IMMUNITY - CHAPTER 9
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
What is adaptive immunity
antigen-specific immune response.
antigen must be processed + recognised first.
includes humoral and cellular immunity
Faster FUTUREE responses
humoral immunity
Involves B cells
Produces antibodies (target specific antigens)
Uses complement proteins
Works in extracellular fluid
It's an antibody-based response
cellular immunity
Uses T cells & macrophages to fight pathogens
Releases cytokines
No antibodies involved
what is lymph
Clear fluid like plasma
returns leaked fluid
transports lymphocytes/APCs,
site for lymphocyte maturation.
what happens in lymph nodes during immune response
contain many B & T cells + macrophages filter lymph
Macrophages show antigens to T cells
APCs present antigens to Tᴴ cells
Lymphocytes multiply → nodes swell (early sign of infection)
Where do B and T cells mature?
B cells mature in bone marrow
RESPONSIBLE FOR HUMORAL IMMUNITY
T cells mature in thymus
RESPONSIBLE FOR CELL MEDIATED IMMUNITY.
lymphatic system
made of lymph, lymphatic vessels, primary and secondary lymphoid organ/tissue
main lymphocytes
T cells, B cells and natural killer cells
primary lymphoid organs and secondary lymphoid organs
primary - Bone marrow and thymus.
secondary - Spleen, lymph nodes, tonsils, adenoids, appendix, Peyer’s patches.
immunity, adaptive and innate
resistance to infectious disease
innate immunity is natural, non specifc, fast and no memory
adaptive immunity is aquired, specifc, slow and has ;memory’
antigens (more detail)
molecule that triggers immune response
epitope is The part of an antigen recognized by antibodies or T/B cells.
^specifc part of antigen that antibody binds
cells involved in cell mediated immunity
helper T cells, Cytotoxic T cells, Memory T cells
helper T cells : cell mediated immunity
do not directly kill cells
release cytokines to activate macrophages, B cells, and cytotoxic T cells,
Cytotoxic T cells : cell mediated immunity
Kill infected, cancerous, or foreign cells directly.
Memory T cells :cell mediated immunity
Persist after infection to provide fast responses if re-exposed.
How do helper T (TH) cells get activated?
1. APCs present antigens on MHC II to TH cells.
2. CD4 (t helper) binds MHC II (activates TH cell.)
3. TH releases cytokines →
apc
Pathogen engulfed by antigen-presenting cell (e.g. macrophage).
Pathogen broken down into antigen fragments.
Antigen binds to MHC II inside the cell.
Helper T cell binds to presented antigen → activates immune response.
cell mediated pathway
cell infected w bacteria/virus. foreign antigen fragments r created within cells
MHC 1 binds antigen fragment
MHC protein presents antigen to cytotoxic T cell
if cell (not wbc) is infected w pathogen, antigens can be taken from pathogen and be presentd to MHC 1
cytotoxic t cells bind to antigens presented
cytotoxic t cells recognise cancerous cells
activated cytotoxic t cells eliminate infected cells directy
:
How do cytotoxic T (TC) cells get activated?
Infected normal cells present antigens on MHC I to TC cells.
CD8 binds MHC I → activates TC cell.
TC cells kill infected cells directly.
humoral immunity cells
Plasma cells, Memory B cells
Plasma cells
Plasma cells -
after activation, B lymphocytes → plasma cells (bc B cell receptors bind to specific antigen)
produce antibodies specific to antigen
Memory B cells
stay long time in lymphoid tissue
can differentiate into plasma cells during re- infection
clonal selection
antigen selects B cell (bc receptors match), that will eliminate the antigen,
What is clonal expansion?
Rapid division of selected B cells to fight an infection.
plasma and memory B cell production, positives of memory B cell production
as well as plasma cells, memory B cells also produced.
when particular pathogen comes into contact, antibody production is faster
using memory, skip clonal selection and go straight to clonal expansion.
