Exam 6 Camelids
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
Choanal Atresia
congenital and hereditary diseases
failure of nares to open during embryogenesis
inherited condition
nasal obstruction: partial or complete
camelids are semi-obligate nasal breathers. complete obstruction leads to death after birth
partial obstruction results in a lifespan of 5-8 months (due to kidney absence)
symptoms: open-mouthed breathing, stertor, nostril flaring, difficulty eating, high risk for aspiration penumonia
nasal fluid test: water flows out when filling the nasal cavity (indicates choanal atresia)
rubber tube test: tube inserted through the nose dosesnt pass beyond the eye level
nasal endoscopy: visual examination of nasal passages
contrast radiography: imaging with contrast to identify obstruciton
ultrasound: checks for presence of both kidneys
blood work indicators : elevated BUN and creatinine levels indicated absent kidneys
treatment:
surgical correction to open the blocked passage, enabling normal airflow and drainage
prognosis:
typically poor, euthanasia in 90% of cases
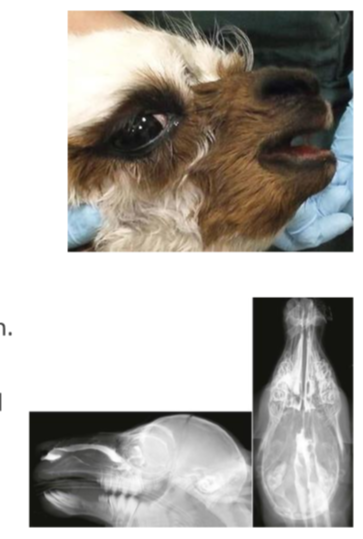
Wry face
Congenital and hereditary disease
more common in llamas than alpacas
mild cases cause dental issues, needing dental work 2-3 times annually
severe deviations often lead to euthanasia due to eating difficulties
Diagnosis:
palpation of bony deviation
confirmed with lateral radiographs

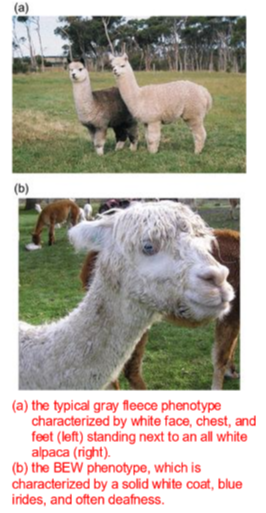
Blue-eyed white (BEW) alpacas or lethal white
Congenital and hereditary disease
all-white color prized for valuable fiber
BEW alpacas have two blue eyes a solid white coat, and are deaf
almost always born to two tuxedo grey parents
affected animals fail to move with the herd stand still and do not respond to calls
considered a welfare issue
Diagnosis:
genetic testing confirms the condition
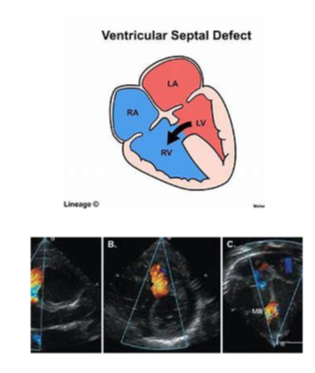
Ventricular septal defect (VSD)
congenital and hereditary disease
small defect: potential for normal lifespan
large defect:
stunted growth
poor exercise tolerance
murmur may be present
eventually signs of heart failure
very large defect (>1 inch): typically results in death within a minute of birth
diagnosis can be confirmed by ultrasonography, necropsy
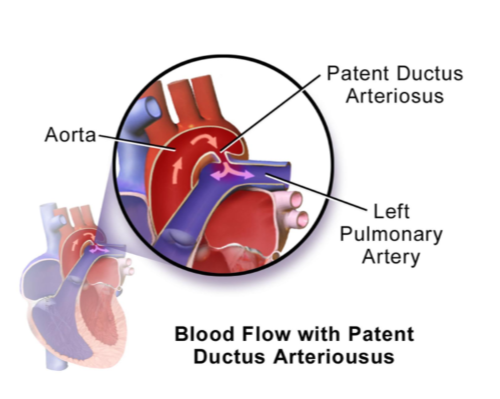
Patent Ductus Arteriosus (PDA)
closure typically occurs by 2-4 days of age
essential for long-term survival
often linked to complex congenital heart issues
clinical findings: - continuous murmur
Diagnosis:
echocardiography: left to right shunting
mild left ventricular enlargement
scant pericardial effusion
treatment:
surgical closure using an Amplatz canine duct occluder (ACDO)
Joint/bone congenital and hereditary diseases
polydactyly: 3 or more claws instead of the usual two
typically live up to 6-8 months of age
develop severe arthritis or face fiddiculty in mobility
often euthanized due to welfare concerns
Carpus valgus
successful treatment
early intervention with casting or splinting
surgical treatment is also an option

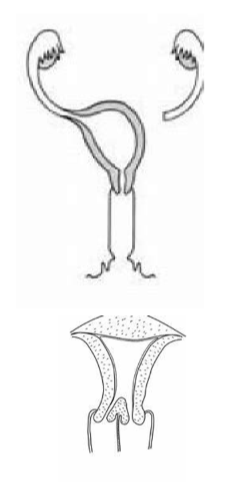
Uroenital defects congential and hereditary disease
Females:
uterus unicornis
one horn instead of two
can lead to dystocia
double cervices - fail to conceive, lead to dystocia
segmental aplasia of vagina/uterus - lead to dystocia
Males:
all may interfere with breeding
hypospadia - urethra opening is somewhere other than the tip of the penis
persistent frenulum
retained testicles
Hermaphrodites
true hermaphroditism: presence of both ovarian and testicular tissue
pseudohermaphroditism: discrepancy between external gentialia and internal reproductive organs
Clinical signs:
ambiguous gentialia (eg enlarged clitoris, underdeveloped penis)
infertility
Diagnosis:
physical exam and external genitalia assessment
hormonal testing (testosterone, estrogen)
ultrasound or laparoscopy to identify reproductive organs
Treatment:
surgical removal of abnormal reproductive organs (gonadectomy)
prognosis:
poor for reproductive purpose
Immunodeficiency syndromes in Llamas and Alpacas
Classification:
primary (inherited) immunodeficiency
secondary (acquired) immunodeficiency: develops due to disease, malnutrition or external stressors
Clinical signs
chronic or recurrent infections (bacterial, viral, fungal or parasitic)
weight loss and poor body condition
growth failure
poor wound healing
persistent diarrhea or respiratory infections
Diagnosis:
clinical history and physical exam: chronic infections, failure to thrive
hematology and immunology tests:
leukopenia
decreased immunoglobulin levels (IgG, IgA, or IgM)
lymphocyte function tests
flow cytometry to assess immune cell populations
culture and sensitivity testing: identifies pathogens involved in recurrent infections
genetic testing: identifies hereditary immunodeficiency syndromes
Treatment:
nutritional support with high-quality feed
proper hydration (oral or intravenous fluids)
antibiotic or antifungal therapy: based on culture results
plasma or whole blood transfusion
prognosis:
primary immunodeficiency : poor prognosis; affected animals often fail to survive long-term
secondary immunodeficiency: variable prognosis; depends on the underlying cause and response to treatment
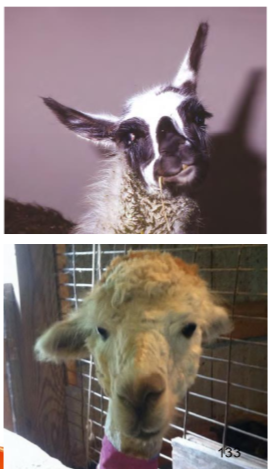
Berserk male syndrome behavioral disorder
aberrant behavior syndrome, novice handler syndrome
increased aggression towards humans: screaming, charging, spitting, biting, and laying on top of people; can be fatal
develops in young (llamas (crias) with excessive human attention
more common in intact males but not exclusive to them
prevention: discourage behaviors in young llamas such as
nose bumping
rearing up
wrapping legs around the owners waist
spitting behavioral disorder
Normal: used for social hierarchy or defense
Behavioral disorder: excessive spitting at humans signals stress, fear, or poor socialization
causes: overhandling, competition, fear, pain, or lack of training
prevention:
