Fluid and Electrolyte Regulation in Health and Disease
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
Electrolytes
Minerals in the body that conduct electricity.
Basic metabolic panel (BMP)
A blood test that provides information on electrolytes and fluid balance, renal function, and glucose levels.
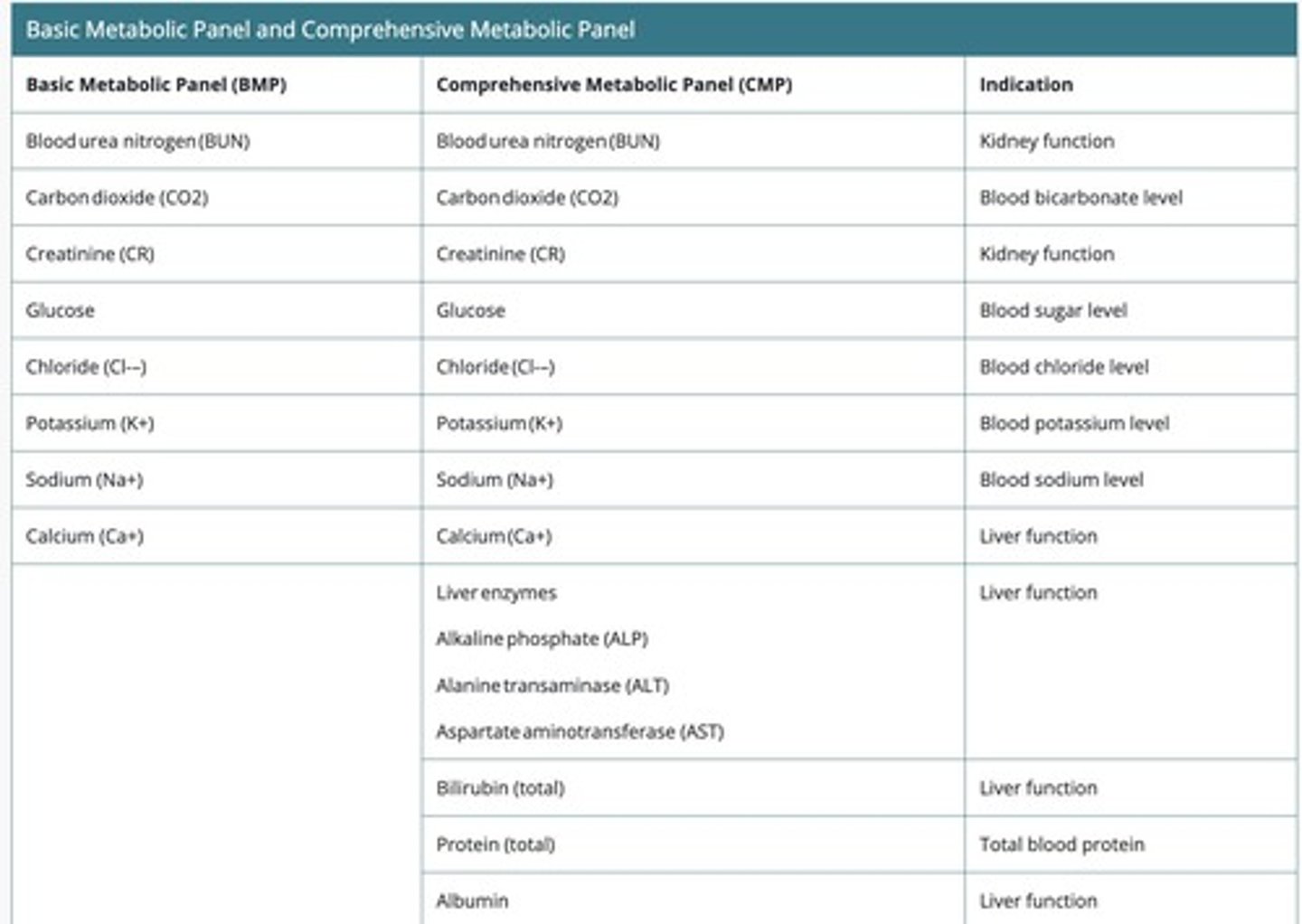
Complete metabolic panel (CMP)
Everything in a BMP + protein and liver function.
Serum Reference Range
285-295 mOsm/kg.
Urine Reference Range
50-1200 mOsm/kg.
Osmolality
A blood or urine test that can help monitor water and electrolyte balance.
Intracellular space
Space within a cell.
