6 Ischemic Heart Disease
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
what is ischemia?
reduced/inadequate blood supply to an organ or part of body
what is ischemic heart disease
imbalance between myocardial oxygen supply and demand
when oxygen demand does not equal oxygen supply what happens?
myocardial hypoxia
what is the ischemia most often caused by
coronary artery disease (atherosclerosis) - fixed plaques that limit myocardial blood supply by decreasing the vessel’s lumen
what is an infarction?
irreversible tissue damage from prolonged ischemia
what is the most common presentation of ischemia?
angina pectoris (uncomfortable sensation inchest due to myocardial ischemia) ; chest pain/pressure on left side
what are other common signs and symptoms of ischemia?
neck/jaw pain
shoulder/arm pain
nausea/vomiting
sweating
shortness of breath when active
fatigue
tachycardia
chest pain caused by ischemia can be prompted by
coacaine use
cold temperatures (shoveling in cold temps → vasoconstric → increase afterload)
emotional stress
physical exertion (increases oxygen demand)
what are the relieving factors of myocardial ischemia vs myocardial infarction?
ischemia : relieved with rest or nitroglycerin within 10-15 min
infarction : symptoms persist after 15 minutes and not relieved with rest or nitroglycerin
what is the duration of myocardial ischemia vs myocardial infarction?
ischemia : chest pain less than 15 minutes
infarction : chest pain more than 15 minutes
what is the severity of myocardial ischemia vs myocardial infarction?
ischemia : no permanent damage to heart muscle
infarction : serious condition that could cause permanent damage ; blood flow must be restored within 20 minutes to prevent irreversible damage
what is nitroglycerine?
vasodilator (relaxes smooth musvle and blood vessels) that reduced heart’s workload
what is stable angina?
chronic pattern of angina pectoris (physical exertion or emotional stress) relieved by rest
what is variant angina?
angina discomfort at rest due to coronary artery spasm (transient ST elevation)
what is silent ischemia?
asymptomatic episodes of myocardial ischemia
what is unstable angina?
pattern of increased frequency and duration of angina pectoris produced by less exertion or rest
what is a myocardial infarction
myocardial necrosis due to occluded blood supply
what else can cause ischemia besides CAD?
thrombus (sudden rupture of plaque)
coronary artery spasm (temp tightening of arterial muscle walls that can spontaneously prevent myocardial blood flow)
hypotension (decreased perfusion pressure)
anemia (decreased blood oxygen)
myocardial blood flow depends on? which is most referred to and why?
myocardial oxygen supply
rate of coronary blood flow (most referred to bc we can’t change amount of oxygen in blood)
what is myocardial oxygen supply?
determined by hemogloabin concentration
what is the rate of coronary blood flow?
more dynamic and deals with coronary perfusion
what is the equation to calculate flow in blood vessels?
Q (flow) = P (pressure) / R (vascular resistance)
when does coronary perfusion dominance take place and why?
diastole bc myocardium is relaxed and coronary vasculature is not compressed
what is coronary perfusion pressure?
pressure gradient that drives coronary blood flow
coronary perfusion pressure is approximated by
aortic diastolic pressure (diastolic pressure in aorta is greater than in LV which allows dominant diastolic coronary perfusion)
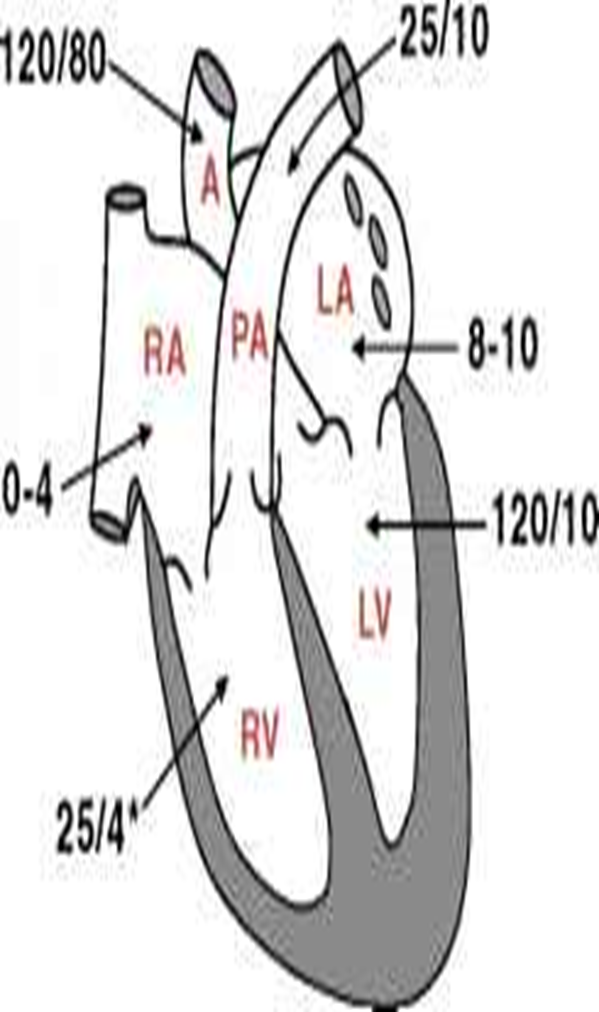
what is the diastolic pressure of the LV typically around and why is that important?