proper socialization, calm environment, and boundary training
remove stressors, use positive reinforcement, behavior modification
behavior modification / training
llama spits when approached during feeding
1) stand at a distance where the llama eats calmly
2) gradually move closer over several days, rewarding calm behavior with treats
3) if the llama shows signs of discomfort (ears back) stop and retreat then try again later
4) over time the llama learns that calm behavior results in rewards reducing the need to spit
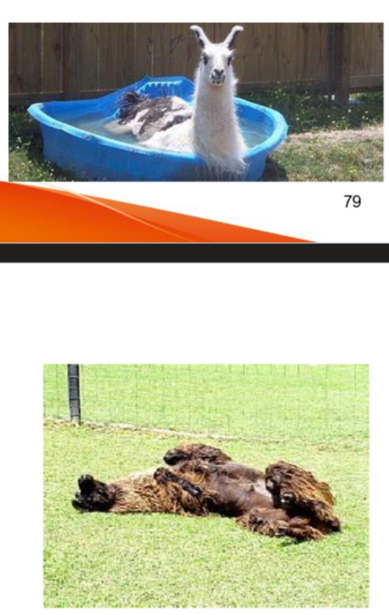
Obesity
common nutritional problem in llamas and alpaca
causes:
high quality forage relative to needs
overfeeding of supplements
effects
increased susceptiblity to heat stress
metabolic disorders
infertilty
locomotive problems
prevention
provide exercise
regular assessment of body weight or condtion score
balance diet to maintain optimal conditon
reduce forage intake or quality
feed lower qulaity forages exclusively
segregate obese animals to prevent food stealing
increase stocking density or grazing intensity
graze only on mature pastures
-
Protein energy malnutrition (PEM)
insufficient provision of feed (quality and or quantity)
causes
malnutrition, starvation
improper ration formulation
risk factors
higher nutritional requirements for young, pregnant, and lactating animals
environmental conditions especially extreme cold, increase energy needs
cold conditions inrease maintenance energy by up to 75%
clinical signs
poor hair coat, alopecia, ill thrift, low body condition score (BCS)
potential hepatic lipidosis in pregnant/lactating females
diagnosis: feed analysis - good quality grass should have 8-10% protein
treatment: provide protein-rich supplements
prevention:
ensure adequate nutrition
balance the diet
avoid overfeeding protein in summer to prevent exacerbating heat stress
assess body condition scores reqularly

Vitamin D deficiency
results in reduced uptake of calcium and phosphorus
In crias:
born with angular limb deformities, especially carpal valgus
angular limb deformities may develop by 3 to 4 months of age
Rickets: shifting leg lameness and joint enlargement, especially in the carpus
In adults:
lameness, angular limb deformities
limb fractures, poor growth, surgical implant failure
Diagnosis:
blood levels normal range 75-200 nmol/l
dietary analysis: examine calcium to phosphorus ratio in a growing cria (>1.5)
treatment:
supplements: provide adequate vitamin D in dietary supplements
injections for winter born crias
administer vit A, D and E injections from 2 weeks of age until spring
caution: potential for injection site reactions and anaphylaxis
viamin D3 gel or paste: administer every 2-3 weeks
caution: excess vit D may lead to dystrophic and renal calcification

Copper deficiency
Essential roles of copper (Cu): energy metabolism, hemoglobin metabolism, bone, tendon, cartilage, and melanin production
factors affecting availability
absorbed in the small intestine (SI) and stored in the liver
beta-carotene aids absorption
availability depressed with increased molybdenum, sulfur, iron, zinc, cadmium, selenium, calcium in the diet
forage differences: lush forages from alkaline soil have lower Cu compared to hays and legumes
Copper deficiency effects:
Stringy fiber, excess shedding, hair loss
Rusty haircoat color
anemia
depressed immune function, leading to increased respiratory diseases
infertility
abnormal growth of bone, connective and tendon tissue, resulting in lameness
poor growth
Diagnosis: liver copper levels by liver biopsy
treatment and prevention:
maintain a dietary Cu: Mo ratio of 6 to 10:1
Cu: Mo ratio of 16:1 or greater is associated with Cu toxicity
Iron Deficiency
Clinical signs:
poor growth
chronic weight loss
diarrhea
non-regenerative microcytic hypochromic anemia
decreased hemoglobin levels
treatment:
poor response to oral supplementation of iron
parenteral injection of iron dextran:
Selenium deficiency (white muscle disease)
Cause: forages low in selenium
clinical signs:
muscle weakness (skeletal form)
acute death (cardiac form)
in adutls: infertility, stillbirths, very weak newborn crias, depressed immunity
Diagnosis
feed analysis
blood level of selenium or glutathione peroxidase
treatment and prevention
arl selenium supplements
subcutaneous injection of baum selenate (slow release for 12 months)
selenium overdosing is toxic
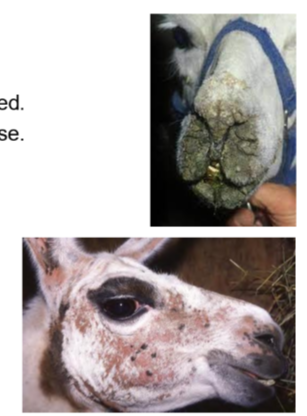
zinc deficiency (Dermatosis)
Clinical signs:
papules or dry plaques of alopecia
initial hyperemic lesions may become thick, crack, and bleed
lesions on ventral abdomen, inner thighs, bridge of the nose
Diagnosis:
skin biopsy reveals parakeratosis
blood level of zinc
treatment and prevention
oral supplements of 1g zinc sulfate daily
application of skin softeners on affected skin
systemic antibiotics may be necessary
prevention invovles ensuring adequate zinc in the diet
Hypocalcemia
occurs at peak lactation (2-4 weeks post parturition)
clinical signs and diagnosis:
anorexia, sternal recumbency, low body temperature
C1 atony and bloat
confirmation: serum levels of calcium
treatment
IV calcium borogluconate (100 ml of 20% solution)
repeated daily until fully recovery (3-4 days)
Hypomagnesemia
extremely rare in SACs, with llamas less likely than alpacas
occurs in spring and autumn/winter
associated with lush grass (high in potassium interfers with magnesium absorption)
clinical signs
recumbency and convulsions triggered by stress
frothing at the mouth, rapid eye movement, increased heart rate
treatment:
MgSO4 20% solution: 100 ml SQ
followed by IV solution containing 20% calcium borogluconate, 5% magnesium hypophosphite, and 20% glucose
prognosis: grave
prevention: provide magnesium-rich supplements, such as molasses licks containing 5% magnesium or magnesium oxide particles
Hypophosphatemia
Common in Llamas/alpacas:
grazing on pastures deficient in phosphorus
excessive dietary calcium or deficiency of vitamin D
Clinical signs:
generalized lack of calcification (decreased bone density)
pica (craving for anything containing phosphorus). this could lead to fatal botulism
treatment: sodium phosphate injections daily
prevention: provide phosphorus-rich supplements
Recumbency in SACs
Causes:
gastrointestinal diseases
colic: impaction, or displacement of intestines
gastric ulcers
respiratory diseases
pneumonia: severe pneumonia can lead to severe respiratory distress
tracheal collapse: difficult breathing results in recumbency
metabolic diseases: hypocalcemia, hypokalemia, hypophosphatemia, hypomagnesemia, fatty liver
neurologic diseases: P. tenuis, listeriosis, trauma
musculoskeletal diseases: septic arthritis, laminitis, osteomelitis, fractures, dislocations, severe muscle damage
septic diseases: endotoxemia, septicemia, abscesses
Metabolic diseases
Diagnostics for recumbent Llamas
clinical exam
lab tests: hematology, biotchemistry, urinalysis, cultures
imaging: ultrasound, radiography, MRI, CT scans
specialized procedures: endoscopy, arthroscopy, cerebrospinal fluid analysis
Consequences of recumbency:
physical consequences
pressure sores: decubitus ulcers, particularly on bony areas like the hips and elbows
muscle damage leading to compartmental syndrome
muscle atrophy
nerve damage
joint stiffness
respiratory complications
pneumonia: high risk for aspiration pneumonia
decreased lung expansion: leading to decreased respiratory function
digestive problems
gastorintestinal stasis: bloat, constipation
colic: pain and discomfort from abdominal distention
gastric ulcers: due to distress and anxiety
Treatment of recumbent Llamas
General care:
repositioning: regularly change the animals position to prevent sores and improve circulation
padding: use soft bedding or paddig to reduce pressure on bony aeas and prevention sores
Medical treatment:
IV fluids
nutritional support: ensure adequate nutrition through high-quality feed or supplement feeding
pain management: NSAIDs
address underlying causes
specific treatments: antibiotics for infections, anti-parasitics for infestations, or surgical intervention for physical injuries
correction of metabolic imbalances
physical therapy and rehabilitation
prognosis of recumbent llamas
pronsis is influened by various factors including:
underlying cause: condition causing recumbency (trauma, metabolic disorder, infection) significantly impacts recovery
duration of recumbency: longer recumbency increases risks (pressure sores, muscle atrophy, organ failure)
early and appropriate treatment: timely and correct intervention improves recovery chances
response to treatment: positive response to therapy indicates better prognosis
overall health status pre-existing conditions or poor health worsen outcomes
Hyperlipemia
elevated levels triglycerides in blood
Causes:
often triggered by stress, negative energy balance, pregnancy or systemic illness
Clinical signs
lethargy, anorexia, weakness
neurological signs (depression, seizures
colic, diarrhea, or constipation
Diagnosis:
bloodwork: elevated triglycerides, cholesterol, and lipemia (milky plasma)
may also show elevated liver enzymes
treatment:
address underlying cause (stress, illness)
provide nutritional support (high-energy, low fat diet)
IV fluids adn medications to reduce lipid levels (isulin, heparin)
IV fluids with 0.9% saline and 5% glucose
antigastric ulcer medications
Prognosis - guarded to poor especially if untreated or advanced
complications - if not treated hepatic lipidosis develops. hepatic lipidosis can be fatal if not addressed promptly
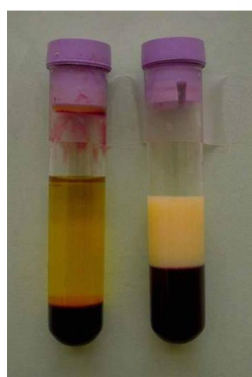
Hepatic lipidosis
Excessive fat accumulation in the liver leading to liver dysfunction
Causes:
often secondary to hyperlipemia, starvation, or anorexia
negative energy balance during late pregnancy. pregnancy toxemia (ketoacidosis)
Clinical signs:
similar to hyperlipemia (lethargy, anorexia, weakness)
jaundice (yellowing of mucous membranes)
neurological signs due to liver failure (hepatic encephalopathy)
Diagnosis:
bloodwork: elevated liver enzymes (AST, GGT) bilirubin, and bile acids
ultrasound: enlarged, hyperechoic liver
liver biopsy: confirms fat accumulation in liver cells
treatment:
dietay management provide a high quality energy rich diet hand feed if necessary
energy supplements: administer high energy drenches; several commericial products are avialble. propylene glycol is not advised (toxic)
gastric ulcer prevention
prognosis - poor to guarded especially if liver damage is severe. fatal if not recognized and treated aggressively within 2448 hours

Hyperglycemia, Hyperosmolarity, and insulin resistance of Llamas and alpacas
common in very sick camelids
blood glucose levels can reach up to 500 mg/dl
can be stress related and transient requiring no treatment if it resolves quickly
persistent hyperglycemia may require insulin therapy
Clinical signs:
increased uriation
fine muscle tremors
severe cases seizures and coma
concurrent hypernatremia may be present
treatment:
regular insulin
Polioencephalomalacia (vitamin B1 deficiency)
Acute progressive neurological disease
presents with recumbency, muscle fasciculations, convulsions, opisthotones, blindness with intact pupillary light reflex (PLR)
Diagnosis:
thiamine blood level
fluorescence of brain tissues (cerebral cortex) on ultraviolet exposure
histology reveals perineuronal vacuolation
treatment
thiamine injections: 8-10 mg/kg body weight intramuscularly every 4 hours for 4 treatments
fluid support oral or IV fluids
nutritional support administer energy-rich drenches
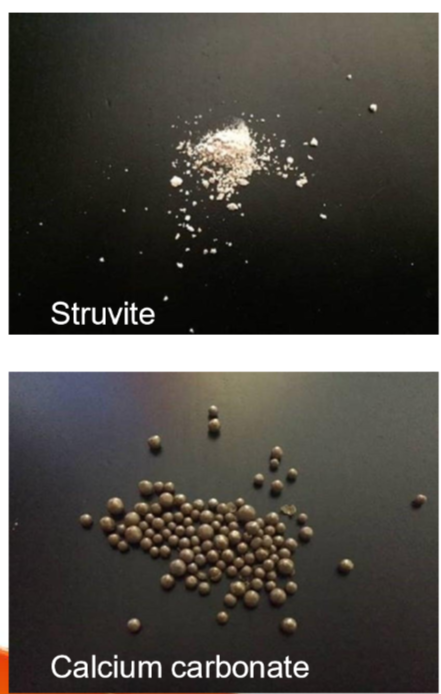
Urolithiasis
Male llamas and alpacas are prone to urethral blockage due to their genito-urinary anatomy
types of Uroliths:
Phosphatic (struvite, apatite, amorphous magnesium calcium phosphate)
caused by high-grain diets and low calcium to phosphorus ratio
calcium salts: less common but can occur
silica and oxalates: associated with certain forages or diets
clinical signs:
