Deprescribing, Frailty + Bone Health
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
What are the consequences of problematic polypharmacy? + The solutions to problematic polypharmacy?
Consequences
→ Increased cost, pill burden and medicines waste
→ Leads to prescribing cascade
→ Hospitalisations
→ Increased frailty, falls and mortality
→ Increased clinical workload
Solutions: aim to reduce ADRs, increase appropriateness, reduced falls, improve adherence, maintain quality of life, reducing readmissions, cost benefits
What are the interventions to polypharmacy?
Medication reviews, clinical decision support tools, checklists,
audit, feedback, patient education & training
→ Deprescribing tools – ACB, Opioid deprescribing,
Medicines overuse in dementia and people living with learning disabilities, Medichec, STOPP/START tool, STOPPFrail tool, ThinkCascades tool, PrescQIPP
Approach – should be person-centred
Anticholinergic burden
Adverse Drug Reactions (ADRs) associated with anticholinergics:
- Dry eyes, urinary retention, dizziness, cognitive impairment, and falls
- Anticholinergic effects intensify with stronger medications or combinations
- Older patients, due to multiple medications and age-related changes, are more susceptible to ADRs
Anticholinergic Burden Scales:
- Created to quantify the effects of anticholinergic medications
- Over 22 different published scales, with the Anticholinergic Cognitive
Burden Scale (ACB) and the German Anticholinergic Burden Scale (GABS) being chosen for reliability https://www.acbcalc.com/
- Designed as practical tools for optimising prescribing, especially in older patients
Association with cognitive impairment and dementia:
- Longitudinal studies show a link between anticholinergic use and the risk of developing cognitive impairment + death
- Dose-dependent association found between long-term anticholinergic use and dementia risk
Anticholinergic Burden Calculator:
- Designed to aid clinicians during medication review
- Offers alternatives with lower anticholinergic burden, considering patient suitability
- Emphasizes the importance of continuing medications with robust clinical evidence
Evidence-based decision-making with anticholinergics:
- Acknowledges that many medications with anticholinergic properties are prescribed based on strong clinical evidence.
- The Anticholinergic Burden Calculator supports clinicians in decision-making during medication reviews, considering both evidence-based prescriptions and alternatives with a lower burden.
Addressing the consequences of polypharmacy
Person-centred deprescribing
1. Assess the patient
2. Agree goals
3. Identify potentially inappropriate medicines
4. Assess risks and benefits
5. Agree actions
6. Communicate with others
7. Monitor, review and adjust regularly
![<p><span><mark data-color="purple" style="background-color: purple; color: inherit">Frailty</mark></span></p><p class="MsoNormal"><span>Frailty – gradual decreased physiological reserve with increased vulnerability to stressors, a multisystem decline</span></p><p class="MsoListParagraphCxSpFirst">-<span> 10% of >65’s and 25-50% of >85’s</span></p><p class="MsoListParagraphCxSpMiddle">-<span> Linked with multimorbidity, LTCs [75% of >75s have more than one LTC], 20-50% of older people with CVD are frail</span></p><p class="MsoListParagraphCxSpMiddle">-<span> Phenotype model – patient characteristics which predict poorer outcomes (unintended weight loss, reduced grip or muscle strength/gait speed, self-reported exhaustion, trouble with DAL)</span></p><p class="MsoListParagraphCxSpMiddle">-<span> Cumulative Deficit Model – accumulation of deficits that increase frailty index (hearing loss, low mood, tremor, disease such as dementia)</span></p><p class="MsoListParagraphCxSpLast">-<span> Frailty increases with comorbidities</span></p>](https://knowt-user-attachments.s3.amazonaws.com/2b806bf2-da61-46a1-a0a1-2417d082218e.png)
Frailty
Frailty – gradual decreased physiological reserve with increased vulnerability to stressors, a multisystem decline
- 10% of >65’s and 25-50% of >85’s
- Linked with multimorbidity, LTCs [75% of >75s have more than one LTC], 20-50% of older people with CVD are frail
- Phenotype model – patient characteristics which predict poorer outcomes (unintended weight loss, reduced grip or muscle strength/gait speed, self-reported exhaustion, trouble with DAL)
- Cumulative Deficit Model – accumulation of deficits that increase frailty index (hearing loss, low mood, tremor, disease such as dementia)
- Frailty increases with comorbidities
G8 Screening Tool (geriatric screening tool) - What is it + what are the criteria?
Neuropsychological conditions are disorders that affect brain function, leading to impairments in areas like cognition, behavior, and emotions. Examples include Alzheimer's disease, Parkinson's disease, stroke, epilepsy, and various neuropsychiatric disorders like depression and schizophrenia.
