63-66 Metabolism and Temperature Regulation
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Metabolism of Nutrients in the Organism
Metabolism is the set of biochemical reactions that allow cells to extract energy from nutrients and use them for maintenance, growth, and repair. The three primary macronutrients — carbohydrates, proteins, and lipids — undergo distinct metabolic pathways but are interrelated through various biochemical conversions.
Carbohydrates
Digested into glucose, which serves as the primary energy source.
Excess glucose is stored as glycogen in the liver and muscles or converted into fat.
The liver plays a critical role in glucose homeostasis by releasing glucose when needed.
Proteins
Broken down into amino acids, which are used for protein synthesis and cellular functions.
Some amino acids are converted into glucose via gluconeogenesis.
Excess amino acids are deaminated, and their nitrogen is excreted as urea.
Lipids
Used as an energy source, particularly when carbohydrates are scarce.
Stored as triglycerides in adipose tissue.
Broken down into fatty acids and glycerol, which are oxidized to generate ATP.
Metabolism of Carbohydrates: The Level and Regulation of Glucose in the Circulating Blood
Blood Glucose Levels = 2.8 - 6 mmol/L
Hormonal Regulation
Insulin (from the pancreas) lowers blood glucose by promoting glucose uptake and glycogenesis.
Glucagon (also from the pancreas) increases blood glucose by stimulating glycogenolysis and gluconeogenesis.
Cortisol enhances gluconeogenesis by mobilizing amino acids from protein stores.
Glycogen Metabolism
Glycogenesis: Formation of glycogen from glucose for storage.
Glycogenolysis: Breakdown of glycogen to release glucose when needed.
Gluconeogenesis
The liver converts amino acids and glycerol into glucose when carbohydrate intake is low.
This process is stimulated by low blood sugar and high cortisol levels.
Pentose Phosphate Pathway
Generates NADPH, which is crucial for fatty acid synthesis and cellular antioxidation
Metabolism of Proteins and Its Control
Protein metabolism involves the breakdown and synthesis of proteins for cellular functions.
Protein Breakdown
Proteins are hydrolyzed into amino acids, which can be used for energy or converted into other molecules.
Deamination removes the amino group, producing ammonia, which is then converted into urea in the liver.
Amino Acid Utilization
Some amino acids enter the citric acid cycle to produce ATP.
Other amino acids are converted into glucose (gluconeogenesis) or fatty acids.
Urea Cycle
The liver removes excess nitrogen by converting ammonia into urea for excretion.
If this process is impaired, ammonia accumulates, leading to toxicity.
Hormonal Control
Growth hormone promotes protein synthesis.
Cortisol mobilizes proteins for gluconeogenesis under stress conditions
Metabolism of Lipids and Its Control
Lipid metabolism provides an essential energy source and structural components for cells.
Lipid Storage and Mobilization
Lipids are stored in adipose tissue as triglycerides.
When energy is needed, triglycerides are broken down into glycerol and fatty acids.
Fatty Acid Oxidation (Beta-Oxidation)
Fatty acids are transported into mitochondria via the carnitine shuttle.
Beta-oxidation breaks fatty acids into acetyl-CoA, which enters the citric acid cycle to produce ATP.
Liver’s Role in Lipid Metabolism
Converts fatty acids into ketone bodies during fasting or carbohydrate restriction.
Synthesizes cholesterol and phospholipids for cellular functions.
Hormonal Regulation
Insulin promotes fat storage and inhibits lipolysis.
Glucagon and adrenaline stimulate lipolysis and fatty acid oxidation.
Thyroid hormones increase the rate of lipid metabolism.
Cholesterol Metabolism
The liver produces cholesterol for bile acids and cell membranes.
Excess cholesterol is transported via lipoproteins (LDL, HDL)
Energy Metabolism in the Organism
Energy metabolism refers to the biochemical processes by which the body converts nutrients into usable energy, primarily in the form of adenosine triphosphate (ATP). The three major macronutrients—carbohydrates, proteins, and lipids—are oxidized to generate ATP.
ATP as an Energy Currency
ATP stores energy in high-energy phosphate bonds and releases it as needed for cellular functions.
The body produces ATP through glycolysis, Krebs cycle, and oxidative phosphorylation.
