4 - Pupils
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
What can pupil testing reveal?
Retinal or Neurological disease
What is the iris and pupil in optical terms?
Iris = diaphragm
Pupil = aperture
How is the pupil formed?
→ formed by atrophy of anterior mesoderm tissue (the pupillary membrane)
during fetal development, a pupillary membrane stretches across the eye but normally regresses (disappears) fully before birth
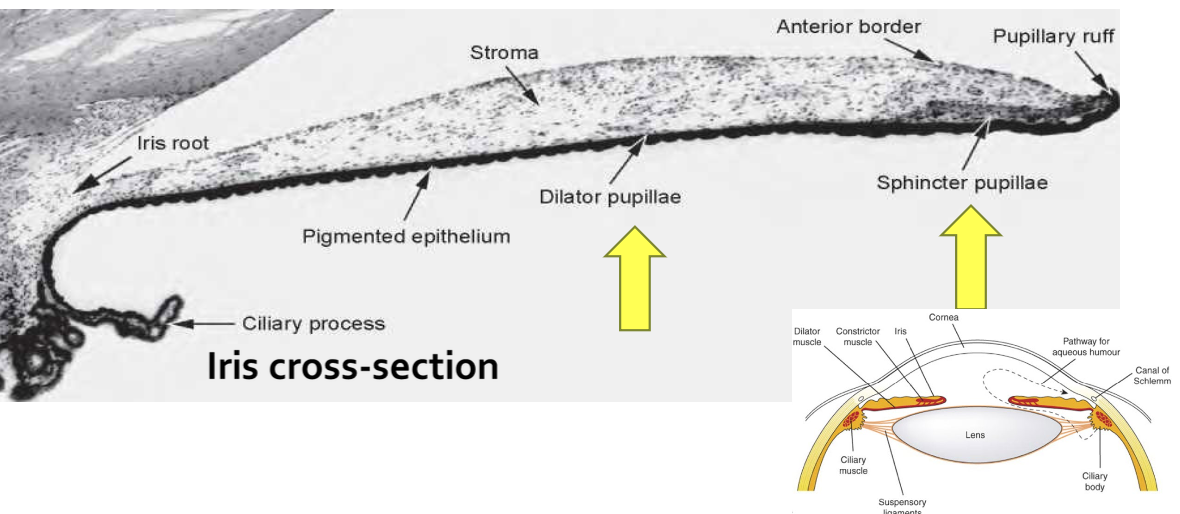
What developmental remnants might remain visible after birth?
In some individuals, remnants of this fetal tissue do not fully disappear, resulting in:
Persistent Pupillary Membrane (PPM) - appear as fine strands/cobwebs
Epicapsular stars - appear as stars

Note: Both aren’t harmful but can block vision if present in high amounts
What muscles of the body are only derived from neural ectoderm?
Iris muscles
For the Sphincter Pupillae muscle, identify its Location, Innervation & Action.
Location: Circularly around the pupil
Innervation: PNS
Action: Constricts the pupil (Miosis)
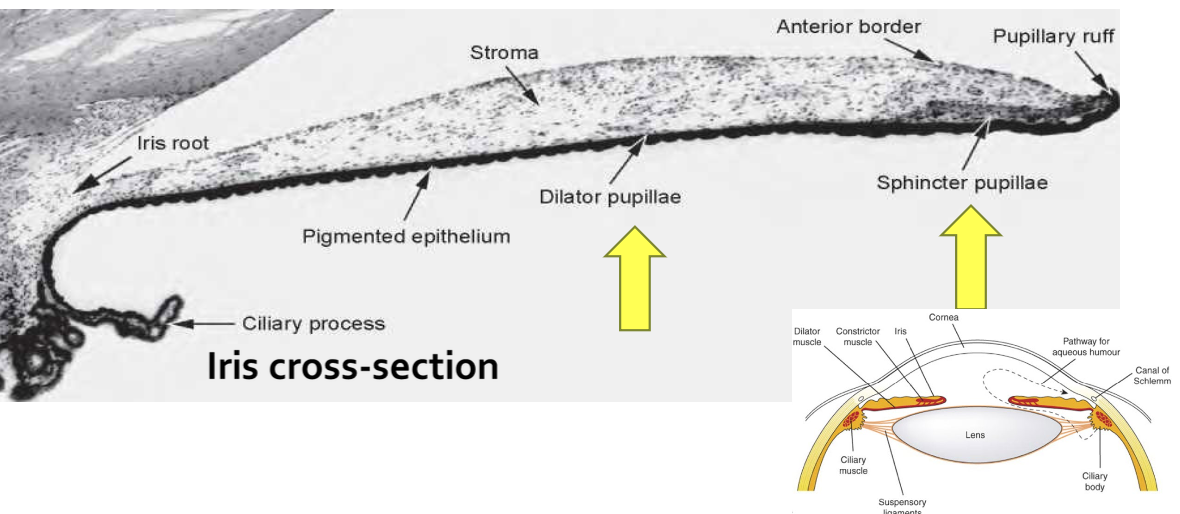
For the Dilator Pupillae muscle, identify its Location, Innervation & Action.
