Chapter 11: Excretory & Digestive System
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
157 Terms
What is excretion?
Excretion is the disposal of waste products from the body.
Which organs are primarily involved in excretion?
The kidneys, liver, large intestine (colon), and skin.

What role does the liver play in excretion?
The liver excretes wastes by chemically modifying them and releasing them into bile. It also synthesizes urea, which is released into the bloodstream.
What is the function of urea in the body?
Urea carries excess nitrogen resulting from protein breakdown and is excreted in urine.
How does the colon contribute to excretion?
The colon reabsorbs water and ions from feces and can excrete excess ions into the feces.
What is the excretory role of the skin?
The skin produces sweat, which contains water, ions, and urea, acting as an excretory organ, though its primary role is temperature regulation.
What is the primary role of the kidneys in excretion?
The kidneys excrete hydrophilic wastes such as urea, sodium, bicarbonate, and water, and maintain homeostasis.
What are the three main excretory and homeostatic roles of the kidneys?
1) Excretion of hydrophilic wastes, 2) Maintenance of constant solute concentration and pH, 3) Maintenance of constant fluid volume.
What is the process of filtration in the kidneys?
Filtration is the passage of pressurized blood over a filter where cells and proteins remain in the blood while water and small molecules are squeezed into the renal tubule.
What is selective reabsorption in the kidneys?
Selective reabsorption is the process of taking back useful items (e.g., glucose, water, amino acids) while leaving wastes and some water in the renal tubule.
What is the process of secretion in the kidneys?
Secretion involves adding substances to the filtrate, increasing the rate at which substances are eliminated from the blood.
What happens during the concentration and dilution of urine?
The kidney selectively reabsorbs water to decide whether to produce concentrated or dilute urine.
Why is maintaining a constant serum Na+ concentration important?
Significant variations in serum Na+ concentration can be fatal due to dysfunction of neurons, cardiac muscle cells, and other cell types.
What is the fluid in the renal tubule called after filtration?
Filtrate
How does the kidney ensure homeostasis?
By filtering blood, reabsorbing useful substances, secreting additional substances, and concentrating or diluting urine to maintain balance.
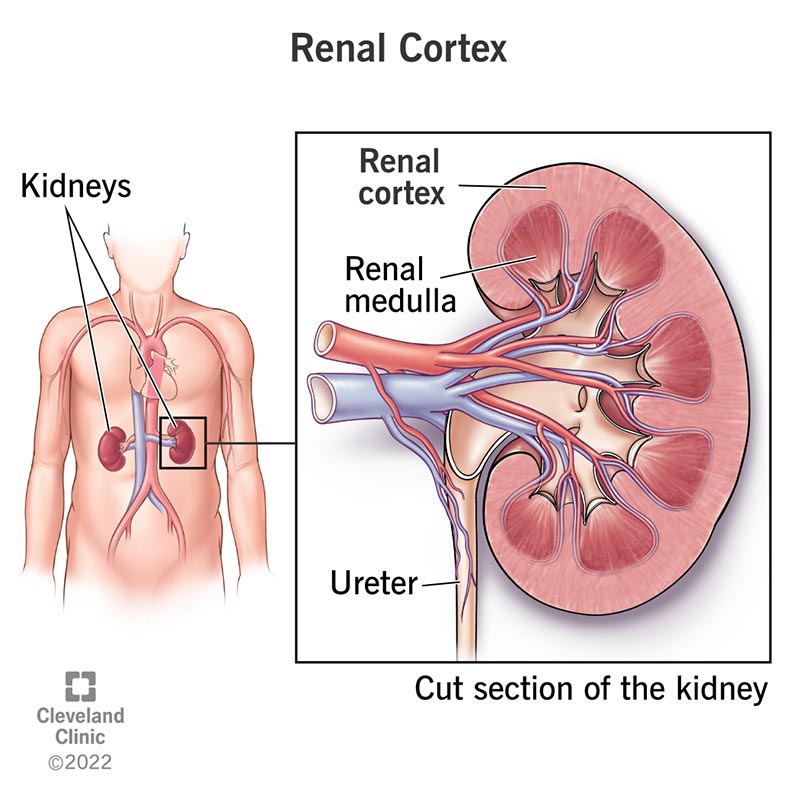
How does blood enter and exit the kidneys?
Blood enters the kidneys via the renal artery, a branch of the abdominal aorta, and exits via the renal vein, which empties into the inferior vena cava.
How is urine transported from the kidneys to the bladder?
Urine leaves the kidneys through the ureters, which transport it to the urinary bladder.
What controls the release of urine from the bladder?
The release of urine is controlled by two sphincters: an internal sphincter (smooth, involuntary muscle) and an external sphincter (skeletal, voluntary muscle).
What happens when the bladder becomes full?
Signals of urgency are sent to the brain, leading to the relaxation of the internal sphincter and, if appropriate, the external sphincter to allow urine to flow out.
What are the two main regions of the kidney's internal anatomy?
The outer region is the cortex, and the inner region is the medulla.
What are medullary pyramids?
Medullary pyramids are pyramid-shaped striations within the medulla due to the presence of many collecting ducts.
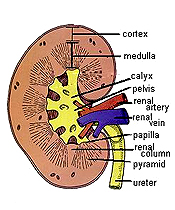
What is a papilla in the kidney?
A papilla is the tip of a medullary pyramid where urine empties into a calyx.
What does the renal pelvis do?
The renal pelvis is a large space where urine collects before being emptied into the ureter.
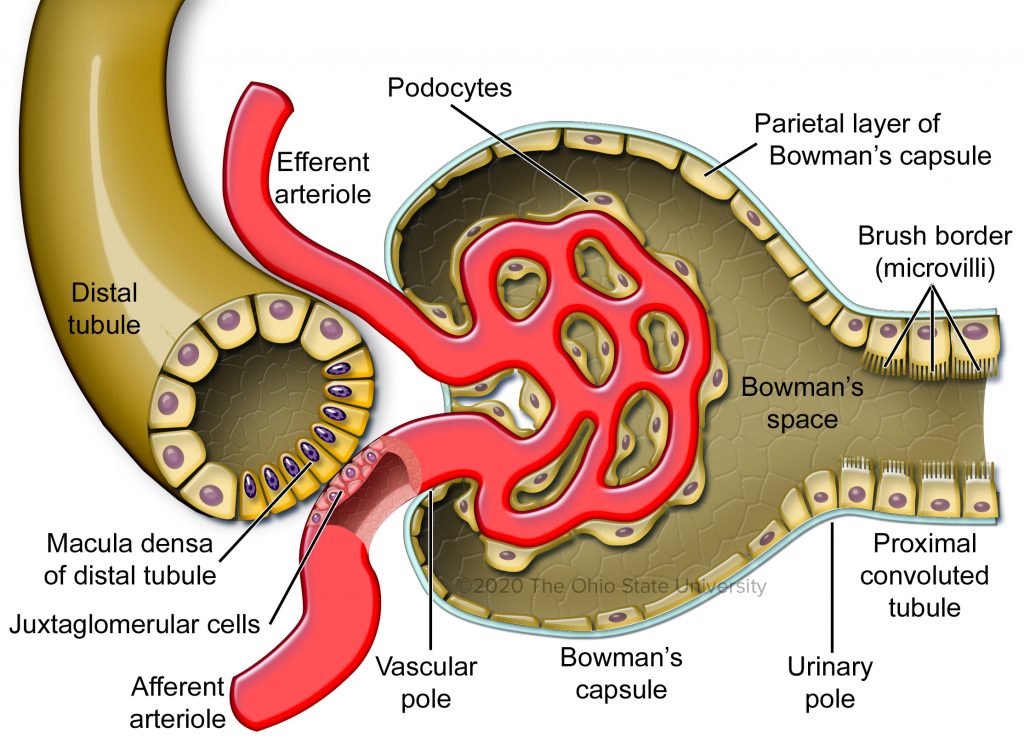
What are the two main components of a nephron?
The nephron consists of a rounded capsule surrounding capillaries where filtration occurs, and a coiled renal tubule.
What is the role of the renal tubule in the nephron?
The renal tubule receives filtrate from the capsule and empties into a collecting duct, which then dumps urine into the renal pelvis.
How does blood flow through the nephron for filtration?
