HISTEM W2 Basic Tissues
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
What are the 3 embryological cell layers in which basic tissues develop from?
Ectoderm
Mesoderm
Endoderm
What type of epithelial tissue is derived from the ectoderm?
Skin and oral mucosa
What type of epithelial tissue is derived from endoderm?
Respiratory and digestive tract epithelium
What type of epithelial tissue is derived from mesoderm?
Urinary tract
Describe the different epithelial cell arrangements: Simple, Stratified, Pseudo stratified
Simple - single layer
Stratified - 2 or more layers
Pseudostratified - 1 layer but looks like 2
Describe the different epithelial cell shapes: Squamous, cuboidal, columnar, transitional
Squamous - flat
Cuboidal - cube
Columnar - rectangular/column shaped
Transitional - changes shape
Describe the 2 epithelial cell functions:
Keratin - dead layer, no nucleus
Ciliated - hair-like projections (propel other substances)
Describe simple squamous epithelium. Where can it be found?
Very thin, flat cells that may vary in shape.
Covers connective tissue with little ECM
Performs filtering function on moist surfaces
Endothelium - single cell lining vessels and serous cavities
Location:
Pulmonary alveoli
Inner and middle ear
Blood and lymphatic vessels
Heart
Serous cavities
Describe simple cuboidal epithelium. Where can it be found?
cube-like, nucleated cell
fx: protection/covering for organs, contributes to secretion
Location:
Lines the ducts of various glands such as salivary glands
Describe simple columnar epithelium. Where can it be found?
Rectangular shape with nucleus near the base of the cell
fx: protection, secretion/absorption due to goblet cell (secretes mucous)
May be ciliated or not
Location:
Non-ciliated → stomach, large/small intestines,
Ciliated → uterus, fallopian tubes, ductus deferens, small intra-pulmonary bronchi
Describe psuedostratified columnar epithelium. Where can it be found?
Crowded columnar cells, with nucleus at different levels
fx: moistens, warms and clean lining membranes
May be ciliated or not
Location:
upper respiratory tract including nasal cavity and para nasal sinuses
What type of epithelium is found in the upper respiratory tract, nasal cavity and paranasal sinuses?
Pseudostratified columnar epithelium
Describe non-keratinized stratified squamous epithelium. Where can it be found?
Many layers of non-keratinized cells on an irregular basal layer
Cell shape can range from cuboidal to squamous
Location:
Buccal and alveolar mucosa
Ventral part of tongue
Soft palate
Sulcular epithelium
Esophagus
Describe keratinized stratified squamous epithelium. Where can it be found?
Many layers of keratinized squamous cells
fx: keratin layer is used for protection
Create cell differentiation among its 5 layers.
Location:
skin
Free gingiva
Attached gingiva
hard palate
dorsal side of tongue
Lips
What are the 5 keratinized layers of epithelium (exists in epidermis)?
Stratum basale
Stratum spinosum
Stratum granulosum
Stratum lucidum
Stratum corneum
Describe transitional epithelium. Where can it be found?
ranges between stratified squamous,(non keratinized) and stratified columnar epithelium
Varying cell shapes: polyhedral, dome, flat
Cells are soft, pliable and loosely arranged - elastic
Location:
urinary bladder
What is the turn over time for epithelial cells?
rapid.
skin is 27 days,
oral cavity is 14 days
What are the 3 layers that make up the basement membrane?
Lamina lucida (clear layer)
Lamina densa (dense layer
Reticular lamina ( contains collagen and reticular fibres)
Basal lamina is lamina lucida +densa
Basement membrane is thin, acellular and located between epithelium and connective tissue
What are the 3 major cell types found in connective tissue? What are each of their functions?
Fibroblasts - synthesize protein fibres and intercellular substances to sustain connective tissue
Macrophages - immune cells that help fight infections that may enter the connective tissue layer
Mast cells (basophils) - involved in allergic responses
What are the 3 types of connective tissue fibers?
Collagenous fibers - composed of collagen and have great tensile stregnth
Elastic fibers - microfilaments embedded in elastin (protein) that can stretch and return to original shape
Reticular fibers - composed of reticulin (protein); very fine hair like fibers that branch and form a network in the tissue
What are the 8 main types of connective tissue?
Loose connective tissue
Fibrous connective tissue
Adipose tissue (fat)
Elastic connective tissue
Reticular connective tissue
Cartilage
Bone
Hemopoetic tissue (produce RBC)
Define Loose connective tissue and its function and location(s).
