Diabetes Overview and Diabetes in Primary Care (pharm is separate)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
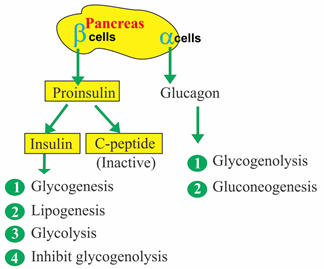
which islet cells are in charge of the following:
glycogenolysis, gluconeogenesis, glycolysis, lipogenesis, inhibiting glycogenolysis, glycogenesis
glucagon is responsible for gluconeogenesis and glycogenolysis;
insulin is responsible for glycolysis, glycogenesis, lipogenesis, and inhibiting glycogenolysis
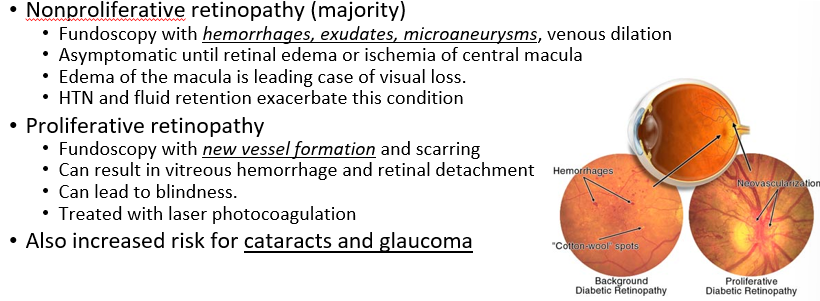
what is the leading cause of blindness in the US?
DIABETIC RETINOPATHY
You do a fundoscopy on a diabetic patient and note hemorrhages, exudates, microaneurysms, and cotton wool spots. You do not notice neovascularization. What type of retinopathy is this?
nonproliferative retinopathy
What is the 3 diagnostic criteria of late autoimmune diabetes of adults? (LADA)
age >30 yo
(+) autoAb to islet B cells
insulin independent at least 6m post Dx
LADA is colloquially known as type 1.5 diabetes, because it features characteristics of both Type 1 and Type 2; basically, the autoAb are targeting the Beta cells but there is a slow onset and the pancreas is still producing some insulin; that’s why it’s often mistaken as Type 2 DM
what is the dark velvety marking on the back of the neck that can be a symptom of diabetes?
Acanthosis nigricans

What are the criteria for diabetes diagnosis?
Must meet at least one of the following:
2 fasting glucose measurements >126 mg/dL
single random glucose => 200 mg/dL with symptoms (polyuria, polyphagia, polydipsia)
2 hour post prandial (or 75g oral glucose tolerance test OGTT) => 200mg/dL
HbA1C => 6.5%
what are the recommendations for DM screening?
all overweight adults should be screened every 3 years (or upon symptoms); screen earlier for those with risk factors
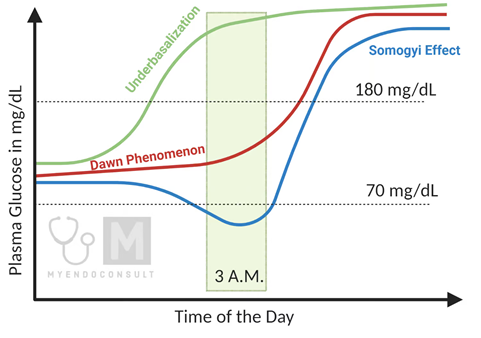
describe the difference between Dawn vs. Somogyi effect. How do you treat these?
Dawn Phenomenon - early morning episodes of hyperglycemia (with 3am elevated)
TX - limit carbs at bedtime, exercise after dinner, adjust/increase basal insulin or consider continuous insulin
Somogyi effect - nocturnal hypoglycemia leads to rebound AM hyperglycemia (S shape) with a reduced 3 am glucose
TX - reducing bedtime basal insulin dose, or have a bedtime snack
why should you use caution when imaging (with contrast) in patients who have DM and CKD?
They are at risk for developing acute renal failure due to contrast
How would we treat a diabetes patient who has microalbuminuria?
