MECHANISMS OF INFECTION
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
what are pathogens
disease causing organisms
fully virulent - possess virulence factors i.e. structures and systems that help pathogens cause disease via infection and damage of host tissues
show clonality
what are opportunistic pathogens
possess some virulence factors i.e. structures and systems that help pathogens cause disease via infection and damage of host tissues
often commensals
tend to cause problems in immunocompromised or a susceptible area e.g. wound
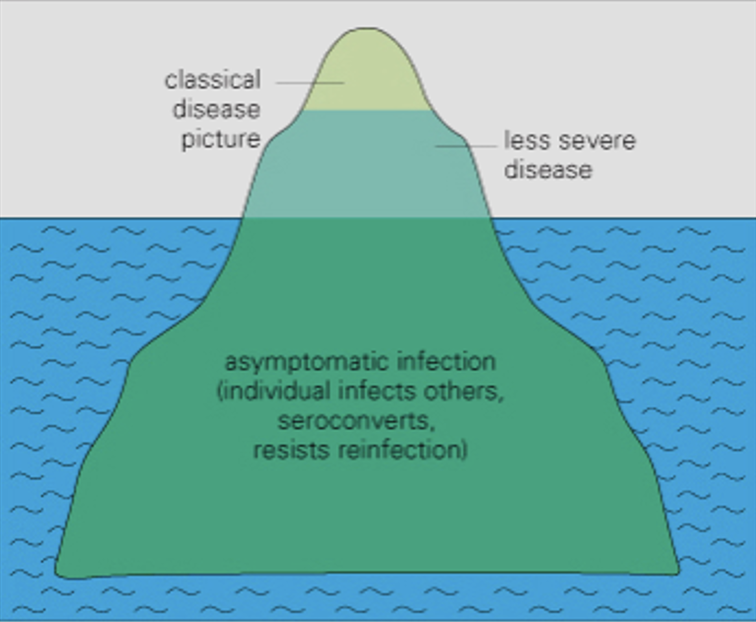
iceberg concept of disease
only a small portion of a disease is visible and detected e.g. in death, hospitalisation
the majority of people w a disease are asymptomatic and hidden/ undetected
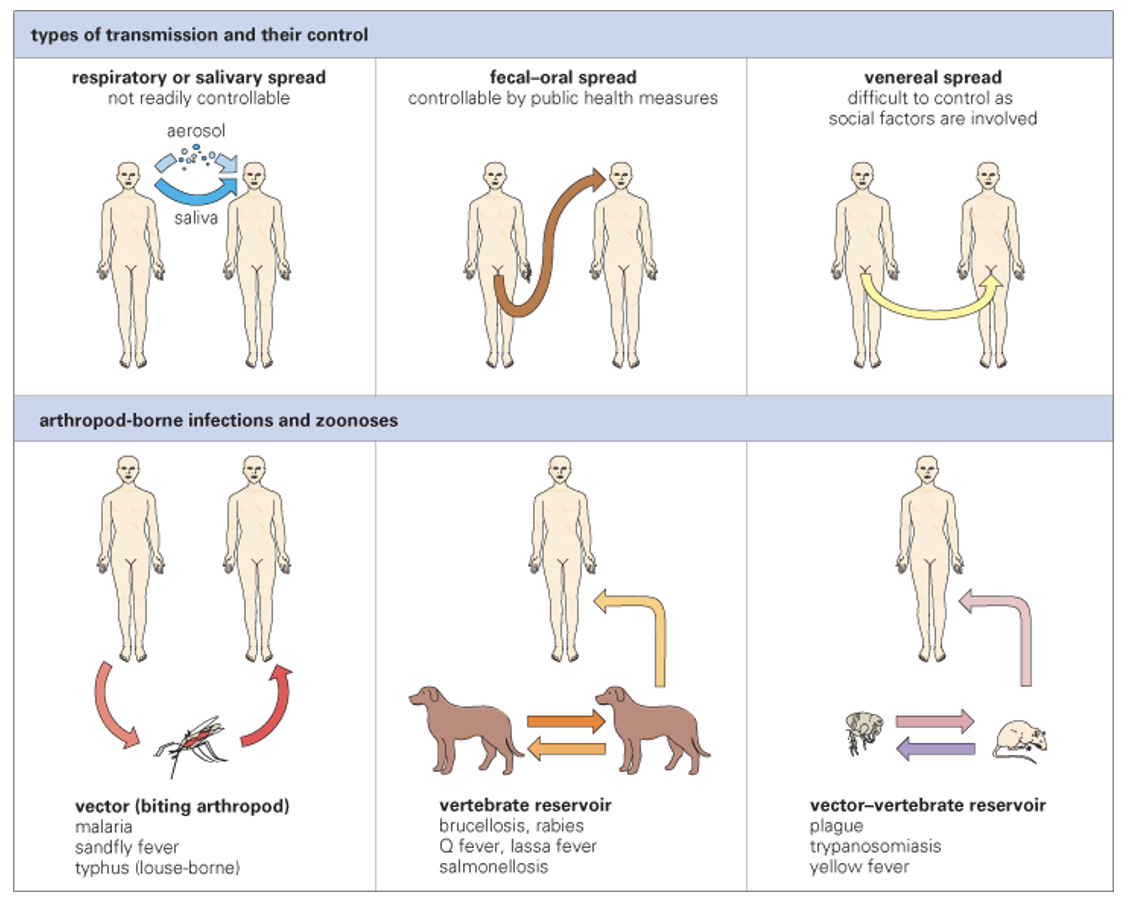
routes of transmission (6)
respiratory/ salivary
fecal/ oral
venereal spread - sexual contact
anthropod-borne infections and zoonoses
vector e.g. malaria
vertebrate reservoir e.g. rabies
vector-vertebrate reservoir e.g. yellow fever
define horizontal transmission and vertical transmission
horizontal transmission: microorganism is passed between individuals who are not related as parent and offspring (same generation) e.g. plague, influenza
vertical transmission: microorganism is passed from a parent to its offspring e.g. HIV, Hep B
what is colonisation and how does it lead to a bacterial infection
when bacteria are present on/ in body wo causing disease/ illness
colonisation » bacterial infection if balance between host and bacteria is disrupted, if opportunistic pathogens exploit host nutrients, if host has a weak immune system
requirements for colonisation and infection (6)
successful transmission
adhere to susceptible cells/ surface by pilli/ fimbriae, polysaccharide/ protein adhesins
grow on/ in host
local/ systemic spread
evade host defences
invade by subversion of the endocytic system
infectious dose threshold must be reached
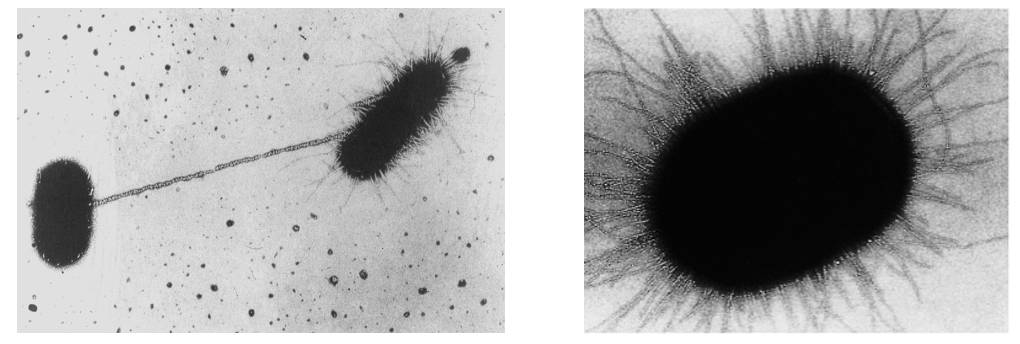
how do bacteria adhere to human cells
via pilli/ fimbriae
^ have adhesin molecules located at the tip
colonisation and infection: surface protein adhesion