Blood flows from the renal artery into an afferent arteriole, then into the glomerulus (a ball of capillaries), and exits via the efferent arteriole.
What causes the fluid to leak out of the glomerular capillaries into Bowman’s capsule?
Constriction of the efferent arteriole creates high pressure in the glomerulus, causing fluid (essentially blood plasma) to leak out.
What is the role of the glomerular basement membrane?
The glomerular basement membrane acts as a filter, allowing small substances to pass through while retaining larger substances, like blood cells and plasma proteins, in the blood.
Where does filtrate go after it enters Bowman’s capsule?
Filtrate moves from Bowman’s capsule into the renal tubule.
How are substances too large to pass through the glomerular basement membrane handled?
These substances remain in the blood in the glomerular capillaries and drain into the efferent arteriole.
What happens during selective reabsorption in the nephron?
Useful substances like glucose, amino acids, and water are reabsorbed from the filtrate back into the bloodstream via peritubular capillaries.
Where does most reabsorption occur in the nephron?
Most reabsorption occurs in the proximal convoluted tubule (PCT), where approximately 70% of the filtrate volume is reabsorbed.
How is reabsorption regulated in the distal convoluted tubule (DCT)?
Reabsorption in the DCT is more regulated and controlled by hormones.
What is the purpose of secretion in the nephron?
Secretion moves substances into the filtrate to ensure they are eliminated from the body, acting as a backup method for removing what wasn’t filtered out.
Where does most secretion occur in the nephron?
Most secretion occurs in the distal convoluted tubule (DCT) and the collecting duct.

What role does antidiuretic hormone (ADH) play in urine concentration?
ADH increases water reabsorption in the distal nephron by making the collecting duct permeable to water, concentrating the urine

What happens when ADH is not secreted?
Without ADH, the collecting duct remains impermeable to water, leading to the production of a large volume of dilute urine.

How does alcohol affect ADH secretion and urine production?
Alcohol inhibits ADH secretion, resulting in increased urine production and dehydration

What does aldosterone do in the nephron?
Aldosterone increases sodium reabsorption in the distal nephron, which raises blood pressure by increasing plasma osmolarity and water retention.
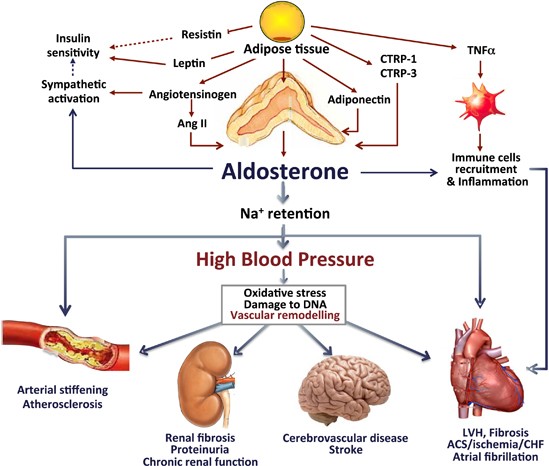
How do ADH and aldosterone work together to regulate blood pressure?
Aldosterone increases sodium reabsorption, raising plasma osmolarity and triggering ADH release, which increases water reabsorption and blood volume.
Describe the structure of the nephron.
The nephron includes Bowman’s capsule, proximal convoluted tubule (PCT), loop of Henle (descending and ascending limbs), distal convoluted tubule (DCT), and collecting duct.

What is the role of the loop of Henle in urine concentration?
The loop of Henle creates a high osmolarity in the medulla, which facilitates water reabsorption from the collecting duct.

What is the countercurrent multiplier system?
It refers to the mechanism where the descending limb of the loop of Henle is permeable to water, and the ascending limb is permeable to ions, which helps concentrate the medulla and facilitates water reabsorption.
What are vasa recta and their function?
Vasa recta are blood vessels that follow the loop of Henle and help maintain the high salt concentration in the medulla by performing countercurrent exchange, thus reabsorbing water back into the bloodstream.
How does countercurrent exchange improve efficiency?
By maintaining a concentration gradient, countercurrent exchange enhances the efficiency of processes like respiration and water reabsorption.
What is the function of the juxtaglomerular apparatus (JGA)?
The JGA regulates systemic and local (glomerular) blood pressure through its components: juxtaglomerular (JG) cells and macula densa.
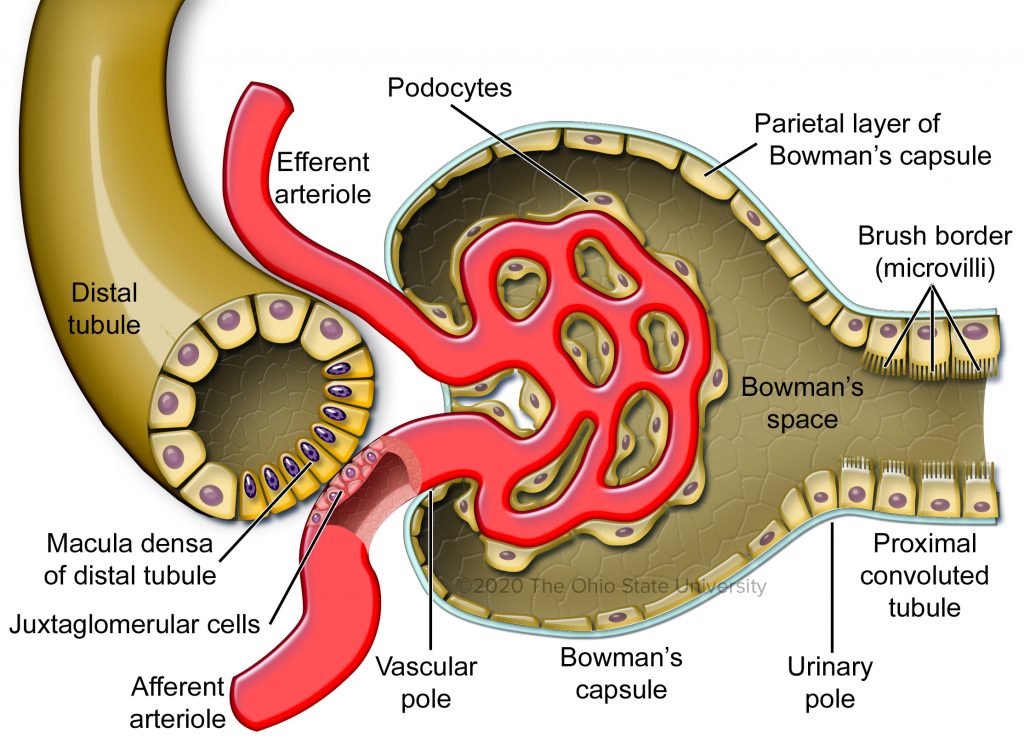
What do juxtaglomerular (JG) cells do?
JG cells are baroreceptors that monitor systemic blood pressure and secrete renin when blood pressure decreases.
What is the role of renin in blood pressure regulation?
Renin catalyzes the conversion of angiotensinogen to angiotensin I, which is then converted to angiotensin II.
Angiotensin II raises blood pressure by constricting blood vessels and stimulating aldosterone release.
How does angiotensin II affect blood pressure?
Angiotensin II is a vasoconstrictor that increases blood pressure and stimulates aldosterone release, which helps retain sodium and water, further raising blood pressure
What is the role of the macula densa in blood pressure regulation?
The macula densa monitors filtrate osmolarity and stimulates JG cells to release renin when osmolarity decreases. It also dilates the afferent arteriole to increase blood flow and filtration rate in the glomerulus.
How do the kidneys regulate blood pH?
The kidneys maintain blood pH by excreting HCO3– when pH is too high and excreting H+ when pH is too low.
This process involves the enzyme carbonic anhydrase.
What role does carbonic anhydrase play in pH regulation?
Carbonic anhydrase catalyzes the conversion of CO2 to carbonic acid (H2CO3), which dissociates into bicarbonate (HCO3–) and protons (H+). This helps the kidney reabsorb or secrete bicarbonate or protons to adjust pH.
How long does it take for the kidneys to adjust blood pH?
Renal pH adjustments are slow and can take several days to normalize plasma pH after a disturbance.
What is the role of the lungs in pH regulation?