complete blockage:
bladder rupture: abdominal distention, pain, and shock
inability to urinate, severe discomfort and systemic illness
incomplete blockage
stranguria (difficulty urinating)
prolonged urination posture
urine dribbling or blood-tinged urine
depression, tooth grinding (sign of pain)
diagnosis:
physical exam: palpation of a distended bladder or abdominal pain
imaging: ultrasound or radiography to identify uroliths
urinalysis: blood, crystals, or signs of infection
Lymphosarcoma
typically seen in animals aged 4-5 years old
often seen in the terminal stage due to a lack of clear signs early on
presents with lethargy, lymphadenopathy, several months of weight loss and reduced appetite
progresses to terminal recumbency and death
diagnostic indicators
fine needle aspiration or biopsy: cytology and histopathology confirm neopalstic cells
in most cases, ascites on abdominal ultrasound
rare shedding of cells in abodminal fluid
elevated hepatic enzymes if invasion into the liver occurs
prognosis generally a grave prognosis
Liver abscess
Hepatic abscesses much more common than tumors
associated with rumenitis
laboratory findings:
elevated white blood cell count (WBC) and fibrinogen
hepatic enzymes may not be markedly elevated
diagnostic confirmation: confirmation by U/S, necropsy
treatment
prolonged antibiotic therapy (1 month or more)
use of NSAIDs
hand feed or use energy rich drenches
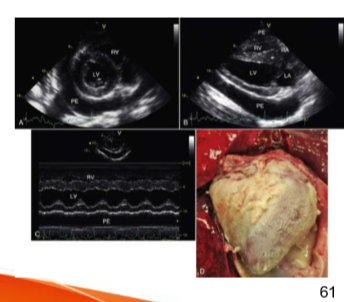
Pericarditis and epicarditis
Etiology:
Idiopathic (most common)
secondary to septic events, dilated cardiomyopathy pleuropneumonia, pulmonary hypertension or congenital heart disease
hypoproteinemia (associated with mild effusion)
Clinical signs:
lethargy
tachycardia
muffled heart sounds
tachypnea
cardiac tamponade (in severe cases)
treatment:
pericardiocentesis
systemic antibiotics and anti-inflammatory drugs
supportive care (IV fluids)
prognosis
favorable with prompt intervention
idiopathic cases may resolve without recurrence
secondary cases depend on underlying disease
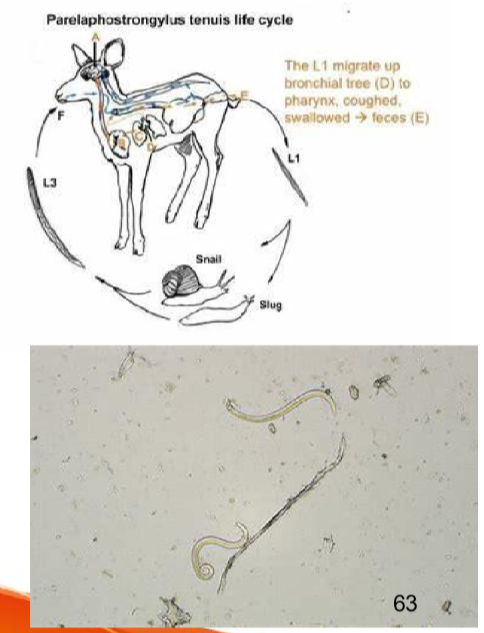
Parelaphostrongylus tenuis (P. tenuis)
Meningeal worm (white-tailed deer parasite)
white-tailed deer is the normal host
requires a snail in the life cycle
SACs and ruminants become aberrant hosts by ingestin the larvae
larvae migrate through the body penetrating the spinal cord and entering the brain
Clinical signs: Generalized ataxia, convulsions, coma and death
Diagnosis:
cerebrospinal fluid (CSF) analysis reveals high protein
necropsy shows L4 or L5 larvae in spinal cord or brain tissue
prognosis: poor prognosis
treatment:
supportive care
anti-inflammatory drugs: phenylbutazone
anthelmintics (dewormers)
invermectin
fenbendazole
prevention:
deer control remove any deer from the area maintain good fences
ivermectin injections administer monthly ivermectin injections starting at 1 month of age
snail control implement measures to control snail populations
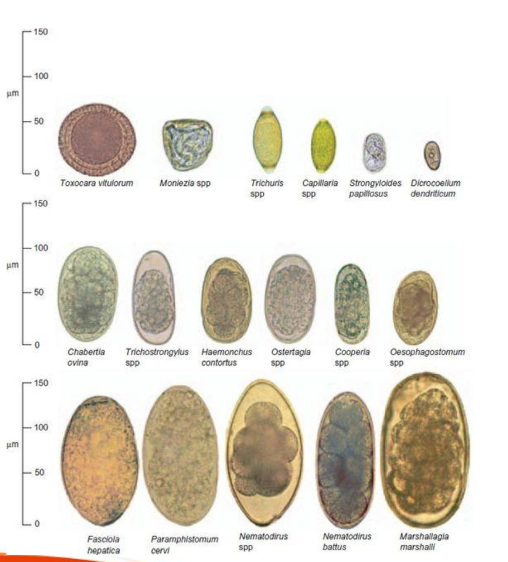
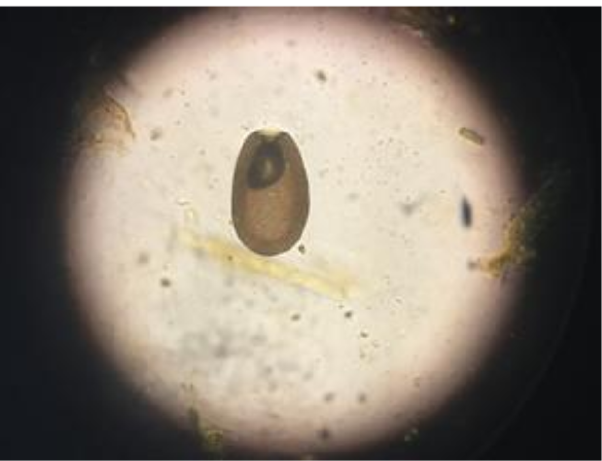
internal parasitism
Gastrointestinal Nematodes: Haemonchus contortus, Trichostrongylus, Nematodirus
Lungworms: Dictyocaulus viviparus, D. filaria
tapeworms; trichuris moniezia
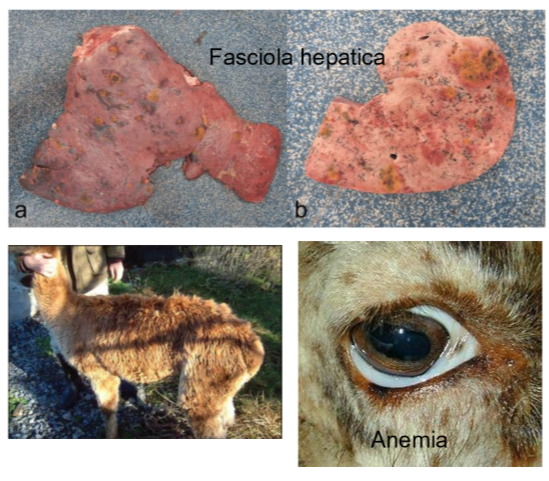
flukes: fasciola hepatica
Clinical signs:
anemia, poor growth
rough hair coat
diarrhea, with dog-formed feces (tubular or clumped)
treatment guidelines
targeted deworming: deworm only those that need treatment
base treatment on clinical signs, FAMACHA score 3+ (indicating the need for deworming) and egg count
prevention measures:
pasture management
hygiene practives
dewormig: maintain a routine deworming and fecal schedule
administer fenbendazole drench every 3 to 4 months
provide ivermectin or doramectin injections once every month
Coccidiosis
symptoms: diarrhea, weight loss, poor growth
diagnosis: fecal smears
treatment: treat only if a high oocyst count is identified on fecal examination or if diarrhea is present
treatment options
amprolium
sulfadimethoxine
ponazuril
Decoquinate (added to feed to reduce oocyst production)
preventive measures
daily cleaning: scrape pens and remove soiled or wet bedding every day
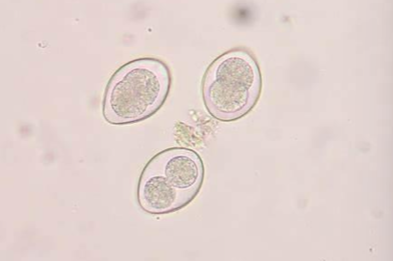
Coccidiosis - Eimeria macusaniensis
causes significant and permanent intestinal damage
diagnosis: fecal smears
affects mostly immunocompromised, young, or old animals
clinical signs:
lethargy, anorexia, weight loss, sudden death (hemorrhagic diarrhea)
stunting or ill thrift with chronic diarrhea
treatment:
treat if suspected even if no oocysts are found in feces
amprolium
sulfadimethoxine
ponazuril
decoquinate (added to feed to reduce oocyst production)
Mange (Sarcoptes, Psorotptes, Chorioptes, Demodex)
foot mites (Chorioptes) is most common
Clinical signs:
pruritus, alopecia, hyperkeratosis, scaling
resembles Zinc deficiency (not itchy)
Diagnosis: Deep scrapings and skin biopsy
treatments:
subcutaneous injections of eprinomectin or moxidectin
local treatment with Amitraz or diazinon
repeated treatment every 2 weeks for 2 to 4 treatments to eliminate newly hatched mites
oral therapy is not effective
for Chorioptes and refractory Sarcoptes:
higher doses of moxidectin by subcutaneous injections every 2 weeks
local therapy with amitraz or diazinon

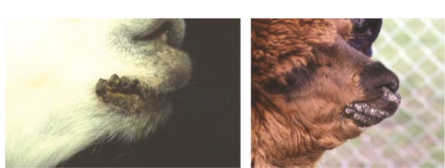
Munge in Llamas and Alpacas
is a severe dermaittis in camelids
Clinical signs:
heavy adherent hyperkeratotic crust
primarily affects paranasal and perioral regions
may extend to the bridge of the nose, periocular, and periaural areas
inflammatory lesions may wax and wane
Treatment: -treat secondary bacterial infections
some animals do not respond to treatment
may be associated with juvenile llama immune deficiency syndrome
further immune system evaluation and medical work up recommended
LIce
Transmission:
spread through close body contact
Clinical signs:
heavy infestation causes debilitation
lesions are common at the base of the tail, sides of thorax and abdomen, upper limbs, and flank