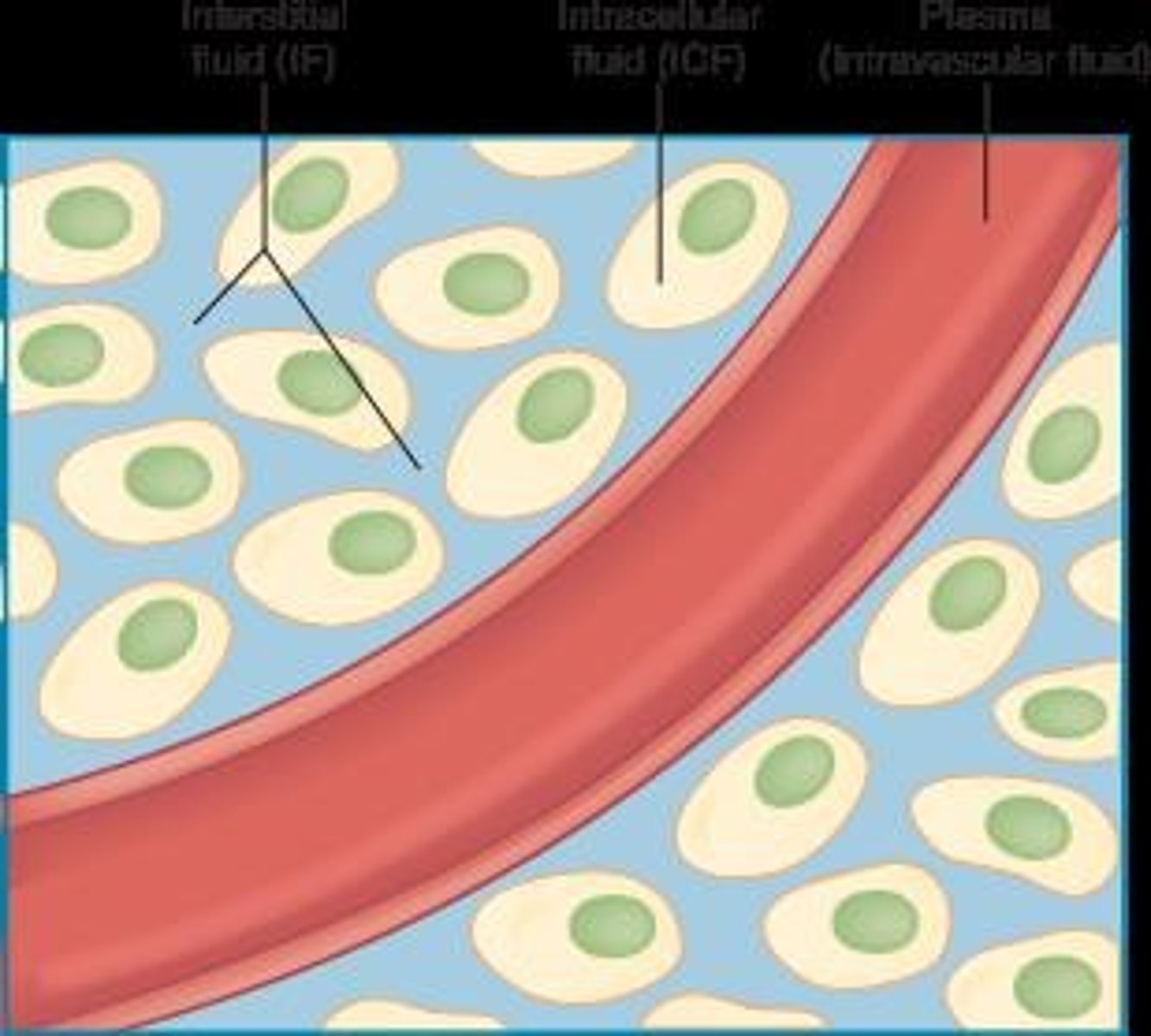
Extracellular space
Space outside the cell (interstitial + intravascular).
Interstitial space
Space outside of the cells.
Intravascular
Space within vasculature including chambers of the heart, arteries, and veins.
Osmosis
Movement of water across a semipermeable membrane.
Homeostatic mechanisms
Processes that help maintain stability in the body's internal environment.
Thirst response
Innate mechanism to promote water consumption.
Insensible fluid loss
Fluid loss that occurs without the person being aware, such as respiratory droplets and sweating.
Dehydration / Hypovolemia
A condition resulting from excessive fluid loss.
