Preventive Dentistry
1/960
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
961 Terms
Mechanism of action
systemically and topically
Systemically
Ingested, or taken into the body during consumption of foods or beverages
Topically
Directly to the exposed surfaces of teeth erupted into the oral cavity
Maximum caries inhibiting effect includes
systemic exposure before eruption, topical fluoride throughout life
After eruption and throughout the life span of teeth, fluoride on the outer most surface of enamel is dependent on (topical/systemic)
Prevent demineralization, encourage remineralization
daily topical sources of fluoride
Post-eruption
continuous daily presence of fluoride can inhibit initiation and progression of dental caries
uptake is the most rapid during the 1st years after eruption
Uptake of fluoride is the most rapid during the __ years after eruption
1st
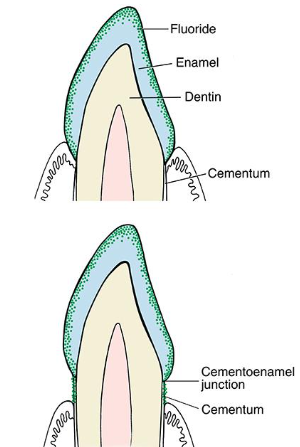
Fluoride in enamel
• Uptake of fluoride depends on the level and length of time exposed
• Hypomineralized enamel absorbs fluoride in greater quantities than healthy enamel
• Hydroxyapatite crystalline becomes fluorapatite
• Intact outer surface enamel has the greatest concentration
Mechanism of action of fluoride to bacteria
• Bacteriocidal to Strep Mutans:
-Bacteriostatic vs. Bacteriocidal?
-inhibits bacterial activity by inhibiting enolase
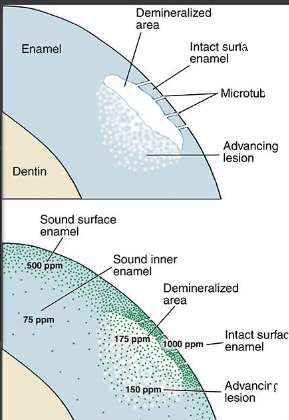
• Inhibits demineralization
• Facilitates remineralization due to formation of fluorapatite
Cariostatic benefits recap
Formation of fluorapatite crystals
Remineralization of enamel-Greatest concentration of fluoride occurs in the outermost surface layers of the enamel
Benefits are related to the number and frequency of fluoride treatments
Topical fluoride therapy
• Delivery Types:
-Rinses
-Dentifrices/toothpastes
-Gels
-Foams
-Varnish
Professional topical fluoride applications
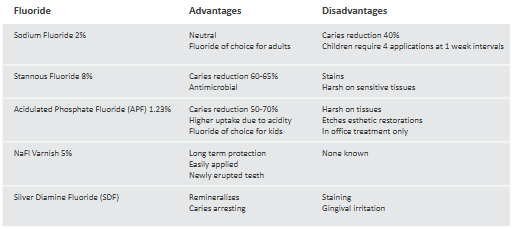
• 2% Sodium Fluoride (NaF) gel or foam
• 1.23% acidulated phosphate fluoride (APF)
• 5% Sodium Fluoride (NaF) varnish
• Silver Diamine Fluoride (SDF)
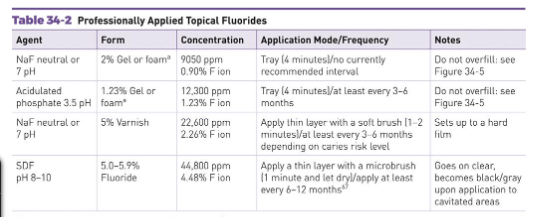
2% Sodium Fluoride Foam
-Available as gel, foam, liquid, & varnish
Basic pH of 9.2
-Because there is an absence of taste, this type of fluoride usually has additive flavoring or sweeteners
1.23% Acidulated Phosphate Fluoride (APF) Gel
Available as a liquid, foam, or gel
Contains 12,300 ppm
Acidic pH of 3.5
Foam applications are widely accepted
by patients because of the pleasant taste
Silver diamine fluoride
-Antimicrobial
-Remineralizing
-Caries arresting
-SDF Information
Fluoride varnish
• Resin material is painted on the teeth
• Basic pH of 9.2
• Main ingredient?