Why do we want to check annually for microalbuminuria in diabetes patients?
if someone has microalbuminuria, start them on ACEi and decrease protein in diet to help slow progression to end stage kidney disease
Checking for microalbuminuria in diabetic patients is crucial because it serves as an early indicator of kidney damage
we also want to check BUN:Cr
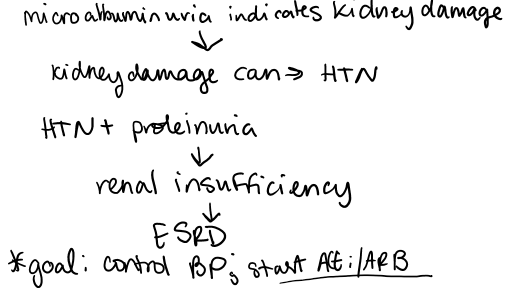
what is the number one cause of end stage renal disease?
diabetic nephropathy
What are some symptoms of autonomic dysfunction in diabetes patients?
impotence, neurogenic bladder, gastroparesis (can be treated with Reglan (metoclopramide)), postural hypotension
Duloxetine, Gabapentin, and Nortriptyline can all be used to treat what symptom of diabetes?
pain associated with peripheral neuropathy
what cranial nerves are often affected in DM?
CN 3, 4, or 6 (can cause eye pain, diploplia dbl vision)
CN III (Oculomotor): Controls most eye muscles, including those responsible for moving the eye upwards, downwards, and inwards, as well as controlling pupil constriction and eyelid elevation.CN IV (Trochlear): Primarily controls the superior oblique muscle, which allows for downward and inward eye movement, especially when looking towards the nose.
CN VI (Abducens): Controls the lateral rectus muscle, responsible for outward eye movement
what is the criteria to diagnose metabolic syndrome?
3 out of the following:
abdominal obesity
hyperglycemia
dyslipidemia
HTN
high TGL
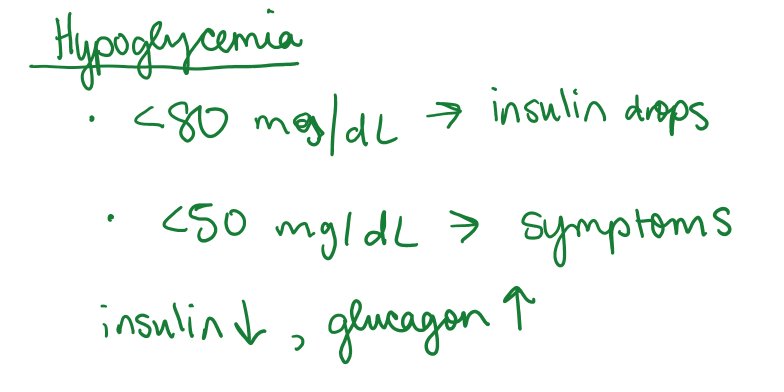
at what level of blood glucose does insulin start to drop? When do people generally start developing symptoms from hypoglycemia?
for most people, hypoglycemia is less than 70 mg/dL, but insulin starts to drop after <80 mg/dL, and symptoms tend to develop when BG is <50 mg/dL
why does adrenal insufficiency lead to hypoglycemia?
Normally, cortisol levels rise in response to stress (fasting, exercise, etc.) to prevent hypoglycemia. In adrenal insufficiency, this adaptive response is reduced and hypoglycemia is more likely. (epinephrine also promotes glycogenolysis and gluconeogenesis)
Why can ESRD lead to hypoglycemia?
reduced insulin clearance can lead to prolonged insulin action
The ominous octet is made up of the following:
decreased insulin secretion
decreased ______ effect (hint: these work in our GI system)
increased lipolysis (due to insulin resistance; usually, insulin suppresses lipolysis)
_____________ (hint: this happens in the kidneys
decreased glucose uptake in muscles
__________ (hint: brain)
increased hepatic glucose production (gluconeogenesis)
increased ______ secretion (by pancreas)
There are all targets of T2D management
decreased incretin effect (GLP-1) this is what tells us we are full
increased glucose re-absorption (SGLT-2)
neurotransmitter dysfunction (i.e. appetite)
increased glucagon secretion
in what patients would hemoglobin A1C not be a good reflection of their blood sugar levels (of prior three months)?
patients who are anemic, or patients with rapid cell turnover/proliferation
What is a normal fasting glucose?
Normal <100; cutoff <126
1 hour oral glucose tolerance test - sugar measured after 50g glucose load, should be less than __________
should be less than 130-140
how often do we monitor A1C in diabetes patients (and what does it depend on?)
A1c stable and at goal: every 6 months
A1c not stable and slightly above goal: every 3 months
A1c well above goal: every 1 month (according to Dr. Cozens; I guess you could monitor other things at these sooner check ups, like their daily glucose trends)