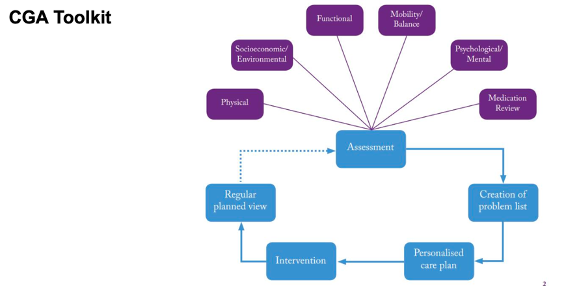
CGA (comprehensive geriatric assessment)
Age = <80 = 2 points, 80-85 = 1 point
Identifies older cancer patients needing CGA
1. Age
2.Declining food intake?
3.Recent weight loss?
4.Mobility level
5.Neuropsychological conditions?
6.BMI
7.>3 prescription drugs daily
8.Self-rated health status
What are the common bone conditons?
Osteoporosis
Characterised by low bone density and structural deterioration.
Often undiagnosed until a fragility fracture occurs.
Key sites: Hip, vertebrae, distal radius.
Osteomalacia
Often due to vitamin D deficiency; presents with bone pain and muscle weakness.
Paget’s Disease (less common but relevant in some populations)
What is the bone health like in elderly pts?
Aging - decreased bone mass, increased + structural deterioration of bone tissue, increased fragility fracture risk
Decreased bone formation + increased resorption, trabecular thinning and loss of connectivity,
→ Reduced osteoblast activity and hormonal changes (e.g., ↓ oestrogen (reduce osteoblast activity), ↓ testosterone, ↓ IGF-1 (growth factor - reduction in growth hormone with age = reduction is new bone generation) + cannot absorb Ca + Vit D well with increasing age .
Fractures; significant morbidity, loss of independence, mortality.
Sarcopenia + frailty: Muscle weakness further increases fall risk and fracture likelihood
What are the risk factors for poor bone health in the elderly?
Non-modifiable:
→ Age, female sex, menopause, family history, white or Asian
ethnicity, previous fragility fracture, rheumatological conditions, parent with hip fracture
Modifiable:
Vitamin D deficiency
Inadequate calcium intake
Sedentary lifestyle
Smoking and alcohol use - thins the bones
Polypharmacy (i.e. corticosteroids, anticonvulsants, SSRIs)
Falls
Low BMI <18.5 - associated with frailty, falls, reduced bone mass
What is the link between Bone health + Cancer?
Cancer + cancer treatments significantly increase the risk of bone loss and skeletal complications.
Bone; third most common site for metastases (after lung & liver).
Bone fragility can lead to pain, fractures, immobility, + reduced QoL.
Cancers commonly affecting the bone include
Breast, prostate, lung, renal, multiple myeloma as well as
Primary bone cancers which are less common
What are the mechanisms of bone involvement in cancer?
Bone Metastasis
Osteolytic or Osteoblastic lesions: Cancer cells disrupt the balance of osteoclast and osteoblast activity via signalling pathways
Treatment-Related Bone Loss
Hormonal therapies
Chemotherapy
→ Direct toxic effects on bone remodelling
→ Induced premature menopause or hypogonadism
Steroids: Glucocorticoid-induced osteoporosis (e.g., in lymphoma or multiple myeloma)
Falls - What are the risk factors + risk assessments (main 2)?
Risk assessment tools
- Timed Up and Go (TUG)
- Berg Balance Scale
- Morse Fall Scale
- Frailty Assessment Tools:
- Clinical Frailty Scale (CFS)
- FRAIL questionnaire
- Edmonton Frail Scale
Risk factors - Muscle weakness, poor balance or gait disorders, cognitive impairment, polypharmacy, vision impairment, urinary incontinence, environmental hazards (poor lighting), inappropriate footwear, assistive device misuse
Risk assessment tools - Frax + QFracture
Who should be assessed for fragility fractures?
All women > 65 years, + all men > 75 years.
All women aged < 65 years and all men aged < 75 years with
→ A previous osteoporotic fragility fracture.
→ Current use or frequent recent use of oral corticosteroids.
→ History of falls.
→ Family history of hip fracture.
→ Low body mass index (less than 18.5 kg/m2).
→ Smoking.
→ Alcohol intake of more than 14 units per week.
→ A secondary cause of osteoporosis
Fragility fracture risk → What is used to assess?
FRAX or Qfracture (preferred) AND clinical judgement
Absolute risk of hip and major osteoporotic fractures (spine, wrist, shoulder) over 10 years
FRAX assigns green, amber or red zone score for fracture, but underestimates some risk factors (high alcohol, heavy smoking, regular corticosteroid use)
→ red zone = need prevention strategies in place
Qfracture – 10% threshold = A score of over 10% means high risk of fragility fractures and a DXA scan should be conducted
What is used for diagnosis + screening?
Bone Mineral Density (BMD) via DXA scan:
- T-score ≤ -2.5 = Osteoporosis
- Screening recommended in:
· All women ≥65 and men ≥70
· Younger individuals with risk factors (e.g., previous fracture, steroids)
FRAX tool: 10-year probability of fracture with or without BMD.