Location: Radially situated
Innervation: SNS
Action: Dilates the pupil (Mydriasis)
What are the normal characteristics of healthy pupils size?
Normal in size (2-8mm)
Central/Circular (slightly inferior and nasal)
BALANCE b/w sphincter & dilator → normal pupil size
List the functions of the pupil.
• Controls retinal illumination
• Helps facilitate light or dark adaptation
• ↓ optical aberrations
• ↑ depth of focus
List the 4 Components of Pupillary Testing.
Observation: the pupil shape, location, and size
Pupil reaction to light
Swinging flashlight test
Pupillary reaction to a near stimulus (accommodation)
When taking case history, what should you look for in terms of pupil?
Symmetry of pupils
Symmetry of eyelids at rest
Facial symmetry overall
What is the Normal Pupil Position?
Slightly inferonasal (~0.5 mm) from center of the iris
Abnormal Pupil Position: Define Corectopia.
displacement of the pupil

Abnormal Pupil Position: Define Polycoria.
more than one pupillary opening in the iris
How does age affect pupils?
Pupils become smaller and less reactive to light with age
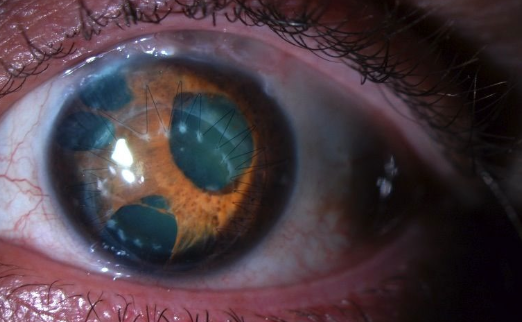
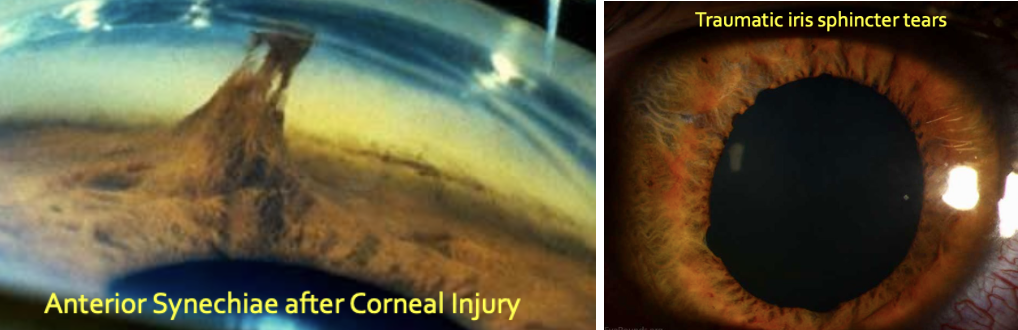
How can trauma affect pupil shape and size?
Anterior synechiae: adhesion b/w iris and cornea → pulls iris tissue & distorts pupil shape
Traumatic iris sphincter tears: damage to iris muscles → prevents normal constriction → dilated pupil
What is a hippus?
→ non-rhythmical, small-amplitude (<1mm) variation in pupil size that occurs in healthy eyes after light stimulation
constant tug-of-war b/w the sphincter and dilator muscles
doesn’t occur due to accommodation
What are the normal pupil size ranges under bright and dim light?
💡 Bright: 1.5 – 4.0 mm
🔦 Dim: 3 – 8.5 mm
What is Anisocoria? What is it caused by?
→ Unequal pupil size
Cause:
Physiological (normal variant)
Pathological (organic cause)
What is physiological anisocoria?
Seen in ~20% of the population
Pupil size difference: <0.5mm - 1mm
Pupil size difference stays the same in light AND dark
How can we determine if a pt has Physiological anisocoria?
If pt sees 20/20 & their Pupils:
React normally to light/dim
Pupil disparity is the same under light/dim (e.g., OD is bigger by 1mm under dim & bright)
have no other abnormalities (e.g., no ptosis, abnormal pupil reflexes or abnormal near response)
When anisocoria is more pronounced in LIGHT 💡:
What does it indicate?
