Ch 9 The Muscular System
1/79
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
Major characteristics of skeletal muscle
•Cell shape: Very long and cylindrical
•Nucleus: multiple nuclei, peripherally located
•Striations: yes
Cellular unit: fiber
Major characteristics of smooth muscle
•Walls of hollow organs, blood vessels, eye, glands, skin.
•Functions: propel urine, mix food in digestive tract, dilating/constricting pupils, regulating blood flow.
•In some locations, autorhythmic.
•Controlled involuntarily by endocrine and autonomic nervous systems.
Cell shape: Spindle-shaped
•Nucleus: single, centrally located
•Cell to cell attachments: Gap junctions join some visceral smooth muscle cells together
•Striations: no
•Caveolae: indentations in sarcolemma; may act like T tubules.
• Dense bodies instead of Z disks as in skeletal muscle that actin attached to; also have noncontractile intermediate filaments.
Major characteristics of cardiac muscle
•Heart (only in the heart): major source of movement of blood.
•Autorhythmic.
•Controlled involuntarily by endocrine and autonomic nervous systems.
Cell shape: Cylindrical and branched
•Nucleus: single, centrally located
•Cell to cell attachments: Intercalated disks join cells to one another, and gap junctions, these allow action potentials to pass from 1 cell to another (Action potentials of longer duration and longer refractory period)
•Striations: yes (means lots of sarcomeres and proteins)
•Don’t want all or nothing (think tube of tooth paste)
Functions of muscular system
Movement
2. Maintain posture
3. Respiration
4. Production of body heat
5. Communication
6. Heart beat
7. Contraction of organs and vessels
Four functional properties of muscle tissue
•Contractility: ability of a muscle to shorten with force.
•Excitability: capacity of muscle to respond to a stimulus (usually from nerves), all about action potential, negative to positive to negative again
•Extensibility: muscle can be stretched beyond it normal resting length and still be able to contract.
•Elasticity: ability of muscle to recoil to original resting length after stretched.
Describe the connective tissue components of skeletal muscle
Endomysium - surrounds each individual muscle fiber
Perimysium - groups muscle fibers into bundles called fascicles
Epimysium - surrounds entire muscle
•Motor neurons stimulate skeletal muscle contraction.
Blood supply and innervation of skeletal muscle
•An artery and 1 to 2 veins extend with a nerve through the C T layers.
•Extensive capillary beds surround muscle fibers.
Origin of muscle fibers
•Develop from fusion of myoblasts, resulting in large, multinucleated muscle cells.
•Number of fibers remains relatively constant after birth; muscles get larger due to hypertrophy of muscle fibers.
Hypertrophy
Stimulates protein synthesis, weight bearing activities makes muscles bigger
Atrophy
Loss of protein, no weight bearing (paralysis)
I band
No myosin
A band
Equal in length to myosin
H-zone
No actin
M-line
Right down center
Steps of sarcomere contraction
Ca becomes available (from SR)
Bind to troponin
Shift in tropomyosis to rotate
Open the bind site of actin
Full interaction between actin and myosin
Sarcomere relaxation
Remove the Ca with Ca pumps (requires ATP)
Intervation
Nervous system communication to muscle
What is a neuron potential (neuron)
Difference in electrical charge across the membrane of a neuron
What is a chemical potential (neuromuscular)
Energy a molecule has due to its concentration gradient across a membrane
How does the signal pass the sarcolema
Action potential: An action potential (electrical signal) travels along the motor neuron and reaches the neuromuscular junction, where it triggers the release of acetylcholine (ACh)
Depolarization
