Unit 5 - Basic Gait
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
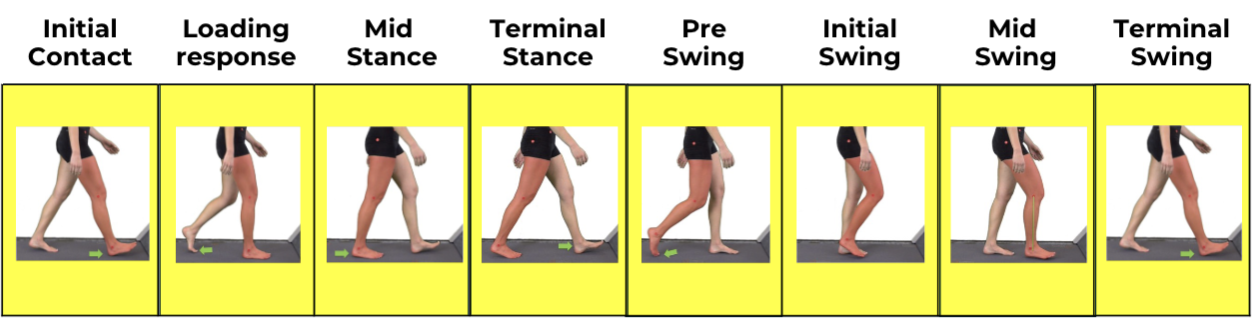
Rancho Los Amigos Phases of Gait
Review of Typical Gait
Gait Parameters: Temporal
cadence
stride and step time
velocity
Review of Typical Gait
Gait Parameters: Spatial
velocity
stride and step length
step width
foot angle
Identifying/Documenting Gait Deviations
Note WHEN the deviation(s) occur: Swing or Stance Phase and which sub-phase e.g., Initial Contact, Loading Response
Ex: Foot drag noted during swing
Describe WHAT the deviation consists of: e.g., rapid ankle plantarflexion during loading response causing a foot slap
Ex: R foot drag during swing
Add impact (RESULTS) on 3 functional tasks of gait: (Weight acceptance, SLS, Swing leg advancement)
Ex: L lateral trunk lean during R swing
Hypothesize possible Impairments causing (WHY) the gait deviation: e.g., foot slap during loading response could be due to weak ankle dorsiflexors
Ex: Delayed ankle temporal sequencing
Observational Gait Analysis
sagittal and frontal
Gait Analysis
notice deviations
determine impairments
Test, Test, Test!!
Analyze hypothesized impairments
Identify what is actually contributing to the deviations
Develop interventions
Task Oriented Approach
Motor Relearning Programme
Augmented intervention
Compensatory strategies
Impairment-based interventions
Part to Whole Task
Pre-gait —> gait
Part to Whole Task
Pre-Gait Indications
Increased comfort
LE WB in stance
Single Leg Stance
Proprioception
Part to Whole Task
Gait
Carryover to whole-task
Continuous task practice
Promote Motor Learning
Gait: Strength
Overview
Gait as a complex, dynamic process
There should be sufficient strength in the upper and lower extremities for effective gait
Focus: Impairment management in physical therapy to improve strength and gait performance
Gait Cycle Overview
Phases of the Gait Cycle:
Stance Phase 60%
Swing Phase 40%
Muscle control important in each phase
Gait: Strength
Upper Extremities
Reciprocal arm swing
Muscles: deltoids, trapezius, latissimus dorsi
Role in trunk rotation, balance, and momentum
Gait: Strength
Lower Extremities
Stance phase: glutes, quadriceps, calves
Swing phase: hip flexors, hamstrings, dorsiflexors
Function: stabilization, propulsion, clearance
Gait: Strength
Arm Swing and Balance
Counterbalance for lower extremities
Assist with maintaining posture and forward momentum
Gait: Strength
Strength Contribution
Role of shoulder, elbow, and wrist muscles in supporting gait dynamics
Gait: Strength
Role of Lower Extremities in Gait
Coordination
Alternating movement: stance and swing phase
Strength Contribution
Power generation for forward propulsion
Stability during stance phase
Gait: Strength
Effects of UE Weakness
Reduced arm swing → decreased trunk rotation
Poor balance control
Compensation via increased trunk motion
Gait: Strength
Effects of LE Weakness
Gluteus medius weakness → Trendelenburg gait
Quads weakness → knee instability
Dorsiflexor weakness → foot drop, toe drag
Gait: Strength
Common Impairments in Gait
Weakness in Lower Extremities
Foot drop
Knee instability
Decreased hip stability
Upper Extremity Impairments
Reduced arm swing
Poor posture affecting balance
Impact on Gait Patterns
Gait: Strength
Functional Consequences on Gait
Decreased walking speed
Increased energy cost
Higher fall risk
Altered posture & compensatory movement patterns
Gait: Strength
Assessment of Muscle Strength
MMT (Manual Muscle Testing)
Handheld dynamometry
Functional gait analysis (10MWT, TUG, 6MWT)
Gait: Strength
Strengthening Interventions: UE
Improve postural control and arm swing
Exercises: shoulder flexion/extension, lats pulldowns, scapular stability
Gait: Strength
Strengthening Interventions: LE
Focus muscles: glutes, quads, hamstrings, dorsiflexors, calves
Examples: bridges, step-ups, resisted marching, toe raises
Gait: Tone
Types
Normal
Hypotonia
Hypertonia (Spasticity, Rigidity)
Gait: Tone
Impairment Management
Tone’s role in postural control and movement
Gait:
Phases: Stance phase & Swing phase
Reciprocal movement
Coordination and timing in gait
Gait: Tone
Tone in UE
Reduced arm swing
Poor postural control
May rely on compensatory trunk movements
Reduced coordination and stability
Gait: Tone
Tone in LE
Hypertonia (e.g., spasticity in calf muscles): toe walking, stiff-legged gait
Hypotonia: poor push-off, knee buckling
Muscle groups commonly affected: gastrocnemius, hamstrings, quadriceps
Gait: Tone
Hypertonicity in Gait (UE) —> Common Presentation & Impact on Gait
Common Presentation