• Sets up quickly when interacting with saliva
• Releases fluoride up to several hours after application
• Safe for young children under the age of 6
• Reduces demineralization around ortho brackets
Stannous fluoride
Liquid most common-Available in a powdered form in either bulk containers or capsules
An acidic solution which should be prepared just prior to use-Acidic pH of 2.4-2.8
Bitter or metallic taste
May be combined with glycerin to mask the adverse taste
Compare and contrast
Application of fluoride
In office:
• Fluoride trays
• Fluoride varnish with special applicator brush
• Brush on foam (can also use cotton applicator)
• Rinse
At home:
• Custom fluoride trays
• Toothpaste
• Rinse
Application of fluoride (how long?)
• 60 seconds for those patients whose fluoride treatment is either a maintenance or a preventative measure
• 4 minutes for those patients who have caries or potential carious activity
Application of fluoride precautions when administering treatments
• Minimal amount needed
• Upright patient position
• Use efficient suctioning
• Patient expectorates thoroughly on completion of the fluoride application
Application of foams/gels
Adequate size tray for the patient
Have patient rinse prior to the fluoride treatment
Tray remains in the patients mouth for 60 seconds to 4 minutes
Patient is instructed not to eat, drink, or rinse for 30 minutes following the treatment
Application of varnish
• Recommended primarily for children
• Contain 5% NaF
• Recommend repeating at 4–6 month intervals
• Dry teeth prior to painting on the varnish
• Patients should be instructed to avoid abrasive foods, hot foods and liquids and brushing teeth for approximately 24 hours (see manuf. Instructions)
• Do not use suction –varnish creates a clogged hose line
Application frequency
Following the initial fluoride therapy, patients should have a fluoride treatment at either a 3-,6-,9-, or 12-month interval depending on the caries status.
Patients at a low caries risk should have fluoride treatments every 6–12 months.
Other sources of fluoride
Prophylaxis paste
Mouthrinses (ACT, Biotene)- Recommended for patients with dry mouth, orthodontics, patients undergoing radiation/chemo, high caries risk (low potency and high frequency)
Prescription toothpastes (Control Rx, Prevident)
Take-home gels
Fluoride-releasing dental materials (i.e., sealants and composites)
Multiple fluoride therapy
• No single fluoride treatment provides total protection against dental caries
• Fluoride combination programs use a fluoride-containing prophylactic paste and a topically applied fluoride solution
• Systemic fluoride can be included
• Results in overall caries reduction of 75%
MI Paste - Remineralizing
Not a fluoride:
• MI Paste Plus does contain a small amount of fluoride (900ppm), otherwise same formula as MI Paste
• Casein (milk protein) and Recaldent are active ingredients: Do not use in a patient with an allergy to milk proteins BUT Lactose intolerant patients are okay
• Recaldent = calcium and phosphate; these minerals stabilize acid, reduce tooth sensitivity, and strengthen tooth enamel
• Minerals released when saliva comes into contact
Acute fluoride toxicity
results from large doses of fluoride over a short period of time
symptoms:
•Nausea and vomiting
•Increased salivation
•Stomach cramping
•Convulsions
Acute fluoride toxicity treatment
• Immediate treatment
• Induced vomiting
Protection of the stomach by binding fluoride with orally administered calcium/aluminum preparations:
• MILK!