Overhydration / Hypervolemia
A condition resulting from excessive fluid intake.
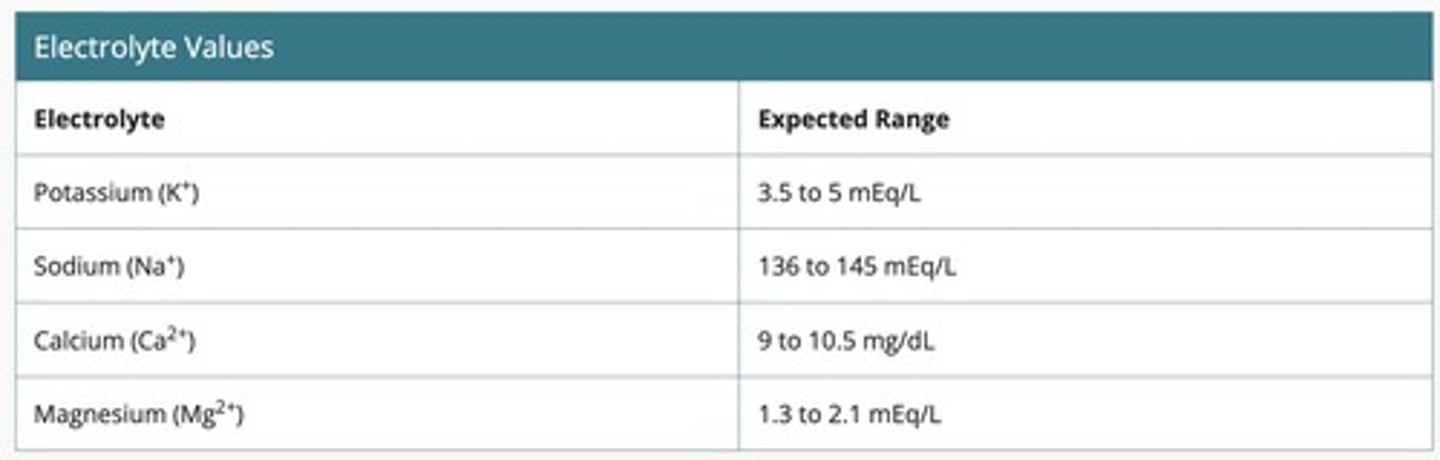
Potassium (K+)
Electrolyte with a serum level reference range of 3.5 - 5.0 mEq/L.
Recommended dietary allowance (RDA) for Potassium
Adult Males: 3400 mg, Adult Females: 2600 mg.
Hypokalemia
Serum level <3.5 mEq/L, may present with fatigue, constipation, muscle weakness, and cardiac arrhythmias.
Critical lows for Hypokalemia
Critical lows: <3 mEq/L in adults; Severe life-threatening: <2.5 mEq/L.
Symptoms of Severe Hypokalemia
Respiratory paralysis/failure, paralytic ileus, hypotension, tetany, rhabdomyolysis.
Hypokalemia
A condition characterized by low potassium levels in the blood.
Hypokalemia: Treatment
Starts with identifying the underlying cause, which may include medications, diuretics, certain cardiac conditions, GI loss, metabolic alkalosis, decreased oral intake, excessive alcohol use, chronic kidney disease, diabetic ketoacidosis, excessive sweating, and folic acid deficiency.
Hypokalemia: Routine tests
CMP/BMP.
Hypokalemia: Replacement Options
Oral supplementation, IV supplementation, encourage high potassium foods, and changing to a potassium-sparing diuretic.