Flexor synergy patterns: shoulder adduction, elbow flexion
Minimal arm swing
Balance and trunk rotation affected
Impact
decreased efficiency, asymmetry
Gait: Tone
Hypertonicity in Gait (LE) —> Common Presentation & Impact on Gait
Common Presentation
Equinus foot (tight calf)
Knee hyperextension
Hip adduction (scissoring gait)
Impact
Reduced step length, poor foot clearance
Gait: Tone
Hypotonicity in Gait (UE) —> Common Presentation & Impact on Gait
Common Presentation
Reduced arm swing
Poor postural control
Impact
May rely on compensatory trunk movements
Gait: Tone
Hypotonicity in Gait (LE) —> Common Presentation & Impact on Gait
Common Presentation
Poor push-off during terminal stance
Difficulty with knee control → buckling
Impact
Wide base
Slow, unsteady gait
High risk of falls
Gait: Tone
Gait Patterns Seen with Hypertonia
Spastic hemiplegic gait: Stiff leg, circumduction
Scissoring gait: legs cross midline due to hip adduction
Decreased stride length and cadence
Poor foot clearance
Gait: Tone
Gait Patterns Seen with Hypotonia
Ataxic gait: Unsteady, wide-based, irregular steps
Trendelenburg gait: Hip drop due to weak abductors
Joint hypermobility → compensatory overuse
Gait: Tone
Physical Therapy Goals
Improve functional mobility
Normalize tone as much as possible
Prevent contractures or instability
Improve reciprocal movement
Improve postural control
Enhance gait efficiency and safety
Gait: Tone
Interventions for Hypertonicity
Passive and active ROM
Positioning to reduce synergy patterns
Neuromuscular re-education
Functional arm tasks during ambulation
Constraint-Induced Movement Therapy (CIMT)
Stretching and prolonged positioning
Weight-bearing and gait training
Orthotics (e.g., AFOs)
Functional Electrical Stimulation (FES)
Botulinum toxin injections
Task-specific training
Gait: Tone
Interventions for Hypotonicity
Strengthening and endurance training
Core stabilization and postural control
Balance and proprioception exercises
Assistive devices as needed (canes, walkers)
Task-specific practice to improve motor learning
Gait: Tone
Common Neurological Conditions Affecting Tone
Stroke
Cerebral palsy
Multiple sclerosis
Parkinson’s disease
Spinal Cord Injury
Other traumatic and neurological conditions
Gait: Ataxia/Incoordination
Ex: Safety Considerations
Guard the patient appropriately: gait belt, use safety harness when necessary
Assess for fall risk established outcome measures
Improve overall balance and postural control with activities
Improve coordination and overall lower limb progression sequence
Improve overall confidence in ambulation
Fall prevention education
Gait: Ataxia/Incoordination
Ex: Interventions —> Pre Gait activities
Static trunk control: Sitting and Standing
Weight shifts in standing
Forward and side stepping with upper limb support > progress to without upper limb support
Turning around in place: with and without upper limb support
Initial gait training in parallel bars, focus is on proper lower limb progression
Gait: Ataxia/Incoordination
Ex: Interventions —> Gait training: Improving gait pattern
Practice stepping over obstacles: initially had a smaller height, progress to at higher height
Practice weight shifting: front and back, side to side
Marching in place
Walking forward with emphasis on feet at shoulder width distance and symmetrical step length
Use external cues: auditory, tape on ground (visual)
Gait: Ataxia/Incoordination
Ex: Interventions —> Gait training: Progression
Ambulating in a closed space to ambulating in a busy clinic area
Continue to evaluate the use of assistive devices with the idea that the patient should be progressed safely to the less use of assistive devices
Ambulating on hard surfaces to carpeted surfaces and ambulating up and down a ramp
Use of technology such as VR systems to improve ambulation
Gait: Ataxia/Incoordination
Ex: Home Exercise Program
Prioritize safety: patient and caregiver education
Encourage functional performance: ambulating to mailbox, backyard
Promote confidence and independence
Gait: Somatosensation
Impact on Basic Gait
These sensations guide limb positioning and movement awareness during gait
Basic gait involves part-to-whole task training, single leg stance, and continuous task practice
Deficits in somatosensation impair foot clearance, weight shifting, and balance
Gait: Somatosensation
Ex: Treatment Considerations
Emphasize proprioceptive retraining for knee and ankle
Use repetitive, task-specific, and meaningful interventions
Utilize visual, tactile, and auditory cues
