Pharma 1A: Cell Biology, Drug Targets (G Proteins) and Drug-Receptor Interactions
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
Which G protein targets adenylyl cyclase (AC)?
Gs
What is the signaling cascade for Gs?
Activation of AC, leading to increased cAMP production and PKA activation
Example receptor for Gs?
Beta 1 adrenoceptor
Example cellular effect of Gs?
Increase in force of heart contraction
Which G protein targets phospholipase C (PLC)?
Gq
What is the signaling cascade for Gq?
Activation of PLC, leading to production of IP3 and DAG. DAG activates protein kinase C. IP3 causes calcium release from intracellular stores
Example receptor for Gq?
Alpha 1 adrenergic receptors
Example cellular effect of Gq?
Contraction of vascular smooth muscle
Which G protein (alpha subunit) inhibits adenylyl cyclase?
Gi
What is the signaling cascade for Gi (alpha subunit)?
Inhibition of AC, decrease in cAMP production, and PKA activity.
Example receptor for Gi (alpha subunit)?
Muscarinic acetylcholine receptors
Example cellular effect of Gi (alpha subunit)?
Oppose actions of beta 1 adrenoceptor, decrease in force of heart muscle contraction
Which G protein (beta gamma subunit) targets adenylyl cyclase?
Gi (beta gamma subunit)
What is the signaling cascade for Gi (beta gamma subunit)?
Targets potassium channels, causing opening and resulting in muscle relaxation
Example receptor for Gi (beta gamma subunit)?
Acetylcholine receptor
Example cellular effect of Gi (beta gamma subunit)?
Slow down heart rate
Describe the drug target and mechanism of action of digoxin
Digoxin treats heart failure. it targets the K/Na pump. Digoxin binds to the extracellular part of the pump, inhibiting it. This means Na cannot leave thus Ca2+ levels rise in the cell, causing heart contraction to happen with more force.
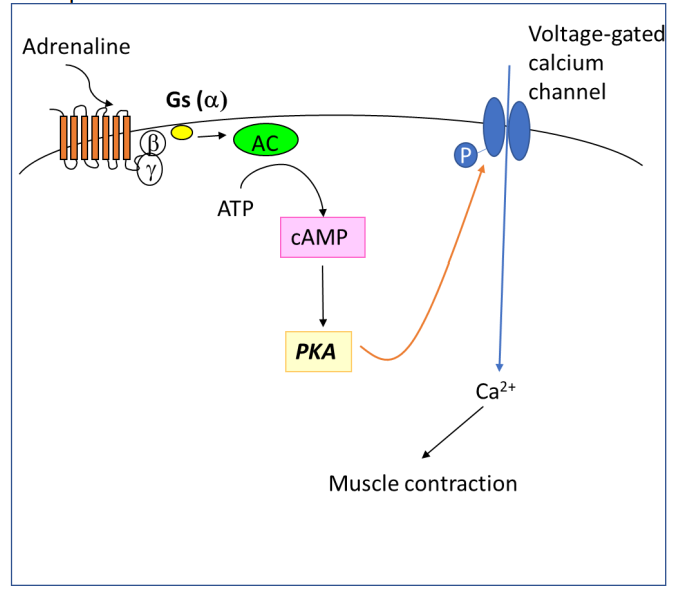
Draw a diagram to illustrate the signal transduction pathway for the beta1- adrenoceptor in the heart. Include the receptor, G protein subunits, transduction mechanism and intracellular cascade that leads to a change in cardiac muscle contraction.
Adrenaline activates the beta 1 GPCR. This causes a conformational change in the receptor. GTP replaces GDP bound to the G protein. This causes the alpha subunit of the Gs G protein to split from the beta-gamma subunit of the G protein. The alpha subunit activates adenylyl cyclase, which converts ATP to cAMP. cAMP activates protein kinase A, which phosphorylates voltage-gated calcium channels in the cell membrane. The influx of calcium is increased, which leads to stronger muscle contraction
name the 4 main types of receptors
ligand gated ion channels
g protein coupled receptors
kinase linked receptors
nuclear receptors
name and briefly describe the 3 methods of chemical signalling
paracrine
Signaling cells release molecules affecting nearby target cells in the same tissue
endocrine
Endocrine glands release hormones into the bloodstream.
synaptic
Between neurons or between a neuron and a target cel
in the signal transduction pathway activated by Gq-protein coupled receptors, what are the names of the first and second effectors and first and second messengers?
First Effector: Phospholipase C (PLC)
Second Effector: Protein Kinase C (PKC)
First Messenger: Ligand binding to Gq-coupled receptor
Second Messengers:
Inositol Trisphosphate (IP3)
Diacylglycerol (DAG)
Some clinically approved anti-cancer agents target kinases. Explain what kinases are and why they are targeted in certain cancers.
kinases - enzymes that catalyse the transfer of phosphate groups from ATP to specific target molecules.