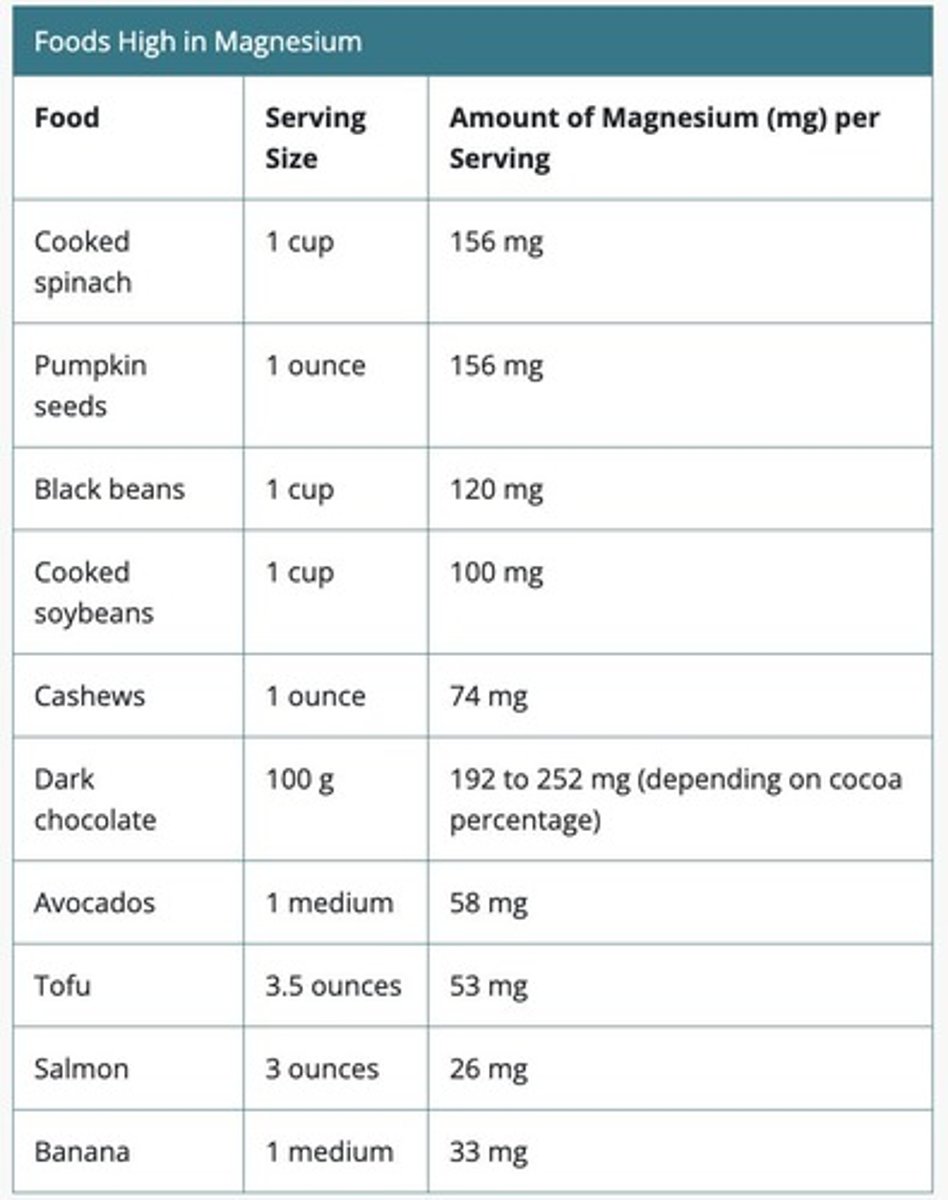
High Potassium Foods
cooked spinach, pumpkin seeds, black beans, cooked soybeans, cashews, dark chocolate, avocados, tofu, salmon, banana
IV Potassium - SAFETY
If given incorrectly, the patient can suffer GREAT HARM. Must be diluted in 100 - 1000ml compatible solution. Dose should not exceed 40 mEq/L unless treating severe hypokalemia. Rate of administration: 10-20 mEq/hour. Continuous ECG monitoring must be in place. Serum levels need to be rechecked periodically. NEVER EVER IV PUSH IV POTASSIUM.
Hyperkalemia
A condition characterized by high potassium levels in the blood.
Hyperkalemia: Serum Levels & Presentation
Serum level >5.0 mEq/L; critical high: >6 in adults. Mild hyperkalemia (5.1-5.9) is usually asymptomatic but increases the risk for life-threatening cardiac dysrhythmias, muscle weakness, and paralysis. Severe/life-threatening hyperkalemia (>7 mEq/L) can lead to paralysis, heart failure, and death.
Hyperkalemia: Treatment
Starts with identifying the underlying cause, which may include renal failure, dehydration, diabetes mellitus, medications, trauma, excess intake of this electrolyte, burns, transfusion of pRBCs, acidosis, and sepsis.
Hyperkalemia: Routine tests
CMP/BMP.
Hyperkalemia: Removing excess potassium
Hemodialysis if due to renal failure, loop and thiazide diuretics, resin medication: sodium polystyrene sulfonate, and insulin (must monitor glucose simultaneously).
Hyperkalemia: Stabilize the heart
Calcium gluconate or calcium chloride.