treatment
topical dust or pour on
Ivermectin subcutaenously (not effective for bting lice)
Ticks
SACs are ssuceptible to tick paralysis
ticks can cause inner ear infections, resulting in Horner syndrome
vector for anaplasma, hemoplasma
treatment:
topical dust or pour on
Ivermectin subcutaneously
Heat Stress
serious problem in hot summer season
factors affecting thermoregulation:
thermoregulation fails if:
environmental air is stagnant
ambient temperature is higher or the same as body temperature
ambient humidity is high enough to prevent evaporation
obesity
dehydration
clinical signs:
sternal recumbency (cushing)
depression
dehydration
panting with respiratory rate > 30
tachycardia with heart rate >100
frothing at the mouth
drooping lower lip
lateral recumbency, collapse and death
Heat stress treatment and recovery
cool the animal down: hose down + fan
rehydrate if dehydrated (offer cool water, not ice water, to prevent shock)
orogastric intubation with cold water with electrolytes
severe cases or recumbent animals: IV cool fluids with electrolytes
NSAIDs
B vitamins to improve appetite, B1 prevents cerebro-cortico necrosis
antibiotics for recument animals with comproised immune systems
grave prognosis if temperature rises to 108 F
during recovery
small amounts of feed multiple times dialy
add selenium and vitamin E and vit C to the diet to help protect the heart and vasculature
add vitamine A and D to help absorb minerals
prevention:
provide shade, pond
avoid fescue with endophyte acremonium species
do not feed too much protein
appropriate and timely shearing
avoid breeding during the heat of the day
avoid moving animals from cold climates to hotter climates
Enterotoxeias
Enterotoxemia type C
produce alpha and beta exotoxins
hemorrhagic eneteritis, hemorrhagic diarrhea
abdominal cramps, lying on one side of the body
sudden death
blood stained intestinal contents
Enterotoxemia type D
produce alpha and epsilon exotoxins
sudden death
CNS signs (convuslions, circling, prostration with opisthotonos, paddling and coma)
Diagnosis: Detection of toxins in intestine contents by PCR
treatment:
IV fluids
Antisera
Antibiotics
prevention:
hygien
consistent nutritional management
vaccination
Tetanus
wound infection (castration) with Clostridium tetani
produces neurotoxins affecting the central nervous system
Clinical signs:
stiff gait and difficulty moving
msucle rigidity, including lockjaw
hyperresponsiveness to stimuli
recumbency adn eventual respiratory failure
Diagnosis: based on clinical signs and history of trauma or surgical procedures
treatment:
antitoxin
antibiotics: penicillin
muscle relaxants: control muscle spasms (diazepam)
wound care: clean and debride any wounds
supportive care: IV fluids and nutritional support
prevention:
regular vac with tetanus toxoid
proper hygiene surgical and obstetrical procedures
Dental Issues
Overgrown Incisors:
affects forage prehension, making it difficult for camelids to eat properly
require regular inspection and trimming if needed
Tooth root abscesses
most common in molars
clinical signs:
focal swelling over the affected tooth (often mandibular > maxillary)
possible fistulous tract with purulent drainage
reluctance to eat, abnormal chewing behavior
unilateral nasal discharge, hypersalivation
weight loss pain
Tooth root abscesses in Llamas and alpacas
Diagnosis:
physical exam: detects swelling and pain
radiography: confirms diagnosis, assesses bone damage
culture and sensitivity: identifies bacterial cause
treatment options: systemic antibiotics such as Metronidazole + penicillin or Amoxicillin clavulante
-complications
bone sequestra damage to adjacent teeth
jaw fracture aspiration pneumonia
Stomatitis
Etiology:
trauma: oral injuris from grass awns (barley, foxtail, spear grass) or chemical irritants (caustic agents)
foreign material: hairy caterpillars on plants can cause irritation
Clinical signs:
ptyalism (excessive drooling)
dysphagia (difficulty swallowing)
resistance to oral examination
Diagnosis:
oral examination: requires sedation, mouth speculum and light source
ulcer evaluation: check for embedded foreign material
treatment and management:
remove foreign material if present
modify diet (change hay quality, remove from affected pasture)
Ddx:
Actinobacillosis
Bovine viral diarrhea
Malignant catarrhal fever
Megaesophagus in Llamas and Alpacas
Etiology:
no consistent causes idetified
no age or sex predilection
clinical signs
chronic weight loss
postprandial regurgitation
hypersalivation, excessive frothing while eating
Diagnosis: Barium contrast radiography or fluoroscopy confirms esophageal dilation
treatment and management dietary modifications:
soft, easily swallowed feed
elevated feeding platforms
prognosis: fair to poor some animals maintain condition long-term while others continue to decline
carbohydrate overload (acidosis or grain poisoning)
overconsumption, sudden change to grain, or sweet feed
clinical signs:
depressed, dehydration, bloating (left abdomen), ataxic adn staggery, tender gait; sawhorse stance, recumbent, death, diarrhea, surviors may develop abscesses in the liver and other organs, leading to long-term poor performance
Ddx: - polioencephalomalacia: check B1 level
treatment:
in early cases
administer IV fluids and electrolytes
Do C1 surgery to evacuate
thiamine injections
recumbent animals
poor prognosis
administer IV fluids and electrolytes
antibiotics
NSAIDs
prevention: only feed grains/pellets designed specifically for camelids and use them in moderation
Stomach Atony
Common
affects primarily C1-C2
causes
grain overload, feed changes, prolonged antibiotic therapy, spoiled feed, gastric ulcers, obstruction
clinical signs
reduced or no food consumption, weight loss, depression, diagnosis: absence of C1 contractions
treatment:
address primary cause
supportive care
transfaunation
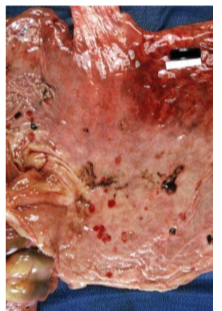
Gastric Ulcers