Kinases are targeted in certain cancers because
Mutated or overactive kinases can contribute to uncontrolled cell growth and survival
Some kinases function as oncogenes when mutated or overexpressed
Aspirin can be used as an anti-thrombotic drug without having a systemic effect on other tissues. Explain the underlying mechanism
Aspirin binds irreversibly and thus inhibits COX. COX converts acid to prostaglandins and thromboxanes. Prostaglandins - inflammation. Thromboxanes - blood clotting. Specific activtiy because thromboxanes only involved in platelets and more prostaglandins can be produced by body if needed.
Explain the 8 steps of how glucose stimulates insulin secretion from β cells in the pancreas. Which ion channel is targeting by sulfonylurea’s? How does this help patients with diabetes?
Step 1: Glucose enters β cells via GLUT2 transporters.
Step 2: Glucose undergoes glycolysis, producing ATP.
Step 3: Elevated ATP levels lead to the closure of KATP channels.
Step 4: Membrane depolarization occurs.
Step 5: VGCCs open due to membrane depolarization.
Step 6: Calcium influx into the β cell.
Step 7: Increased intracellular calcium stimulates insulin exocytosis.
Step 8: Insulin is released into the bloodstream.
Sulfonylureas target ATP-sensitive potassium (KATP) channels on β cell membranes. By targeting KATP channels, sulfonylureas enhance insulin release from β cells, aiding in glucose regulation.
What is the primary function of enzymes?
Enzymes catalyze biochemical reactions. Examples of enzyme drug targets include proteases, kinases, and polymerases.
What is the primary function of enzyme-linked receptors?
Enzyme-linked receptors transduce extracellular signals by activating intracellular enzymatic activity. Examples include receptor tyrosine kinases (RTKs)
Where are nuclear receptors primarily located within the cell?
Nuclear receptors are located in the cell nucleus. They bind to ligands, such as hormones, and regulate gene expression, influencing various cellular processes.
What is the role of voltage-sensitive ion channels in action potential propagation?
Voltage-sensitive ion channels open or close in response to changes in membrane potential, allowing the rapid flow of ions, contributing to the propagation of the action potential.
What is the general role of Ca2+ in signal transduction?
Ca2+ serves as a second messenger, regulating diverse cellular processes by modulating enzyme activity, protein conformation, and vesicle fusion.
What is the primary function of ligand-gated ion channels?
Ligand-gated ion channels open or close in response to ligand binding, regulating ion flow. An example of a drug target in this group is the nicotinic acetylcholine receptor
define “competitive” drug antagonism
binds at the agonist recognition site preventing access of normal ligand
define “non-competitive” drug antagonism
does not bind at the agonist site but inhibits agonist binding in
another way
define “uncompetitive” drug antagonism
this is when binding occurs to an activated form of the receptor (i.e. “use-dependent”).
define “physiological” drug antagonism
when the effect of a neurotransmitter or hormone is countered by the action of another neurotransmitter or hormone
true or false: antagonism can be reversible OR irreversible
true
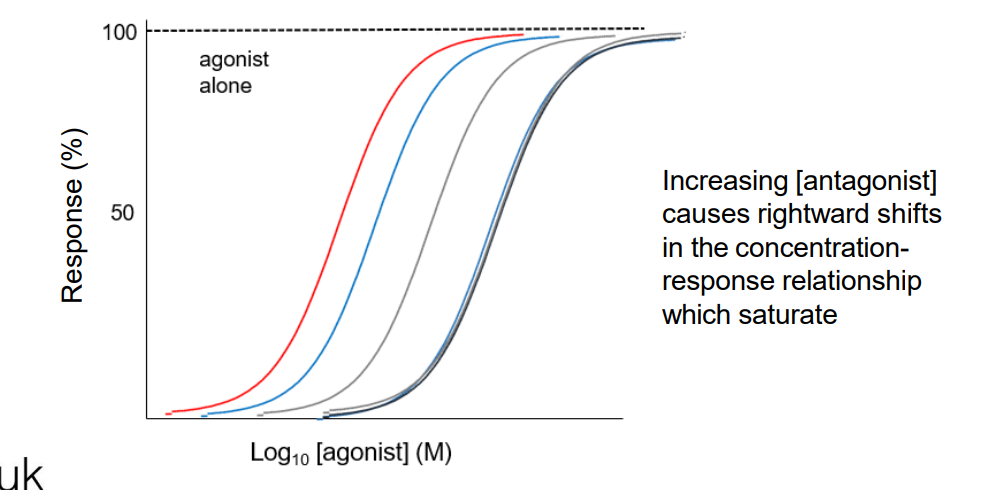
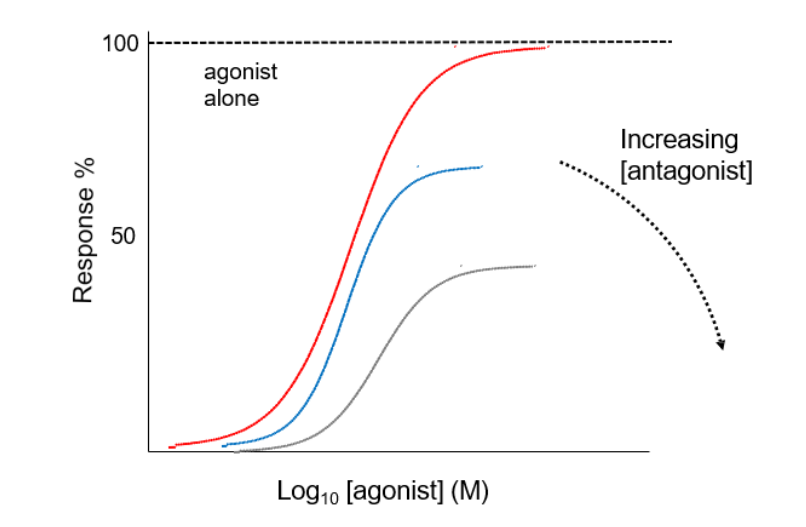
What are the two effects an antagonist can have on the concentration-response curve to an agonist?