Sodium (Na+)
136-145 mEq/L; major electrolyte in ECF and present in most body fluids and secretions.
Functions of Sodium
Neurologic/neuromuscular function, fluid balance regulation, and maintaining blood pressure.
Sodium RDA
<2300 mg per day = approx. 1 teaspoon.
Hyponatremia
A condition characterized by low sodium levels in the blood.
Hyponatremia: Serum Levels & Presentation
Serum level <136 mEq/L; critical level: <120 mEq/L. Mild hyponatremia (130-134) presents as general unwellness; moderate (125-129) includes lethargy and confusion; severe (<125) can lead to muscle twitching, worsening LOC, seizures, coma, and possible death if untreated.
Hyponatremia: Treatment
Starts with identifying the underlying cause, which may include medications, chronic or severe vomiting or diarrhea, drinking excess amounts of water, excess alcohol intake, heart, kidney, and liver problems, and severe burns.
Hyponatremia: Raise sodium levels
Raise sodium levels slowly to avoid overcorrection and prevent further neurologic issues.
Hyponatremia: Routine tests
CMP/BMP and urinalysis - sodium level.
Hypernatremia
A condition characterized by high sodium levels in the blood.
Hypernatremia: Serum level
Serum level >145 mEq/L; critical level: >160 mEq/L.
Hypernatremia: Physiology
Body water loss > solute loss (leaving Na+ behind), too much sodium present in the body, or a combination of both.
Hypernatremia: Diagnosis
BMP / CMP; Plasma Osmolality >295 mOsm/kg
Hypernatremia: Treatment
Address the underlying cause; Initiate IVF replacement containing water and small amount of sodium; Possibly a low sodium diet; Decrease sodium levels slowly to reduce cerebral edema.
Hypernatremia: Patient Education
