CANCER
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
oncogenes
________________ drive cancer progression
tumor suppressors
______________ inhibits cancer progression
DNA proofreading and repair
What is critical in the prevention of cancer?
surgery, radiation, chemo, palliative care
Ways to treat cancer - general
Neoadjuvant
BEFORE SURGERY (see if it shrinks)
Adjuvant
after surgery for the residuals
Maximum tolerated dose (low TI)
Chemo dosing is based on
prevents resistance
Why is combination therapy the norm for chemo?
supervised IV dosing (low TI), hormonal-based or kinase inhibitor may be given orally
Route of administrations for chemo
S phase, M phase
Most chemo drugs target what - efficacy is based on the concept that cancer is a disease of rapidly dividing cells
antimetabolites, DNA damaging agents
Agents that target the S phase (synthesis of DNA)
microtubule targeting drugs
Drugs that inhibits the M phase (mitosis)
Crosslink and damage; inhibit synthesis or transcription, repair inhibitors
Ways that chemo disrupts the DNA
Cyclophosphamide (alkylating agent), cisplatin (platinum drug)
Examples of Chemo agents that crosslink and damage DNA
Doxorubicin (intercalating agent (no unzipping these genes)), 5-FU/MTX (antimetabolites), Topotecan (topoisomerase inhibitorsin)
Examples of Chemo agents inhibit DNA synthesis and transcription
PARP inhibitors
Examples of Chemo agents that inhibit DNA repair
Doxorubicin
Which chemo agent is produced from soil-based streptocyces peucetius and is commonly used for leukemias, lymphomas, bladder, breast, stomach, lung, ovarian, thyroid, sarcoma, and myeloma
Cardiotoxicity (rapid development of heart failure)
What is the dose-limiting effect of doxorubicin - dose dependent and cumulative
Doxil (liposomal formula, deposits in the skin)
If doxorubicin is working great on your patient, but they start to get cardiac side effects, what can we switch them to?
-platins
Examples of platinum agents
neurotoxicity (cisplatin), nephrotoxicity (cisplatin), myelosuppression (carboplastin), hearing loss
ADRs for the -platins
testicular, ovarian (carboplatin), cervical, breast, bladder, head, neck, lung, brain, colorectal (oxaliplatin)
Indications for platinum agents (use in combination…)
thymidine synthase inhibitor (anti-metabolite)
MOA for 5-FU (5-fluorouracil)
breast, colon, rectum, stomach, pancreas, BCC skin cancers
Indications for 5-FU
inflammation of the skin and mouth, CNS damage, diarrhea
ADRs for 5-FU
If we knock out all the pathways for repair → cancer cell dead (watch in peds can give rise to secondary cancers)
Okay so if DNA damage causes cancers, why are we causing more to cure it??
Normal cells have BRCA to fall back on - the others don’t
Why are PARP inhibitors “selective” in a sense for BRCA deficient cells?
Destabilizers (destroy the structure), stabilizers (clump’em together)
Categories of microtubule targeted drugs
Vinca alkaloids (vinblastine, vincristine), eribulin
Microtubule destabilizers can be used in lymphoma, leukemia, sarcoma, neuroblastoma, testicular and lung cancers - what are some examples
Taxanes (paciltaxel, docetaxel), Ixabepilone
Microtubule stabilizers can be used in ovarian, breast, lung, cervical, pancreatic, stomach, prostate, head and neck cancers - what are some examples
rapidly dividing tumors, hematological malignancies, slow-growing tumors, or nondividing cells (slow the signal transduction because there’s no traintracks)
Microtubule targeted drugs are effective in
Bone marrow suppression, GI disturbance (mucositis), alopecia, Neurotoxicity (peripheral neuropathy is dose limiting)
ADRs of antimiotic chemo
CD30 antigen
What is a defining marker of lymphomas
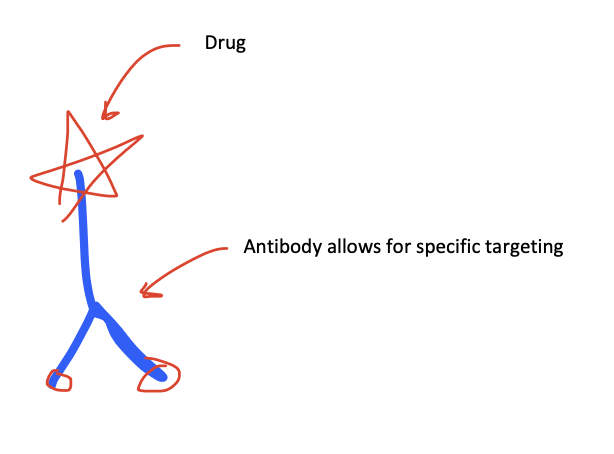
MMAE (monomethyl auristatin E)
What is effective at targeting CD30 but must be attached to an antibody (suicide bomber style)
peripheral neuropathy, neutropenia
Dose limiting effects of MMAE
slow growth (mutate in the midst of chemo), efflux pump (chemo can’t act), evade the immune system (no CD8 or NK response)