Incorporate dual-task or sport-relevant elements to enhance saliency
Gait: Somatosensation
Ex: Compensatory Interventions
Mirror feedback during overground/treadmill walking
Visual floor targets
Metronome pacing
AFO or brace
Verbal/tactile cues
Gait: Somatosensation
Ex: Restorative Interventions
Weight-bearing drills
Compliant and noncompliant surfaces
Task specific training
Dual-task
Gait: Vision
Vision in Basic Gait
Visual Input for Postural Control and Balance
Spatial Orientation and Navigation
Compensatory Gait Strategies Due to Visual Deficits
Increased Fall Risk and Safety Concerns
Gait: Vision
Ex: Treatment Considerations
Improve safe and functional ambulation
Enhance visual-motor integration
Promote independence in mobility
Reduce fall risk
Foster motor learning
Gait: Vision
Ex: Compensatory Interventions
Environmental Modifications
Assistive Strategies
Cueing
Gait: Vision
Ex: Restorative Interventions
Visual-Motor Retraining
Task-Oriented Gait Practice
Gait: Balance
Upright Mobility
Ability to move the body from one place to another while in an upright position:
Walking
Running
Inclined climbing/Stair climbing
Gait: Balance
Upright Mobility requires…
Progression in the desired direction
Postural control and balance
Adaptation to the task and demands of the environment
Gait: Balance
Primary Impairments Affecting Gait
Muscle weakness
Decreased joint ROM
Sensory loss
Poor control of limb segments
Difficulty with balance/coordination
Perceptual impairments
Cognitive impairments
Gait: Balance
Secondary Impairments Affecting Gait
Progression of muscle weakness and limitations in joint mobility
Deconditioning
Skin breakdown
Obesity
Cardiovascular disease
Gait: Balance
Safety Considerations
Assess for fall risk using reliable and valid assessment tools
Include single and dual task activities
Use different surfaces: hard tile, carpet, sand etc.
Identify intrinsic and extrinsic risk factors
Perform home safety assessment
Fall prevention education
Guard the patient appropriately: gait belt, use safety harness when necessary
Gait: Balance
Interventions: General Approach —> Develop a plan of care: Intervention approach
Restoration/Remediation
Neural plasticity: role of experience in neural plasticity
Compensatory
Patient and family education
Referral to other health care providers
Gait: Balance
Interventions: General Approach —> Rehabilitation Approach
Therapeutic exercises
Task-specific functioning training
Use of devices and equipment to support functional mobility
Gait: Balance
Interventions: General Approach —> Prerequisites for gait
Strength training: LE, trunk and UE muscles
Sit to stand training
Standing balance training
Pre-gait training
Gait: Balance
Interventions: General Approach —> Assistive devices for gait training
Overground or body-weight supported treadmill training
Walkers and canes
Ankle Foot Orthosis (AFOs) and knee braces
Functional Electrical Stimulation (FES)
Gait: Balance
Task Specific Functional Training
Body weight-supported treadmill training
A body weight system includes a harness that is placed around the patient’s low trunk and attached to an overhead mobile frame or ceiling track
Percentage of body weight-support depends on the patient’s strength and balance control
Patients practice ambulation without fear of falling
Improvements seen in muscle strength, balance and mobility
Gait: Balance
Clinical Decision Making
Restorative vs compensatory training considerations
Patient goals and life roles
Severity of the condition and/or progressive nature of the condition
Acuity of the condition
Secondary complications
Chronic conditions
Co-morbidity
Cognitive and behavioral issues
Financial support
Discharge destination
Gait: Perception/Cognition/Communication
Perception Involved in Basic Gait
Spatial awareness affects step length, direction, and surface navigation
Visuospatial deficits may cause veering or unsafe foot placement
Figure-ground challenges hinder obstacle negotiation
Deficits reduce safety and independence in community ambulation
Gait: Perception/Cognition/Communication
Cognition Involved in Basic Gait
Attention and memory guide gait sequencing and adaptability
Divided attention increases fall risk in dual-task settings
Executive dysfunction reduces hazard detection and motor correction
Gait: Perception/Cognition/Communication
Communication Involved in Basic Gait
Language comprehension influences response to instructions during gait
Expressive impairments limit ability to share concerns or discomfort
Miscommunication can compromise safety and participation