Muscle contraction (skeletal, cardiac, smooth muscle)
Nerve impulse conduction (ATP maintains ion gradients)
Active transport of molecules (e.g., Na+/K+ pump)
Biosynthesis of macromolecules (proteins, lipids, nucleic acids)
Cellular signaling (hormone response, secondary messengers)
Oxidative and Anaerobic Energy Production
Aerobic metabolism: Oxygen is used to completely oxidize glucose, fats, and proteins, yielding high ATP output.
Anaerobic metabolism: In the absence of oxygen, glucose is partially broken down to lactic acid, providing a limited ATP supply.
Energy Release and Heat Production
Most energy from food eventually converts into heat.
Muscle contractions, protein synthesis, and organ function contribute to heat production
Energy Values of Nutrients
Carbohydrates: 4.1 kcal/g = 17.2 kJ/g
Proteins: 4.1 kcal/g = 17.2 kJ/g
Fats: 9.1 kcal/g = 38.9 kJ/g
Carbohydrates are the preferred energy source. Immediate energy source, stored as glycogen in liver/muscle.
Fats provide the most energy per gram. Stored as triglycerides; highest energy density for long-term fuel.
Proteins are primarily for tissue repair but serve as an energy source when needed. Used for structural and enzymatic functions; catabolized only when necessary.
Energy Equivalent of Oxygen
Respiratory Quotient (RQ) reflects fuel utilization:
RQ = 1.0 (pure carbohydrate metabolism).
RQ = 0.71 (pure fat metabolism).
RQ = 0.8 (pure protein metabolism).
Carbohydrates: EEO = 21 kJ/L O₂. Most efficient oxygen use; dominates in high-intensity exercise.
Fats: EEO = 19.6 kJ/L O₂. Requires more oxygen; dominant in prolonged, low-intensity activity.
Proteins: EEO = 30.0 kJ/L O₂. Last resort for energy; inefficient oxygen use.
This measurement allows scientists to estimate metabolic rate based on oxygen consumption
During exercise, carbohydrates are preferentially used because they yield more energy per unit oxygen.
Fats are the primary fuel at rest, but their oxidation requires more O₂.
Measurement of the Metabolic Rate - Direct and Indirect Calorimetry
Metabolic rate is the amount of energy used by the body per unit time and can be measured using direct or indirect calorimetry.
Direct Calorimetry
Measures the total heat liberated from the body.
Requires a calorimeter chamber where heat transfer to water is measured.
Not commonly used due to complexity.
Indirect Calorimetry
Estimates energy expenditure by measuring oxygen consumption.