stomach compartment 3 (Equivalent to the monogastric stomach) is most commonly affected
Etiology: stress factors
environmental changes
social changes
disease
hospiralizaiton
clinical signs:
Bruxism (teeth grinding)
ptyalism
anorexia
regurgtation
black feces
recumbency
Diagnosis:
clinical signs
history of stress
U/S thickening and edema of C3 wall
treatment
remove stressor
gastric protectants (sucralfate)
H2 receptor antagonist (ranitidine, cimetidine, famotidine)
proton pump inhibitors (pantoprazole)
Regurgitation and Emesis
Regurgitation:
may be voluntary - defense
esophageal or laryngophrayngela stimulation
anesthesia and recumbency
emesis:
due to the elongated soft palate it is very common for ingesta to pass into the nasal cavity - rhinitis, obstruction, aspiration pneumonia
causes C1 overload, gastritis, diaphragmatic hernia, partial esophageal obstruction, poisonous plant ingestion
Johne’s Disease (Paratuberculosis)
Mycobacterium avium subsp paratuberculosis infection
chronic disease with infection starting early in age; clinical signs appear at an old age
organism shed in feces even before clinical signs
protein-losing enteropathy: chronic weight loss, ventral edema, intermittent diarrhea
diagnosis:
fecal culture
fecal PCR
treatment: no specific treatment
preventoin and control:
cull or relocate affected animals
remove crais from positive moms; hand-feed them or orphan them
purchase colostrum or milk replacer only from confirmed negative farms
quarantine and test all new animals

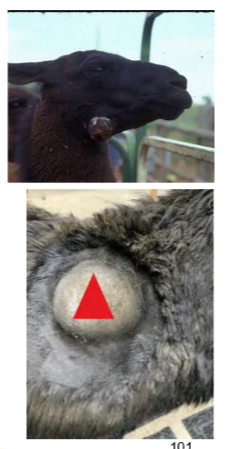
Corynebacterium pseudotuberculosis
Caseous Lymphadenitis:
transmission: direct contact with wounds
abscesses in the lymph nodes: retropharyngeal, axillary or popliteal nodes; affected lymph nodes are cool to touch
Diagnosis
culture of abscessed material
serology
treatment
surgical removal of abscesses
antibiotics are recommended
prevention: cull affected animals. test emaciated animals and cull positives
Diarrhea
Neonatal diarrhea
infectious causes: Rotavirus, coronavirus, cryptosporidia, E. coli
nutritional diarrhea
abundant dam milk production
sudden change in milk replacer
errors in mixing milk replacer or orphans
Diarrhea in young and older animals: Eimeria spp, Salmonella spp, Eosinophilic enteritis, Mycobacterium paratuberculosis, intestinal nematodes
Diagnosis: fecal cultures, fecal smears, PCR, ELISA, EM
Oral administration for fluid therapy
suitable for mild dehydration
administered through orogastric intubation
stressful and not recommended for severe cases

IV administration and intraosseous
IV:
preferred for severe dehydration, ongoing therapy and shock
options: constant rate infusion (CRI) or boluses every 2-4 hours
caution with potassium and calcium supplementation
Intraosseous in neonates if cant get catheter in
fluid solutions
balanced crystalloid solutions (lactated ringers, plasma lyte)
often administerd to patients with metabolic acidosis
normal saline as the main fluid component may cause hyperchloremic metabolic acidosis, inflammation, hypotension, acute kidney injury and death
often administered to patients with metabolic alkalosis
Maintenance fluid plan
(L) = 50mL/kg/day for adults, 80mL/kg/day for neonates
Replacement fluid volume
(L) = body weight (kg) x % dehydration
example:
150kg llama 10% dehdyrated
150kg x 10% = 15L
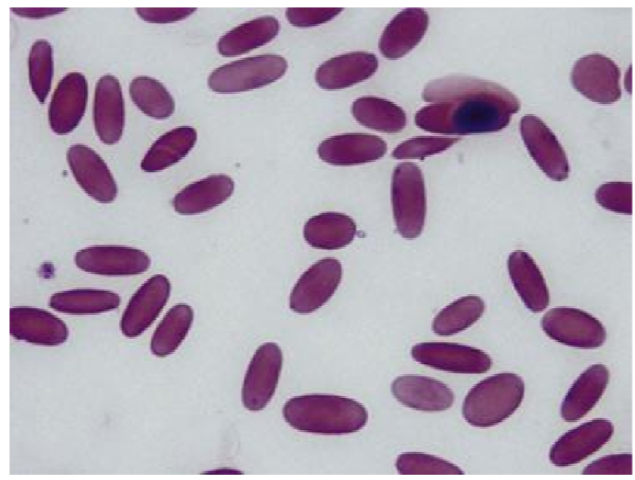
Mycoplasma haemolamae (Hemoplasmas)
Bacteria of the family Rickettsiae
unique to SACs
transmitted by ticks
intracellular causing extravascular hemolysis
Clinical signs:
fever, anemia, depression, icterus, infetility, edema, poor growth
Diagnosis:
Blood smear, PCR, ELISA
treatment:
oxytetracycline injections
blood transfusion if PCV is less than 15%
Pneumonia in Llamas and Alpacas
commonly caused by bacterial infections
Pasteurella, Mannheimia, Haemophilus, Mycoplasma
Viral infections
BHV-1, adenovirus, coronavirus)
aspiration of foreign material
clinical signs:
depression, anorexia, fever, cough, nasal discharge, tachypnea
Diagnosis
based on clinical signs, physical exam findings (lung auscultation)
rads, U/S, and culture of respiratory samples (nasal swab, BAL)
treatment
antibiotics (based on culture and sensitivity). oxytetracycline or Florfnicol
supportive care
oxygen therapy for severe cases
prognosis: good with prompt treatment; poor if untreated, particularly in severe or chornic cases leading to complications like pleural effusion or lung abscesses
Chronic obstructive pulmonary disease (COPD)
chronic inflammation due to dust, mold and allergens in poorly ventilated environments
Clinical signs:
chronic cough, nasal discharge, labored breathing
wheezing, exercise intolerance, weight loss
Diagnosis:
based on CS, history, physical exam
rads, bronchoalveolar lavage (BAL), endoscopy for confirmation
treatment:
environmental management (immprove ventilation)
bronchodilators, coticosteroids, mucolytics
low-dust diet, restricted exercise dung flare ups
prognosis:
chronic with varialbe severity, early management improves quality of life, but progressive cases may cause irreversible damage
Ringworm
Fungal infection - Trichophyton verrucosumis:
spread via contact with spores
lesions: crusty, circular plaques (2-3 cm diameter) on head, face, neck, body, and limbs
Diangosis: culture, direct microscopic examination of hairor skin scale
treatment:
usually self-limiting unless immunosuppressed
Povidone iodine topical application (1:4 solution)
Thiabendazole ointment (2%-4%, q3d)

Contagious Ecthyma (Orf)
self-limiting (3-4) weeks)
highly contagious
lesions olips, mouth, teats: raised erythremic areas, papules, or lesions with crust
diagnosis: PCR
zoonotic
treatment: no specific treatment. supportive treatment
prevention:
vaccination by scarification
autogenous vaccine
Rabies
aggressive or furious syndrome: vocalization and per acute death
Paralytic (Dumb) syndrome:
Tenesmus
ptyalism
bloat, pruritus, muscle tremors, aimless running, recumbency
diagnosis: Euthanize the animal and contact public health officials to coordinate testing at an approved rabies laboratory
