Assessment and Management of Patients with Vascular Disorders and Problems of Peripheral Circulation
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
Health History: arterial
-Pain
-Intermittent Claudication: pain (muscular, crampy), discomfort or fatigue cause by inability to the arterial system to provide adequate blood flow to the tissues in the face of increased demand s for nutrients and oxygen during exersice
-Pain occurs as metabolites aggravate the nerve endings in surrounding tissue
-50-70% of lumen obstructed before pain occurs
arterial issue
-getting blood from heart to periphery
-no oxygen getting to extremities
-ex: intermittent claudication/fatigue
physical assessment PAD
◦Inspection of skin (pallor, rubor with dependent position)
◦Loss of hair
◦Brittle nails
◦Dry, scaling skin
◦Atrophy
◦Ulcerations- dry and occur in the periphery
◦Edema
◦Gangrenous changes (dry)
-Pulses
Diagnostic Evaluation for PAD
-Doppler Ultrasound Studies
-Ankle-brachial index (ABI)-> ratio of systolic blood pressure in the ankle to the systolic blood pressure in the arm
◦Able to quantify the degree of stenosis
◦With increasing disease there is a progressive decrease in Systolic pressure distal to involved sites
-Exercise testing
-Duplex Ultrasonography
-CT scanning
-Angiography
exercise testing
see how long patient can walk without caludication, ankle BP will drop and AKI will be large
Duplex Ultrasonography
non invasive
CT scan
-contrast injected
-watch allergies and renal function (order baseline BUN and Creatanine)
angiography
isolate blood vessels to look at them
arterial pain pulses and skin
Pain
-Intermittent claudication to sharp unrelenting (calf)
Pulses
diminished or absent
-may hear bruit
-pulses can be unequal
Skin
-dependent–rubor
-elevation-pallor
-shiny
-cool to cold
-nails thickened and rigid
-less hair
venous pain, pulses, and skin
Pain
-aching, cramping
Pulses
-Present but may be difficult to palpate through edema
Skin
-pigmentation-medial and lateral malleolus
-thickened
-tough skin
-frequently reddish –blue color & associated with dermatitis
venous issues mean
blood pools
arterial ulcer
-location
-pain
-shape
-base
-leg edema
Location: tips of toes, toe webs, heel starts in periphery and moves up
Pain: very painful
Depth: deep often into joint
Shape: circular
Base :Pale to black and dry gangrene
Leg Edema: minimal unless leg is in a dependent position
venous ulcer
-location
-pain
-shape
-base
-leg edema
Location:
-medial or lateral malleolus (ankle)
-anterior tibial area
Pain: minimal if superficial (because they have circulation)
Depth : superficial
Shape: irregular border
Base: granulation tissue, beefy red to yellow fibrinous if chronic
Leg Edema: moderate to severe
Diagnostic tests for PVD
-venography
-along with all the PAD tests
Prevention
-Reduction of fat in diet
-Exercise
Reduce lipid levels (LDL < 100)
-Cholesterol < 200
-Triglyceride < 150
Statins
◦Lipitor, Mevacor, Zocor, Pravachol, Crestor
-Niacin, Questran, Zetia
-Manage HTN
medical management
-surgical
-radiologic procedures
surgical management
Vascular surgical procedures
◦Improve blood supply from aorta to femoral artery
◦Outflow procedures: provide blood supply to vessels below the femoral artery
radiologic procedures
◦Arteriogram
◦Angiography (both)
-venogrpahy
patient on statins what do you monitor
liver enzymes/function
Nursing Management
-Improving Peripheral Arterial Circulation (exercise and dangle legs)
-Promoting Vasodilation and Preventing Vascular Compression (warm compress becareful because they can burn easily)
-Relieve Pain
-Maintain Tissue Integrity
what does walking help improve
collateral circulation
-walk walk walk until pain, then rest, then walk again.