T-tubules: The action potential then travels down the T-tubules (invaginations of the sarcolemma), allowing the signal to reach deeper parts of the muscle fiber
Calcium release: The action potential activates the sarcoplasmic reticulum (SR), causing it to release calcium ions
Contraction: The calcium ions enable the interaction between actin and myosin filaments, leading to muscle contraction
Single motor unit
Single signal sent from brain to activate muscle, all or nothing, depolarization vs repolarization, contraction vs relaxation
Rules for neuromuscular junction
•As long as the impulse is “on” release Ca and contract muscle continuously
•If “off” no Ca, no impulse, but still contraction because there’s Ca in muscle still
•Stoping release and pumps do not release Ca anymore
Action potential
•Starts as an electrical signal, converts to chemical signal when gets inside
How an action potential causes a contraction with a neuromuscular junction
Starts in brain at rest
Depolarization (opens one channel at a time)
Ca comes in
Ach is released
Ach binds to receptor
Causes voltage change in sarcolema
Opens sarcolemas gate to open
Binds to troponin
Contracted
How an action potential causes relaxation with a neuromuscular junction
Starts in the brain (voluntary)
Relaxation - depolarization (0 - -70mv)
Ca gates close one at a time
Na and Ca are pumped out (always are anyway)
Achase (enzyme) eats (digests) Ach
Components of a muscle fiber
Sarcolema, transverse tubules (T tubules), sarcoplasmic reticulum, triad, myofibrils, myofilaments
Sarcolema
Plasma membrane; surrounds sarcoplasm(cytoplasm)
Transverse tubules (T tubules)
Inward folds of sarcolemma; project into the interior of muscle cell
Sarcoplasmic reticulum (S R)
Specialized smooth endoplasmic reticulum; stores calcium
Triad
Two terminal cisternae and their associated T tubule form a triad
Myofibril
Bundles of protein filaments (myofilaments) that cause contraction, also composed of repeating units called sarcomeres. Mechanical component structures allow muscles to contract.
Sarcomere
Functional unit of muscle contraction
Myofilaments
Individual protein filaments that make up myofibrils. Mechanical component structures allow muscles to contract.
Types of myofilaments
•Actin (thin) myofilaments.
•Myosin (thick) myofilaments.
•Myofilaments arranged into orderly units called sarcomeres.
Actin (thin) myofilaments
•Two strands of fibrous (F) actin form a double helix extending the length of the myofilament; attached at either end at sarcomere
Myosin (thick) myofilament
•Many elongated myosin molecules shaped like golf clubs.
•Molecule consists of myosin heavy chains wound together to form a rod portion lying parallel to the myosin myofilament and two myosin heads that extend laterally.
•Myosin heads: can bind to active sites on the actin molecules to form cross-bridges
Diagram of myofilaments in a sarcomere
🚨
How does the sliding filament model explain the contraction of muscle fibers
—Actin myofilaments sliding over myosin to shorten sarcomeres and contract muscle
—During relaxation, sarcomeres lengthen because of some external force, like contraction of antagonistic muscles.
What happens to the A band, I band and H zone during contraction
A band: stays the same (because its the thick myosin filaments)
I band: shortens (because its thin actin filaments)
H zone: may disappear (because it is the area with zero overlap between thick and thin filaments)
Resting membrane potential
—Membrane voltage difference across membranes (polarized).
•Inside cell more negative due to accumulation of large protein molecules. More K* on inside than outside. K* leaks out but not completely because negative proteins hold some back.
•Outside cell more positive and more Nat on outside than inside.
•Nat/K* pump maintains this situation.
—Must exist for action potential to occur.
