Patho Exam 2 - Cardiovascular
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
Hypertension
Consistent elevation of systemic arterial blood pressure with sustained systolic blood pressure of 130 mmHg or greater or diastolic pressure of 80 mmHg or greater
Primary (Essential) Hypertension
Genetic and environmental factors contribute to this type of hypertension, which forms 95% of cases
Secondary Hypertension
Caused by an underlying primary disease or drugs, accounting for approximately 5% of hypertension cases
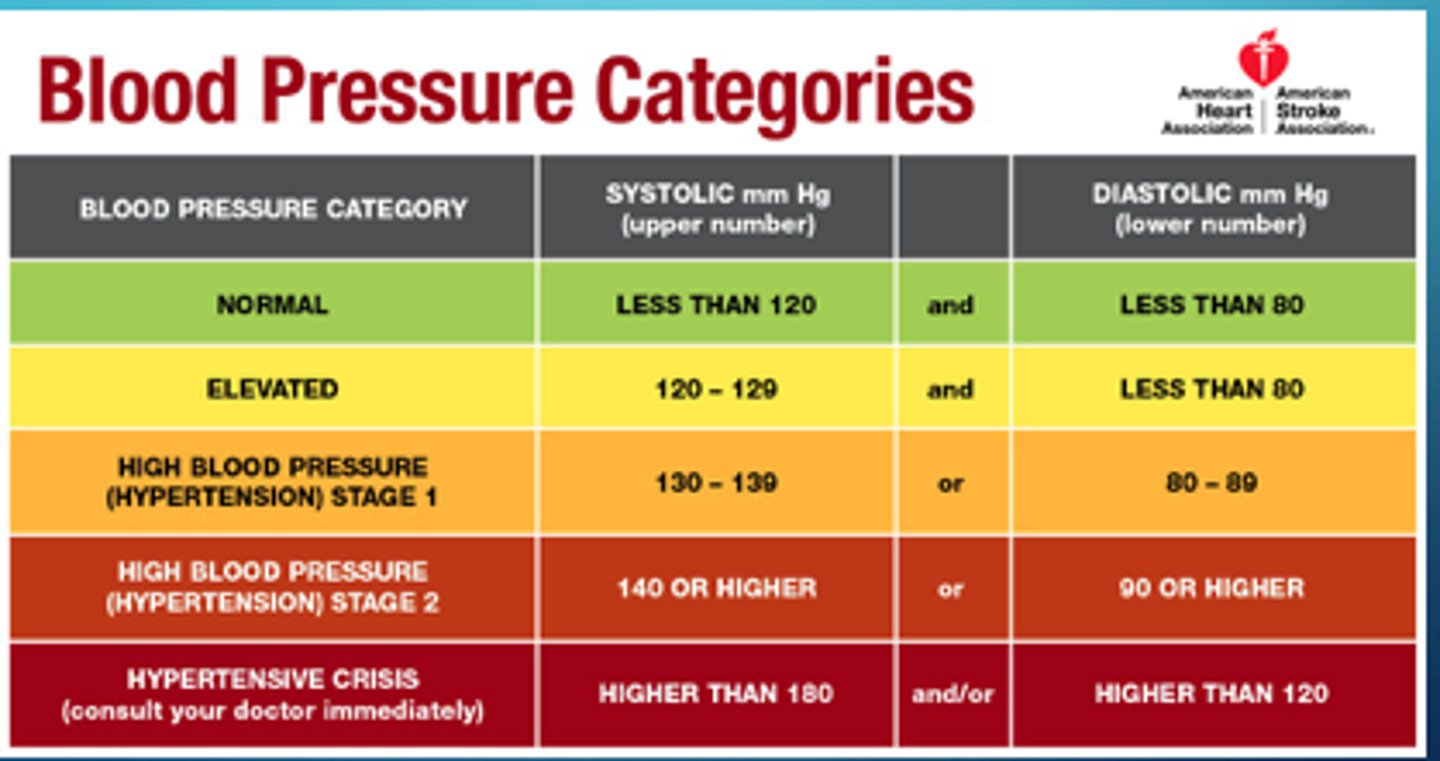
Blood Pressure categories
Normal: sys <120 and dia <80
Prehypertensive: sys 120-129 and <80
Stage 1 htn: sys 130-139 or dia 80-89
Stage 2 htn: sys >/= 140 or >/= 90
Hypertensive crisis: sys >180 or dia > 120
What are the main factors contributing to primary hypertension? (pathogenesis)
- Increase in arteriolar vasoconstriction leads to increase in total peripheral resistance leading to elevated blood pressure
- Overactivity of SNS and RAAS
- Alterations in natriuretic peptides
- Inflammation, endothelial dysfunction, obesity-related hormones, and insulin resistance
What happens over time in primary hypertension that leads to tissue damage?