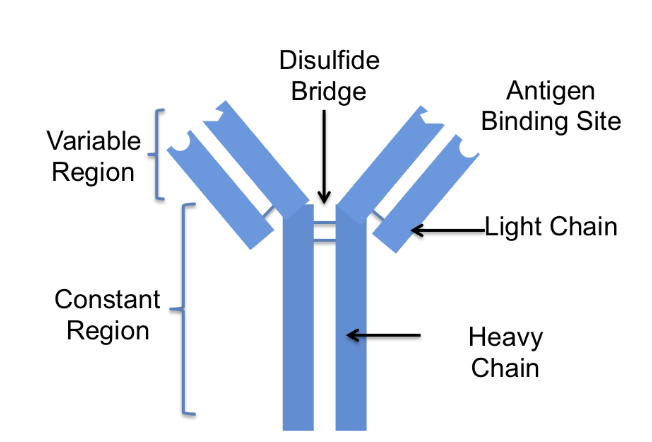
Antibodies (aka immunoglobin)
Made by B cells to neutralise pathogens
4 polypeptides: 2 heavy, 2 light
Forms Y shape
Tips of Y (variable region) bind to antigen
What are 5 main functions of antibodies?
Neutralisation, agglutination, opsonisation, precipitation, complement activation.
Neutralisation (toxins vs pathogens)?
Toxins: antibodies bind to toxin, block action.
Pathogens: antibodies bind to surface antigens of pathogens, block entry into host cells.
agglutination
Antibody clumps/binds to antigens
activates phagocytes + complement cascade
precipitation
Antibodies bind soluble antigens → becomes precipitate, so they drop out of solution.
antibody opsonisation
antibodies Mark pathogen for phagocytosis.
What are the five classes of antibodies?
IgG, IgM, IgA, IgE, IgD
What does IgG do?
Main antibody in blood, long-term immunity.
What does IgM do?
First antibody produced in infection.
What does IgA do?
Found in mucosal areas (gut, airways).
What does IgE do?
Involved in allergic reactions.
What does IgD do?
activate B cells by detecting antigens.
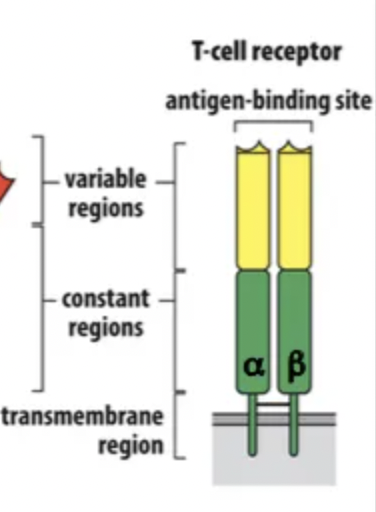
T cell receptors
On T cells;
recognises antigens bound on MHC.
has 2 peptide chains, 1 binding site.
immunological memory
First time b/t cell meets antigen = primary immune response
Second encounter (same situation) = secondary response (mainly IgG)
secondary response is Faster & stronger due to memory B and T cells made from primary response
immunity - source of antibodies and gaining immunity
source of antibodies
active immunity
passive immunity
gaining immunity
natural immunity
artificial immunity
passive immunity
antibodies aquired by a person from external source
offers immediate, not long term immunity
natural immunity - passive
antibodies enter person naturally
e.g. antibodies from mother (placenta or breast milk)
natural immunity - artifical
antibodies injected (e.g. antivenom, hepatitis A IgG)
➡ Provides immediate but short-term protection (no memory)
natural immunity - Active immunity
antibodies produced by an individuals own adaptive immune system.
types of active immunity
Natural: infection triggers B cells to produce antibodies
Artificial: vaccination stimulates antibody production
➡ Slower onset but long-term (memory B and T cells formed)
vaccine
uses weakened/dead pathogens to trigger antibody production, protecting against future infections.
4 types of vaccine
Live attenuated , Inactivated/killed, Toxoids, Sub-unit
Live attenuated
strong, long-lasting (e.g. MMR)
Inactivated/killed
weaker, may need boosters (e.g. rabies)
Toxoids
inactivated toxins (e.g. tetanus)
Sub-unit
only parts of pathogen, weakest (e.g. HPV)
Why do live attenuated vaccines provide stronger immunity than inactivated vaccines?
They produce stronger, longer-lasting immunity than inactivated vaccines, which often need boosters or multiple doses (2-3).