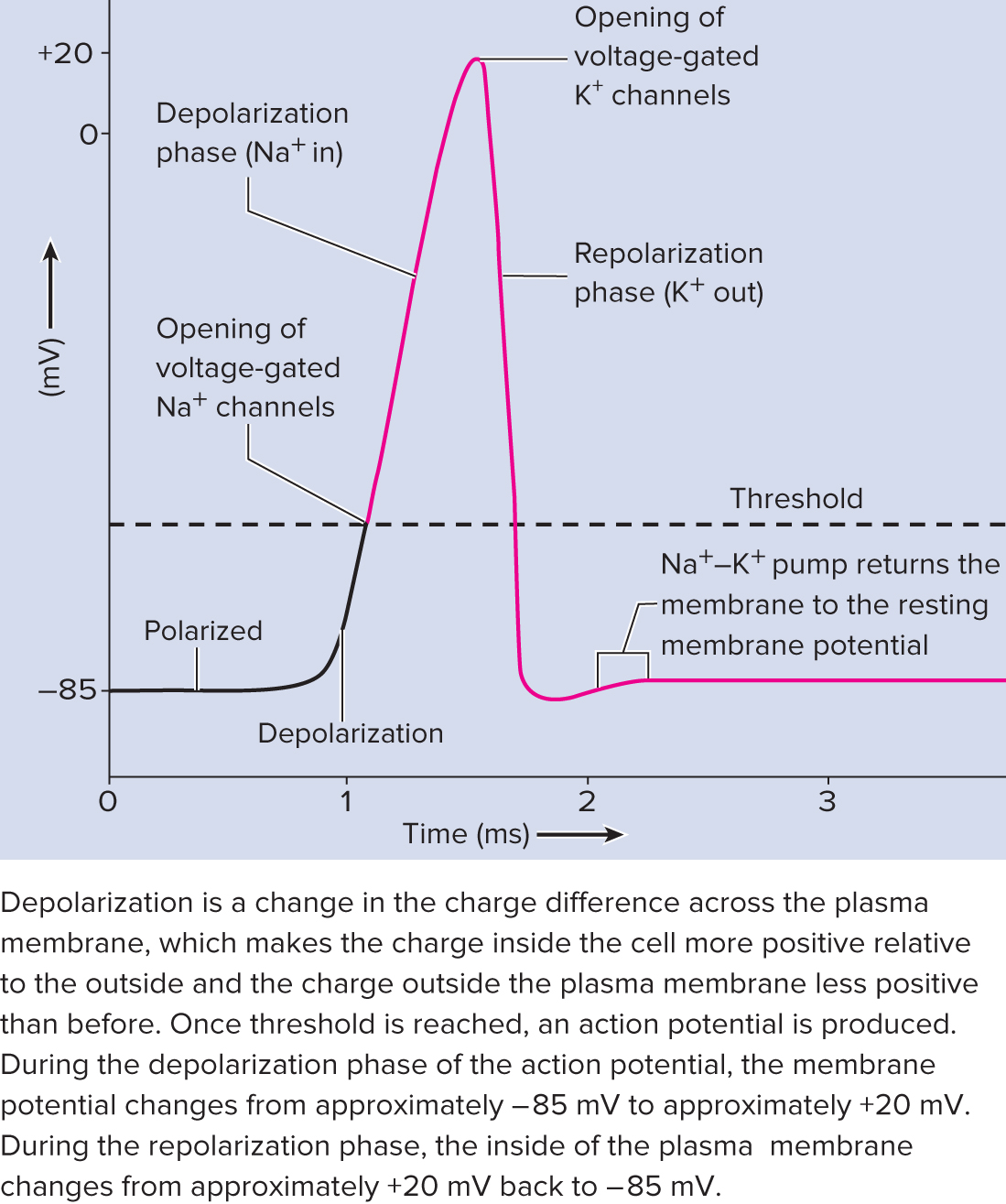
Role of ion channels in the production of an action potential
Resting (membrane potential) - 70 mv, Na and K channels are closed, some K leaks through, making inside cell more negative
Depolarization - 0 mv, Na channels open (chain reaction/one channel opens at a time), Na diffuses into cell, fully contracted because more positive now
Repolarization - Na channels close, return of resting membrane potential (at first it drops lower than original, then pumps even it out again)
Action potential graph
If a muscle is already contracted, can I contract it more or again?
No, cannot depolarize again until we have something to contract
All-or-nothing principle
As it pertains to action potentials, if threshold is reached, the cell will respond completely
Describe the structure of a neuromuscular junction
🚨
How is an action potential transmitted across the junction
When an action potential reaches the presynaptic terminal of a motor neuron, it causes voltage-gated Ca2+ channels in the presynaptic membrane to open. As a result, Ca2+ diffuse into the axon terminal.