• Lime water or Maalox
Maintenance of blood calcium levels with intravenous calcium
Chronic toxicity
skeletal fluorosis
dental fluorosis
Purpose of toothbrushing
Removal of plaque biofilm and disturbance of its re-formation (to control and prevent periodontal diseases and carious lesions)
Removal of food, debris, and stain
Stimulation of the gingival tissues (remove biofilm from gingiva as well)
Application of a dentifrice containing specific ingredients to address caries, periodontal disease, or sensitivity

Tooth brush history
Chew sticks (siwak) found in Egyptian tombs in 3500 BC (1st oral hygiene care); twigs have antimicrobial properties (oils and tannins) and freshen breath
First toothbrush invented in China (1728); 1st modern day replica of a toothbrush
• Handle made of bone
• Bristles made of wild boar hair
Early 1900’s, first toothbrush was patented
• Switched from natural bristles to nylon bristles during WWI (able to change size and shape of bristles)
1916-Dr. Alfred C. Fones, founder of dental hygiene, wrote Mouth Hygiene; How to teach school children how to brush; public health out-reach program
• Developed Fones brushing method
• 1939-first power toothbrush was developed in Switzerland (Broxodent; had a cord)
1960s-US was introduced to it
1980s-electrical toothbrushes hit the market in the US
The first oral hygiene care product is dated all the back to ___ BC
3500
1st toothbrush was invented in China in
1728
The first toothbrush was patented in the early
1900s
In 1916, Dr. Alfred C. Fones wrote Mouth Hygiene and developed the __ brushing method
Fones
In 1939, the 1st power toothbrush was developed in Switzerland and it was called the
Broxodent

The US was introduced to powered toothbrushes in the
1960s
The electrical toothbrushes hit the US market in
1980s
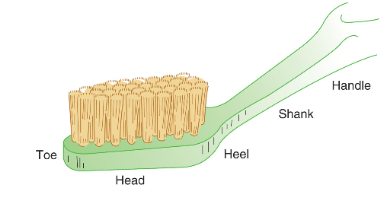
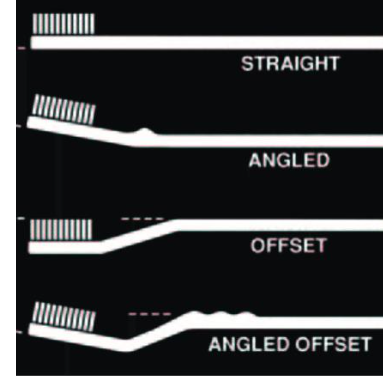
Manual toothbrush design
Head-working end, has bristles
Handle-part grasped; angulations can help ergonomic graso
Shank-connects head and hanlde
Sizes-large, medium small
Texture (hardness, firmness, stiffness) of the bristle-hard, medium soft, extra soft
Little evidence of the most effective characteristics of a toothbrush, so clinical expertise and individual patient needs should be considered (true/false)
true
When bristles are bunched together they are called
tufts
Which textures of the bristle is preferred? (hard, medium soft, extra-soft)
soft, extra soft
Why is medium and hard not recommended for bristle texture
can cause abrasions
What we recommend for manual toothbrush designs depends on
patient’s needs
Ex) small mouth need a small head or orthodontic patients needs a specific head
Manual toothbrush design Lateral Basic Profiles
Concave
Convex
Multilevel
Flat
Concave
short bristles in the middle
better for facial surfaces
Convex
long bristles in the middle
better for lingual surfaces
Multilevel
multi lengths=improved cleaning
effective in interproximal surfaces compared to flat
Flat
same bristle length
(Nylon/natural) bristles are superior
Nylon
Texture refers to
hardness, firmness, and stiffness of the bristle
Shorter bristles means the bristles are (stiffer/softer) and (more flexible/less flexible)
stiffer, less flexible
Nylon
• Superior to natural hog bristles
• Flex 10x more often before breaking
• Do not split
• Do not abrade
• Easier to clean
• Create Texture (End-rounding)-due to heat treatment; no sharp edges which decreases gingival trauma
Can be standardize (shape and stiffness of the bristles)
End rounding bristles are the result of ___ treatment
heat
Toothbrush handles
Provides comfort and compliance
Important aspects:
• Easy to hold
• Does not slip/rotate during use
• No sharp corners/projections
Durable
Moisture resistant (no mold)
Angles and curves may help reach hard to reach areas
Larger handle best suited for patients with limited dexterity which include: older patients, children, those with a disability
Note) can place a tennis ball at the end of a handle for an easier grip
Tooth selection is based on
Patient dexterity (larger handle?)
