calcification, or congenital anomalies
Chronic Valvular Diseases: Clinical Presentation
Gradual symptoms like exertional dyspnea, fatigue, angina.
Example: Chronic aortic stenosis → left ventricular hypertrophy → compensated cardiac output
Chronic Valvular Diseases: Management
Monitoring, medical therapy, timely surgical intervention
Diagnostic Techniques for Valvular Function Assessment
integral to the medical clinical decision-making process as they guide the timing and type of interventions, from medical management to surgical procedures valve repair or replacement
Echocardiography
Cardiac Catheterization
Other diagnostics: ECG, chest X-ray; vital for assessing cardiac function
Early recognition and management of valvular problems are crucial to prevent catastrophic outcomes
Echocardiography
TTE: Non-invasive, visualizes valve anatomy, function, and blood flow.
TEE: Detailed images, especially for mitral valve and prosthetic valves.
Stress Echo: Evaluates valvular function under stress conditions
Cardiac Catheterization
Assesses severity of stenosis/regurgitation, critical for surgical planning
Medical Management of Severe Valvular Disease
Surgical Interventions
Percutaneous Interventions
Medical Management of Severe Valvular Disease: Surgical Interventions
Valve Repair: Preserves the native valve; techniques include annuloplasty and chordal procedures.
Valvulotomy: Incisions to relieve stenosis, often for congenital issues.
Valve Replacement:
Mechanical Valves: Durable, require lifelong anticoagulation.
Bioprosthetic Valves: Made from animal tissue, no long-term anticoagulation needed, shorter lifespan
Medical Management of Severe Valvular Disease: Percutaneous Interventions
Transcatheter Aortic Valve Replacement (TAVR): Minimally invasive for severe aortic stenosis, especially in high-risk patients.
Percutaneous Balloon Valvuloplasty: Dilation to improve valve function and flow
Medical Management of Severe Valvular Disease: Advancements
Minimally invasive techniques and potential innovations like regenerative medicine aim to
improve outcomes
PT Considerations in Acute Recovery from Valvular Surgery
Minimally invasive surgeries and repairs
Valvular Replacements
PT Considerations in Acute Recovery from Valvular Surgery: Minimally invasive surgeries and repairs
Smaller incisions are associated with less pain and quicker recovery which can allow for faster progression of activities toward pre-operative function.
Repairs preserve native valve tissue, leading to more physiological function and quicker activity progression compared to replacements
PT Considerations in Acute Recovery from Valvular Surgery: Valvular Replacements
Open-heart valve replacements or complex multi-valve surgeries often require longer recovery times and a more conservative approach to physical therapy to prevent excessive strain on the heart and surgical site.
PTs should be cautious in advancing activities, considering the higher risk of post operative complications and slower healing
PT Considerations in Acute Recovery from Valvular Surgery: Monitoring Considerations
Hemodynamic Stability:
Monitor for changes in cardiac output, dyspnea, fatigue, or abnormal rhythms.
Incision Sites:
Inspect for infection or dehiscence.
Bleeding:
Long-term anticoagulation increases bleeding risk. PTs should monitor for bleeding and educate patients on recognizing warning signs
Cardiomyopathies
Structural & functional abnormalities are not primarily due to CAD, HTN, valvular disease, or congenital defects.
Leads to systolic or diastolic dysfunction, heart failure, arrhythmias, or sudden death.
Differentiated by:
Functional Categories: Dilated, hypertrophic, restrictive.
Causal Viewpoint: Genetic, acquired, or mixed
Cardiomyopathies: Diagnostic Tools
Echocardiography and myocardial biopsy distinguish between types
Dilated Cardiomyopathy (DCM)
Mitochondrial Dysfunction and Dilation:
primarily involves mitochondrial dysfunction in the heart muscle, reducing energy availability and impairing the heart's ability to pump effectively, leading to ventricular dilation as the heart compensates for decreased contractility.
Systolic Dysfunction:
The primary concern is systolic dysfunction leading to reduced ejection fraction and cardiac output
Hypertrophic Cardiomyopathy (HCM)
Myocardial hypertrophy:
characterized by asymmetrical myocardial hypertrophy, myocardial disarray, rapid ventricular emptying and a preserved or slightly elevated ejection fraction.