Explain the events of excitation/contraction coupling
•Links electrical and mechanical components of contraction.
•Action potential produced on sarcolemma - propagated into T tubules - calcium channels on S R terminal cisternae open - calcium enters sarcoplasm, binds troponin - muscle contraction.
Cross-bridge movement
ATP dependent
Conditions needed for muscle relaxation
3 ATP dependent steps
1. Sodium-potassium pump transports Na* out of the muscle fiber and K+ into the muscle fiber to return to and maintain resting membrane potential.
2. ATP is required to detach the myosin heads from the active sites for the recovery stroke.
3. ATP is needed for the active transport of Ca?* into the sarcoplasmic reticulum from the sarcoplasm.
What is a muscle twitch
The response of a muscle fiber to a single action potential along its motor neuron
Phases of a muscle twitch
•Lag or latent – from the stimulus to the beginning of the contraction.
•Contraction – released and cross-bridging cycling occurs.
•Relaxation – returns to SR and muscle fiber returns to precontraction length.
Types of muscle contractions
Isometric: no change in length but tension increases (postural muscles of body)
Isotonic: change in length but tension constant
Describe a motor unit
A single motor neuron and all muscle fibers innervated by it.
How do motor unit numbers affect muscle control
•Large muscles have motor units with many muscle fibers.
•Small muscles that make delicate movements contain motor units with few muscle fibers.
How do whole muscles respond in a graded fashion
Depending on the force generated in the individual muscle fibers.
How can a fiber contract with more force
Increasing the number of cross-bridges
Factors are:
•Frequency of stimulation
•Muscle fiber diameter
•Muscle fiber length at the time of contraction
How can the force of contraction be increased
By a larger muscle fiber in diameter (this is because larger diameter fibers have more myofibrils and therefore can form more cross-bridges which provides more force of contraction)
Fatigue
•Definition: Decreased capacity to work and reduced efficiency of performance, consumption/loss/lack of ATP
•As soon as a muscle fiber contracts it relaxes, but by the time it relaxes it is charged up and ready to contract again. After awhile we run out of ATP (fatigue) so we can’t contract anymore
What do cells need to survive
•Oxygen
•Muscle fatigue - can’t replace ATP with aerobic so use anaerobic, longer muscles stay in anaerobic more lactic acid (felt through pain/soreness)
Summarize what occurs in treppe
It’s a phenomenon observed in muscle tissue where consecutive stimulations (without allowing them to fully relax) result in progressively stronger contractions until a plateau is reached
Explain multiple-motor-unit recruitment
Strength of contraction depends upon recruitment of motor units (a muscle has many motor units)
Describe wave summation in terms of incomplete tetanus and complete tetanus
•Wave summation: repeated muscle contractions occur so rapidly that each new contraction builds upon the tension from the previous one, progressively stronger contractions
•Incomplete tetanus is when muscle stimulation occurs at a frequency where some relaxation occurs between contractions (like how you shouldn’t take a break on your run, because less ATP to use after break)
•Complete tetanus is the eventual progression if the stimulation frequency increases further, eliminating any relaxation phase
Explain the connection between the initial length of a muscle and the amount of tension produced
—Active tension: force applied to an object to be lifted when a muscle contracts.
—Active tension curve: active tension increases or decreases as a muscle fiber changes in length
How is muscle tone maintained
Constant tension by muscles for long periods of time; due to small percentage of all motor units contracting out of phase with one another
What is a slow-twitch muscle fiber
•It is type 1
•Contract more slowly, smaller in diameter, better blood supply, more mitochondria, more fatigue-resistant than fast-twitch, large amount of myoglobin.
•Postural muscles, more in lower than upper limbs. Dark meat of chicken.
What is a fast-twitch muscle fiber
•Type 2
•Respond rapidly to nervous stimulation, contain myosin that can break down A T P more rapidly than that in Type I, less blood supply, fewer and smaller mitochondria than slow-twitch.