Over time, damage to arterial walls occurs leading to a decreased blood supply which leads to ischemia and necrosis of tissues
Non-modifiable risk factors for hypertension
family history, gender (more common in middle age men and more common in women 65 yrs or older), age, ethnicity (more common in blacks)
Modifiable risk factors for hypertension
diet, sedentary lifestyle, obesity and weight gain, metabolic syndrome, elevated blood sugar levels, type 2 diabetes, dyslipidemia, alcohol, smoking
How is hypertension diagnosised?
It is measured on two or three different days, after 5 minutes of rest, with no smoking or caffeine intake for 30 minutes.
What is the baseline assessment and what does it rule out?
CBC and kidney panel (BUN and creatinine)
Urinalysis
Lipid profile
EKG
Echocardiogram
It rules out secondary hypertenstion
What are the two treatment paths for hypertension? Which one comes first?
Lifestyle changes should be done before pharmacological methods
Life style changes include (7)
Low sodium diet
DASH diet
Exercise
Weight loss
Decrease stress
Alcohol moderation
Education
Pharmacological agents used to treat hypertension (6)
Diuretics
ACE-inhibitors
ARB - Angiotensin-II receptor blockers
Calcium channel blockers
Aldosterone antagonists
Beta Blockers
What is atherosclerosis?
Thickening and hardening of arteries due to deposition of lipid-laden macrophages, leading to plaque formation (atheroma)
Angina Pectoris
Chest pain resulting from myocardial ischemia, characterized by transient deprivation of coronary blood supply
Three types of angina
Stable
Unstable
Prinzmetal
What is classic or stable angina?
Occurs on exertion
Transient substernal chest pain described as pressure, heaviness, squeezing, burning, or choking sensation. Pallor, diaphoresis, or nausea.
Short lasting (1-5 minutes)
relieved with nitroglycerin or rest
Severity and duration is an indication of progression
Physical assessment is often normal
Diagnostic tests for stable angina
Baseline labs
Electrocardiogram (EKG) - baseline
Exercise stress test
Treadmill
Nuclear/dobutamine if cannot tolerate exercise
Echocardiogram
CT scan and angiography
Cardiac catheterization
Treatment goals for stable angina
Relieve symptoms
slow progression of the disease
Reduce potential complications such as MI
Treatment medications for stable angina
Nitrates (nitroglycerin)
beta blockers
calcium channel blockers
statins (cholesterol control)
unstable angina
chest pain that occurs while a person is at rest and not exerting himself
Not relieved by nitroglycerin
Longer duration and lower threshold
Opposite of stable angina
Reversible myocardial ischemia without detectable myocardial necrosis
Myocardial Infarction
Irreversible damage to the heart muscle due to prolonged lack of oxygen supply, often caused by coronary artery obstruction
What is the most common cause of myocardial infarction?
Atherosclerosis
What is the clinical presentation of myocardial infarction?
History of chest pain (Intense and unremmitting for 30-60 minutes, Retrosternal and often radiating to neck, shoulder, jaws, and down to the left arm, described as squeezing, aching, burning)
Epigastric pain - a feeling of indigestion or fullness and gas
Nausea, vomiting, diaphoresis
Often occurs in the AM
Goals of treatment for MI include
Determine the presence or absence of a MI
Characterize locus, nature, and extent
Detect recurrent ischemia or MI
Detect early or late complications
Estimate prognosis
Laboratory test for MI
12-lead EKG - important tool in initial evaluation and triage
Cardiac biomarkers - troponin and CK-MB
CBC
Comprehensive metabolic panel
lipid profile
Management avenues for MI: Prehospital/extra mural
Get to the hospital ASAP. IV access. Supplemental O2 if SaO2 < 90%. Nitroglycerin. EKG and telemetry if available.
Management avenues for MI: ER
Targeted history and focused exam. 12-lead EKG within 10 min of arrival. IV access. Goal is to restore O2 supply and prevent further ischemia. Pain relief. Prevention and treatment of complications.
Management avenues for MI: Medical
O2, aspirin, nitrates (vasodilate decreasing demand), analgesia (morphine). Anti-hypertensive, statins. Reperfusion (fibrinolysis, anti-platelets).
Management avenues for MI: Interventional/Surgical
Percutaneous coronary intervention (balloon angioplasty). Coronary artery bypass graft (CABG). External counter pulsation (ECP).
Shock
Condition where the cardiovascular system fails to adequately perfuse tissues, leading to impaired cellular metabolism
STEMI
ST-elevation myocardial infarction, a classification of myocardial infarction based on EKG findings
Non-STEMI
Non-ST-elevation myocardial infarction, another classification of myocardial infarction based on EKG findings
Prinzmetal Angina
Variant/vasospastic angina occurring at rest or during sleep, often without evidence of cardiac or atherosclerotic heart disease.
Females greater than males
younger - ages 20-30
Heart Failure
Inability of the heart to pump enough blood to meet the body's needs, often a complication of other cardiopulmonary conditions leading to inadequate perfusion of tissues.