Gingival condition (slimmer bristle for subgingival? Bulbous tissue, receding gums/soft?)
Specific patient needs (powered over manual; size of mouth and handle)
Bristle Stiffness:
• Types of bristles/filaments
• Diameter
• Length
• Number of bristles/filament
Soft and extra soft are the golden rule!!!
Soft and extra soft bristles (are/aren’t) the golden rule
are
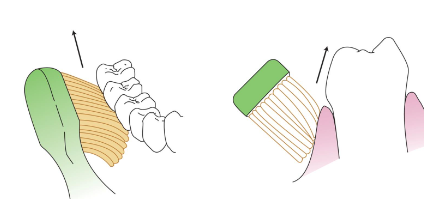
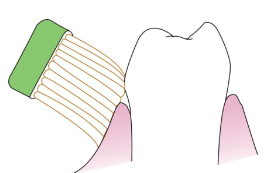
Bass Method
• Acceptable for all patients
• Periodontal Involvement
• Toothbrush bristles are angled apically at a 45-degree angle to the long axis of the tooth
• Filaments subgingival
• Jiggle with short horizontal strokes
• 2–3 teeth at a time
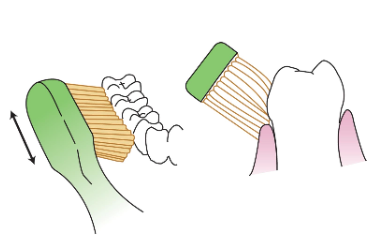
Rolling Method
• Most appropriate for children
• Bristles positioned apically along the long axis of the tooth
• Bristles rolled against the tooth from the apical position toward the occlusal plane
• Repeat several times
Stillman Method
• Bristles positioned apically along the long axis of the tooth
• Edge of the brush head touches the facial or lingual aspect of the tooth
• Brush is slightly rotated at a 45-degree angle and vibrated over the crown
• Massage and stimulate gingiva while cleansing cervical areas
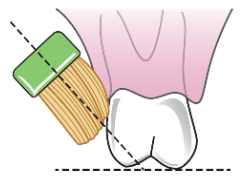
Charters Method
• Used to clean around appliances
• Bristles placed at a 45-degree angle toward the occlusal or incisal surface of the tooth
• Bristles should touch at the junction of the free gingival margin and tooth
• Circular vibratory motion is used
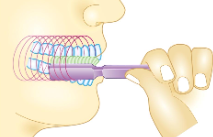
Fones method
• Used mainly by young children
• Teeth are clenched, brush is placed inside cheeks
• Brush moved in circular motions
• Can be damaging if done too vigorously
Leonard method
• Toothbrush is placed at a 90-degree angle to the long axis of the tooth
• Moved in a vertical, vigorous motion up and down the teeth

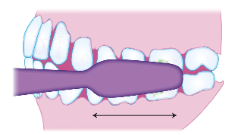
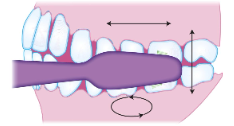
Horizontal method
• Teeth are edge to edge
• Brush maintains a 90-degree angle to long axis of tooth
• Horizontal strokes
• Can cause toothbrush abrasion
Smith Method
• Physiologic technique –follows the pattern of food during mastication
• Bristles are positioned directly onto the occlusal surface
• Brush is moved back and forth
• Recommends a few gentle horizontal strokes to clean the sulcus areas near furcations
Scrub technique
• Combination of horizontal, vertical, and circular strokes
• Incorporates vibration movements in certain areas
• Not an appropriate method
Which technique is not recommended for brushing?