Energy Expenditure (kcal) = VO2(L) × Energy Equivalent of Oxygen(kcal/L)
Uses the energy equivalent of oxygen (4.825 kcal/L) for precise calculations.
More practical and widely used.
Basal Metabolic Rate (BMR) and Daily Energy Requirements for Different Physiological States
BMR is the minimum energy required to maintain vital body functions at rest.
Heart function
Respiration
Brain activity
Kidney filtration
Cellular repair and maintenance
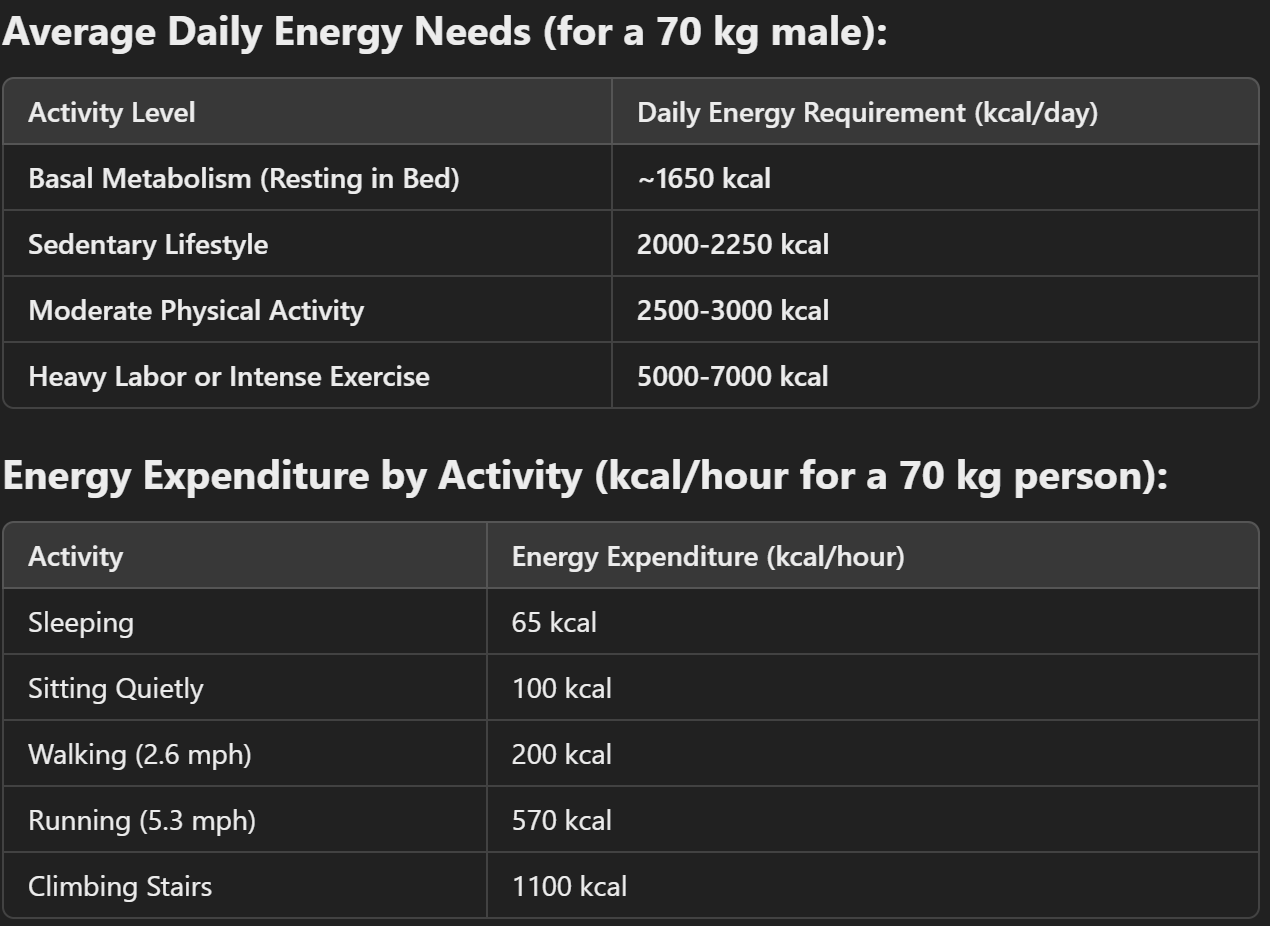
The total energy requirement depends on BMR, physical activity, and food digestion.
Energy needs vary based on activity level, age, sex, and health status.
Factors Affecting BMR
Body size & muscle mass: More muscle = higher BMR. Muscle is metabolically active.
Age: BMR decreases with age due to muscle loss
Thyroid hormones: Increase BMR by 50-100% in hyperthyroidism, decrease it by 40-60% in hypothyroidism. Regulates cellular metabolism.
Sex: Men have higher BMR than women due to greater muscle mass
Fever/Infection: BMR increases. Increased immune activity and heat production.
Starvation: BMR decreases. Metabolic adaptation to conserve energy.
Feeding: Main Principles in Defining Physiological Standards – Plastic and Energy Needs of the Organism
The regulation of food intake is a highly coordinated physiological process that ensures the body receives the necessary energy (caloric needs) and plastic materials (building blocks for growth, repair, and maintenance).
1. Plastic Needs (Macronutrient Roles in Tissue Building)
The plastic role of nutrients refers to their function in tissue growth, repair, and cellular function. Key macronutrients involved are:
Proteins → Supply amino acids for tissue growth, enzyme production, and cellular repair.
Fats → Provide lipids essential for cell membrane integrity, hormone synthesis, and energy storage.
Carbohydrates → Although primarily an energy source, glucose is essential for nucleic acid and glycoprotein synthesis.
The daily protein requirement for tissue maintenance is 30-50 grams
2. Energy Needs (Metabolic Fuel for the Body)
Energy is derived from the oxidation of macronutrients, and physiological energy requirements vary based on age, sex, body composition, and activity level. The energy balance must be maintained to prevent malnutrition or excessive weight gain
Carbohydrates: 4.1 kcal. Immediate energy source.