Thin membrane between organs that protects and binds them together.
Fx: Serves as protective padding for deeper structures
Location: beneath skin (dermis layer) and between muscles
Describe Fibrous connective tissue and its function and location(s).
aka Dense connective tissue
composed of strong collagenous fibers
fx: provide support
Location:
tendons, ligaments, eyes, skin (dermis layer)
Describe Adipose tissue and its function and location(s).
Specialized type of loose connetive tissue that stores fat
fx: protective cushion and heat insulation
Location:
Hypodermis
Certain abdominal membranes
Oral cavity
Around kidneys, heart and various joints
Describe Elastic connective tissue and its function and location(s).
Tissue composed mainly of elastic fibers that give tissue strength and elasticity.
fx: allows tissue to stretch
Location:
vocal cords
certain hollow internal organs
Describe Reticular connective tissue and its function and location(s).
Network of interwoven reticular fibers forming a supportive framework
fx+location: supports walls of blood vessels, internal organs (liver, spleen, lymphatic organs)
Describe Cartilage tissue and its function and location(s).
Intercellular material that is composed of collagen and intercellular substance. It lacks direct blood supply.
fx: provides support and decreases friction (i.e cartilage in joints)
Location:
ends of bones in joints, in the rib cage, nose, ears, and airways
What is perichondrium?
Fibrous connective tissue sheath containing blood supply that surrounds most cartilage
What are the 2 types of cells found in cartilage?
Chondroblasts - produces cartilage matrix, lies internal to the perichondrium
Chondrocytes - mature chondroblasts that maintain the cartilage matrix
What are the small spaces surrounding chondrocytes in the cartilage matrix?
Lacuna → mature chondrocytes are located IN lacuna
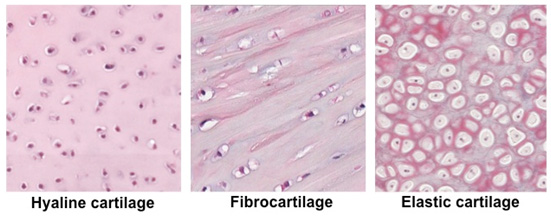
What are the 3 major types of cartilage?
Hyaline
Elastic
Fibrocatilage
Describe Hyaline cartilage
Most common type of cartilage in the body
glassy, translucent appearance
All cartilage starts as hyaline cartilage
fx: provides a smooth, low-friction surface for joint movement, supports respiratory passages, and plays a role in bone growth
Location: embryonic skeleton, growth centers, mandibular condyle
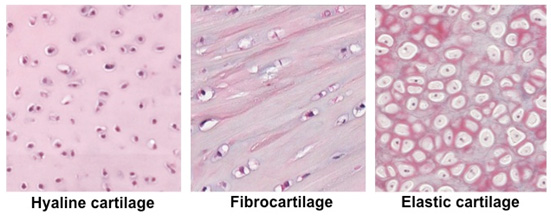
Describe Elastic cartilage
a flexible connective tissue characterized by its high content of elastic fibers and collagen fibers. Exceptional elasticity and resilience.
fx: provides flexibility, structural support in areas that its located
Location:
external ear, auditory tube, epiglottis, parts of the larynx
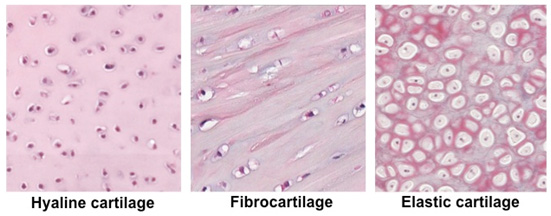
Describe Fibrocartilage
Composed of a mixture of dense collagen fibers and cartilaginous tissue (hyaline).
→ always found near hyaline cartilage and will gradually merge into it.