Mechanisms of resistance in cancer cells
mutation at the specific binding site, a different driver (upregulation of complementary pathways), efflux pumps
Innate resistance of cancer cells can be due to
breast, prostate, ovarian
Cancers driven by hormones
binding of hormone to intracellular receptor, nuclear translocation of receptor, regulation of gene expression drives the growth
Hormone driven cancers require 3 steps what are they
LH releasing hormone (LHRH) agonist, LH antagonist, androgen receptor antagonists,
Which classes of medications can be used for androgen deprivation therapy (ADT) for the treatment of androgen dependent prostate cancer
leuprolide, goserlin (note: testosterone flairs initially then crashes in about a month)
Examples of LHRH agonists
degarelix (no flair)
Examples of LH antagonists
hot flashes, decreased bone density, loss of muscle mass, weight gain, insulin resistance, ED, low libido, cognitive impairments
Side effects of Androgen deprivation therapy - think menopause
Bicalutamide (partial agonist), Enzalutamide (multiple spots of inhibition)
Examples of androgen receptor antagonists (effective even in castration resistant tumors)
taxane-based chemo (microtubule disruption)
ADT has an initial response rate of 80-90% but nearly all men progress to castration resistant prostate cancer - what do we do now?
decreased estrogen levels, inhibit estrogen receptor mediated transcription
Strategies for inhibiting estrogen signaling
Aromatase inhibitors, Estrogen receptor antagonists
Gameplan for post-menopausal women or those with NO ovaries
GnRH/LHRH agonists, SERMs
Gameplan for pre-menopausal women with ER-positive breast cancer
tamoxifen (antagonist in breast, agonist in uterus and bone)
Examples of SERM
anastrozole, letrozole, exemestane
Examples of aromatase inhibitors
fulvestrant
Examples of estrogen receptor antagonists
Trastuzumab (herceptin - targets and neutralizes the receptor, can add a conjugate to the antibody)
What is the gameplan for HER-2 positive cancers? (used in combination)
immunotherapy + chemo
What is the gameplan for triple negative breast cancer?
single chromosomal translocation generating BCR-ABL on a philly chromosome
CML can be caused by a
Imatinib (gleevec - kinase inhibitor)
What drug can selectively block BCR-ABL activitty
when the main driver of the tumor can be inhibited
When are kinase inhibitors helpful
VEGF inhibition, VEGF kinase inhibitor
What drug classes target the angiogenesis of cancers
bevacizumb (avastin)
Examples of VEGF inhibitors (useful for cervical, colorectal, glioblastoma, ovarian, renal)
Sorafenib (HCC, renal, thyroid), Sunitinib (GI, pancreatic, renal)
Examples and uses of VEGF kinase inhibitors
hemorrhage, clots, HTN, healing defects, GI perf, fatigue, diarrhea, heart failure
Side effects of anything that target angiogenesis
checkpoint inhibitors (note: you need the TCR/HLA action for these to work)
Immunotherapy classes of anticancer drugs
PD-1 inhibitors (CD8), PD-L1 inhibitor (cancer cell), CTLA-4 inhibitor
Classes of checkpoint inhibitors
Pembrolizumab (keytruda - melanoma, lung, head, neck), Nivolumab (melanoma, lung, renal, lymphoma)
Examples of PD-1 inhibitors
Atezolizumab, durvalumab
Examples of PD-L1 inhibitors (Used for urothelial, lung)
ipilimumab (melanoma)
Examples of CTLA-4 inhibitors
patients with high mutational burden (long-term survival advantages in 30%)
Checkpoint inhibitors work by letting the immune system go crazy - when is the useful?
Autoimmune effects (could be a delayed onset), EXPENSIVE AF
ADRs for checkpoint inhibitors
Phase 1 (safety) → Phase 2 (effective) → Phase 3 (compare to the STANDARD - not ethical to use placebo)
Describe the clinical trial process for chemo agents
early diagnosis, new therapeutic options, better management of toxicities
What causes an increased survival in cancer?
secondary cancers, long term toxicities, financial debt
Challenges of surviving cancer