a patient with PAD when they elevate legs what will happen
the legs will be pale
neurovascular check is what
6 Ps
medical management of PAD
-Exercise program
-Walking program
-Cessation of tobacco use
-Endarterectomy
-Bypass grafts
PAD Pharmacological Therapy
SYMPTOMATIC CLAUDICATION
-Trental- decreases viscosity to help blood flow better
-Pletal- vasodilator and inhibits platlet agregation
ANTI-PLATLET
-Aspirin (ASA)
-Plavix
Stabalize plaque
-Statins
nursing management to maintain circulation PAD
◦frequent checks for pulses, color, capillary refill, temp
-check area distal to the graft
-no pulse contact HCP
nursing management Potential complications PAD
◦urine output, mental status, central venous pressure and pulse rate
◦prevent thrombosis by no leg crossing and no prolonged leg dependence
Discharge planning PAD
◦assessment of patient's ability to be independent
◦educate the patient regarding lifestyle modifications
Aneurysms
Localized sac or dilation formed at a weak point in the wall of an artery
Life threatening-> rupture leads to hemorrhage and death
saccular vs fusiform vs dissecting
◦Saccular- ON ONE WALL
◦Fusiform -all the way around
-dissecting-ruptured all blood comes rushing out
Thoracic Aortic Aneurysm
-70% of all cases cause by atherosclerosis
-50-70 years
-Most common site for dissecting aneurysm
-1/3 of patient with thoracic aneurysm die due to rupture
-chest xray
Clinical Manifestations of thoracic aneurysms
-Variable, dependent on how rapidly the aneurysm dilates and how the pulsating mass affects surrounding intrathoracic structures
-Asymptomatic
Constant, boring (may occur only when supine)
-Dyspnea or cough
-Hoarseness, stridor or aphonia
-Large veins in chest compressed: become dilated
Diagnosis for thoracic aortic anyeurism
-Chest x-ray
-Computed tomography angiography (CTA)
-Transesophageal echocardiography (TEE)
medical management for Thoracic anyeurysm pt one
Blood pressure control with dissection
◦SBP < 90-120 mm Hg or MAP < 60-75 mm Hg
◦Esmolol
◦Hydralazine
◦Nipride
medical management for Thoracic anyeurysm pt 2
Emergent surgery to repair aneurysm and restore vascular continuity with graft
◦3-4% risk of paraplegia
◦Endovascular grafts place percutaneously in interventional radiology
◦No cross-clamping required
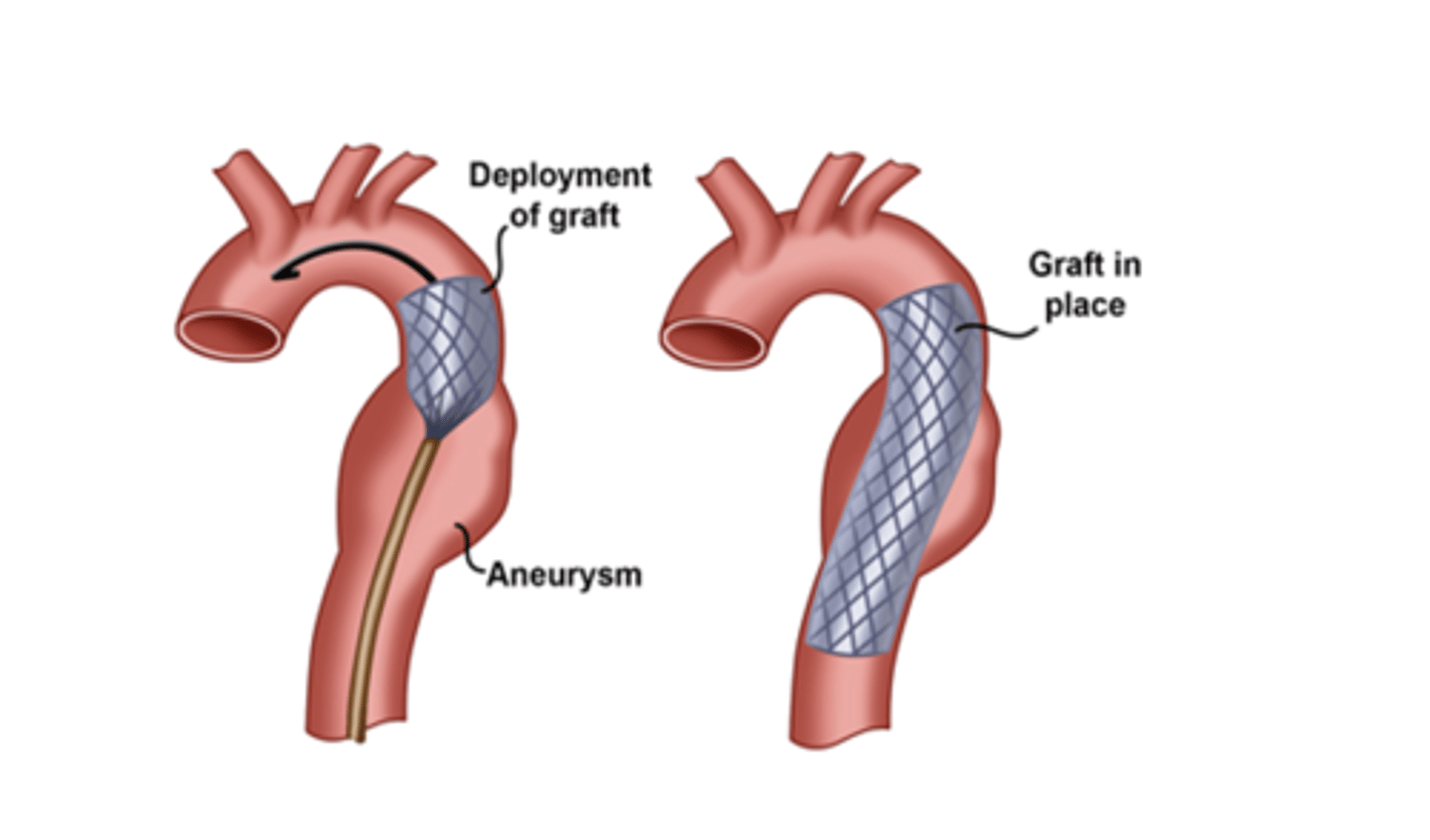
graft pic
Abdominal Aortic Aneurysm
-Etiology->atherosclerosis
-Men> women
-Caucasian> black
-Location: Occur below the renal arteries (infrarenal aneurysm)
If untreated->eventual rupture and death
-Pathophysiology
◦Damaged medial layer of the vessel
abdominal aortic anyeurism clinical manifestation
-40% have symptoms
-Feel their heart beating in their abdomen when lying down
-Abdominal pulsatile mass
-Thrombus may occlude vessel -> emboli-> cyanosis and mottling of toes
does a patient with a minor anyeurysm get surgery
usually not right away -Evaluation via CTA every 6-months
Pharmacologic Management of abdominal aortic anyeurism
-Close blood pressure monitoring
-Antihypertensive agents
Diuretics
Beta-blockers
ACE inhibitors