Which pupil is abnormal?
What are possible causes?
→ Larger pupil is abnormal (b/c it isn’t constrict in light) = PNS issue
Possible causes:
Adie’s tonic pupil
CN 3 palsy
Iris sphincter injury or ischemia
Acute glaucoma
Pharmacologic dilation
When anisocoria is more pronounced in DARK 🔦:
What does it indicate?
Which pupil is abnormal?
What are possible causes?
→ Smaller pupil is abnormal (b/c it isn’t dilated in dark) = SNS issue
Possible causes:
Horner’s Syndrome
Iris pathology (e.g. inflammation, uveitis)
What is the sympathetic pathway NOT stimulated by?
light
Sympathetic Nervous System Activation
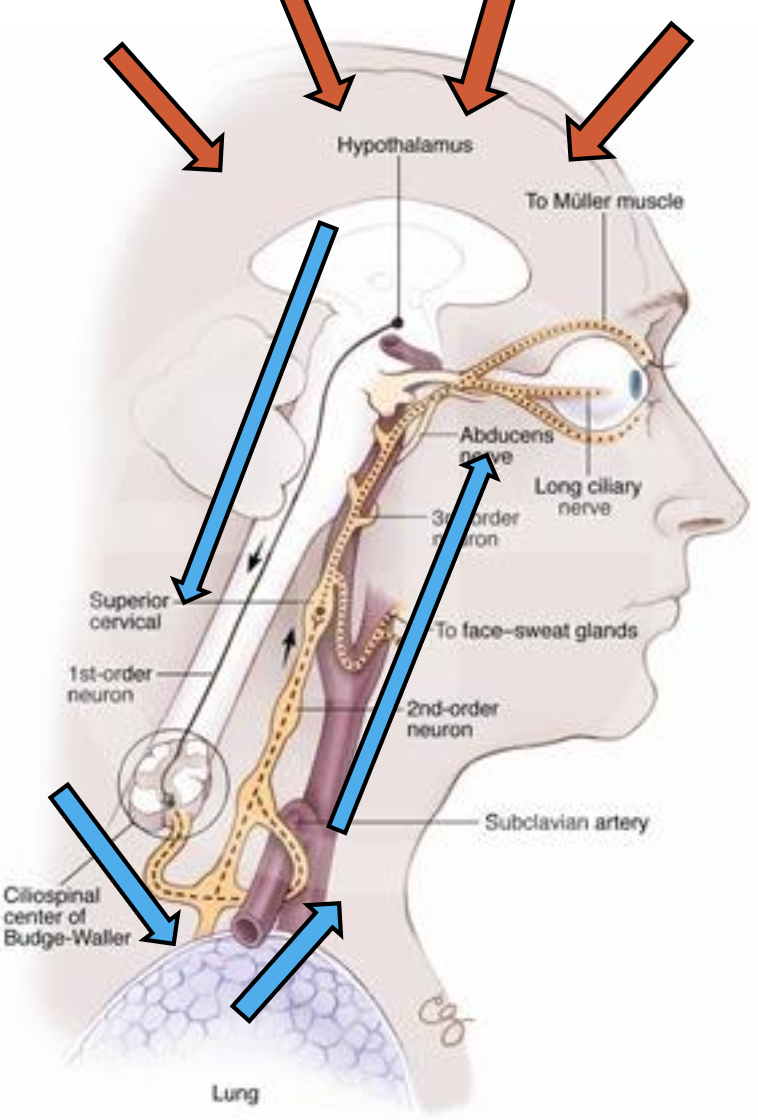
The afferent neuron stimulates the hypothalamus. The efferent pathway consists of a three-order neuron synapsing process. Outline the pathway leading to Synapse #1.