→ Cells are enclosed in capsules of matrix giving it great tensile strength
fx: serves as shock absorber and protective cushion
Location: intervertebral discs, between bones in pelvic girdle, and TMJ
Describe bone tissue
Highly vascularized, rigid connective tissue that makes up most of the mature skeleton.
matrix contains mineral salts and collagen
fx:
provides internal support for body structures, and protects vital organs,
serves as attachment site for muscles
manufactures RBC in red bone marrow
stores calcium and other minerals
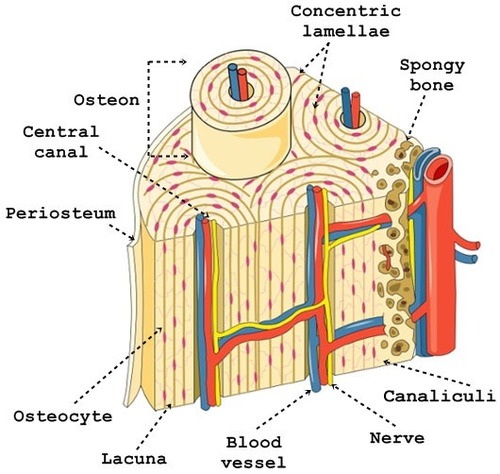
How are the cells of bone arranged?
Concentric circles around osteonic canals
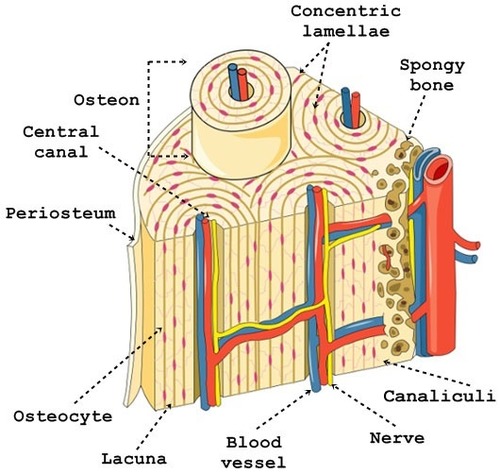
What are canaliculi? Why are they important for bone?