Scrub
Modified brushing method
Integrates a rolling stroke after use of the vibratory motion
Brush position maintained after the completion of the original method's stroke
Bristles then rolled coronally over the gingiva and teeth
Used with any and all of the previous methods
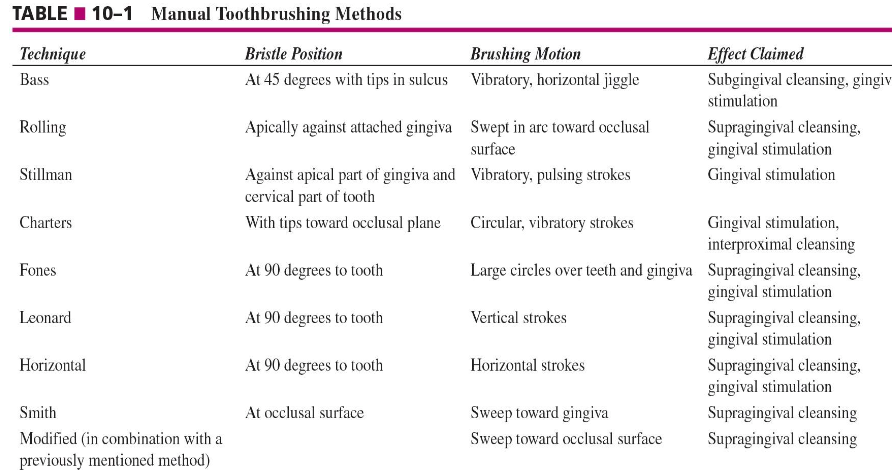
Summary of methods chart
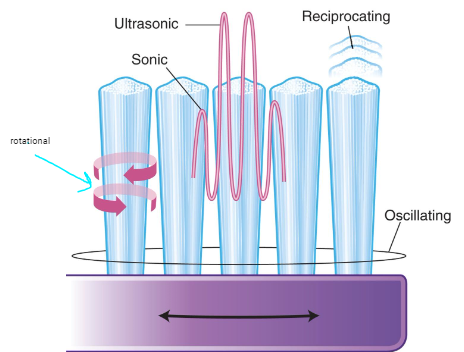
Powered toothbrushes
electric or battery operated
brush movements range from 3,800 to 7,600 per minute
Main pattern of movements: oscillation, reciprocation, rotational
Oscillation
bristles move in a constant back and forth motion
Reciprocation
up and down or back and forth movement
Rotational
circular pattern
Powered tooth brush movement
Sonic-sound waves that disrupt/break up biofilm
Ultrasonic-higher electrical frequency that disrupt biofilm
Ionic-temporarily reverse negative charge to a positive charge on a tooth that will help break up biofilm
Advantages of powered toothbrushes
• Helpful for
Parents who brush their children's teeth
• Physically or developmentally disabled
• Elderly or arthritic
• Dexterity issues (larger handle is easier to grasp)
Patients with a history of failed attempts at more traditional biofilm removal methods
Orthodontic patients
Patients undergoing complex restorative and prosthodontic treatment
Aggressive brushers
Caretaker must brush another person’s teeth
Faster brush movements compared to a manual brushing movements (true/false)
true
Powered toothbrushes should use __ pressure
light
lightly press bristles, don't press too hard since it may cause gingival recession some powered toothbrushes have sensors that warn you if there's excessive pressure
Time and frequency
2 minutes twice a day
Factors that can extend brushing time/frequency:
-Orthodontics brush longer/frequently
-Patients with higher sugar intake
How long should be brush?
2 minutes
How often should we brush?
Twice a day
Factors that extend brushing time and frequency
Orthodontics brush longer/frequently
Patients with higher sugar intake
Supplemental brushing (Tongue Scaper)
• Remove bacteria from tongue that the toothbrush may not be able to reach
Remove bacteria that induce halitosis (anaerobic bacteria that produce sulfur products)
ADA seal of acceptance
Marketing tool
Expensive process (larger corporations may have more compared to smaller companies)
Clinical assessment of toothbrushing
• Goal: Remove dental plaque biofilm from teeth without damaging teeth and surrounding structures.