1st Order Neuron (Central Neuron)
Begins in the hypothalamus
Descends through brainstem
Enters spinal cord at C8–T1
Ends at the Ciliospinal center of Budge = ⭐ Synapse #1
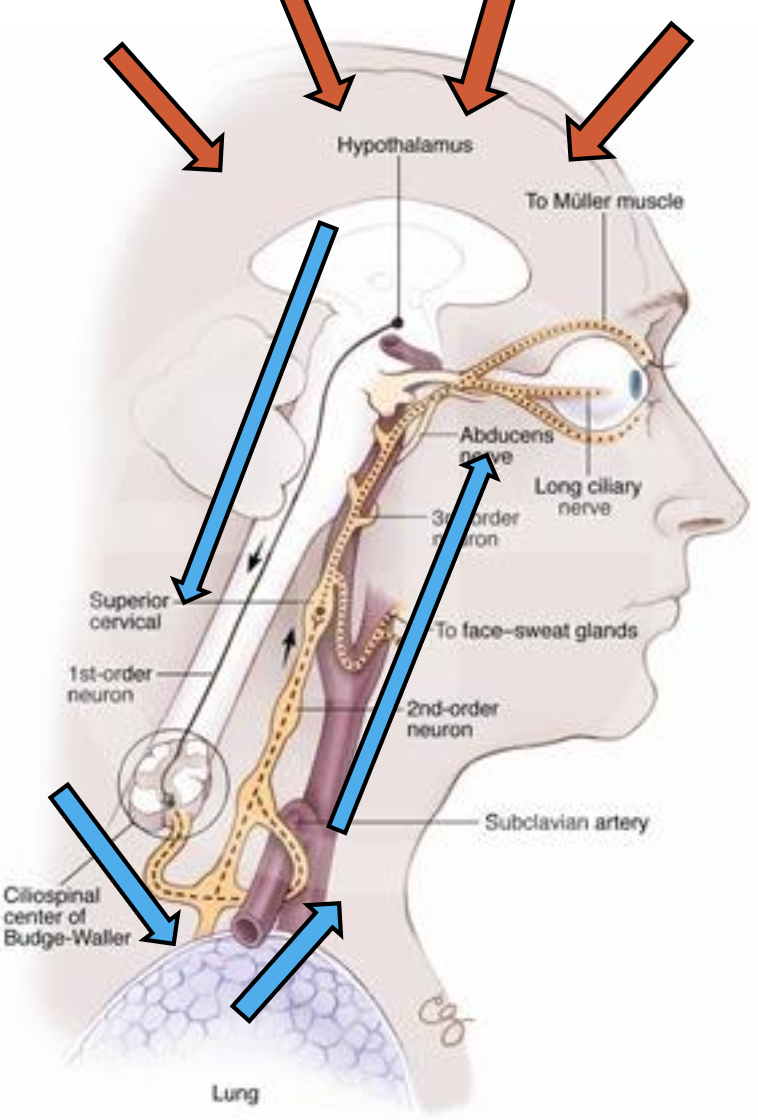
Sympathetic Nervous System Activation
The afferent neuron stimulates the hypothalamus. The efferent pathway consists of a three-order neuron synapsing process. Outline the pathway leading to Synapse #2.
2nd Order Neuron (Pre-ganglionic Neuron)
Exits spinal cord at C8–T1
Travels over apex of lung
Ascends through sympathetic chain in neck
Ends at the Superior cervical ganglion = ⭐ Synapse #2
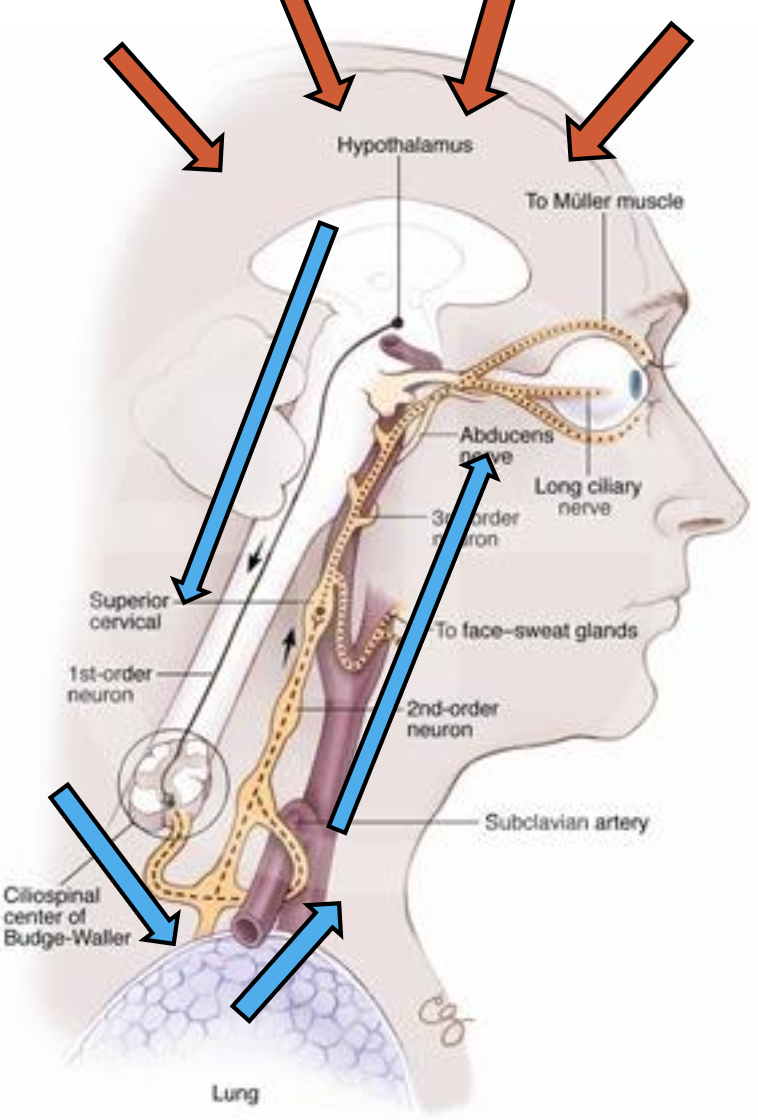
Sympathetic Nervous System Activation
The afferent neuron stimulates the hypothalamus. The efferent pathway consists of a three-order neuron synapsing process. Outline the pathway leading to Synapse #3/Dilation.