histopathology of brain tissue: Negri bodies in neurons of the hippocampus (and other brain locations)
Fluorescent antibody staining
prevention: killed rabies vaccine, annually
Herpesvirus (EHV-1)
Clinical signs:
blindness with nonresponsive pupils
recumbency
Diagnosis: serology
Necropsy findings:
retinal detachment
retinitis
optic nerve degeneration
treatment
antivirals
interferon
steroids
IV fluids
prevention: vaccination with equine vaccine
West Nile Virus
transmitted by flies
neurologic signs:
ataxia
sudden blindness
paralysis
head tremors
diagnosis: serology, PCR
treatment: supportive care (50% survival)
prevention
equine vaccines used: 3 injections at 3 week intervals (may cause injection site swellings and anaphylaxis)
mosquito control
Eastern equine encephaltiis
transmitted by mosquitoes
Clinical signs:
acute CNS disease
head twitching
seizures
cranial nerve defects
most commonly sudden death
Diagnosis:
difficult antemortem (increased protein concentration in CSF)
necropsy: PCR, immunohistochemistry on nervous sytem tissue
treatment: no specific treatment
prevention: vaccination with equine vaccines
BVD
pestivirus infection: Noncytopathic BVDV 1b is most common
clinical signs (acute infection):
ill thft, lethargy, weight loss, nasal discharge, pneumonia, abortion, stillbirth, and weak premature neonates, persistently infected (PI) crias
persistently infected (PI) crias:
important sources of transmission, clinical signs in PI crais:
death due to acute or chronic mucosal disease
anemia
leukopenia
pneumonia
death
Diagnosis
PCR on whole blood
VI on blood or tissues
serology
herd screening: PCR on pooled blood samples
prevention:
vaccination using killed BVDV cattle vac
identify PI animals and cull them
maintain a closed herd
repeat screening
improve hygiene
Foot and mouth disease (FMD)
Clinical signs:
fever as high as 104 F
anorexia
vesicles on lips, gums, tongue, feet, teats
transmission:
aerosol
direct contact
contaminated water or feed
diagnosis:
rule out vesicular stomatitis and blue tongue
Tuberculosis (TB)
Mycobacterium bovis (Bovine Tuberculosis):
transmission: inhalation
symptoms:
chronic weight loss and poor body condition
chronic coughing or respiratory distress
lethargy and decreased appetite
enlarged lymph nodes
diagnosis: tuberculin skin testing
treatment
antibiotics long term
supportive care
success of treatment is often poor
prevention:
biosecurity: regular testing and monitoring of animals
vaccination: in areas where TB is endemic, bacillus calmette-guerin (BCG) vaccine may be considered
feed management: avoid feeding potentially contaminated feeds
carcass disposal: properly dispose carcasses and other animal products to prevent the spread of the disease
Pinkeye
common during summer months and fly season
viral or bacterial infections, often Moraxella like microorganisms
clinical signs:
painful eyes
yellowish eye discharge
mild to moderate chemosis (swelling)
blepharospasm (involuntary eye closure)
conjunctivities
epiphora (excessive tearing)
corneal opacity and ulceration
blindness
diagnosis:
clinical signs observation
ophthalmic swab for gram stain culture
treatment:
antibiotic injections
topical antibiotic ointments
NSAIDs for pain relief
prevention
autogenous vaccine
control flies to reduce the risk of infection

Otitis Externa
causes:
spinose ear tick (Otobius megnini)
grass awns causing epithelial damage
signs:
head shaking, scratching ears, head tilt, abnormal pinna positioning, hyperemic and ulcerated epithelial surface
exudation from the ear canal foul odor
diagnosis:
cultured samples may be non-diagnostic
treatment:
clean ear canal 1-2 times daily using dilute chlorhexidine
apply broad-spectrum antibiotic and anti-fungal otic ointment
small animal preparations or intramammary infusions for lactating cows can be used
Otitis media and interna
causes:
direct extension from external ear canal
ascending infection from eustachian tube
grass awns penetrating tympanic membrane
listeria monocytogenes in severe cases
clinical signs:
head tilt, ear droop, flaccid lower lip, collapsed nasal opening with deviation
facial nerve paralysis with decreased facial sensation, loss of reflexes
horners syndrome: ptosis, miosis, and protrusion of nictitating membrane
Disoreintation, ataxia, circling
diagnosis:
rads and CT scans for extent and damage
treatment:
antibiotic injections
procaine penicillin G
enrofloxacin
ceftiofur hydrochloride
ampicillin
surgical options
lateral bulla osteotomy and ear canal ablation
Chronic wasting disease
A prion disease primarily affecting cervids (deer, elk and moose)
clinical signs: progressive weight loss, lethargy, abnormal behvior, tremors, ataxia, and difficulty swallowing
diagnosis: definitive diagnosis is made post-mortem via histopathology of brain tissue
treatment: no effective treatment exists
prognosis: poor; CWD is fatal and there is no known cure
Rye grass staggers
Etiology: caused by Neotyphodium loii fungus in infected ryegrass
clinical signs: muscle tremors, ataxia, stiffness, difficulty walking (worsens with excitement)
Diagnosis: based on clinical signs and pasture history, confirmed by detecting toxins in ryegrass
treatment:
remove from contaminated pasture
supportive care, anti-inflammatory drugs, and muscle relaxants
prognosis:
good with early removal; chronic exposure may cause lasting damage or death
Endometritis
primary cause of reproductive failure in camelids
common pathogens:
Escherichia coli
Streptococcus zooepidemicus
Clinical signs:
repeat breeding, early embryonic death, or abortion
abnormal vaginal discharge
urterine wall thickening (detected via ultrasound)
diagnosis: clinical signs, ultrasound and bacterial culture
treatment:
uterine lavage: warm isotonic or a weak antiseptic solution (dilute povidone-iodine)
intrauterine antibiotics: infused in saline adn delivered directly into the uterus
penicillin K
gentamicin sulfate