Gait: Perception/Cognition/Communication
Ex: Treatment Considerations
Emphasize symmetrical gait training and midline orientation
Incorporate structured visual and tactile cues for foot placement
Use simplified, step-by-step verbal instructions
Minimize environmental distractions during early sessions
Integrate visual scanning and perception drills during gait
Progressively increase cognitive demands with dual-task practice
Gait: Perception/Cognition/Communication
Ex: Compensatory Interventions
Use floor markers
Provide structured verbal cues
Minimize environmental distractions
Use visual prompts
Gait: Perception/Cognition/Communication
Ex: Restorative Interventions
Repetition of symmetrical gait with fading of cues
Visual scanning tasks to enhance spatial awareness
Obstacle navigation with cognitive overlay (naming, counting)
Task-specific training in varied real-world environments
Gait: Movement Disorder
Ex: Gait Impairments in PD
Reduced step length and arm swing
Balance impairment and increased fall risk
Decreased gait speed
Stooped posture
Decreased trunk rotation
Shuffling gait / Festination
Gait: Movement Disorder
Ex: Gait Impairments in PD —> Interventions
Develop a plan of care
Approach:
Restorative/remediation
Compensation
Task specific functional training
Use of assistive devices and equipment
Fall prevention education
Patient and family education
Home exercise program
Gait: Movement Disorder
Ex: Interventions—> General Approach
Cues:
Auditory: metronome, counting
Visual cues: cones, markings on ground, laser light
Manual cues: PNF techniques prior to treatment: Rhythmic initiation, contract relax
Posture: use of mirror or video recording to give cues for upright posture
Strength: to improve functional performance
Gait: emphasize larger, bigger steps (focus on normal gait progression)
Balance and Fall prevention
Assess for the need for assistive devices: rollator walker, U-step walker
Gait: Movement Disorder
Ex: Interventions—> Task Specific Training
Freezing of gait: 4S’s
Stop
Stand tall
Sway (sway side to side before stepping)
Step big
Treadmill training, including body weight supported treadmill training
Overground training
Obstacle course training
Dual task training
Robotic assisted walking
Gait: Extrinsic Feedback Strategies
What is gait?
A rhythmical, repetitive movement pattern distinguished by a characteristic sequence of limb & trunk movements.
Involves forward propulsion, postural control & balance, & adaptation to environmental conditions
Gait: Extrinsic Feedback Strategies
Stance phase: IC
Moment the foot contacts the ground
Gait: Extrinsic Feedback Strategies
Stance phase: LR
Rapid transfer of weight onto the stance limb. 1st period of double support
Gait: Extrinsic Feedback Strategies
Stance phase: MSt
Body progresses over a single, stable limb
Gait: Extrinsic Feedback Strategies
Stance phase: Tst
Continued progression over the stance limb. Body moves ahead of the limb; weight transferred onto forefoo
Gait: Extrinsic Feedback Strategies
Swing phase: PSw
Rapid unloading of stance limb as weight transferred onto the contralateral limb. 2nd period of double support
Gait: Extrinsic Feedback Strategies
Swing phase: ISw
Thigh begins to advance as foot clears the floor
Gait: Extrinsic Feedback Strategies
Swing phase: MSw
Thigh continue to advance as the knee begins to extend & foot clears the ground in forward progression
Gait: Extrinsic Feedback Strategies
Swing phase: TSw
Knee extends; the limb prepares to contact the ground for initial contact
Gait: Extrinsic Feedback Strategies
Task Analysis: Stage of Learning —> Initial (Cognitive)
Provide lots of visual FB
Demonstrate task
Emphasize desired outcome & critical task elements
Provide KR to reinforce successful movement outcomes
Provide KP when errors are consistent
Allow for trial-&-error learning
NOTE: Although constant FB improves performance in early learning, it is important to start incorporating variable FB to improve retention
Gait: Extrinsic Feedback Strategies
Task Analysis: Stage of Learning —> Intermediate (Associative)
Less dependent on visual FB
Encourage pt. to self-assess motor performance & focus on the "feel of the movement"
Provide variable FB to improve retention: summary, faded, bandwidth
Reduce hands-on assistance
Continue to provide KR with successful movement outcomes
Continue to provide KP with consistent errors
Stress relevance of functional outcomes
Gait: Extrinsic Feedback Strategies
Task Analysis: Stage of Learning —> Advanced (Autonomous)
Only occasional FB required
Focus on key errors