Canaliculi connect concentric circles (lamellae) to the osteonic cancls which allows interaction between osteocytes (mature osteoblasts).
crucial for nutrient transport, waste removal, and communication between osteocytes, facilitating bone's ability to adapt to mechanical stress
What are osteogenic cells? Where are they located?
Stem cells that will differentiate into osteoblasts.
Located on the inner layer of periosteum.
What are osteoblasts?
Produces protein components of bone matrix that are required to build bone.
What are osteocytes?
Mature osteoblasts trapped in the bone matrix within the lacunae. They maintain the bone matrix.
What are osteoclasts?
Bone-resorbing cells located in Howship’s lacunae (shallow pits caused by resorption).
dissolve and break down old or damaged bone cells
make space for osteoblasts to create new bone tissue in areas that are growing or need repair
Define osteon
The unit structure in compact bone that consists of 5-20 lamellae (layers).
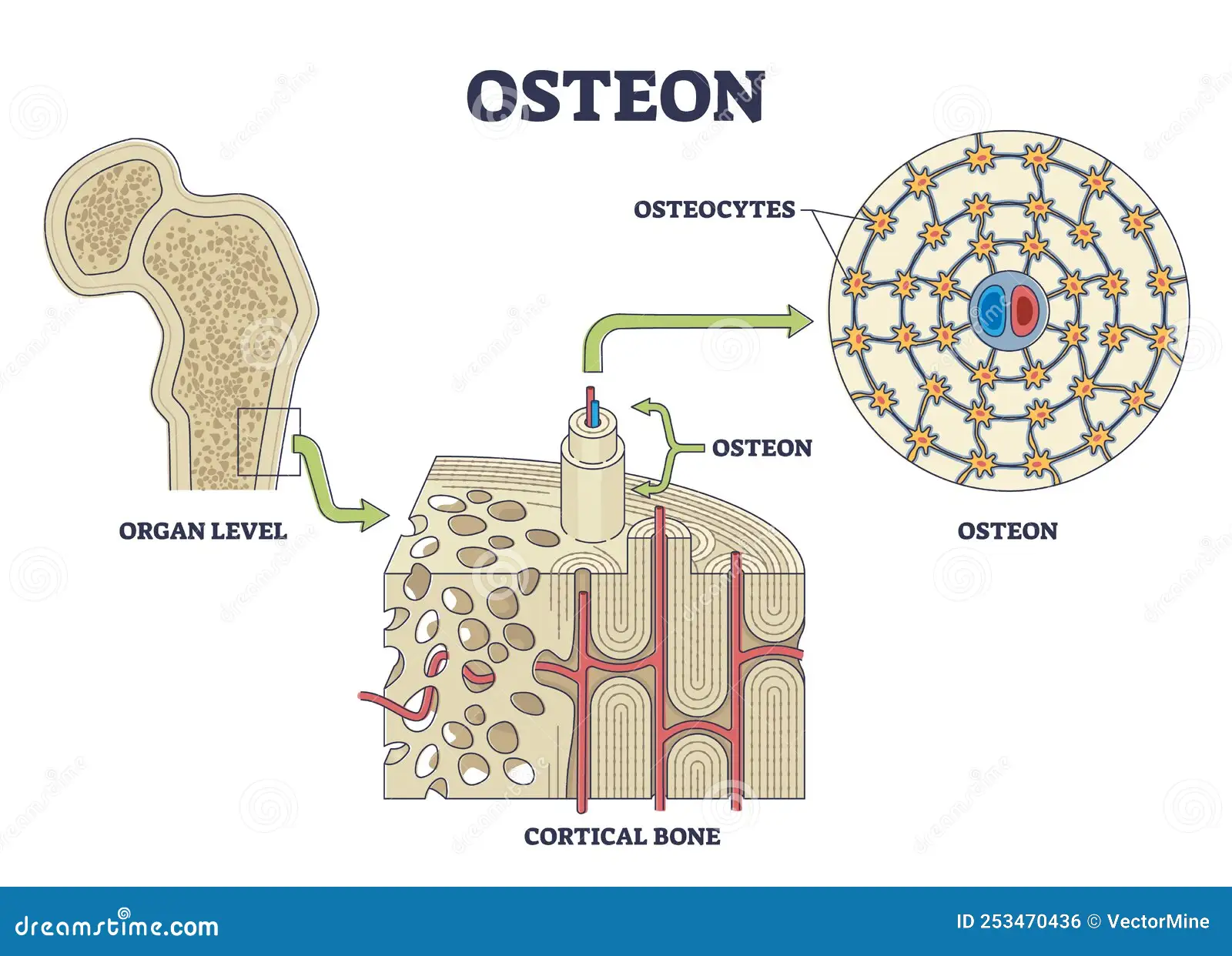
Define Haversian canal
Central vascular canal that runs longitudinally within the osteon surrounded by the lamellae.
contains nerves and blood vessels
provides nutrients for bone tissue
Define Volkmann’s canal
Similar to the Haversian canal, but it runs obliquely or at right angles from the Haversian canal.
branches from the Haversian canal to provide innervation to more superficial bone tissue
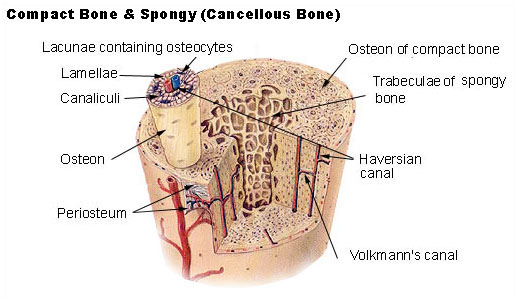
What are lamellae?
Organized arrangements of concentric sheets (like growth rings of a tree)
Describe the Periosteum
Double layered dense connective tissue sheath.
Outer layer contains blood vessels and nerves