Consider:
- Vitamin D levels, Serum calcium and phosphate, PTH, TSH, renal function, markers of bone turnover in complex
- cases
Baseline and periodic BMD testing (DXA scans) for:
- All patients on aromatase inhibitors or androgen deprivation therapy
- Long-term corticosteroid use
- Metastatic bone disease
Laboratory tests:
- Serum calcium, phosphate, vitamin D, PTH, ALP (especially if elevated in bone metastasis)
Imaging:
- Bone scans, PET-CT, MRI for bone metastases
What are the fall prevention strategies?
Exercise
→ Weight-bearing (walking, dancing), resistance/strength training, balance and flexibility exercises (Tai Chi, yoga)
Lifestyle - Smoking cessation, Alcohol moderation, Home safety interventions, Medication review (de-prescribing high-risk drugs), Vision correction, Footwear and orthotics, Nutrition
Calcium and Vit D
→ Calcium: at least 1g daily with Vitamin D: 400–1,000 IU/day (higher if deficient)
→ Adequate protein intake, caution in CKD2-3B, avoid in CKD4-5
Frailty Management:
G8/Comprehensive Geriatric Assessment (CGA), Multidisciplinary interventions, Nutrition optimisation (especially protein + Vitamin D), Resistance + aerobic exercise, Social support + caregiver involvement
What are the treatment options for poor bone health?
1st line - Bisphosphonates (alendronate, risedronate, zoledronic acid), inhibitors of bone resorption
Alternatives:
→ Denosumab (especially in renal impairment)
→ Teriparatide or abaloparatide (anabolic agents), Romosozumab (dual action; newer specialist option)
→ Hormone replacement therapy (select postmenopausal women; assess risk-benefit) ie SERMs in postmenopausal women = maintains bone density + reduce fracture risk
Consequences of Falls, Fractures + Frailty → What are the impacts? + Monitoring and Follow-up
Fracture Management and Post-Fracture Care
Hip fracture mortality: ~20% at 1 year.
- Immediate orthopaedic and geriatric co-management improves outcomes. Post-fracture osteoporosis treatment should begin during hospitalization or shortly after.
Physical injuries: fractures, head trauma
Psychological: fear of falling, depression, loss of confidence
Functional decline
Increased institutionalisation and healthcare costs
Higher mortality
Monitor + Follow-up
Tolerance to treatment after 12-16 weeks (ADRs such as upper GI effects)
Check adherence after 12 weeks
Reassess need for continued bisphosphonate after 5 years
Maintain good oral hygiene
Attend routine dental check-ups & inform dentist of treatment
Report sigs/symptoms of osteonecrosis of the jaw
Suggest non-pharmacological and pharmacological interventions to monitor AH’s mood/wellbeing (Hx of depression + Anxiety).
What monitoring and follow up could be put in place for AH’s mental health?
Non-pharmacological – CBT with written materials or face-to-face therapy if needed, friends and family support
Activity/exercise, counselling, social or peer support, school-specific support, mindfulness, creative therapy, regular routine, structure, good sleep hygiene and family involvement.
Family group therapy for parental and sibling support such as videos from Cancer Research UK.
Signpost to the teenage Cancer Trust, Headspace for Teens, courses to support self-care.
Pharmacological – SSRIs, SNRIs, TCAs, anxiolytics
Monitoring + Follow-up
Initial Baseline Assessment: Monitor mood at diagnosis or during early treatment. Increased risk of relapse or exacerbation of mental health due to past history. Routine Monitoring: Every 2 to 4 weeks during active treatment.
Follow-Up: Continue at monthly or bi-monthly intervals post-treatment or during survivorship care.
SSRIs are most commonly prescribed for anxiety. Would counsel on use + monitor for efficacy from 4-6 weeks.
Could use PHQ-9 modified for adolescents score – PHQ9-A.
Self-monitoring for signs of low mood depression or anxiety, functioning or any concerns around self-harm.
Support from family to monitor for behavioural or mood changes.
Using one example question and one example statement, explain how you would engage AH to establish rapport and build a supportive environment in your consultation
Engage AH directly while also involving his parents to build rapport.
Make efforts to gently draw him into the conversation, e.g., using his name, asking open-ended questions. Tell me how you are feeling today?
Ensure AH feels involved in decision-making by getting his input and using it to inform decision-making. I’ve heard what your parents think, but I’d also like to hear your thoughts about this?
Acknowledge the emotional strain he might be under. For example:
“I understand this has been a difficult time for you. If at any point you need a break or have questions, just let me know.”
“I’m aware that you have struggled with your mental health in the past and this must be difficult. Would you like to talk about it at this time or would you prefer to discuss that at a later point?”
Provide opportunity to AH for questions. Ensure privacy and confidentiality for the consultation. Offer to come back or speak again if he needs time.