The lungs help regulate blood pH by exhaling excess CO2, which removes an acid (H2CO3) from the blood, thus raising the pH.
How does hyperventilation affect blood pH?
Hyperventilation increases the removal of CO2, which raises blood pH by reducing the amount of carbonic acid in the blood.
What hormone does the kidney produce, and what is its role?
The kidney produces erythropoietin (EPO), which stimulates red blood cell production in the bone marrow.
What type of hormones affect the kidney?
Most hormones affecting the kidney are peptides, except for aldosterone, which is a steroid.
What is the primary function of the digestive system?
The primary function is digestion and absorption of foodstuffs.
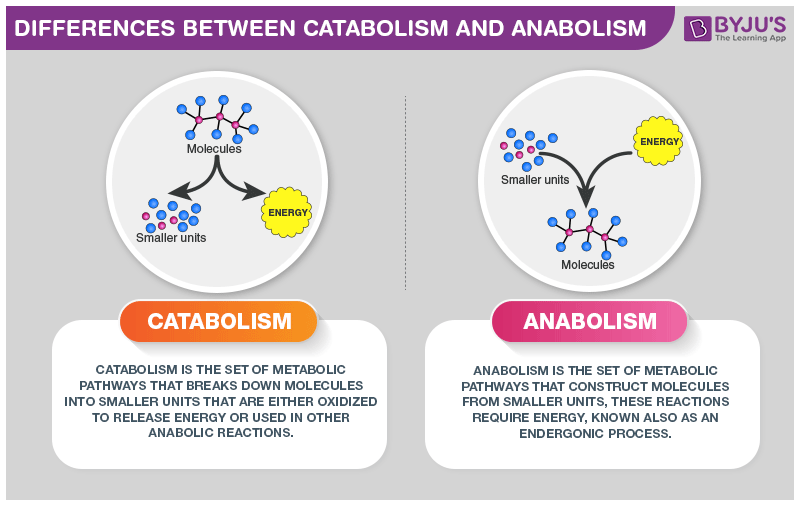
What is the difference between catabolic and anabolic reactions?
Catabolic reactions break down molecules to supply energy — either oxidized to release energy or used in other anabolic reactions
Anabolic reactions synthesize macromolecules — construct molecule from smaller units — requires energy
What is digestion, and how is it accomplished?
Digestion is the breakdown of polymers (like polypeptides, fats, and starch) into their building blocks, accomplished by enzymatic hydrolysis (reaction where water is used to break down chemical bonds).
Polypeptides = amino acid chains linked by peptide bonds
Starch = carbohydrates from in fruits, vegetables and grains

Carbohydrates break down into
Glucose

Lipids break down into
Fatty acid and glycerol (naturally occurring alcohol)
What are triglycerides?
Triglycerides are a type of fat found in your blood made up glycerol and three fatty acid chains.
Triglycerides store unused calories and provide the body with energy.
When you eat, the calories your body does not need to use right away are converted into triglycerides. These are stored in fat cells
Hormones later release triglycerides for energy between meals

What are the different types of lipids?
Triglycerides
Phospholipids
Sterols (cholesterol)
Waxes
What role do vitamins play in the digestive process?
Vitamins in their active forms serve as helpers for enzymes, enabling reactions to occur more efficiently without being used up themselves, unlike substrates, which are transformed into new products during the reaction.
What are the primary and secondary functions of the digestive system?
Primary function: digestion and absorption of foodstuffs
Secondary function: protection from disease
What is the GI tract, and what is its significance?
The GI tract, also known as the digestive tract or alimentary canal, is a long muscular tube from the mouth to the anus, where digestion is accomplished.
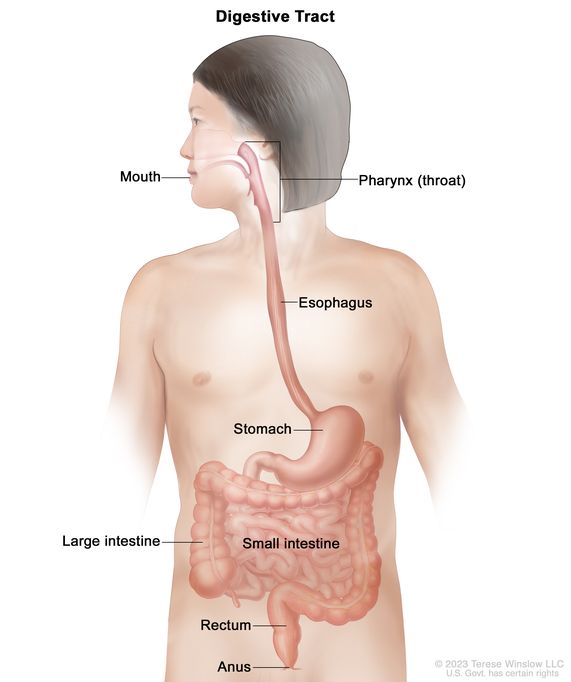
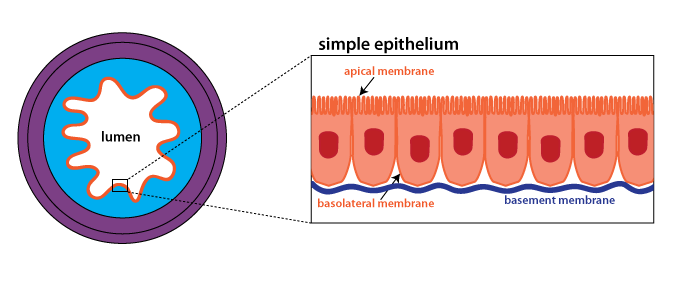
What is the GI lumen, and why is it significant?
The inside compartment of the gut where usable components of foodstuffs are extracted, while wastes are left for excretion.

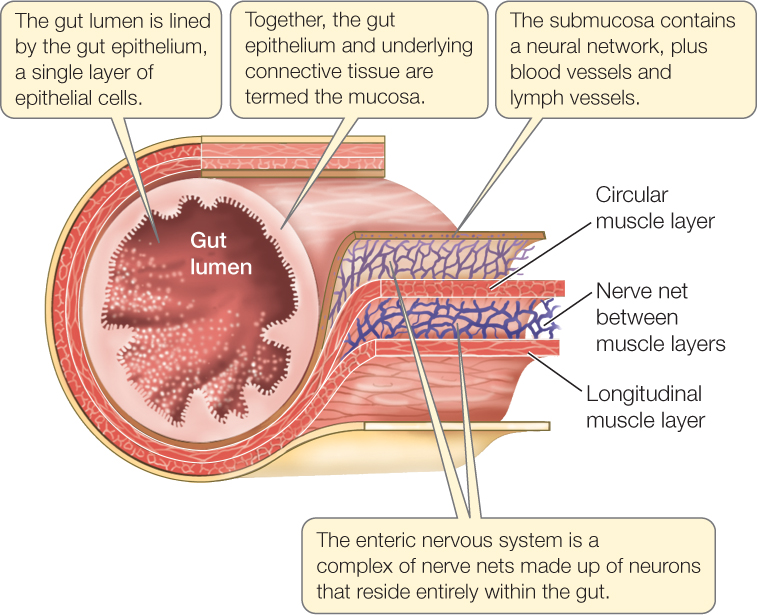
What type of cells line the innermost part of the GI lumen?
Composed of epithelial cells, similar to those on the outer surface of the body and respiratory tract.