Inner layer contains osteoblasts
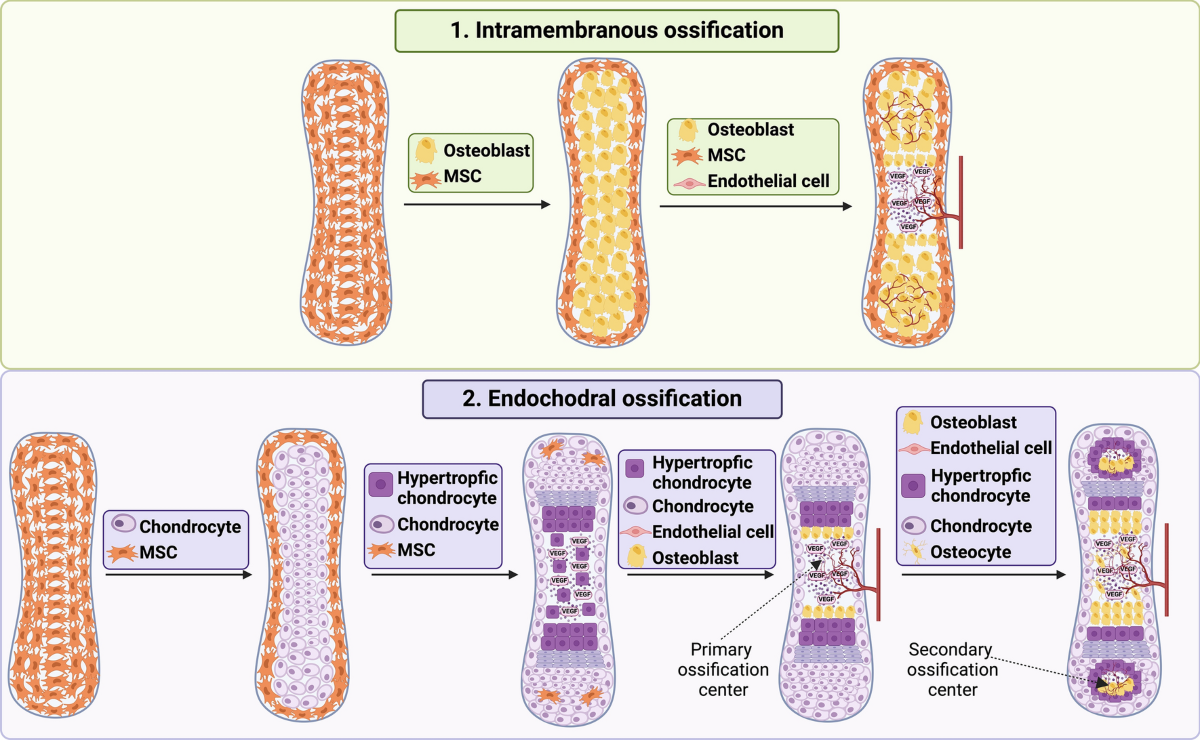
What are the 2 methods of Ossification (bone development)
Intramembranous
Endochondrial
Describe Intramembranous ossification. Where does it occur?
Formation of steoid (young bone) within 2 dense connective tissue sheets (intramembraneous) which eventually replaces the outer connective tissue (appositional growth)
Location:
fontanelles (soft infant skull spots)
maxilla
majority of the mandible
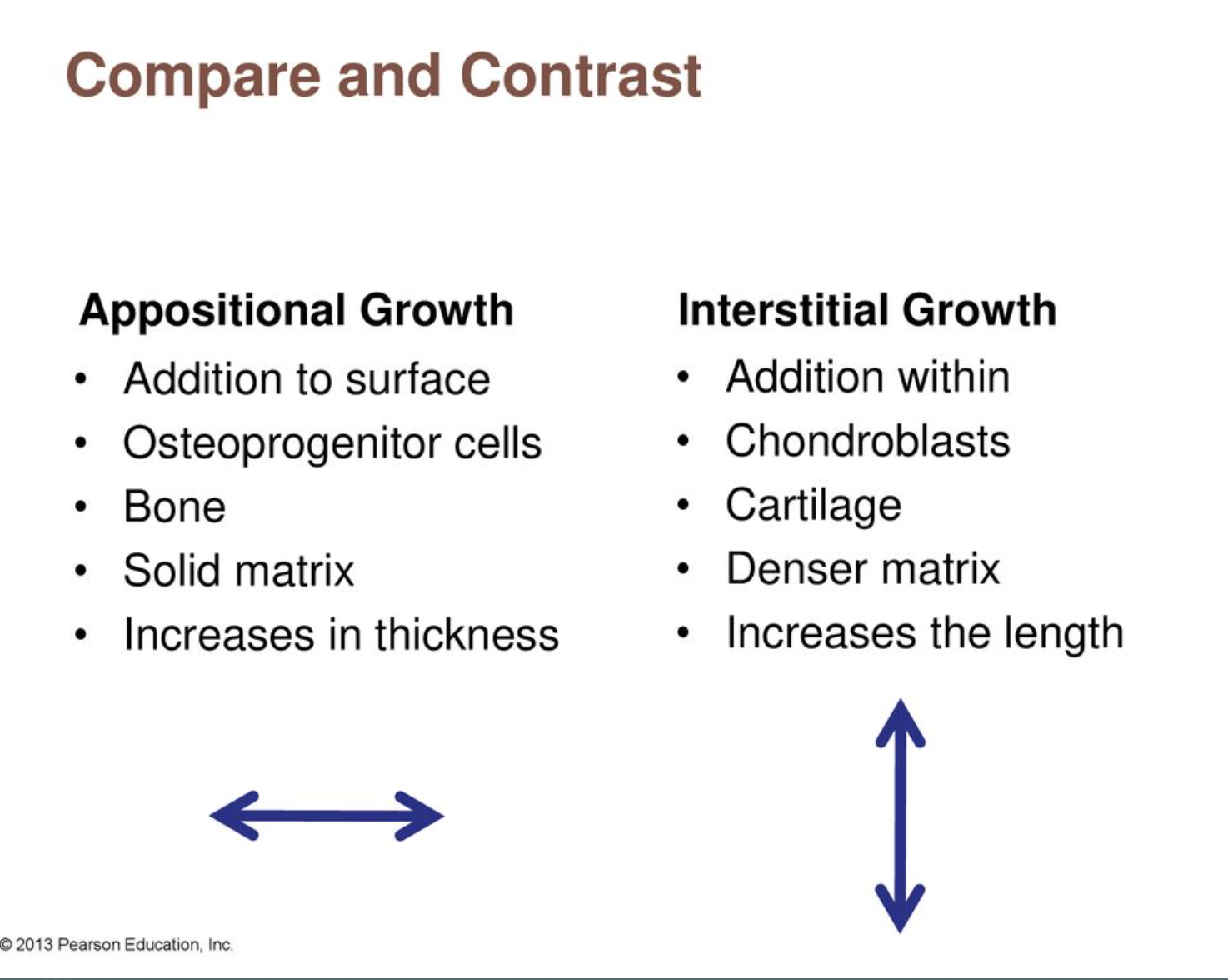
Define appositional growth
Appositional growth refers to the increase in the diameter of bones by the addition of new bone tissue on the surface of existing bone
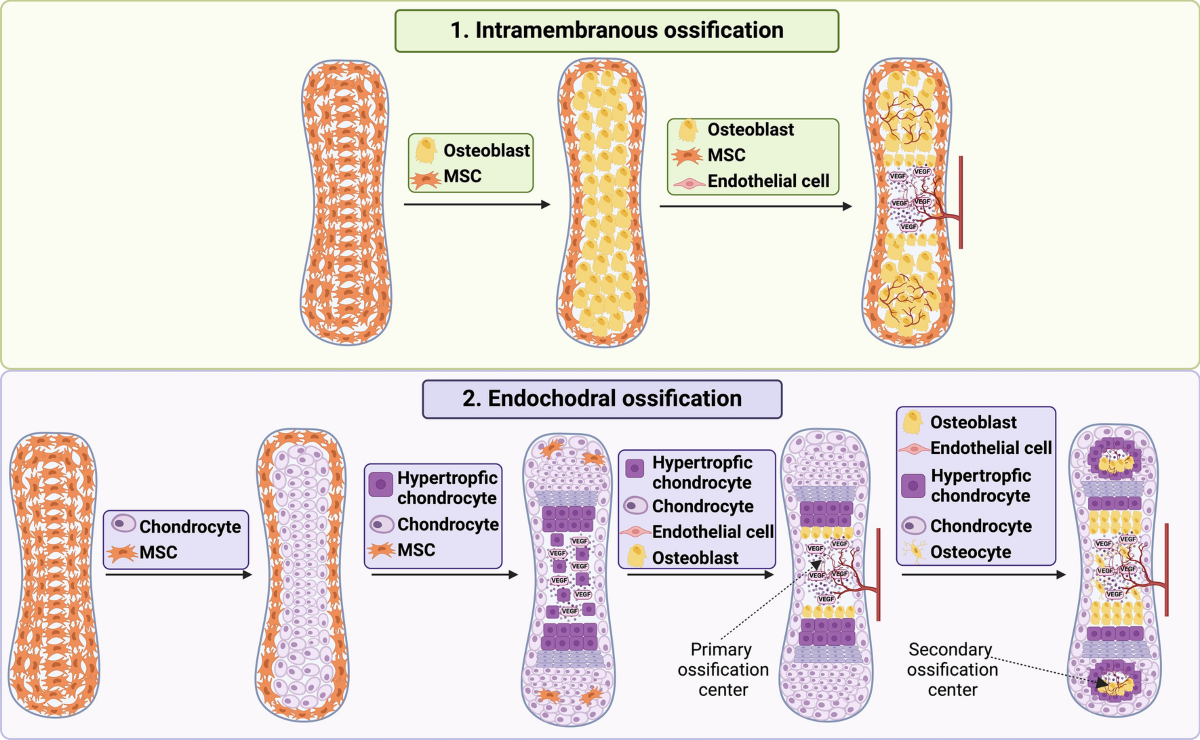
Describe Endochondrial ossification
Formation of osteoid (young bone) within a hyaline cartilage model.