3rd Order Neuron (Postganglionic Neuron)
Begins at superior cervical ganglion
Follows internal carotid artery
Enters skull via carotid canal
Passes through cavernous sinus
Joins nasociliary branch of trigeminal nerve (CN V1)
Branch off and penetrate the eye as long posterior ciliary (LPC) nerves
LPC nerves innervate the iris dilator muscle
Iris dilator muscle contracts → dilation
What does a lesion anywhere in the SNS pathway primarily lead to?
Constricted, small pupil (miosis)
Besides the pupil, what other areas are affected by sympathetic nerve lesions?
Ipsilateral eyelid, orbit, and adjacent facial skin → Ptosis (drooping eyelid) & anhidrosis (loss of sweating)
What is Horner’s syndrome?
Miosis
Ptosis
Anhidrosis
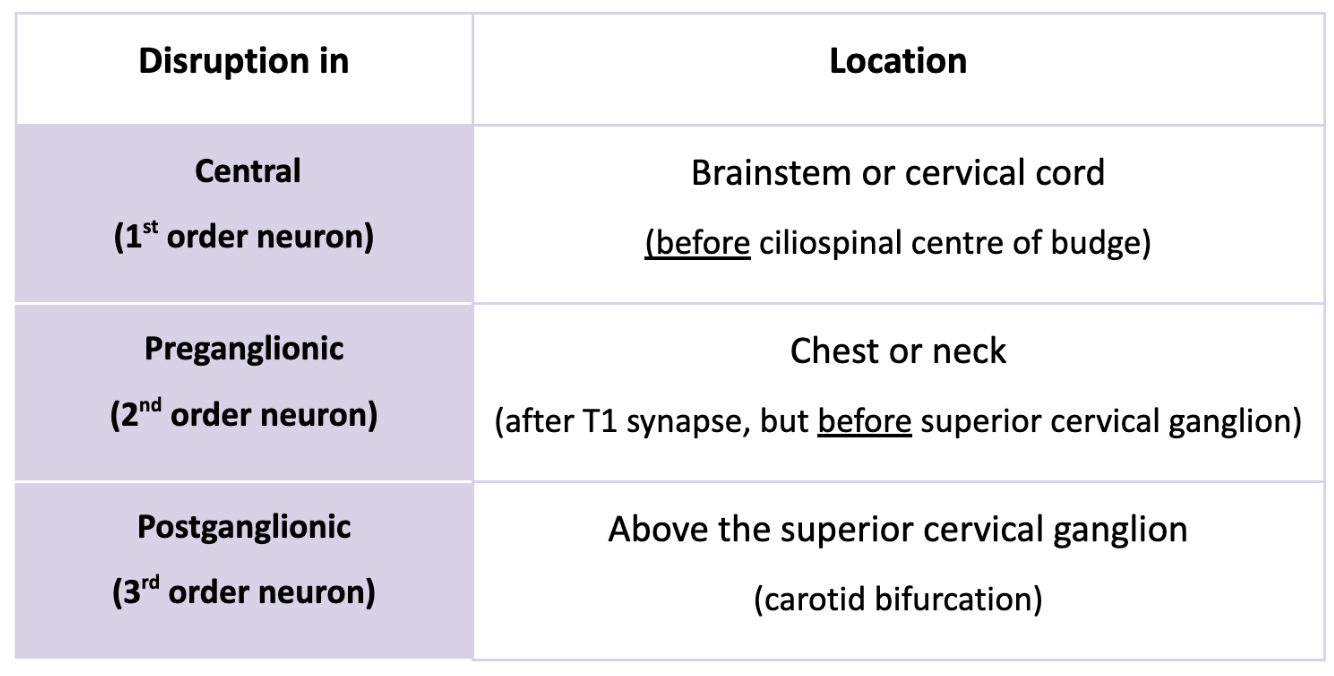
How can Horner’s syndrome be confirmed?