depression of the maximal response
RIGHTWARD displacement of the curve.
What is depression of maximal response?
when an antagonist partially or fully prevents the agonist from eliciting its full response.
when does depression of maximal effect occur?
when the antagonist binds irreversibly or competes with the agonist for binding
what does rightward displacement of the curve suggest (in a conc-response curve of an agonist where an antagonist is present)?
a decrease in the potency of the agonist in the presence of the antagonist
how does the antagonist affect the agonist's binding?
makes it more difficult for the agonist to bind or activate the receptor
what happens to the concentration response curve in rightward displacement?
it requires higher concentrations of the agonist for the same effect
What is the therapeutic index of a drug? Define the numerator and denominator. What is it a measure of?
The therapeutic index: the ratio of the dose that produces therapeutic effects to the dose that produces toxic effects.
LD50/ED50
LD50 - the median lethal dose
ED50 - median effective dose
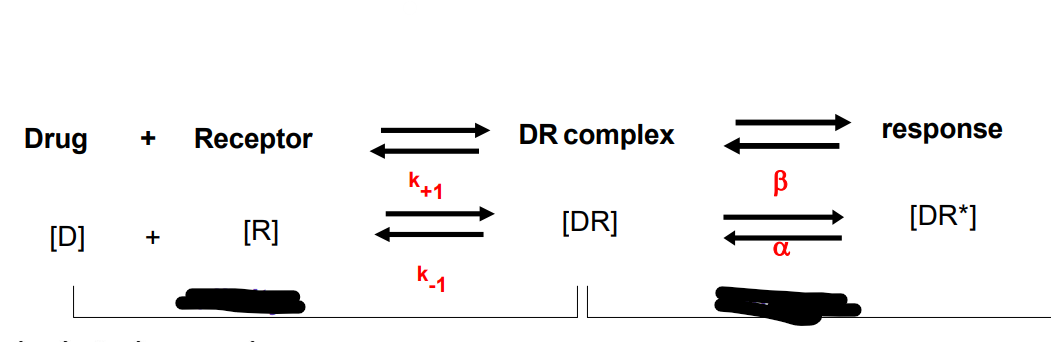
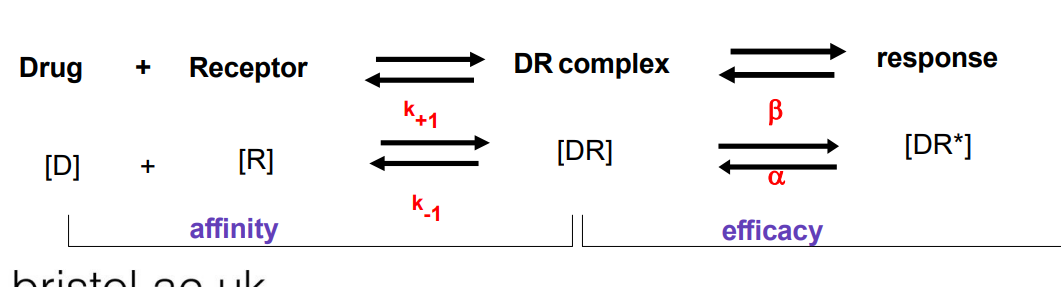
What information does the KD provide?
KD is a measure of the affinity of binding of the drug to the receptor
KD = [drug] that binds to 50% of the available receptor
In terms of ligand-receptor binding, what is the significance of a low Kd?
A low Kd signifies that the ligand binds tightly to the receptor, requiring lower concentrations for effective binding.