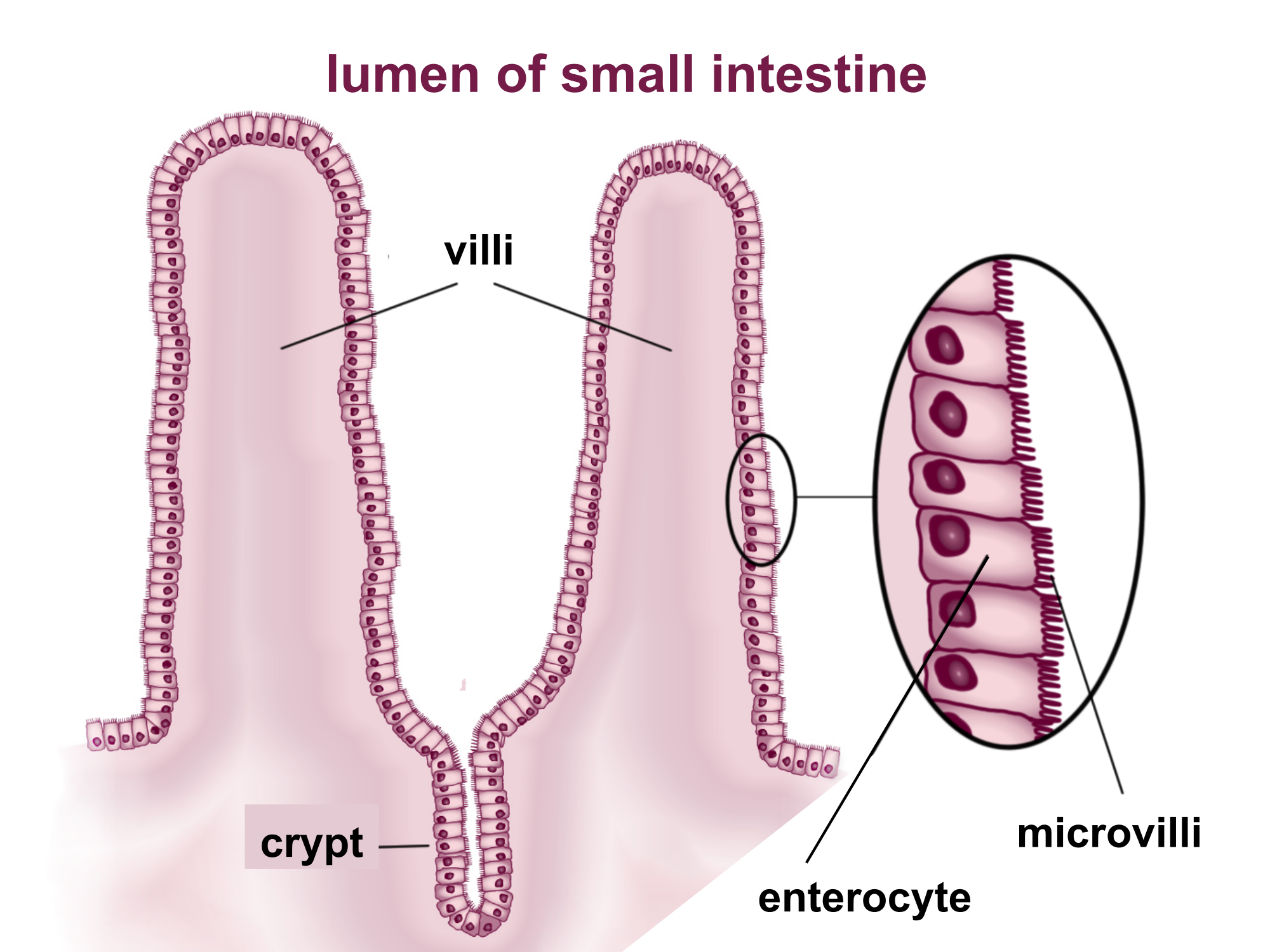
What are microvilli, and what is their function in the small intestine?
Outward folds of the plasma membrane on the apical surface of epithelial cells in the small intestine, increasing surface area for absorption.
What is the difference between the apical and basolateral surfaces of epithelial cells in the GI tract?
The apical surface faces into the lumen, while the basolateral surface is opposite, facing away from the lumen.
What is GI smooth muscle, and how does it differ from other muscle types?
Smooth microscopic appearance, contrasting with striated muscles like skeletal and cardiac muscles, which appear striped.
What are the two layers of smooth muscle lining the gut, and how do they function?
The two layers are the longitudinal layer (running lengthwise) and the circular layer (encircling the gut), which work together for GI motility.
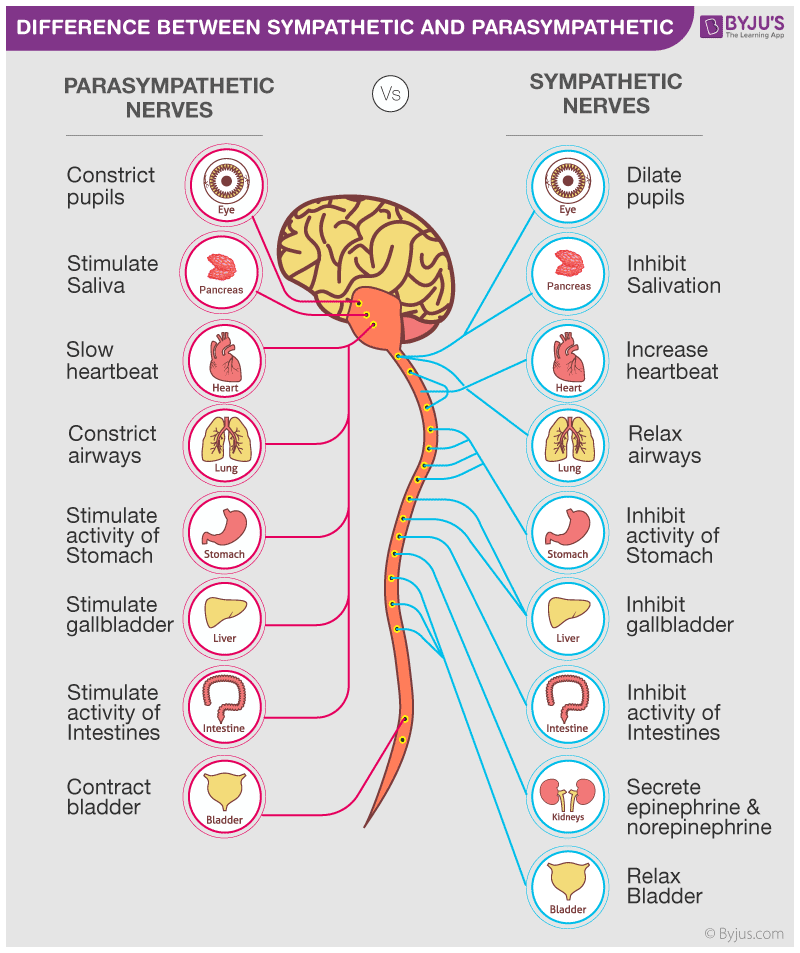
What is GI motility, and what factors influence it?
Rhythmic contraction of GI smooth muscle
Influenced by automaticity, functional syncytium, the enteric nervous system, hormonal input, and the autonomic nervous system.
Automaticity in the GI system refers to the inherent ability of certain cells to generate and coordinate the electrical impulses that control the movement of the digestive tract, ensuring smooth and efficient digestion without conscious effort.
A functional syncytium refers to a group of individual cells that are connected and function as a single, coordinated unit. This is essential for the synchronized contraction of muscles in the heart and GI system, allowing these organs to perform their vital functions effectively.
The enteric nervous system is a specialized network of nerves within the GI tract that operates independently to regulate digestion, motility, secretion, and blood flow, all while communicating with the brain. Its ability to function autonomously makes it a vital component of digestive health and overall well-being.
Hormonal input involves the regulation of bodily functions through hormones, which are chemical messengers that influence a wide range of physiological processes.
The autonomic nervous system is responsible for controlling involuntary functions of the body, helping to maintain balance and respond to changes in the environment. It consists of the sympathetic, parasympathetic, and enteric divisions, each with specific roles in managing bodily functions like heart rate, digestion, and stress responses.