Avoiding high salt foods; Importance of adequate hydration.
Hypernatremia: Possible Causes
Loss of body water; Infants and older adults are at most risk; Medications; Gastroenteritis; Vomiting; Prolonged Suctioning; Burns; Excessive Sweating; CKD; DM; Impaired thirst response.
Calcium: Background
Most abundant mineral in the body; 99% found in bones and teeth; The rest: our blood and various other cells.
Calcium: Main Functions
Bone mineralization; Muscle contraction; Nerve transmission; Clotting time of blood; Hormone secretion; Normal heart function.
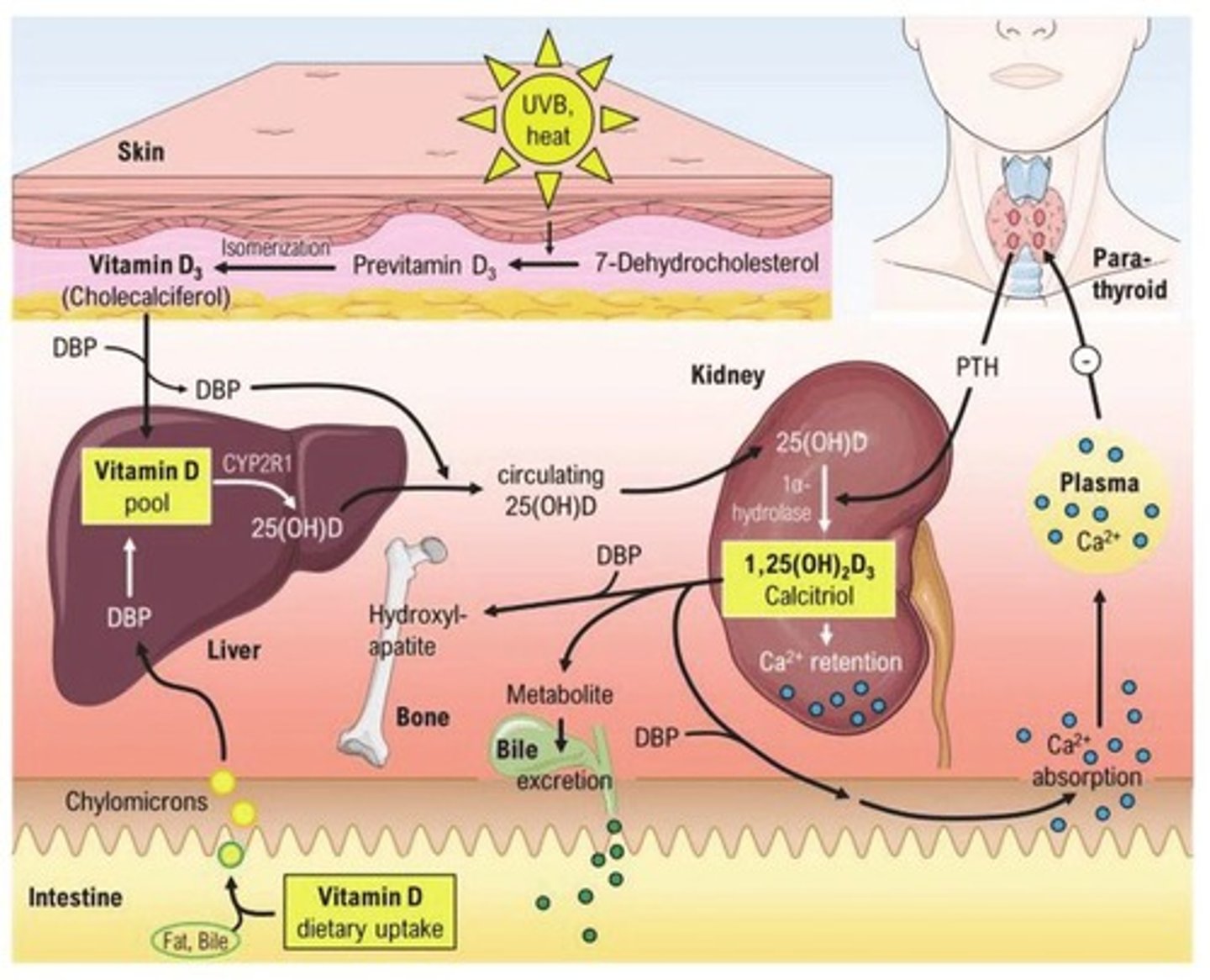
Calcium Absorption
Absorption into the body depends on adequate supply of Vitamin D.
RDA Vitamin D
600 IU (adults); 800 IU (elderly).
RDA Calcium
Depends on age; Young children; Teenagers; Older adults, especially women.
Calcium Excretion
Excreted through the kidneys which is signaled by the Parathyroid Gland.
Calcium: Serum Levels
Serum: 9-10.5 mg/dL; Ionized Calcium: 4.5-5.6 mg/dL.
Ionized Calcium
Represents active, unbound amounts of calcium in the blood; Generally estimated to be 50% of one's total calcium.
Hypocalcemia: Serum Levels
Serum: < 9 mg/dL; Ionized: <4.5 mg/dL; Critical values: Serum: < 6 mg/dL; Ionized: < 2.2 mg/dL.
Hypocalcemia: Multi-system Effects
Respiratory, Cardiac, Neuro, MSK, Integumentary.
Hypocalcemia: Presentation - CVD
Chest pain, dysrhythmias, heart failure, syncope.
Hypocalcemia: Presentation - Respiratory
Wheezing, larynx spasms, dysphagia, voice changes.
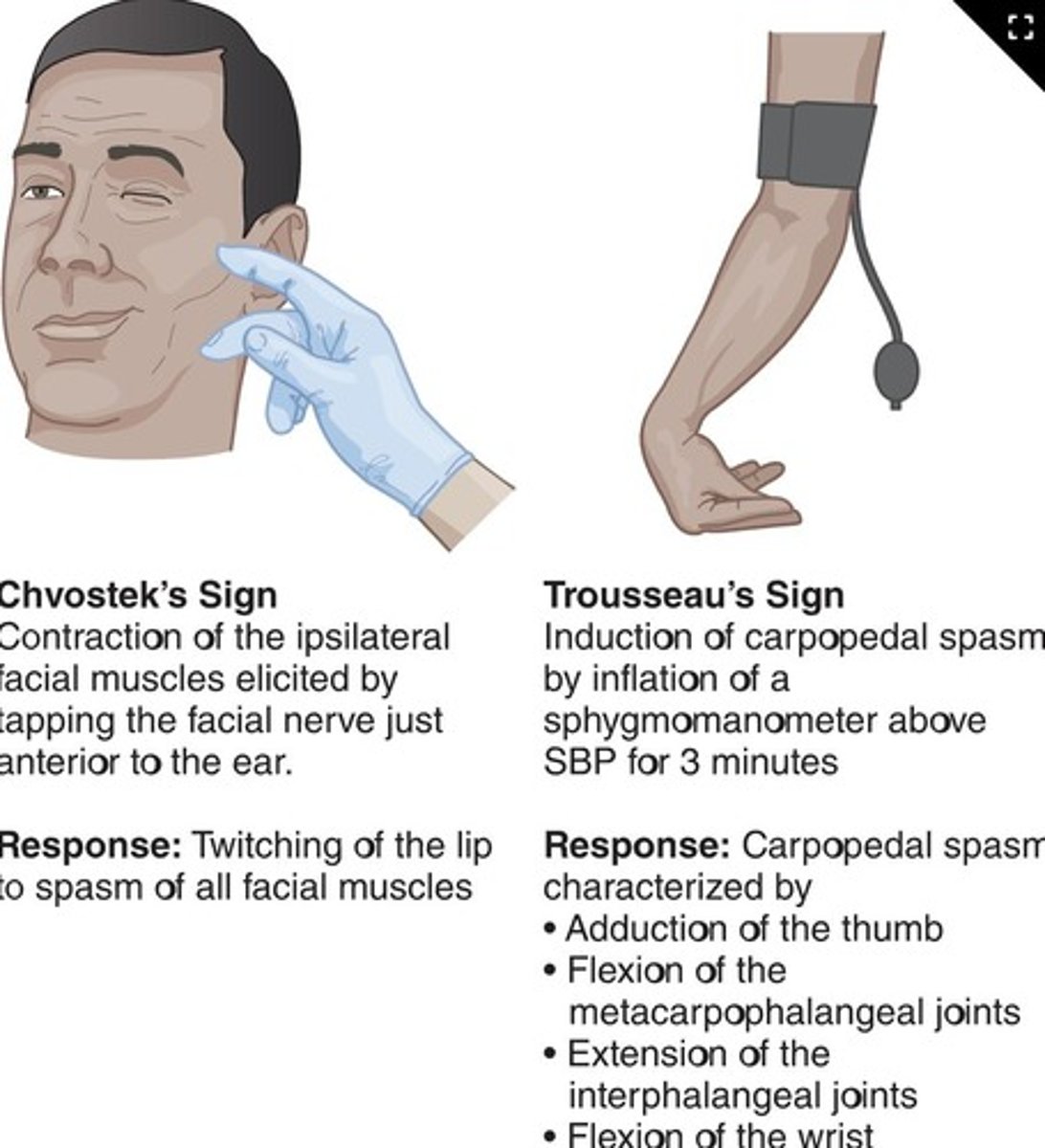
Hypocalcemia: Presentation - Neuro/MSK
Peripheral neuropathy, muscle cramping, spasms of back and lower extremities; Confusion, vision difficulties, depression, psychosis, dementia, lethargy, seizures, personality changes.