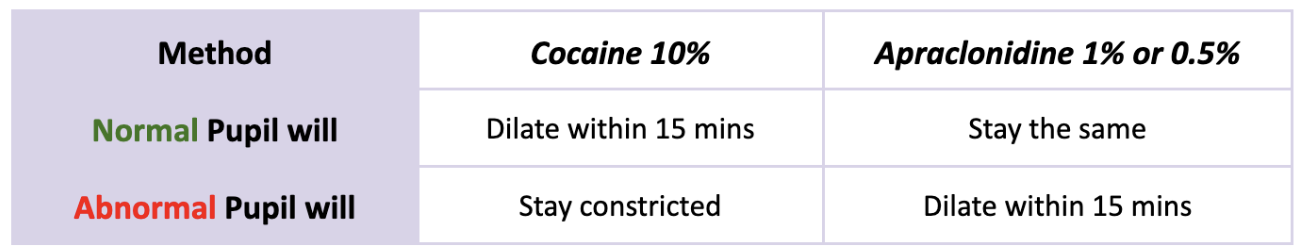
What are the 3 types of neuron lesions involved in Horner’s Syndrome, and where are they located?
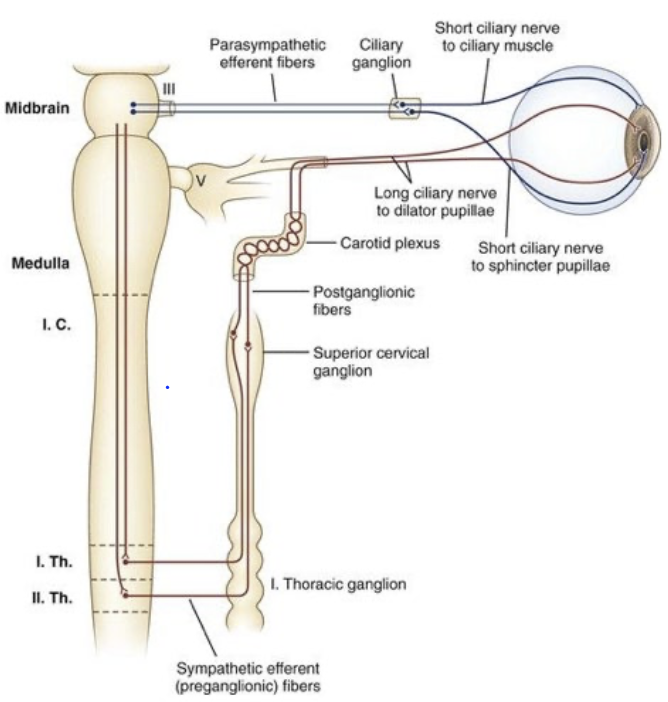
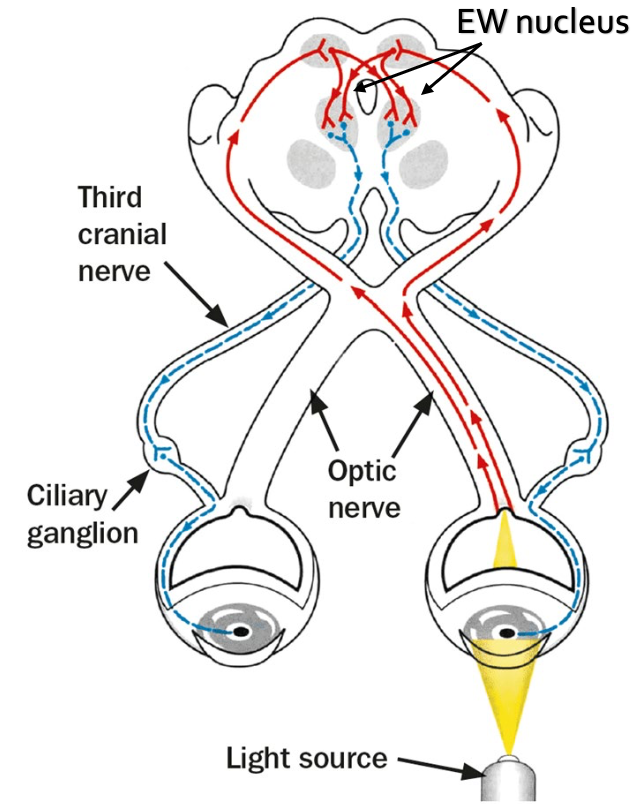
Parasympthetic Nervous System Activation
Outline the Afferent Pathway (Sensory Input).