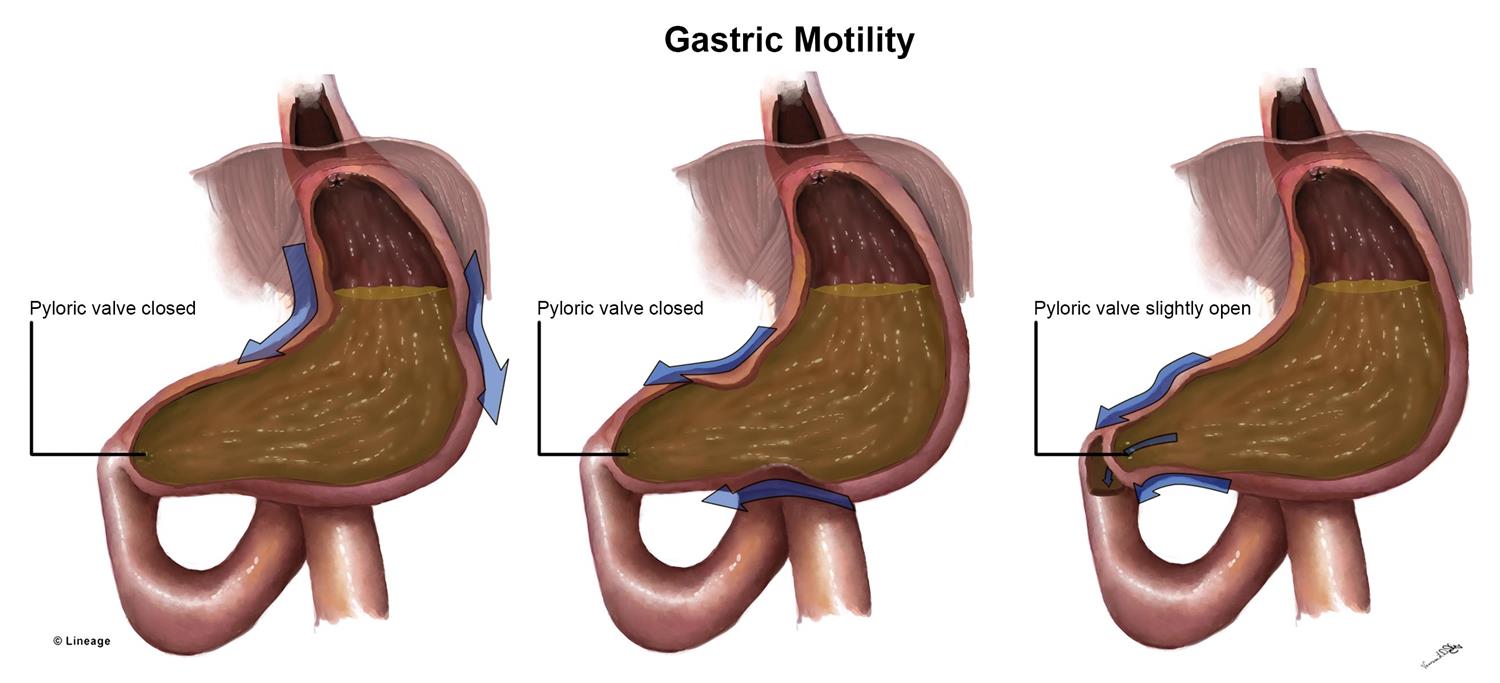
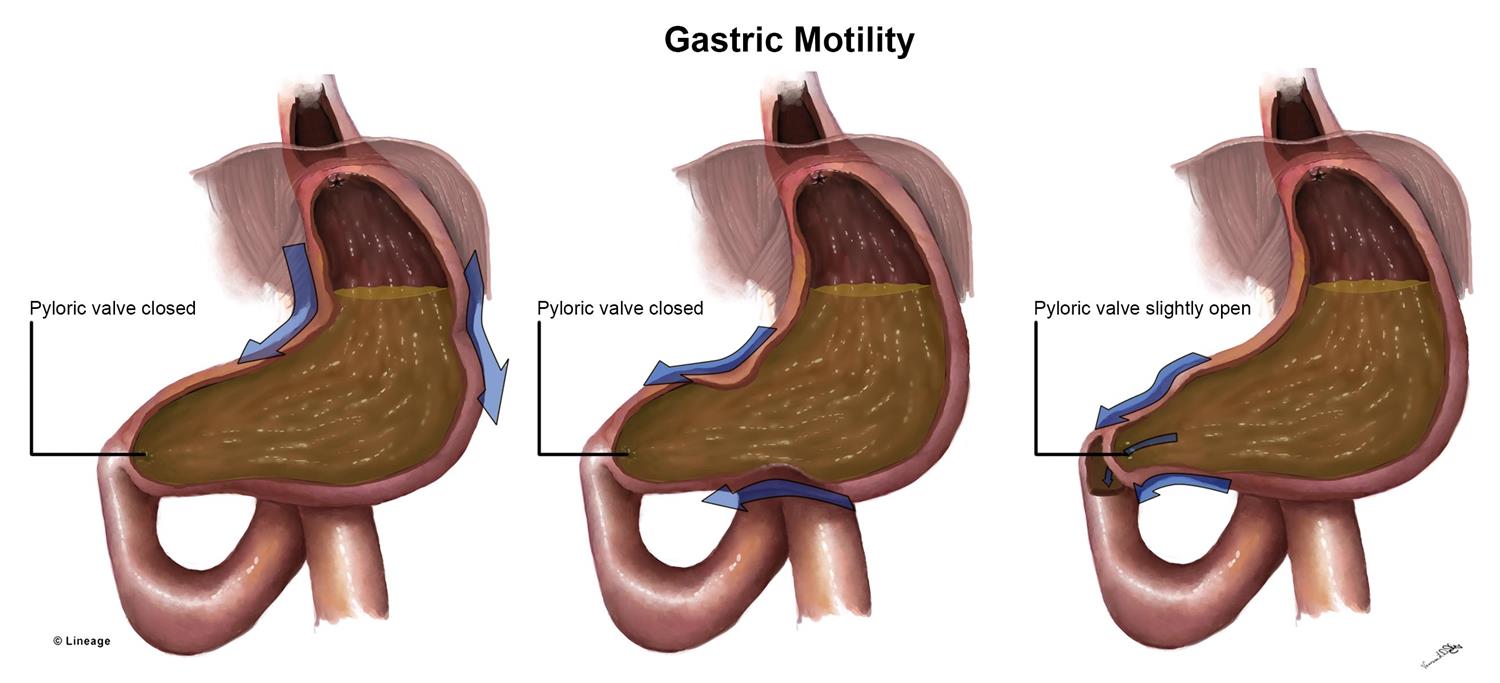
What are the purposes of GI motility?
Mix food and move it down the gut, with mixing accomplished by disordered contractions and movement by peristalsis.
What is the enteric nervous system, and what are its functions?
A branch of the autonomic nervous system, helps regulate local blood flow, gut movements, and fluid exchange in the GI tract, pancreas, and gall bladder.
What are the two networks of neurons in the enteric nervous system, and what are their roles?
The myenteric plexus regulates gut motility
The submucosal plexus regulates enzyme secretion, gut blood flow, and ion/water balance.
How are GI secretions regulated?
GI secretion is stimulated by food in the gut and the parasympathetic nervous system, and inhibited by sympathetic stimulation.
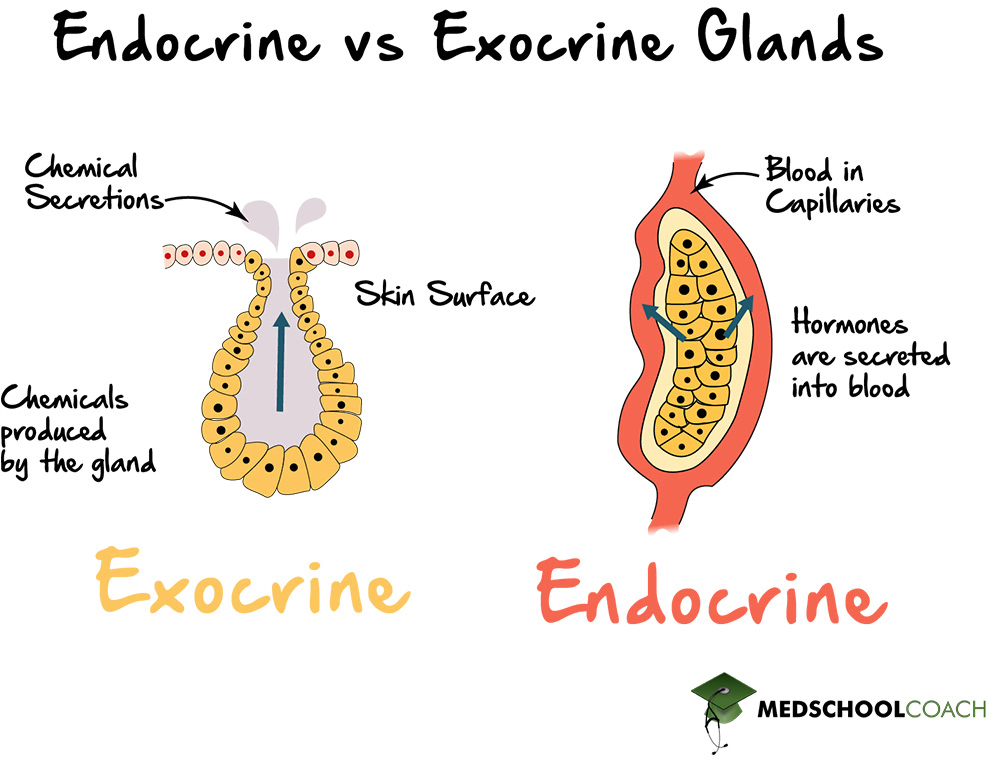
What is the difference between endocrine and exocrine secretion in the GI tract?