surface proteins on pathogens help bacteria to adhere to host cells’ proteins/ glycoproteins and invade them
e.g. HIV binding to CD4 receptors
colonisation and infection: surface polysaccharide adhesion
polysaccharides act as molecular glue helping bacteria stick to surfaces and each other
important in biofilm formation - bacteria produce polysaccharides that help them adhere to surfaces
biofilms
heterogenous film of bacteria coating surfaces
primary colonisation: surface such as a plastic catheter
secondary colonisation: increased by extracellular polysaccharide and cell interactions
clinical significance of biofilms
causes increased antibiotic and immune resistance
resistance to macrophage enzymes
increased localised enzyme concentration promotes tissue damage
colonisation and infection: motility
motility aids colonisation
allows bacteria to spread from biofilm microcolonies and colonise other tissues
penetrates mucous blanket - moist, mucus-covered lining in the nose that traps harmful particles and moves them out of the body
penetrates intercellular junctions - special regions of contact between plasma membranes of adjacent cells
what is the endocytic system
series of processes involving uptake and delivery of materials into and out of a cell
main types: pinocytosis, phagocytosis, receptor-mediated endocytosis
colonisation: subversion of the host’ endocytic system
bacterial ligand binds to host receptor causing plasma membrane to zipper around bacterium
E.coli:
bacteria pilli binds to glycolipids on host cell surface - helps bacteria generate biofilm-like structures on and inside host
when pilli binds, a pedestal (actin-rich protrusion) is formed beneath which anchors E.coli to host
cell effectors (virulence factors) are injected via pedestal using secretion needles
colonisation: what is an infectious dose threshold
the minimum number of pathogens required to cause an infection - varies between diseases
evasion of host defences (4)
blocking and degradation of immune molecules
avoid phagocytic killing
hide from adaptive immune response
combat physical barriers
complement molecules
complement molecules work together to identify and eliminate pathogens:
opsonization: complement molecules coat pathogens with opsonins to mark them for phagocytosis
inflammation: complement molecules generate proinflammatory mediators to attract immune cells and activate mast cells
lysis: complement molecules assemble membrane attack complexes (MACs) that damage the plasma membranes of pathogens
evasion of host defences: blocking and degradation of immune molecules by Gram +ve and Gram -ve bacteria
Gram -ve: antigens block complement access to membrane
Gram +ve: capsule blocks complement access to membrane by masking surface components
evasion of host defences: avoid phagocytic killing (5)
organism releases toxins e.g. leukocidin produced by staphylocci causing phagocytes to die
organism possesses a capsule which prevents contact w phagocyte
organism escapes from phagolysosome into cytoplasm and replicates within phagocyte
organism resists killing within phagosome by producing antioxidants
organism inhibits fusion of phagosome and lysosome to form a phagolysosome e.g. TB so it survives for longer in macrophages
evasion of host defences: hide from adaptive immune response (6)
organisms can incapacitate T-cells e.g. HIV
organisms can vary their surface antigen e.g. influenza, meningitis, gonorrhoea - difficult to make vaccines for
organism can coat itself w host protein, alter their surface proteins, imitate general structure of host i.e. mimicry
organism can hide in privileged sites - areas of the body that are less likely to trigger immune response
organism can produce a protein which prevents opsonization - coating of pathogens w opsonins to help immune cells identify
organism can degrade/ inhibit complement - network of proteins that work together to destory pathogens e.g. C5a protease of S.pyogenes stops signal to phagocytes
evasion of host defences: combat physical barriers
stomach acid is an example of a physical barrier
Helicobacter pylori activates its urease to convert urea » ammonia + CO2
ammonia neutralises stomach acid
many pathogens have an acid tolerance response (ATR) meaning they can survive in extreme acidic environments
E.coli uses amino acid decarboxylases (AADC) to keep cytoplasmic pH above dangerous levels