Light stimulates the retina → impulse travels via:
Optic nerve (CN II)
Optic chiasm
Optic tract
End: Bilateral projection to midbrain (pretectal nucleus)
Parasympthetic Nervous System Activation
Outline the Efferent Pathway (Sensory Input).
1) 2nd-order neurons (neurons in pretectal nucleus) project to EW nuclei on both sides of midbrain
Now the pathway becomes efferent (motor)
2) Efferent fibers travel from EW nucleus to:
Oculomotor nerve (via the outer portion of CN III)
Ciliary ganglion
Short ciliary nerves
Constrictor (sphincter) pupillae muscle → Constriction
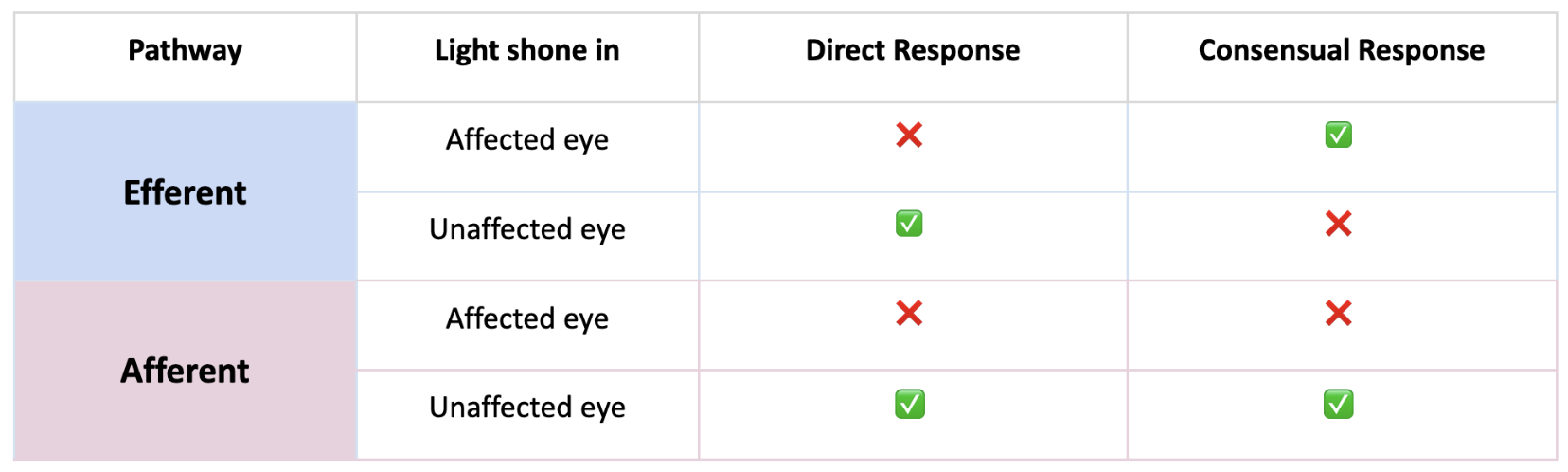
What does it indicate if one eye shows a reduced direct light response but a normal consensual response?
Efferent defect in that eye → problem with CN 3 (oculomotor nerve)
What does it indicate if both the direct and consensual responses are absent in one eye, but normal when the other eye is stimulated?
Afferent defect in that eye → problem with CN II (optic nerve) or optic tract
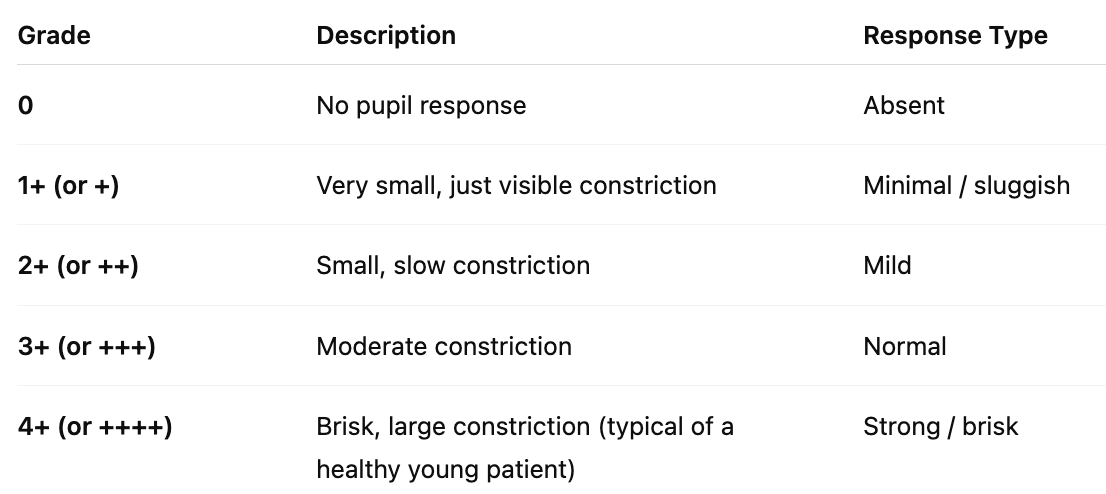
What is the grading scale used to test pupils?