Angiotensin II receptor antagonists
Calcium channel blockers
Surgical Treatment AAA
-Surgery is treatment of choice for AAA >5.5 cm (2 inches)
-Open surgical repair by resection and bypass grafting
-Mortality rate 1-4% with surgery
-Endovascular grafting: local or regional anesthesia
Dissecting Aorta
-Tear develops in the intima or media
-Dissections commonly associated with poorly controlled HTN, blunt chest trauma, cocaine use
-Tear occurs most commonly in the region of the aortic arch
Highest mortality with
-ascending aortic dissection
-Aorta sends the blood to the rest of the body
Clinical Manifestations dissecting aortic arch anyeurism
-Onset is sudden
Severe, persistent pain (tearing or ripping)
-Pain is anterior chest or back and extends to shoulders, epigastric area or abdomen
-Mistaken for an acute myocardial infarction
-Pale, diaphoretic
Tachycardia
-Blood pressure elevated and/or markedly different from one arm to the other
Arterial Embolism & Arterial Thrombosis
-happens from clot that develops in left side of the heart and goes to arterial circulation and get caught somewhere
-most common from Afib, AMI, endocarditis, HF
Arterial Embolism & Arterial Thrombosis CM
◦Depends on size, organ involvement and collateral circulation
◦Acute, severe pain
◦Gradual loss of sensory and motor function
◦Six P's: pain, pallor, pulseless, paresthesia, poikilothermic (cold), paralysis
Arterial Embolism & Arterial Thrombosis DIAGNOSIS
-CHEST XRAY
-ECG (tells us about underlying cardiac issues)
-TEE
Acute Thrombosis
occurs in patients with pre-existing ischemic symptoms
Manifestations acute thrombus
-similar to arterial emboli
-treatment is more difficult secondary to occlusion developing in a vessel which requires surgical reconstruction to restore blood flow
Assessment and Diagnostic Tests acute thrombosis
-Doppler Ultrasonography
Arteriography
◦determines the presence and extent of atherosclerosis
Nursing Management thrombus
-Bedrest with the affected extremity at bed level or slightly dependent
-Extremity is protected from mechanical trauma and kept at room temperature
-If thrombolytic medication administered->
◦ICU for close observation for possible hemorrhaging
-If surgery is indicated the appropriate consents are signed and after the patient is encouraged to move the extremity to prevent stasis of blood
-Possible Complications
◦metabolic abnormalities
◦renal failure
compartment syndrome
Raynaud's Phenomenon
-affects the small blood vessels
-usually in the extremities
-results in low blood flow
-occurs in cold temperatures
-Usually affects women between 16-40
-Varying degrees of involvement
PRIMARY Raynauds phenomenon
no underlying cause
secondary raynauds
◦In association with an underlying disease (rheumatoid arthritis, systemic lupus erythematosus, scleroderma, trauma or obstructive lesions)
raynauds classic clinical picture
bilateral and symmetrical, involves toes and fingers
-White/pallor secondary to sudden vasoconstriction->
-cyanotic secondary to pooling of unoxygenated blood during vasospasm-> exaggerated