• Prevent toothbrush abrasion
• Evaluation: Disclosing solution/tablets
Tablets may be taken home by patients! Chew one before brushing to see where the biofilm is (pink), they can brush and then take another tablet to evaluation brushing effectiveness
Toothbrush care
Rinse brush after every use
Store in a cool dry place (prevent moisture and therefore mildew and mold)
Replace toothbrush every 2-3 months
Can share if each person has a different brush head
Discard toothbrush after a contagious sickness
•Strep throat, flu, etc.
We can share manual toothbrushes (true/false)
false, biofilm is contagious
Ultimate goal for toothbrushing
remove dental plaque biofilm from teeth without damaging teeth and surrounding structures
You should replace a toothbrush every __ months unless the bristles worn out before then
2-3 months
Powered toothbrushes (can/can’t) be shared
can due to people having different brush heads
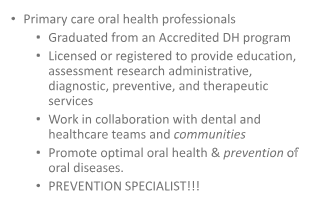
ADHA definition
The father of dental hygiene is
Dr. Alfred C. Fones (1900s)
The first licensed dentist hygienist is
Irene Newman
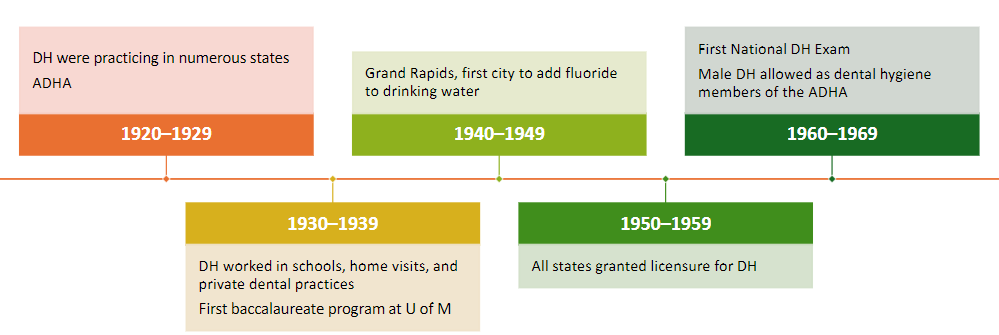
Events from 1910-1919
• First dental hygiene school in Connecticut
• First licensed dental hygienist, Irene Newman
• Hygienists were working in public school settings
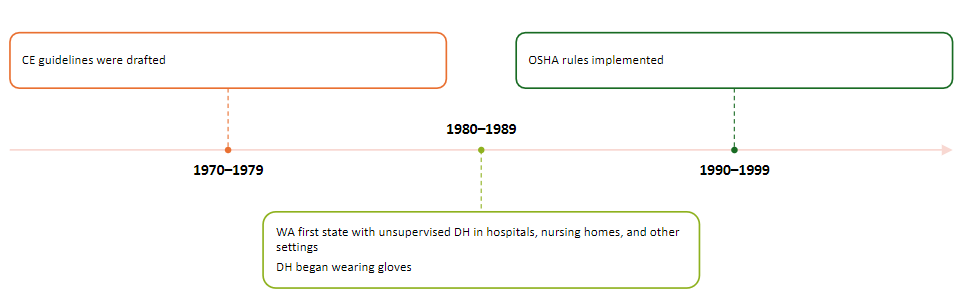
Timeline cont.
Timeline cont. 2
Basic roles of a DH
Education
Assessment
Diagnosis
Prevention
Nonsurgical therapy
Research
Administration
Entrepreneur
Education and prevention is the primary role of a dental hygienist (true/false)
true
Dental hygienists support oral health through their work in many settings including
general and specialty dental practices
public health programs
research centers
educational institutions
hospital and residential care facilities
federal programs, including the military
dental corporate industries
Professional roles of the DH
Clinician
Corporate
Public health
Research
Educator
Administrator
Entrepreneur