Exocrine glands release products into ducts that empty into the GI lumen
Endocrine secretions (hormones) are picked up by nearby capillaries and do not empty into ducts.
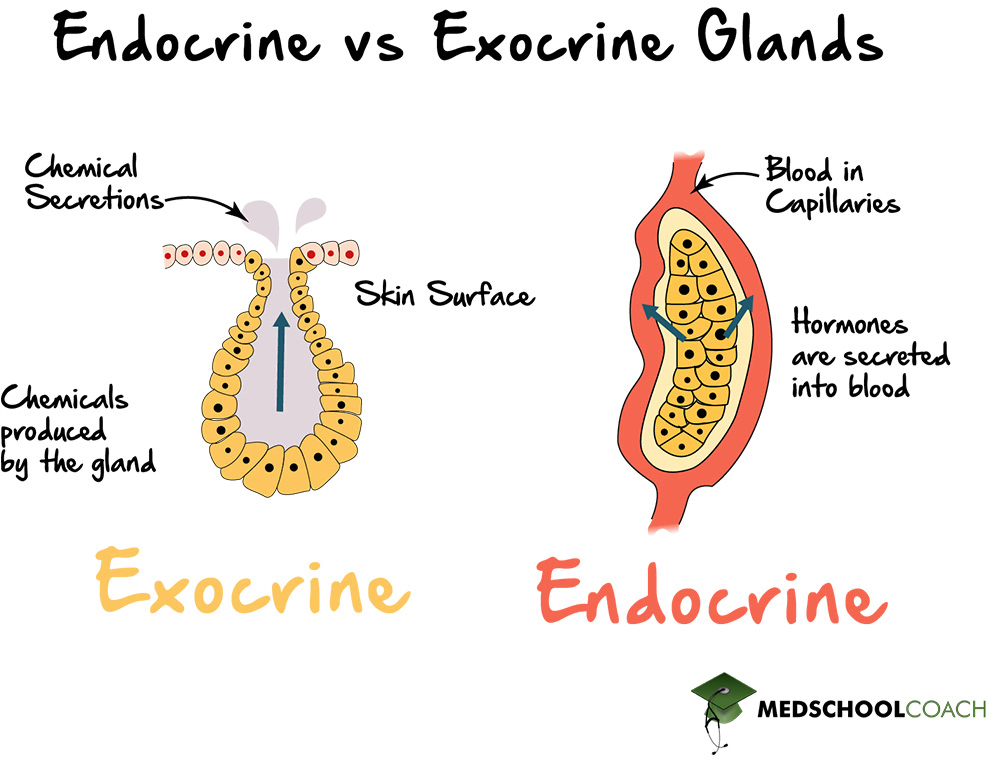
What are acini, and what is their role in exocrine secretion?
Acini are sacs composed of specialized epithelial cells in exocrine glands that secrete products into ducts leading to the GI lumen.
What are goblet cells, and what do they secrete?
Specialized mucus-secreting cells along the GI tract that release mucus to protect and lubricate the gut.
How is water involved in digestion within the GI lumen?
Water is secreted into the GI lumen to dissolve meals for digestion, with most water reabsorbed in the small intestine and the remainder in the colon.
What are the two principal cell types in the pancreas, and what are their functions?
Exocrine cells, known as pancreatic acinar cells, secrete into ducts — release digestive enzymes and zymogens (pro-enzymes) to help digest food. zymogen = inactive precursor to an enzyme that must undergo a biochem change to become active.
Endocrine cells, known as islets of Langerhans, release hormones into the blood — clusters of cells in the pancreas that produce hormones that regulate blood sugar levels
What are the three primary roles of the mouth in digestion?
The three roles of the mouth in digestion are fragmentation (chewing), lubrication (via saliva), and some enzymatic digestion (through salivary enzymes).
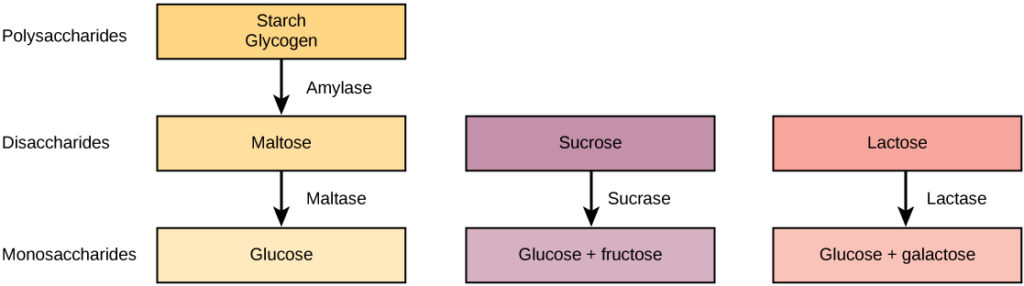
What enzyme in saliva breaks down starch, and what is the smallest fragment it produces?
Salivary amylase (ptyalin) breaks down starch, and the smallest fragment it produces is the disaccharide.
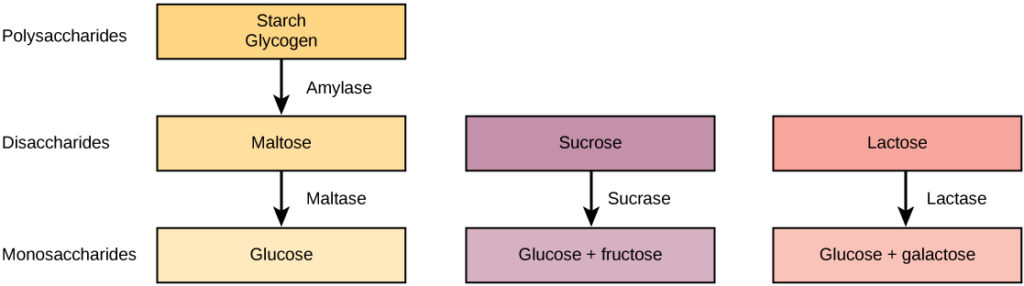
Polysaccharides break down into _______ into _________
Disaccharides
Monosaccharides
What is the role of lysozyme in saliva?
Lysozyme in saliva attacks bacteria, playing a role in innate immunity.