Risk factors for heart failure include
ischemic heart disease and hypertention
High-Output Heart Failure
Inability of the heart to supply the body with nutrients despite adequate blood volume and normal or elevated myocardial contractility
Anemia, beriberi (vitamin B1 deficiency), sepsis, hyperthyroidism
Malignant Hypertension
Severe hypertension leading to organ damage, a systemic complication of high blood pressure
Hypertensive Crisis
Sudden and rapid increase in arterial blood pressure, often life-threatening with end-organ damages
Resistant Hypertension
Hypertension that does not respond to treatment, posing challenges in management
Fatty Streak
Early stage of atherosclerosis characterized by the accumulation of lipid-laden macrophages in arterial walls
Fibrous Plaque
Advanced stage of atherosclerosis where fibrous tissue forms over fatty streaks, leading to arterial narrowing
Complicated Plaque
Atherosclerotic plaque with a fibrous cap that is prone to rupture, potentially causing thrombosis
Congenital Heart Disease
Heart abnormalities present at birth, affecting the heart's structure and function
Cardiogenic Shock
Inability of the heart to maintain cardiac output to circulation, leading to inadequate tissue perfusion. Caused by MI of left ventricle, cardiac arrhythmias, pulmonary embolus, cardiac temponade.
Hypovolemic Shock
Shock resulting from loss of circulating blood volume, leading to decreased tissue perfusion caused by hemorrhage, burns, dehydration, peritonitis, pancreatitis.
Distributive Shock
Shock caused by changes in peripheral resistance, leading to blood pooling in the periphery. Vasodilation
Neurogenic
septic
anaphylactic
Left-Sided Heart Failure
Heart failure affecting the left ventricle, leading to pulmonary congestion.
Known as congestive heart failure
Most common type
"left heart failure is a disease with symptoms"
What are the forward effects of left-sided heart failure?
Fatigue, weakness, dyspnea, exercise intolerance, cold intolerance
What are the compensatory mechanisms seen in left-sided heart failure?
Tachycardia and pallor, secondary polycythemia, daytime oliguria
What are the backup effects of left-sided heart failure?
Orthopnea, cough producing white or pink tinged phlegm, shortness of breath, paroxysmal nocturnal dyspnea, hemoptysis, rales
Right-Sided Heart Failure
Heart failure affecting the right ventricle, resulting in systemic fluid retention and signs like pedal edema and ascites
"Right heart failure is a disease with signs"
What are the forward effects (decreased output) of right-sided heart failure?
Fatigue, weakness, dyspnea, exercise intolerance, cold intolerance
What compensations can be seen in right-sided heart failure?
Tachycardia and pallor, secondary polycythemia, daytime oliguria
What are the backup effects of right-sided heart failure?
Dependent edema in feet, hepatomegaly and splenomegaly, ascites, distended neck veins, headache, flushed face
Diagnosis of heart failure
FACES of HF: Fatigue, Activity limitation, Congestion, Edema, Shortness of breath
Echocardiogram (gold standard) - shows heart anatomy
Plasma - BNP or NT-pro-BNP levels
X-ray - enlarged heart
Brain Natriuretic Peptides (BNP)
Hormones secreted by the heart in response to stretching of heart muscle cells, used as a diagnostic marker for heart failure
NT-pro-BNP
N-terminal pro-B-type natriuretic peptide, a biomarker for heart failure used in conjunction with BNP levels
Ejection Fraction
Percentage of blood pumped out of the heart's chambers with each contraction, a measure of heart function
Medical treatments for Heart Failure
Digoxin
ACE-Inhibitor
ARB - angiotensin-II receptor blockers
ARNI - Angiotensin receptor-neprilysin inhibitor
Ivabradine - pacemaker current inhibitor
Vericiguat - cardiac muscle relaxer and a novel agent
Spironolactone - potassium-sparing diuretic
Implantable cardioverter - defibrillator (pacemaker)
Troponin
Protein released into the bloodstream when heart muscle is damaged, used as a marker for myocardial infarction
Test of choice
Coronary Artery Disease
Any vascular disorder that narrows or occludes the coronary arteries leading to myocardial ischemia leading to myocardial infarction.
also called ischemic heart disease or coronary heart disease
Etiology of CAD
Atherosclerosis (most common cause)
Modifiable risk factors for CAD
Smoking, inactivity, hypertension, diabetes mellitus, obesity, excessive alcohol consumption, cholesterol management, and inflammation
Neurogenic (vasogenic) shock
Vasodilation owing to loss of sympathetic and vasomotor tone. Caused by pain and fear, spinal cord injuries, hypoglycemia
anaphylactic shock
systemic vasodilation and increased permeability owing to severe allergic reaction.
Caused by insect stings, drugs, nuts, shellfish
Septic shock
vasodilation owing to severe infection, often with gram-negative bacteria.
Caused by virulent microorganisms (gram-negative bacteria) or multiple infections.