2. Innate Immune System
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms
What are the 3 main functions of the innate immune system
Controls/Eliminates infection
Eliminates damaged cell and influences repair
Stimulates the adaptive immune response
What are the Main “Players” of the Innate Immune System other than cells?
Physical Barriers
Skin and Mucosa
Enzymatic barriers
Lactoferrin, Lysozyme
Explain the 6 types of Physical barriers and the characteristics of each
Skin
Dry
Slightly acidic pH (4)
Sloughing (skin falls off)
Impenetrable when intact
Mucosa
Mucin slides off or traps pathogens
Lactoferrin and Lysozyme enzymatic barriers and Defensins
Muco-ciliary escalator: mucin-trapped particles are moved towards the pharynx to be either swallowed or expelled
Normal Flora: good bacteria compete with pathogens by
Occupying binding sites
Using resources/nutrients
Producing toxins that kill pathogens by destroying cell wall or causing lysis
Fever:
retards growth
speeds hematopoiesis (thus cell production)
Eye:
Tear washes eye
Blinking
Contains lysozyme
What are the 2 Enzymatic Barriers?
Lysozyme: Breaks down NAM and NAG linkages on Peptidoglycan
Present in tears, saliva and mucus
Urea: denatures proteins
What are the 4 Protein Effectors?
Proteases: cleaves proteins on the pathogen
Defensins:
Antimicrobial peptide found in phagolysosomes, granulocytes and mucosal secretion
Destroys membranes of pathogens by poking holes
Iron-sequestering proteins:
Prevent bacteria from using iron
Present in mucosal secretions
Complement System: 30 protein cascade that either kills or tags pathogen for destruction
Name the 4 major cells of Innate Immunity and their function
NK cells
Not phagocytes
Scan cells for presence of host markers such as MHC markers (determines self and non-self)
Kills infected cells or abnormal cells
Neutrophils:
Phagocyte
Short-lived
Granulocytes: secrete toxic substances (lactoferrin, defensins, lysozyme, ROS and RNS) that kill pathogens
Polymorphonuclear cell due to segmented nuclei
Circulate in the blood until called to site of infection
Monocyte
Macrophage progenitor cell
Circulates in the blood for 3 days and only differentiates once it enters tissues (cytokine regulated)
Macrophage:
Long lived
Tissue fixed: “the commander” that patrols the tissue and calls others for backup through cytokines
Phagocyte and APC
Dendritic cells:
Phagocytic
APC
Not tissue fixed: leave tissue with pathogenic cargo and travel to one of the 2 lymphoid organs to present
Bridge innate and adaptive
What are the characteristics of the Phagosome/Phagolysosome?
Acidic environment impedes growth
Has ROS and RNS that release superoxide to lumen
Destroys proteins, nucleic acids and lipids
Impairs bacterial metabolism
Antimicrobial proteins and peptides
Lactoferrin
Defensins
Hydrolysis by lysozyme, phospholipases and proteases
Who detects pathogens?
How do phagocytes know when to act?
Macrophages
They have Pattern Recognition Receptors (PRR) that recognize pathogen motifs called Pathogen-Associated Molecular Patterns (PAMPS) → PRR binding PAMP causes phagocyte activation
What are types of Pathogen Recognition Receptors (PRRs)?
Toll-Like Receptors (TLRs)
Recognize and bind extracellular PAMPs
Located on cell surface
TLR2 recognizes Bacterial PG and TLR4 recognizes LPS
Nod-like Receptors (NLRs_
Recognizes and binds intracellular PAMPs
Located on cytoplasm
Nod1 recognizes ubiquitous gram negative and Nod2 recognizes gram -/+ expressed in Paneth cells
Mannose-binding lectins (MBLs)
Bind structures with high mannose content (easy way to determine non-cell bc human cells do not have mannose)
Activate lectin complement pathway
What happens when the phagocyte’s PRR binds the pathogen’s PAMP?
The phagocyte increases its phagocytosis/metabolic activity, releases cytokines to recruit other cells (monocytes and neutrophils) to the site of infection, releases ROS and RNS and other degrative enzymes
A BETTER PHAGOCYTE!!!!


What are the 3 most important Cytokines and what do they do
IL-1, IL-6 and TNF-alpha
Pyrogenic
Increase vascular permeability Increase vasodilation, Increase selectin expression → For extravasation
Increase differentiation of immune mediators
Increase production of acute phase proteins
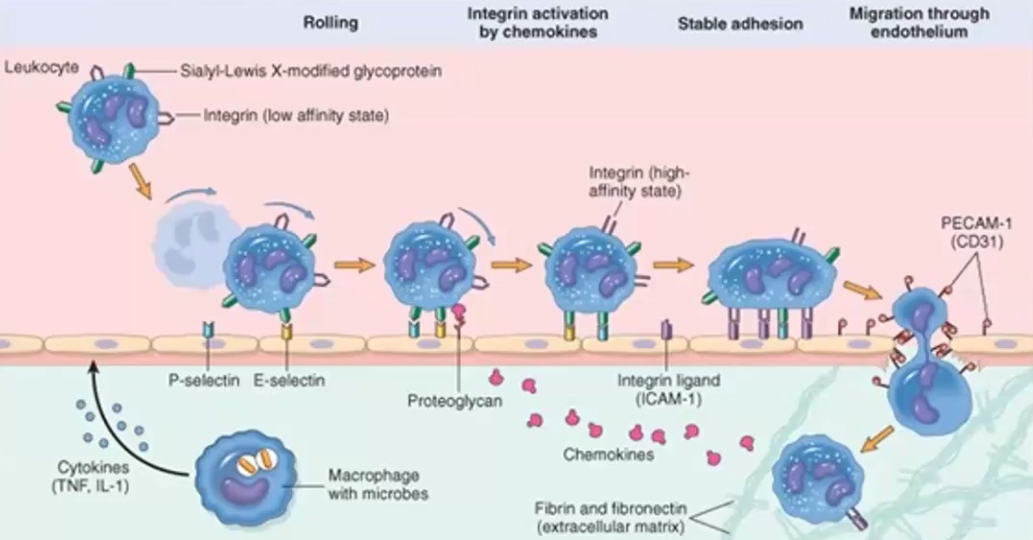
Extravasation
What is it?
Steps
Extravasation is the process through which cells pass from capillaries into tissues
1. Rolling: Cytokines dilate blood vessels, which slows blood down. Selectin expression is increased. Cell binds to selectins via their glycoproteins and roll (bind, detach) slowing down.
2. Activation: Cytokines lead to conformational change in integrin receptors, which allow them to bind to endothelial cells’ ICAM ligand
3. Firm Adhesion: High affinity of Integrin to ICAM leads to firm adhesion, which completely stops leukocyte movement and now spreads onto vessel wall
4. Trans-endothelial migration: Due to cytokine induced cell permeability, the leukocyte is able to squeeze between endothelial cells and pass into the tissues
What are the 3 goals of INFLAMMATION?
What are the 4 Symptoms of INFLAMMATION? Why
Recruiting more cells and effector molecules, provides a physical barrier to prevent spread (swelling/edema/cells), promote tissue repair
Rubor (redness), Calor (heat), Dolor (pain), Tumor (swelling) → Due to soluble mediators increasing vasodilation, cellular influx and even effects on nerves
What is the Acute Phase Response?
What is an example?
Why do we get a fever?
It’s a rapid SYSTEMIC response triggered by the innate system by detection of infection
Fever
We get a fever due to IL-1, IL-6 and TNF-alpha cytokines, which travel to and act upon the hypothalamus