→ 0 to 4+ scale is used to describe the strength and speed of the pupil’s response to light — both direct and consensual reflexes
Parasympathetic Nervous System
If there were a lesion anywhere along the efferent (motor) pathway of the light reflex, what would be affected?
CN III (Oculomotor)
Parasympathetic Nervous System
If there were a lesion anywhere along the afferent (sensory) pathway of the light reflex, what would be affected?
Optic nerve (CN II)
Parasympathetic Nervous System
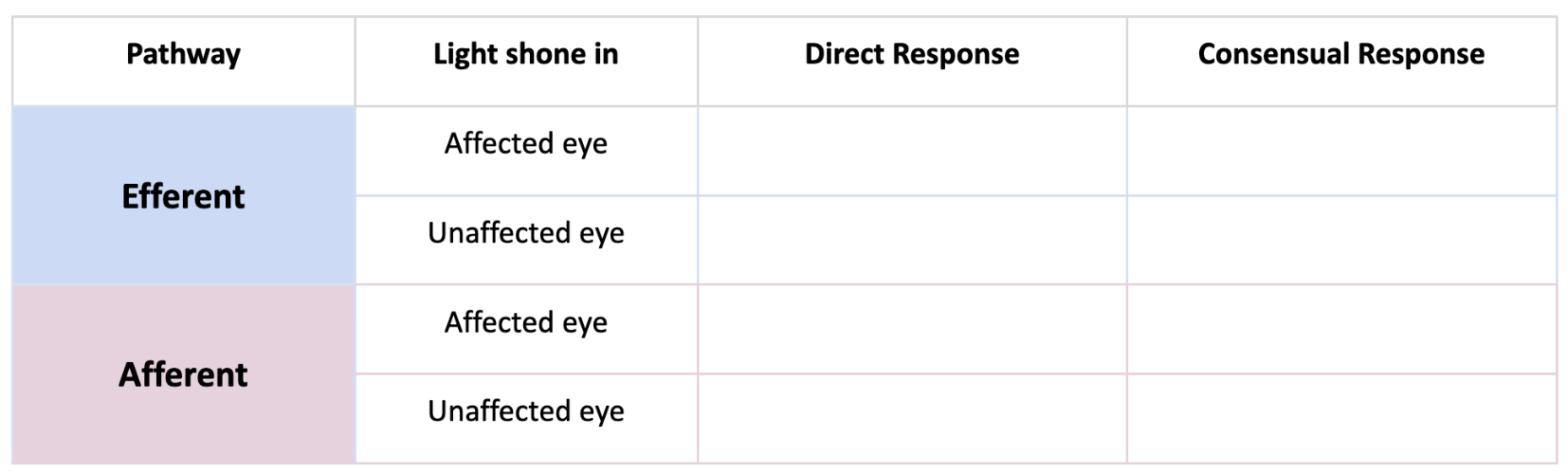
Fill out this table.
When is the swinging flashlight test performed?
→ used to detect RAPD /if there’s an issue in the afferent pathways
Method: You shine light alternately between both eyes, observing pupil constriction
If you were doing the swinging flashlight test, what would be the normal vs abnormal response?
Normal → both pupils constrict equally each time
Abnormal (RAPD) → when you swing the light to the affected eye, both pupils dilate slightly (b/c the brain perceives less light input)
What is RAPD a sign of?
Optic neuropathy
most commonly seen in optic neuritis (inflammed optic nerve)
When is the Light-Near Dissociation test performed?
If pupils fail to respond to light either during:
Direct and Consensual Response test
Swinging Flashlight test
What does it mean if a patient’s pupils don’t constrict to light but do constrict when focusing on a near target? What can this be caused by?
Positive Light-Near Dissociation (LND)
Afferent PNS pathway: broken
Efferent PNS pathway: intact
What can Positive Light-Near Dissociation (LND) be caused by?
Argyll Robertson Pupil (e.g., from neurosyphilis)
Lesion localized in the midbrain
Other midbrain-related pathologies