Location: Occurs in long bones, vertebrae, ribs, head of mandible, base of skull
Define interstitial growth
Interstitial growth ossification refers to the process of bone lengthening through cartilage growth and subsequent replacement by bone tissue.
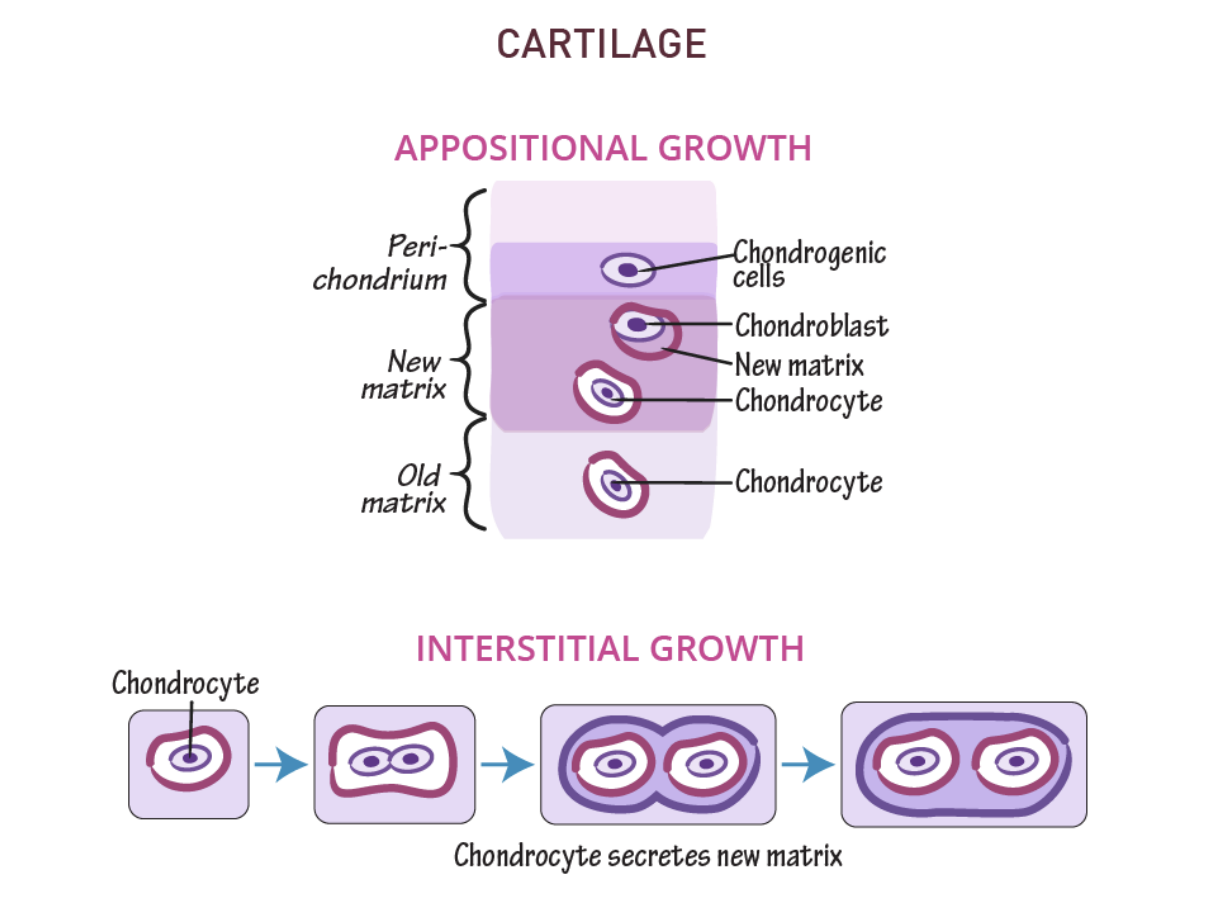
Compare and contrast Interstitial growth and Appositional growth
Compare and contrast immature and mature bone tissue.