•Lower limbs in sprinter, upper limbs of most people. White meat in chicken.
•Comes in oxidative and glycolytic (anaerobic) forms.
Describe how training can increase the size and efficiency of both types of muscle fibers
Effects: Change in size of muscle fibers.
—Hypertrophy: increase in muscle size.
—Atrophy: decrease in muscle size.
How does muscle metabolism cause normal body temperature
•Exercise: metabolic rate and heat production increase, anytime we use ATP we produce heat
•Post-exercise: metabolic rate stays high due to oxygen debt
How do muscles respond to changes from normal body temperature
•Excess heat lost because of vasodilation and sweating.
•Shivering: uncoordinated contraction of muscle fibers resulting in shaking and heat production.
ATP
Used in muscle contraction (break cross bridges between actin and myosin)
Pumps also use ATP
Describe 2 of the sources of energy for ATP production in muscles
Anaerobic respiration
•No oxygen or mitochondria and results in breakdown of glucose to yield A T P and lactic acid
Aerobic respiration
•Requires oxygen and mitochondria and breaks down glucose to produce A T P, carbon dioxide and water
•More efficient than anaerobic
Difference between oxygen deficit and excess postexercise oxygen consumption
•Oxygen deficit refers to the initial period during exercise where the body's oxygen demand exceeds the available supply, forcing it to rely on anaerobic energy systems
•Excess post-exercise oxygen consumption (EPOC) is the elevated oxygen consumption that occurs after exercise as the body restores itself to its resting state, essentially "paying back" the oxygen debt created during the deficit phase
Compare the mechanisms involved in the major types of muscle fatigue
—Acidosis and A T P depletion due to either an increased A T P consumption or a decreased A T P production.
—Oxidative stress, which is characterized by the buildup of excess reactive oxygen species (R O S; free radicals).
—Local inflammatory reactions
•Physiological contracture - state of fatigue where due to lack of A T P neither contraction nor relaxation can occur.
•Psychological fatigue – most common type; comes from the central nervous system rather than the muscles
Contrast physiological contracture and rigor mortis
Physiological contracture: the abnormal, permanent shortening and hardening of muscle tissue, leading to restricted joint mobility and potential deformities
Rigor mortis: development of rigid muscles several hours after death. No ATP, so muscles can’t relax, stay contracted. Ends as tissues start to deteriorate.
Steps of smooth muscle contraction
•If the phosphate is removed from myosin while the cross-bridges are attached to actin, the cross-bridges release very slowly. This explains how smooth muscle is able to sustain tension for long periods and without extensive energy expenditure. This period of sustained tension is often called the latch state of smooth muscle contraction.
•Exhibits relatively constant tension: smooth muscle tone
How do smooth and skeletal muscle contraction differ
•Smooth muscle contraction: involuntary, slower contraction speed (because no striations), ability to sustain contractions for longer periods, a different mechanism for calcium regulation
•Skeletal muscle contraction: voluntary and rapid, with clear striations (which create greater tension) due to the organized arrangement of actin and myosin filaments
Compare the 2 types of smooth muscle as to their action and locations
•Single-unit (also called visceral) smooth muscle, which contracts as a single unit due to gap junctions between cells and is found in most internal organs like the digestive tract and uterus
•Multi-unit smooth muscle cells contract individually and are located in areas like the iris of the eye and arrector pili muscles of the skin, allowing for more precise control over muscle contractions
Explain how smooth muscle activities are regulated
• Ca2+ required to initiate contractions; binds to calmodulin which regulates myosin kinase. Cross-bridging occurs.
• Relaxation: caused by enzyme myosin phosphatase.
Relate the events of cross-bridge movement to muscle contraction
The repeated formation and breaking of cross-bridges pull actin filaments inward, causing the sarcomere (and muscle fiber) to shorten — which is muscle contraction
Discuss the production of an action potential, including repolarization and depolarization
The action potential is a wave of electrical change: depolarization (Na⁺ in) makes it more positive, followed by repolarization (K⁺ out) to reset the membrane