Hypocalcemia: Presentation - Integumentary
Course hair, alopecia, dry skin, itching; Dental problems.
Hypocalcemia: Treatment
Depends on severity; May self-resolve or may need supplementation, dietary changes, or injections of this electrolyte
Hypocalcemia: Patient Education
Instruct on high calcium foods; Limit calcium supplements to < 600 mg/day to promote absorption; Risks to health r/t hypocalcemia.
Hypercalcemia: Serum Levels
Serum: > 10.5 mg/dL; Ionized: >5.6 mg/dL; Critical levels: Serum: >13 mg/dL; Ionized: >7mg/dL.
Hypercalcemia: Complications
Kidney stones, weak bones, brain/heart functioning.
Hypercalcemia: Presentation - Mild
Asymptomatic.
Hypercalcemia: Presentation - Moderate
GI effects (constipation, abdominal pain, N/V, anorexia).
Hypercalcemia: Presentation - Severe
Neuro changes (confusion, behavioral change, increased thirst); polyuria; bone pain; muscle weakness.
Hypercalcemia
Can lead to arrhythmias, delirium, and renal failure.
Magnesium
Most common intracellular electrolyte; 50-60% in the bones; Reference range: 1.3-2.1 mEq/L; Intake: whole foods, supplements, medications; Output: urine/feces; Main Functions: Nerve/Muscle function, Maintain BP, Maintain serum glucose levels, Support bone/teeth health, Synthesize DNA and RNA; RDA: Adult male: 400-420 mg/day, Adult female: 310-320 mg/day.
Hypomagnesemia
Serum: <1.3 mEq/L; Critical low: <0.5 mEq/L; Clinical Signs: Moderate: Nausea, vomiting, decreased appetite, weakness; Severe: Neuro/MSK changes - muscle cramps, spasms, neuropathy, seizures, tetany, personality changes; Cardiac dysrhythmias (*along with other electrolyte disturbances).