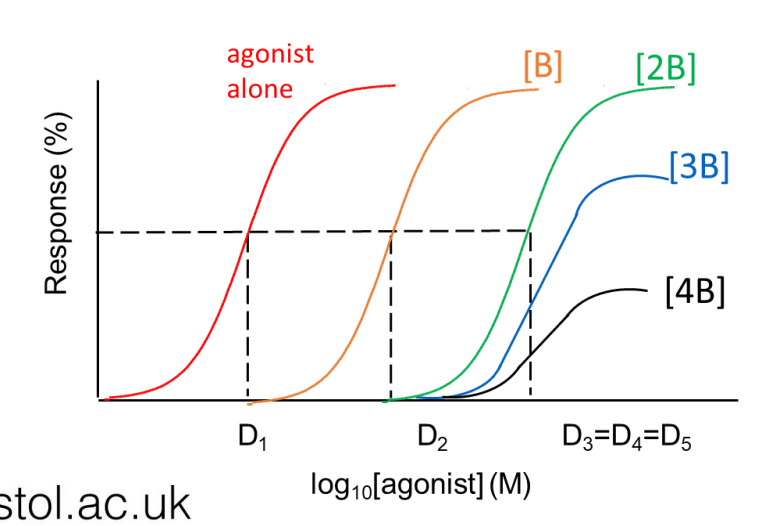
![<p>identify which curve is for the i) agonist only ii) agonist + [B] iii) agonist + [2B] iv) agonist + [3B] where B is antagonist</p>](https://knowt-user-attachments.s3.amazonaws.com/28b84578-e190-4ada-b554-0e7606796798.jpeg)
identify which curve is for the i) agonist only ii) agonist + [B] iii) agonist + [2B] iv) agonist + [3B] where B is antagonist
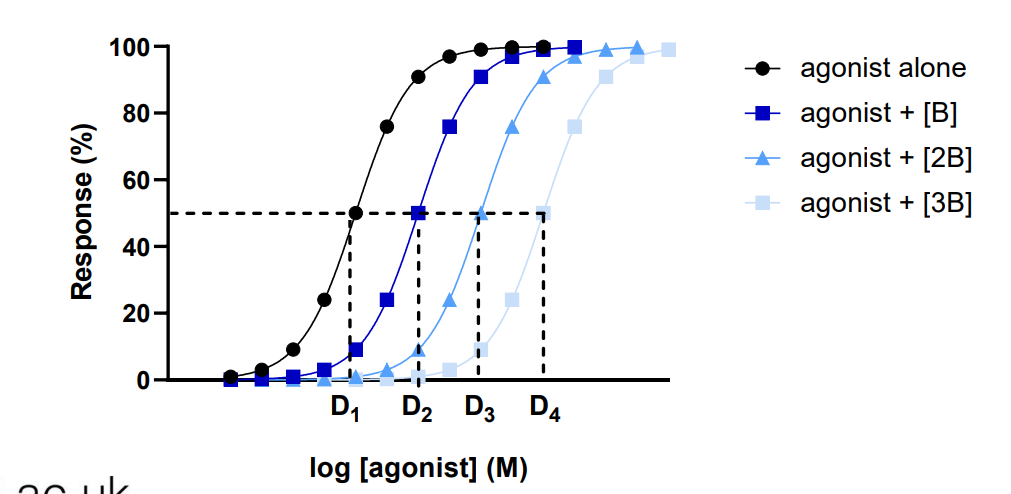
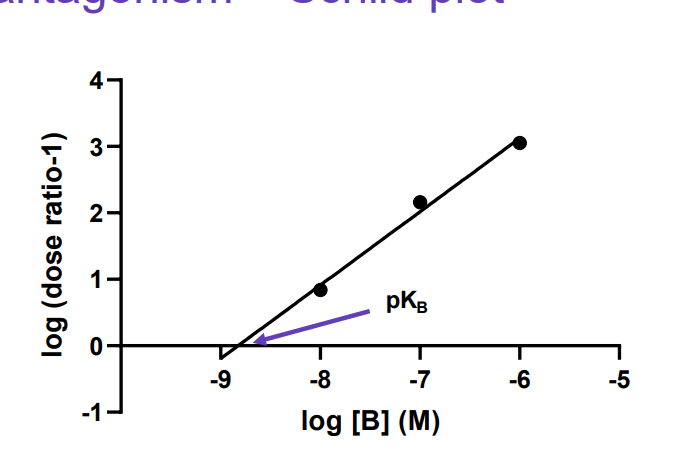
What does a Schild plot for KB look like (ie what are the x and y axes) and how can we i) identify if the antagonist is competitive ii) calculate KB?
i)If the slope is equal to 1 then the antagonist is considered competitive. ii) If the slope is equal to 1, the intercept with the x-axis gives the –log KB