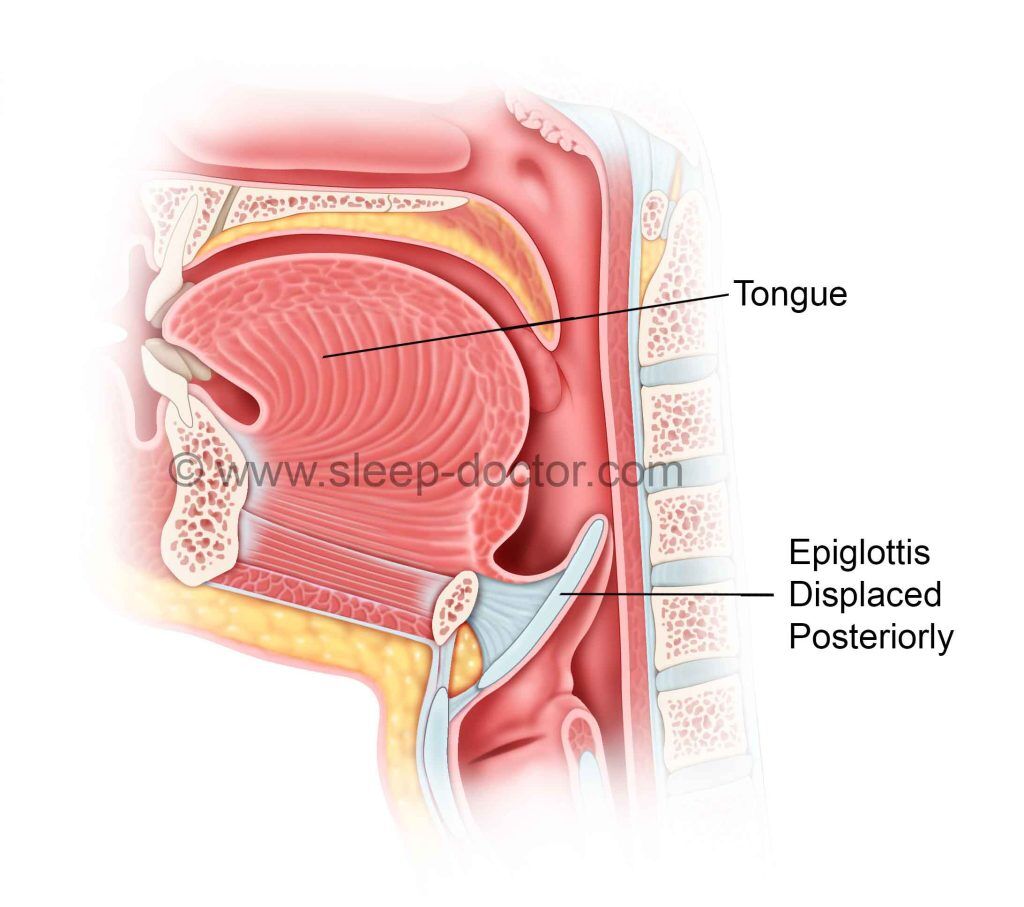
What is the function of the epiglottis during swallowing?
The epiglottis prevents food and liquids from entering the trachea during swallowing by covering the tracheal opening.
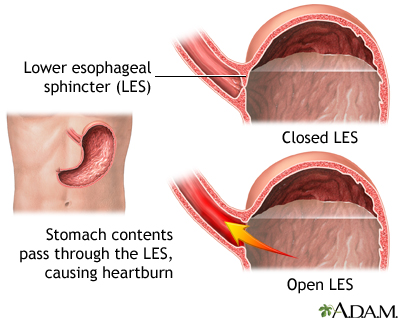
What are the two muscular rings in the esophagus, and what are their functions?
The upper esophageal sphincter controls the passage of food from the pharynx to the esophagus, and the lower esophageal (cardiac) sphincter prevents reflux of stomach contents into the esophagus.

What are the three main purposes of the stomach in digestion?
The stomach's three main purposes are partial digestion of food, regulated release of food into the small intestine, and destruction of microorganisms.
How does the stomach maintain a low pH, and what are the effects of this acidity?
The stomach maintains a low pH through the secretion of HCl by parietal cells. The effects include the destruction of microorganisms, acid-catalyzed hydrolysis of proteins, and conversion of pepsinogen to pepsin.
What is the role of pepsin in the stomach, and how is it activated?
Pepsin is an enzyme that catalyzes the breakdown of proteins.
It is activated from its precursor, pepsinogen, by the acidic environment in the stomach.
What prevents the reflux of chyme from the stomach into the esophagus?
The lower esophageal sphincter prevents the reflux of chyme into the esophagus.
What is the function of the pyloric sphincter?
Regulates the passage of food from the stomach into the duodenum, preventing premature stomach emptying.
:watermark(/images/watermark_only_413.png,0,0,0):watermark(/images/logo_url_sm.png,-10,-10,0):format(jpeg)/images/anatomy_term/pyloric-canal/ufFxD6lLBEkkDKp4xmqi1A_Pyloric_canal.png)
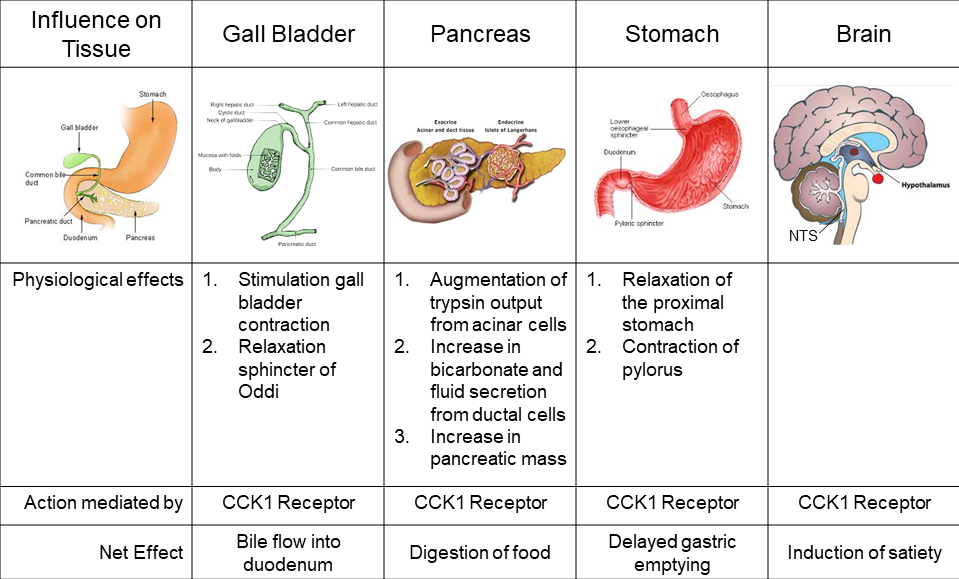
What hormone is responsible for inhibiting stomach emptying and where is it secreted?
Cholecystokinin (CCK) inhibits stomach emptying and is secreted by epithelial cells in the wall of the duodenum.
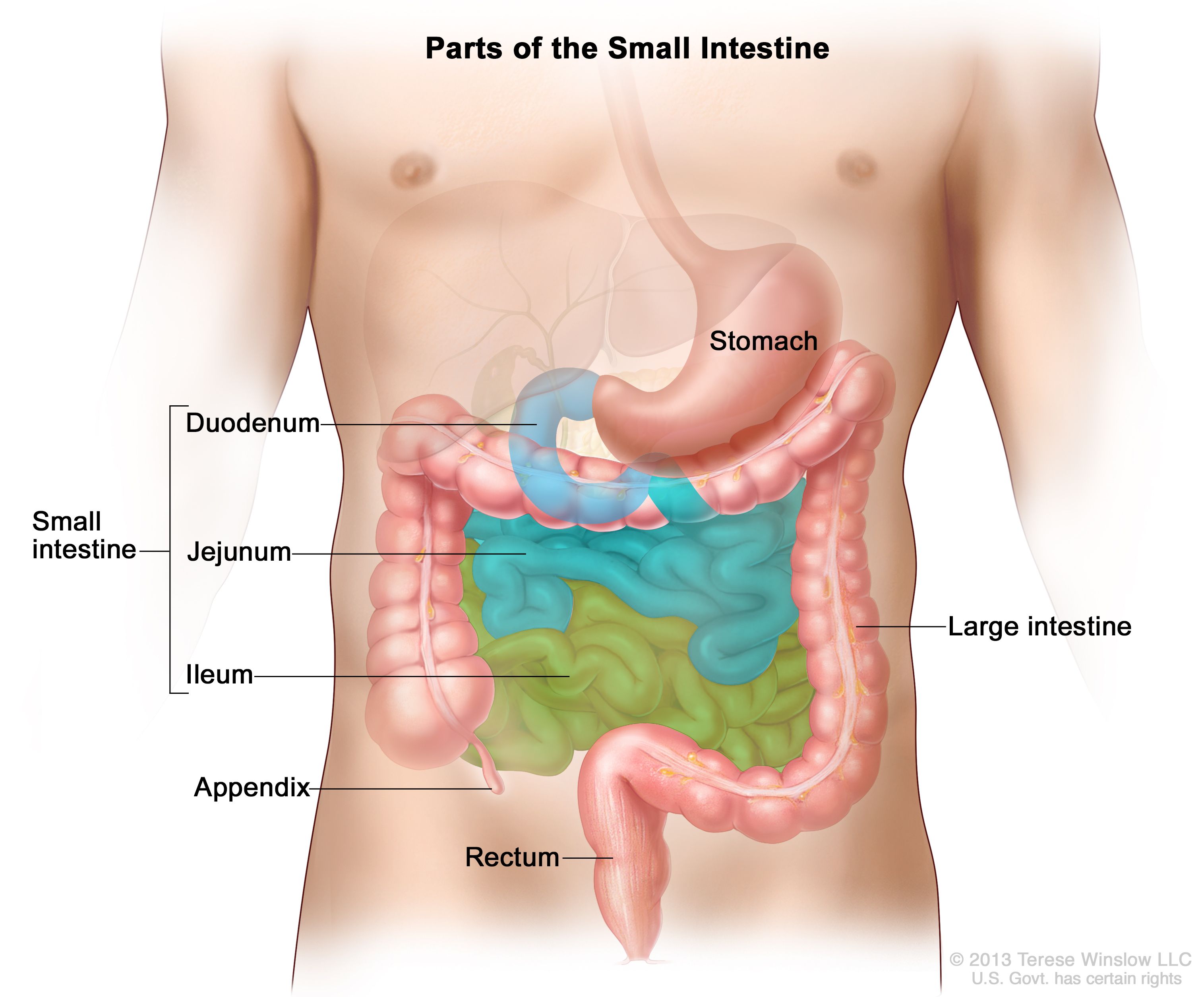
What are the three segments of the small intestine, and where does digestion and absorption primarily occur?