Hypomagnesemia: Treatment
Address underlying cause: Medications (Thiazides, certain abx, PPIs), Decreased intake, Decreased absorption by intestines, Increased excretion by GI tract or kidneys, Excessive alcohol use, T2DM; Poor nutrition, Severe burns, Electrolyte imbalances; Therapies: PO magnesium replacement, IV magnesium replacement if needed, Increase magnesium via diet.
High-Alert Medications: IV Magnesium
Doses should be double-checked with another nurse; Concentration and rate must be validated; Risks: flushing, sweating, potentially respiratory depression if administered too quickly; Neuro risk: decrease LOC if concurrent with a CNS depressant; Monitor urine output!
Hypermagnesemia
Serum level: >2.1 mEq/L
Mildly high Hypermagnesemia
Levels: < 7 mgd/L; Symptoms: Nausea, dizziness, confusion, weakness
Moderately high Hypermagnesemia
Levels: 7-12 mgd/L; Symptoms: Increased neuro sxms: confusion, sleepiness, blurred vision, headaches, decreased reflexes, bladder paralysis, flushing, constipation
Severely high Hypermagnesemia
Levels: >12 mg/dL; Symptoms: Muscle flaccidity, paralysis, decreased RR, hypotension, bradycardia, dysrhythmias
Critical Hypermagnesemia
>15 mg/dL: Seizures, coma, cardiac arrest, and death
Hypermagnesemia Treatment
Address the underlying cause: Kidney disease (acute or chronic), Excessive intake, Decreased GI motility, Medication side effects (Opioids; Anticholinergics)
Hypermagnesemia Medications
Containing Mg: Laxatives, Antacids (Maalox, Mylanta), Lithium
Hypermagnesemia Therapies
Mild cases: Eliminating intake; Severe cases: IV calcium gluconate or calcium chloride, IV diuretics with IV saline, Hemodialysis (if needed)
Dehydration
A loss or lack of water intake without a concomitant loss of sodium
Dehydration Causes
Possible causes: vomiting, diarrhea, diaphoresis, polyuria, illness, fevers, insufficient of water/fluids, inadequate thirst response
Dehydration Presentation
Altered cognitive/neuro-MSK functions; thirst; dry mucosa; oliguria; tachycardia; hypotension; lactic acidosis; shock; coma/death
Dehydration Diagnosis
Lab tests: CMP / BMP = shows hypernatremia, Serum osmolality = elevated, Urine specific gravity = elevated
Dehydration Treatment
Restore water balance in the body; PO: if awake/alert/safe; IV: slow infusion of D5W
Hypovolemia
AKA "Fluid Volume Deficit" (FVD); Loss of BOTH fluid AND electrolytes
Hypovolemia Causes
Possible causes: blood loss, GI loss, severe burns, third spacing, excessive sweating, fever, medications trauma
Hypovolemia Early Signs
Thirst, dry mucous membranes, decreased skin turgor, decreased urine output
Hypovolemia Late Signs
Lethargy, muscle weakness, orthostatic hypotension, tachycardia, chest pain, tachypnea, palpitations, oliguria, hypotension
Hypovolemic Shock
>20% or 1/5 of total body fluid is lost; If not reversed: MULTIORGAN FAILURE
Hypovolemia Diagnosis
CMP/BMP: electrolyte imbalances, increased BUN and CR; CBC: Hct/Hb levels; Urine: highly concentrated with little sodium present
Hypovolemia Treatment
Depends on cause; Goal: control fluid/blood loss; Replace and restore circulation
Hypovolemia Nursing Interventions
Assess vital signs and changes in the physical exam; Monitor I&O; Notify provider of output <30 ml/hr
Hypervolemia
Body has too much water in the extracellular space, particularly the interstitial space
Hypervolemia Causes
Heart failure, Kidney failure, Nephrotic syndrome, Cirrhosis or end-stage liver disease, Pregnancy, Medications (Vasodilators, CCB, glitazones)
Hypervolemia Diagnosis
Physical Exam: weight, edema checks, full head-to-toe; Labs: Sodium levels can be low, high, or normal
Hypervolemia Treatment
Manage the root cause(s); Remove excess fluid; Diuretics; Fluid and sodium restrictions for intake
Gerontologic Considerations
Vulnerable to imbalances due to age-related changes: Less efficient cardiovascular and renal system, Decreased thirst sensation, Decline in total body fluid, Polypharmacy, Underlying health conditions