around 10; important because this shows the ventricles ability to relax during the filling stage
what happens to coronary vasculature in systole and diastole?
in systole coronary vasculature is compressed and in diastole it is not compressed
what conditions decrease aortic diastolic pressure?
hypotension
aortic regurgitation
what does a decreas in aortic diastolic pressure do to coronary artery perfusion?
decreases coronary artery perfusion → decreasing myocardial oxygen supply
what is coronary vascular resistance?
resistance to flow that must be overcome to push blood through coronary vasculature
coronary vascular resistance can be affected by
forces that externally compress arteries (systolic compression of myocardium)
factors that alter intrinsic coronary tone
what is autoregulation?
local blood flow regulation where organ’s intrinsic ability can maintain constant blood flow regardless of perfusion pressure changes
what is the only way to get additional oxygen supply to coronary arteries?
increase blood flow (other arteries can extract oxygen but coronary arteries can not bc it will remove too much)
how does autoregulation increase flow in coronary arteries?
via local chemical environment → vessels vasodilate in order to increase flow
what is vascular tone?
degree of constriction in blood vessels
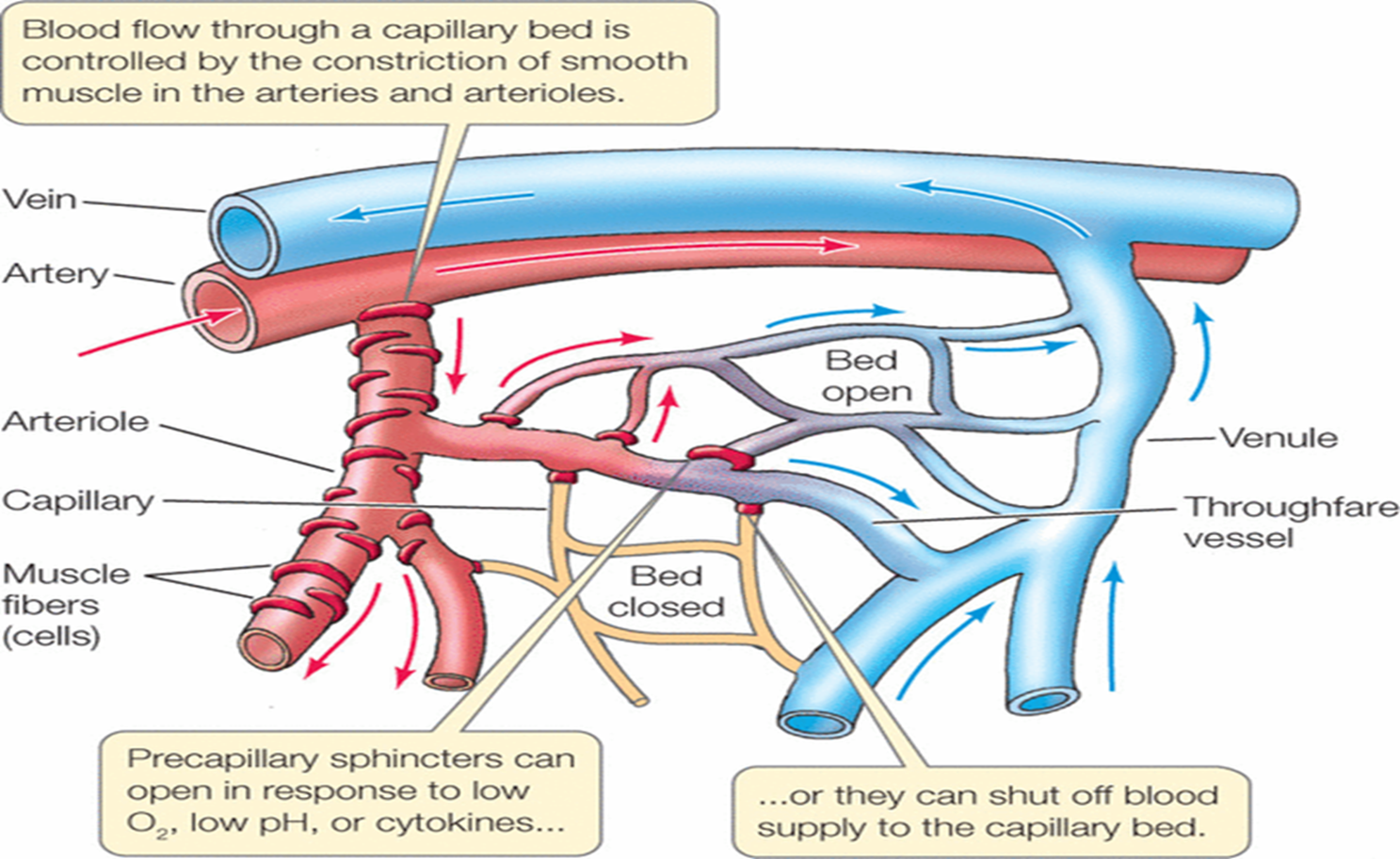
what is increased/decreased vascular tone?