Duodenum, jejunum, and ileum.
Digestion is primarily completed in the duodenum and jejunum, and absorption begins in the duodenum and continues throughout the small intestine.
How does the small intestine increase its surface area for absorption?
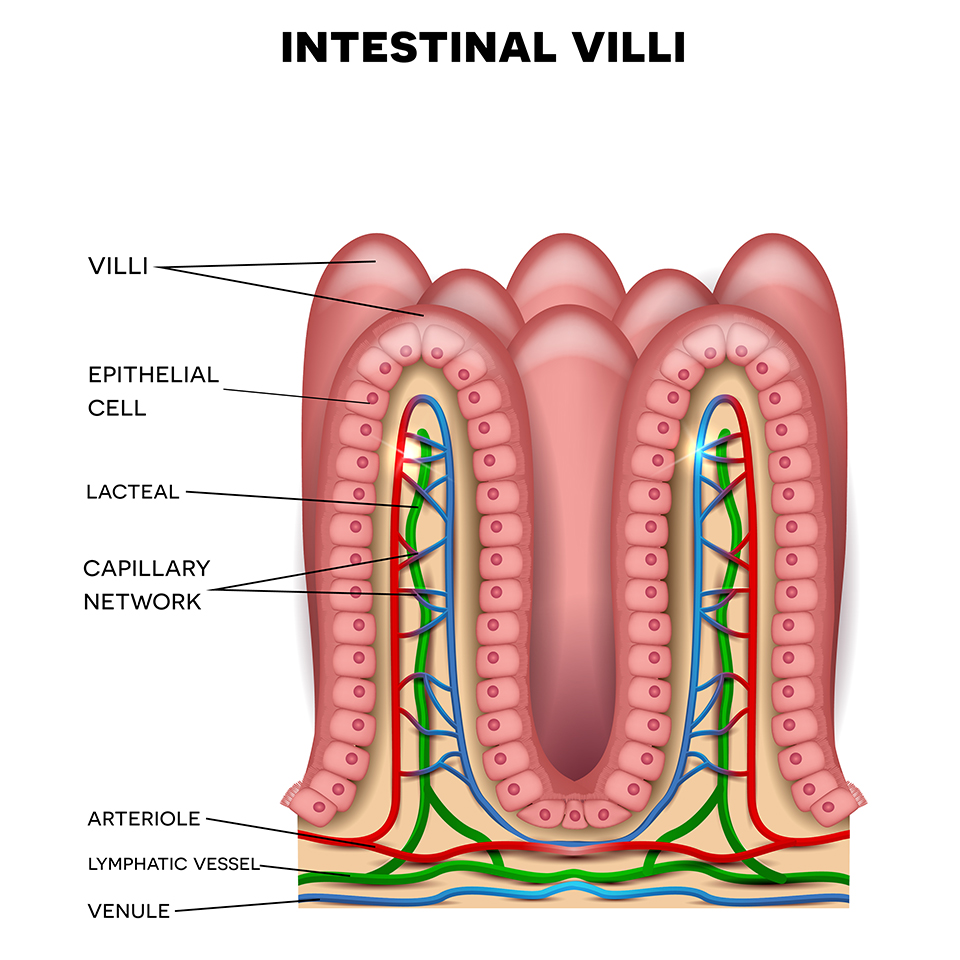
The small intestine increases its surface area through its length, villi (macroscopic projections), and microvilli (microscopic foldings of cell membranes).
What are the three important structures found within the villi of the small intestine?
The villi contain capillaries for absorbing monosaccharides and amino acids, lacteals for absorbing dietary fats, and Peyer’s patches for immune function.
Capillaries: monosaccharides (carb) and amino acids
Lacteals: dietary fats
Peyer’s patches: immune function
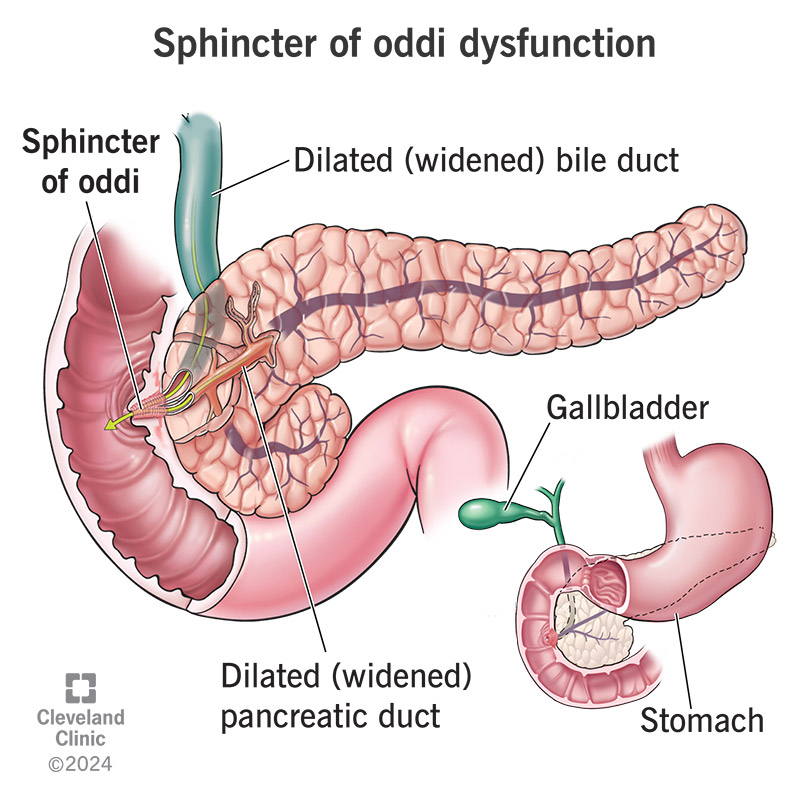
What two ducts empty into the duodenum, and what do they deliver?
The pancreatic duct delivers digestive enzymes and bicarbonate
The common bile duct delivers bile, both of which empty into the duodenum through the sphincter of Oddi.
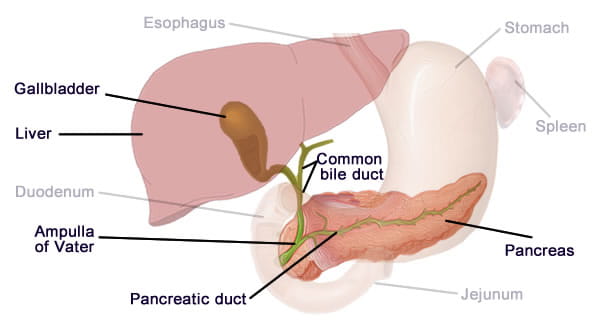
What is the role of bile in digestion?
Digestion of fats and also serves as a vehicle for the excretion of waste products by the liver.