-reperfusion results in rubor (red) secondary to oxygenated blood perfusing area
white, blue, red
management of raynauds
Avoid cold, tobacco and stress
what drug may relieve raynaud symptoms
-Calcium Channel Blockers may effectively relieve symptoms
-nitrates- vasodilation
Deep Vein Thrombosis
vein develop clot in the deep ones
Pulmonary Embolism
clot travels to lungs
-Affects approximately 10-20% medical patients & up to 80% critically ill
superficial and deep veins are effected
Superficial veins: greater saphenous, lesser saphenous, cephalic, basilic and external jugular veins
Deep veins: thin walled, less muscle
Virchow's Triad
decides who is at risk for DVT or PE
◦Endothelial damage
◦Venous stasis
◦Altered coagulation
Endothelial Damage
◦Trauma, surgery, pacing wires
◦Central venous catheters, dialysis catheters
◦Local vein damage, repetitive motion
Venous Stasis
◦Bed rest/immobilization
◦Obesity, age > 65
◦History of varicosities
◦Spinal cord injury
Altered Coagulation
◦Cancer
◦Pregnancy
◦Oral contraceptive use
◦Protein C & S deficiency
◦Polycythemia
◦Sepsis
ASSESSMENT findings for DVT
-Pain
-Heaviness
-Functional impairment
-Ankle engorgement
-Edema
-Increase temperature in leg
-Tenderness
-HOMANS SIGN IS NOT A RELIABLE SIGN FOR DVT

PREVENTION OF dvt
-lovonox
-ambulation
-SCD
-TED HOSE
-LEG EXCERICISES
-Patient with prior history of VTE are at increased risk of new episode: rate of recurrence is 25% in 5 years
DVP/PE: Medical Management
-prevent thrombus from growing and fragmenting (thus risking PE), recurrent thromboemboli and post thrombotic syndrome
-Superficial veins have a ____ of thrombi becoming DISLODGED
- EMBOLI
-lower chance
-dissolve spontaneously (treated at home with bed rest, elevation of leg, analgesics anti-inflammatory)
Anticoagulation Therapy
◦delays clotting time of blood
◦prevents the formation of a thrombus in postoperative patients
◦forestall the extension of a thrombus after it has formed
deep vein thrombosis needs to be put on
anti-coagulant therapy
-bed rest untill blood is therapeutic so clot wont dislondge
ANTICOAGULANT THERAPY CANNOT
◦cannot dissolve a thrombus that has already formed
Anticoagulation Therapy EXAMPLE
-Unfractionated heparin: Heparin
-Low-molecular weight heparin: Lovenox
-Oral anticoagulation: Coumadin
-Factor Xa Inhibitor: Arixtra
-Oral Factor XA inhibitor: Xarelto, Pradaxa
-Thrombolytic therapy: t-PA, TNKase
-Direct thrombin inhibitor: Refludan, Novastan
Contraindications to Anticoagulation
-Nonadherence to medications
Bleeding (GI, GU, Respiratory, Reproductive)
-Hemorrhagic blood dyscrasias
-Aneurysms
-Severer trauma
-Alcoholism
-Recent or impending surgery of th eye, spinal cord or brain
-Severe hepatic of renal disease
-Recent CVA
-Infections
-Open ulcerative wounds
-Occupation involving significant hazard
-Recent childbirth
Heparain (IV)/coumadin (po) monitor
APPT = draw blood from patient q4-6 hrs
-70-100 is therapeutic
-they titrate the drip to accomodate the therapeutic levels DRIP
-(1.5 TIMES NORMAL)