increased : vasoconstriction
decreased : vasodilation
what is vasodilatory reserve?
distal vessels free of flow limiting plaques can adjust vasomotor tone in response to metabolic needs ; these vessels serve as reserve, increasing diameter to meet increasing oxygen demand
what is stunned myocardium?
after transient ischemia → tissue with prolonged systolic dysfuncton that gradually recovers
what is hibernating myocardium?
chronic ventricular contractile dysfunction due to persistently reduced blood supply ; usually due to multi vessel CAD
what are the three major determinants of myocardial oxygen demand?**
ventricular wall stress
heart rate
contractility (inotropic state)
how is myocardial oxygen supply determined?
oxygen content
coronary blood flow
what do positive/negative inotropic drugs do?
positive : increase force of contraction and increase oxygen demand
negative : decrease force of contraction and decrease oxygen consumption
what is wall stress?
force acting on myocardial fibers/wall
what does laplaces relationship demonstrate
wall stress
what is laplaces relationship?
(P*r) / 2h = wall stress
P = intraventricular pressure
r = radius
h = ventricular wall thickness
what is the relationship between wall stress and intraventricular pressure, radius of ventricle, and ventricular wall thickness?
intraventricular pressure : directly related
radius : directly related
ventricular wall thickness : inversely related
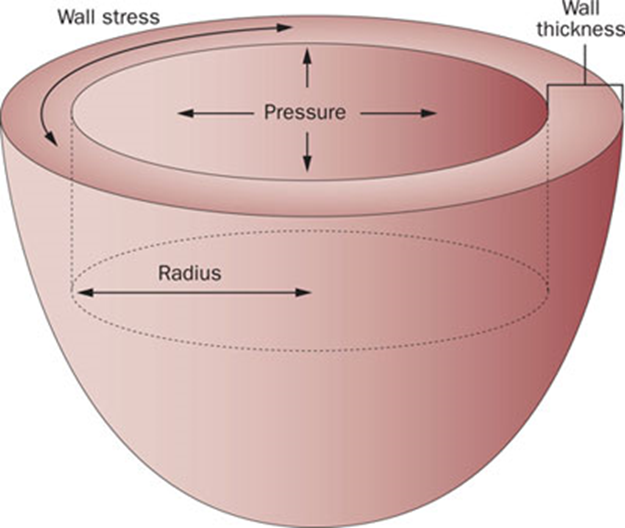
an increase in pressure or radius can be caused by
high blood pressure or increased volume
an increase in pressure or radius causes
increased wall stress → ventricular hypertrophy → more force to contract ventricle
how are wall stress and systolic ventricular pressure related?
directly related
what conditions increase pressure?
aortic stenosis
hypertension
how does wall stress affect afterload and myocardial oxygen consumption?
directly related
conditions that decrease ventricular pressure will also decrease
wall stress and myocardial oxygen consumption
what conditions increase radius in terms of wall stress?
regurgitation of valves ; conditions that increase LV filling and volume
how does wall thickness relate to wall stress and why?
inversely related; because as wall thickens (hypertrophies) force is spread over greater muscle mass which decreases wall stress
how does wall thickness affect oxygen consumption?
initially will decrease oxygen consumption,but overal will require more oxygen/blood flow because they fatigue easier
increased afterload can cause
hypertrophy
how does heart rate relate to myocardial oxygen demand?
slower heart rate → longer diastolic time → more perfusion (delivering oxygen and nutrients through blood)
when does coronary artery perfusion take place?
ventricular diastole
faster heart rate causes
more oxygen consumption → increasing oxygen demand
what is the double issue with tachycardia and myocardial ischemia?
tachycardia increases oxygen demand because ventricle is contracting more frequently ; but there is a decreased oxygen supply due to less time for coronary arteries to fill during diastole
how does bradycardia affect coronary perfusion and why?
can initially improve perfusion due to longer diastolic time (longer time for blood to flow into coronary arteries) ; eventually very slow heart rate can decrease cardiac output
how does myocardial ischemia occur?
when myocardial oxygen supply does not meet myocardial oxygen demand
what does hemodynamic significance depend on?
degree of narrowing
amount of compensatory vasodilation distal resistance vessels can achieve