Diastolic Dysfunction:
Increases LV end-diastolic pressure and predisposes to arrhythmias and sudden cardiac death. It is the leading cause of sudden cardiac death in young athletes in the USA
Common Concerns in both Dilated Cardiomyopathy (DCM) & Hypertrophic Cardiomyopathy (HCM)
Arrhythmias:
require vigilant monitoring for arrhythmias; adjusting exercise based on risk
Hypotension:
Both present a significant risk of exercise-induced hypotension due to their respective impacts on cardiac output, necessitating careful monitoring and cautious progression in exercise intensity to prevent sudden drops in blood pressure
Conditions that can contribute to heart failure
HTN
CAD
cardiac dysrhythmia
renal insufficiency
cardiomyopathy
heart valve abnormality
pericardial effusion
pulmonary embolism
pulmonary hypertension
spinal cord injurt
age-related conditions
Heart Failure: Systolic
impaired cardiac contractile function, where the left ventricle cannot pump blood effectively, resulting in a reduced ejection fraction
Some Causes
Ischemic Heart Disease
Myocardial Infarction, Transient/persistent myocardial ischemia
Dilated Cardiomyopathy
Idiopathic (~50% of cases), Viral, Familial/Genetic, Alcohol, and many more
Valvular Heart Disease
Aortic valve stenosis or regurgitation, mitral valve stenosis or regurgitation
Hear Failure: Diastolic
impaired filling of the left or right ventricle due to hypertrophy and/or changes in the composition of the myocardium
Some causes
Left Ventricular Hypertrophy
Restrictive Cardiomyopathy
Myocardial fibrosis
Pericardial effusion or tamponade
Heart Failure: HFrEF vs HFpEF
Due to overlap between systolic and diastolic dysfunction (i.e., many patients with HF suffer from both) and the widespread use of echocardiograms
HFrEF
Heart Failure with reduced ejection fraction
<40% EF
indicating impaired contractility and systolic dysfunction
falls below 40% due to weakened or damaged ventricular muscle, reducing the heart's ability to contract forcefully and expel sufficient blood during systole
HFpEF
Heart Failure with preserved ejection fraction
>50% EF
reflects preserved contractility but impaired relaxation and filling characteristic of diastolic dysfunction
Thickened and stiffened ventricular walls, as seen in conditions like left ventricular hypertrophy, limits the heart's capacity to accommodate returning blood
Heart failure with midrange ejection fraction
intermediate zone between 40% and 50%
shares characteristics of both HFrEF and HFpEF
Responses to decreased cardiac output include the activation of sympathetic nerves and the renin-angiotensin-aldosterone system in order to:
Increase myocardial contractility and heart rate
Produce arterial vasoconstriction (to help maintain arterial pressure)
Produce venous constriction (to increase venous pressure)
Increase blood volume (to increase preload/ventricular filling)
Increase activity in sympathetic nervous system wil…
stimulate myocardial contractility, heart rate, and arterial/venous tone which results in an increase in central blood volume which serves to further elevate preload (to attempt to increase cardiac output).
Over time, though, the heart becomes insensitive to B-adrenergic stimulation, which results in a decreased force of myocardial contraction and an inability to attain higher heart rates during physical exertion
Declining cardiac output causes…
a reduction in renal blood flow and glomerular filtration rate, which leads to sodium and fluid retention. The RAAS is also activated, leading to further increases in peripheral vascular resistance and LV afterload as well as sodium retention
As cardiac muscle dysfunction worsens…
the heart becomes less and less able to tolerate the increases to afterload/systemic vascular resistance that aims to maintain arterial pressure
The body has ways to compensate for declining cardiac output and include increasing B-adrenergic stimulation and activation of the RAAS system:
B-adrenergic stimulation becomes less effective over time and the RAAS system can eventually work against the heart’s function
As cardiac muscle dysfunction worsens, the heart becomes less sensitive to preload and less able to tolerate increases to afterload. This should help us remember that we should be vigilant in monitoring for:
Fluid Status: reduced sensitivity to preload impairs the heart's ability to pump efficiently, leading to fluid retention as the kidneys compensate for perceived low blood volume.
Conditions that create excessive afterload such as unmanaged hypertension which can place additional strain on the heart, exacerbating myocardial workload and potentially worsening heart failure
Heart Failure: ACC/AHA Staging
Stage A to D
ACC/AHA Staging: Stage A
high risk for developing CHF
no structural disorder of heart
ACC/AHA Staging: Stage B
structural disorder of heart
never developed symptoms of CHF
ACC/AHA Staging: Stage C
past or current symptoms of CHF
symptoms associated with underlying heart disease
ACC/AHA Staging: Stage D
end-stage disease
requires specialized treatment strategies
Heart Failure: NYHA Staging
Class I to IV
NYHA Staging: Class I
no limitation of physical activity
NYHA Staging: Class II
slight limitation of physical activity
comfortable at rest
NYHA Staging: Class III
marked limitation of physical activity
comfortable at rest
Class IIIa or IIIb
NYHA Staging: Class IIIa
no dyspnea at rest
NYHA Staging: Class IIIb
recent dyspnea at rest
NYHA Staging: Class IV
inability to carry on any physical activity without discomfort
symptoms present even at rest
The most common symptom experienced by individuals living with heart failure?
dyspnea
What can cause dyspnea?
Interstitial edema
Pulmonary edema
Reduced respiratory muscle blood flow
Interstitial edema
Lungs become heavy and difficult to move
Pulmonary edema
Fluid transudation into alveoli increases the work of breathing
Reduced respiratory muscle blood flow
Decreased cardiac output and lactic acid accumulation exacerbate dyspnea
What can cause Pulmonary Crackles/Rales?
fluid in alveolar spaces
Heard at lung bases
Pulmonary Crackles/Rales: Caused by fluid in alveolar spaces
due to elevated pulmonary pressures
Pulmonary Crackles/Rales: Heard at lung bases
potentially extending upward with increased severity or changes in position
Orthopnea
Dyspnea when lying flat due to fluid redistribution from the abdomen and legs to the lungs.
Relief:
Sitting up or sleeping with extra pillows
number of pillows used indicates severity
Paroxysmal Nocturnal Dyspnea (PND)
Severe breathlessness and coughing that wake the patient 1-3 hours after lying down.
Cause:
Reabsorption of interstitial fluid from the lower extremities back into circulation, increasing venous return and load on the heart.
Relief:
Sitting upright or standing provides relief, but symptoms can persist
Extra Heart Sounds: S3
(aka ventricular gallop) indicates a more compliant left ventricle. Thought to occur as blood passively fills a quickly distending left ventricle that makes contact with the chest wall during early diastole.
May be normal (“physiologic S__”), particularly in young people, but in the presence of other indicators of heart disease, it is one of the most sensitive indicators of significant ventricular dysfunction