ticarcillin
amikacin sulfate
ceftiofur sodium
systemic antibiotics for 5-7 days
ceftiofur sodium
penicillin
enrofloxacin
prostaglandins: to promote uterine contraction and clearance of infection
prognosis: pregnacy rates after treatment range from 30% to 60%
prevention:
utilitze minimum contamination breeding technique (MCBT)
ultrasound monitoring of ovaian activity
breeding only once when the follicle is mature
intrauterine antibiotic infusion 24 hours after mating
hygiene: stict hygiene practices during breeding and parturition
Abortion
Causes: BVDV, campylobacteriosis, anaplasmosis, coccidiomycosis, toxoplasmosis, and neosporosis
diagnostic approach for abortion:
History, clinical observations, and collection of appropriate samples, including placental and fetal tissues
fetal necropsy: whole ftuses with placenta should be sent to a diagnostic lab for necropsy
Reproductive disorders in male camelids
Preputial swelling: causes include inflammation, trauma
paraphimosis: often due to dirt or hair rings; leads to balanoposthitis and necrosis
scrotal trauma: common from male bites. requires urgent surgical intervention
hydrocele: fluid accumulation caused by heat stress. Diagnosed via ultrasonography
testicular degeneration: caused by heat stress, trauma or systemic diseases; affects semen quality
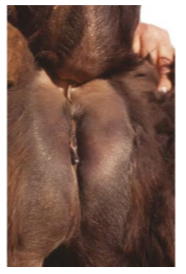
acute mastitis in camelids
occur shortly after paturition
clinical signs:
watery or bloody mammary secretions, fever, anorexia, udder swelling, and pain
treatment:
systemic antibiotics: Ceftiofur, penicillin G, or enrofloxacin
intramammary antibiotics: penicillin, cephalosporins, or amoxicillin
anti-inflammatory therapy
mammary gland stripping
supportive care in toxic mastitis cases
Subclinical mastitis
characterized by high cell counts (CMT)
Strep. agalactae and S. aureus are common isolates
diagnosis: culture, CMT, SCC
treatment: intramammary antibiotics such as penicillin, cephalosporins, or amoxicillin
prevention: proper hygiene, regular udder health checks
musculoskeletal diseases in llamas and alpacas
Angular limb deformities:
congenital or acquired
causes: nutritional imbalances and trauma
diagnosis: rads
treatment: splints, corrective trimming, or surgery
Capture myopathy:
stress-induced muscle damage from prolonged straint
signs: weakness, muscle stiffness, myoglobinuria
treatment: supportive care (fluids, anti-inflammatories)
prognosis guarded
claw defects:
overgrowth, cracks
treatment: regular trimming
Ulcerative pododermatitis
Etiology: trauma, poor hygiene, or wet, unsanitary conditons
clincial signs: lameness, swelling, heat in the affected feet, and visible ulcers or sores on the pads
treatment:
clean the affected area, debride necrotic tissue, and provide topical or systemic antibiotics
supportive care includes anti-inflammatory drugs and foot care (trimming)
prognosis:
good with early intervention
chronic or severe cases may require prolonged treatment or surgical intervention
prevention: regular foot care and environmental management are crucial for prevention
Geriatric Diseases
Dental disease:
involves periodontal issues, tooth loss, and malocclusion
regular dental check ups are required
Arthritis:
presents with joint pain, stiffness, adn reduced mobility
management focuses on pain relief
cataracts:
leads to impaired vision and difficulties in navigation
regular eye checkups are crucial and surgical intervention may be necessary
skin tumors:
tumors can be benign or malignant. surgical removal is required
cardiac disease:
symptoms include fatigue, exercise intolerance, and respiratory distress
regular cardiovascular monitoring is important for early detection
neurological disorders:
can involve spinal cord compression or degeneration
metabolic disorders:
include diabetes or hypothyroidism
proper management involves dietary adjustments and medications
castration
indications:
cohabitation between males
genetic control
reduce aggression
some suggest waiting until 18 to 24 months
early castration may impact bone growth potentially causing joint issues
preoperative:
tetanus toxoid vac
penicllin G injection
12 hour fasting
reastraint and analgesia:
recumbent position under sedation
tratesticular and incisional line blocks
lidocaine 2ml in each testicle, subC along incision line
removal:
each testicle removed after transfixation ligation of the spermatic cord using No 2-0 polyglactin 910
emasculation not recommended due to small cord size
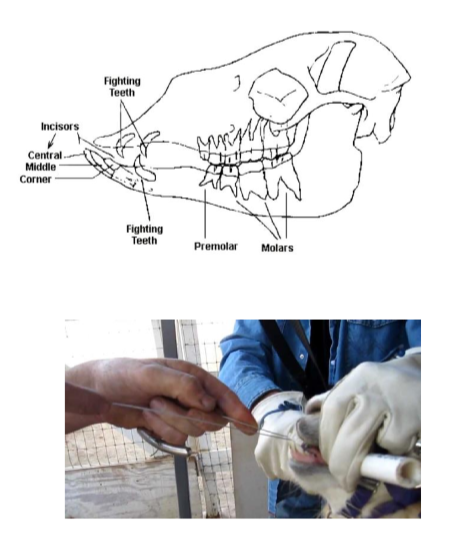
Fighting teeth
Mature male camelids develop upper and lower canine teeth and upper third incisors, known as fighting teeth
danger to handlers and other animals due to their sharpness and size
effect of castration on fighting teeth: no change castration does not alter:
the eruption timetable of fighting teeth
the need for cutting the teeth
their final size
trimming techniques
sedation
motorized tooth saw
OB wire
vaccination program
there are no approved vaccines for SACs
use vaccines approved for sheep, same dose as sheep
clostridium perfringens C and D and Clostridium tetani
first dose at 3 months of age and booster one month later. revaccinate annually
first dose at 2 weeks of age if dam is not vaccinated
vaccinate pregnant females 1 month before parturition
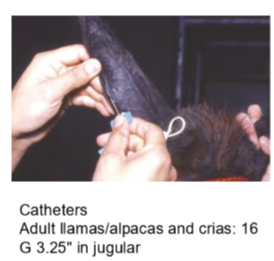
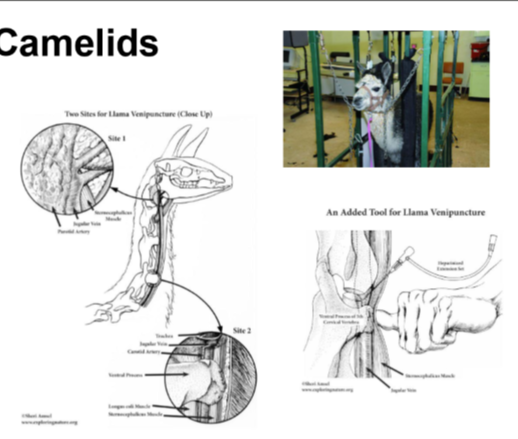
Jugular venipuncture
restrain in a chute
challenging due to lack of jugular furrow and thick skin
avoid hair clipping; slow regrowth
preferable on right side to avoid the esophagus
use 18 gauge, 1.5 inch needle
key sites
High neck: angle of mandible
Low neck: base of neck (5th cervical vertebra) - thinner skin
intramascular and subcutaneous injections

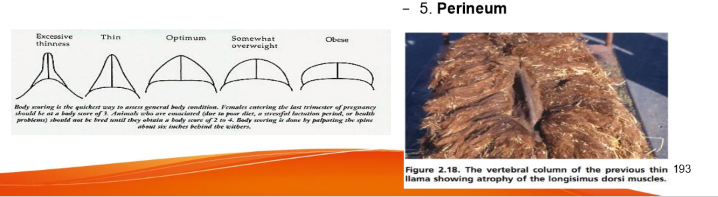
Body condition scoring
Need to palpate fibers can mask emaciation
score 1-5
obesity is a common problem in SACs in North America
places to palpate:
withers
behind the elbow
between the rear legs
between the front legs
perineum