Immature:
First bone produced by either methods of ossification
Indistinct lamellae
Irregular arrangement of collagen fibers
Many cells present
Mature:
Replaces primary bone
Distinct lamellae
Very organized arrangement of collagen fibers
Fewer cells
Describe Hemopoetic tissue
Tissue responsible for producing blood cells. It primarily resides in the bone marrow ( also includes the spleen, liver, and lymph nodes)
This tissue contains HEMATOPOETIC STEM CELLS, which differentiate into various types of blood cells, including red blood cells, white blood cells, and platelets.
*does not contain fibers
What are thrombocytes?
platelets in blood (clotting factor)
smaller than RBC
no nucleus
disc shaped
What are the 6 types of white blood cells (leukocytes)?
Neutrophil - destroys foreign particles by phagocytosis, first to arrive at site of injury
Eosinophil - kills bact and helps control inflammation and allergic reactions
Basophil - controls inflammation and allergic reactions
Monocytes - contains lysosomal enzymes for destroying pathogenic particles. later stages of inflammatkion
Lymphocytes - Mechanism of immunity, chronic. (B cells, T cells and NK cells)
Mast cells - allergic response, contains heparin and histamine
What are the 3 types of Muscle tissue?
Skeletal
Smooth
Cardiac
Order muscle tissue from thinnest to thickest.
Myofilament → myofibril → myofiber → Musle fascicle → Muscle
Describe Skeletal muscle and its identifying characteristic(s).
Voluntary muscle meaning that it requires conscious effort to control the muscle.
Muscle fibers (cells) are long, threadline with alternating light and dark cross markings (STRIATIONS)
Nucleus is off to the side
Describe Smooth muscle tissue.
Involuntary, non-striated muscle cells. nucleus is located centrally.
Location:
walls of hollow internal organs, glands, and linings of blood vessels
Describe Cardiac muscle tissue
Involuntary, striated muscle tissue found only in the heart characterized by its INTERCALATED DISCS between cells. Arranged in branched, interconnecting networks.
Draw and label a Neuron (nerve cell): Dendrites, Axon, Body, Axon terminal, Synapse
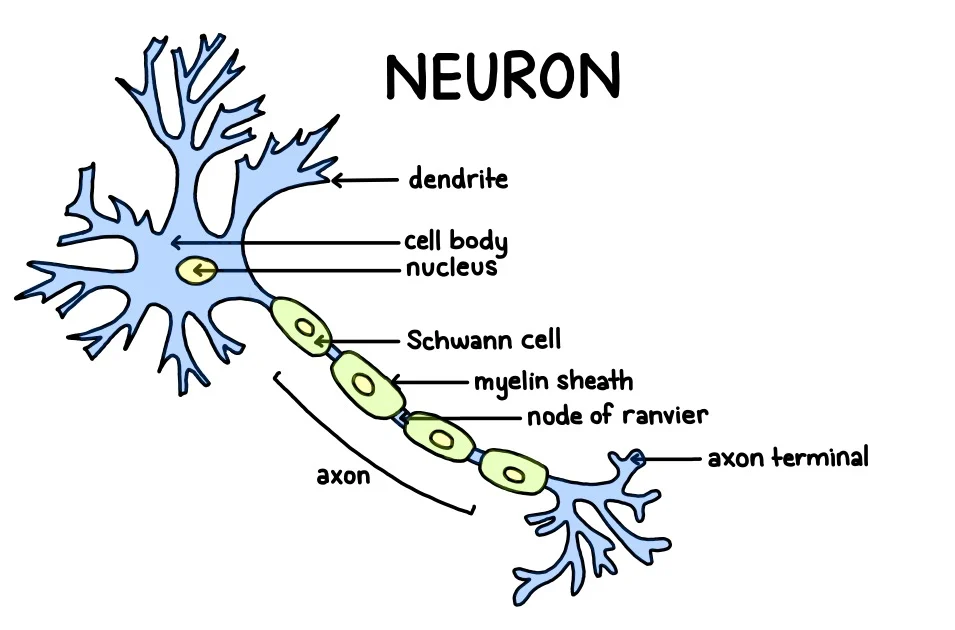
Define synapse
the site of transmission of electric nerve impulses between two nerve cells (neurons) or between a neuron and a gland or muscle cell (effector)
Define ganglion
Grouping of neuron cell bodies outside of the CNS
Compare and contrast afferent and efferent nerves.
Afferent Nerve:
aka sensory neuron
carries info from PNS to CNS (body to brain)
transmits sensory information (pain, temp, tactile info)
Efferent Nerve:
aka motor neurons
carries info from CNS to PNS (brain to body)
transmits motor information for controlling muscle movement