-if level is over 100 we stop the drip for an hour and restart it at a lower rate then it was at before (draw blood in 6 hrs), if less then 70 may need to increase
-For coumadin we do PT/INR qdaily
you keep them on heparin IV and coumadin PO untill when
coumadin has desired effects
-2-3
-once coumadin is at the level we want we stop heparin
Endovascular Management is Necessary when
anticoagulation or thrombolytic therapy is contraindicated, the danger of PE is extreme or venous drainage is severely compromised
-thrombectomy
-Ultrasound assisted thrombolysis
-vena cava filter
Assessing and monitoring anticoagulant therapy WHAT values are important
◦Heparin (aPTT 1.5 times normal)
◦Coumadin (INR 2.0-3.0)
vena cava filter
umbrella that opens to catch clots
-patients who cannot be on anti-coagulants
nursing management on anticoagulants
-Monitoring for bleeding, thrombocytopenia, drug interactions
-Providing comfort
-Compression therapy stockings
-Intermittent pneumatic compression devises
-External compression devices/wraps
Chronic Venous Insufficiency
-Results from obstruction of venous valves in legs or reflux of blood through valves
-Superficial and deep veins involved
-Venous HTN occurs
-PEOPLE WHO STAND FOR LONG HOURS AT RISK
which test confirms obstruction/identifies valvular incompetence?
Duplex ultrasonography
Chronic Venous Insufficiency: Management: Increasing venous blood flow
◦Antigravity activities-> elevate legs 15-20 minutes 4 times/day
◦At night-> foot of bed elevated 6 inches
◦Avoid prolonged sitting or standing
◦Encourage walking
◦Avoid crossing legs
-Graduated compression stockings
arterial ulcers
-Intermittent claudication
-Digital or forefoot pain at rest
-If acute-severe and unrelenting pain
-Small, circular, deep ulcerations of the tip of toes or the area between toes, and the medial side of the hallux or 5th lateral toe
-may never heal
venous ulcers
-Pain- aching or heavy
-Foot and ankle may be edematous
-Ulcers in medial or lateral malleolus, and usually large superficial and exudative
-Average of 6-12 months to heal and as many as 70% will reoccur within 5 years
Leg Ulcers: Management
Pharmacological therapy
◦antiseptic agents, systemic antibiotics
Compression therapy
◦Unna boots, graduated compression stockings
debridement promotes
healing
during necrosis to remove dead tissue
LEG ULCER MED MANAGEMENT (Hyperbaric Oxygen Chamber/ NEG pressure wound therapy)
Hyperbaric Oxygen Chamber
◦Can be used as an adjunct therapy especially in diabetic patients after no improvement in 30 days.
◦90 to 120 minutes once daily for 30 to 90 sessions
Negative pressure wound therapy using vacuum-assisted closure (VAC)
cellulitis is most common
Most common infectious cause of limb swelling
cellulitis manifestations
acute onset of swelling, localized redness, pain and can be accompanied by fever, chills, and sweating
management of cellulitis
Antibiotics (depending on the severity: outpatient or inpatient)
nursing management
elevate limb 3-6 inches above the heart every 2-4 hours and apply warm compresses