Proteins: 4.35 kcal. Energy source if needed; primarily structural.
Fats: 9.3 kcal. Long-term energy storage.
Energy Homeostasis: The body maintains a balance between energy intake (food) and energy expenditure (BMR, physical activity, thermogenesis).
Physiologic Mechanisms of Starvation and Satiety
Starvation – Key Mechanisms
Fuel shift: Body shifts from glucose → fat → protein for energy.
Stages:
0–24h: Glycogen → glucose.
1–3 days: Gluconeogenesis (amino acids, glycerol).
>3 days: Ketone bodies from fat → brain fuel.
>2 weeks: Protein breakdown → last resort.
Hormonal changes:
↓ Insulin, ↑ Glucagon, ↑ Cortisol, ↑ GH → promote fat use & glucose sparing.
Organ effects:
Liver: ketone production & gluconeogenesis.
Muscles: protein breakdown.
Brain: shifts to ketones to conserve protein.
Satiety – Key Mechanisms
Short-term signals:
Stomach stretch, CCK, PYY, and insulin signal fullness.
Long-term signals:
Leptin (from fat) and insulin inhibit hunger via hypothalamus.
Key brain areas:
Lateral hypothalamus = hunger center.
Ventromedial hypothalamus = satiety center.
Hunger signal: Ghrelin rises before meals to stimulate eating.
Temperature Regulation, Body Temperature and Isothermia
The human body maintains a nearly constant core temperature (isothermia) through complex neural, hormonal, and circulatory adjustments.
Normal core temperature ranges between 36°C–37.5°C, with slight variations due to factors such as circadian rhythms, physical activity, and environmental conditions.
Core Temperature: The temperature of deep tissues (brain, liver, heart, and muscles).
Skin Temperature: Varies significantly with environmental conditions and determines heat exchange.
Despite exposure to extreme temperatures (as low as 12.8°C or as high as 54.4°C in dry air), the body maintains core temperature within a narrow range, demonstrating the efficiency of its regulatory mechanisms
Mechanisms of Heat Production (Thermogenesis)
Basal Metabolic Rate (BMR): Energy expenditure at rest maintains body temperature.
Muscle Activity: Exercise and shivering thermogenesis significantly increase heat production.
Thyroid Hormones: Thyroxine (T4) and triiodothyronine (T3) stimulate metabolism, increasing heat production over weeks.
Sympathetic Stimulation (Chemical Thermogenesis): Epinephrine and norepinephrine promote heat production by increasing cellular metabolism
Mechanisms of Heat Loss
Radiation: Infrared heat emission to surroundings. ~60%
Conduction: Heat transfer via direct contact. ~3% to objects, ~15% to air
Convection: Heat carried away by moving air or water. % varies (e.g., wind increases loss)
Evaporation: Water loss via sweating & respiration. ~22% (increases with exercise)
Sweating is a primary cooling mechanism, regulated by sympathetic cholinergic nerves, which stimulate eccrine sweat glands
Neurophysiological Bases of Temperature Regulation
Hypothalamic Thermoregulatory Centers
Anterior Hypothalamus (Heat Dissipation Center)
Activated when the body is too hot.
Triggers vasodilation (increased skin blood flow) and sweating.
Posterior Hypothalamus (Heat Conservation Center)
Activated when the body is too cold.
Induces vasoconstriction, shivering, and increases metabolism
Temperature Sensors
Peripheral Thermoreceptors (Skin): Detect external temperature.
Central Thermoreceptors (Hypothalamus, Spinal Cord, Abdominal Organs): Detect core temperature.
Hyperthermia and Hypothermia
Hyperthermia (Excessive Heat Accumulation)
Occurs when heat production exceeds heat loss
Heat Exhaustion: Dehydration, excessive sweating, and fatigue.
Heat Stroke: Core temperature >40°C (104°F), altered consciousness, and multi-organ failure.
Sweating becomes ineffective due to dehydration.
Vasodilation leads to hypotension and circulatory collapse.
CNS dysfunction occurs due to enzyme denaturation.
Hypothermia (Excessive Heat Loss)
Occurs when core temperature falls below 35°C (95°F).
Mild (32–35°C / 89.6–95°F): Shivering, confusion, and slowed reflexes.
Severe (<32°C / 89.6°F): Loss of shivering, cardiac arrhythmias, and loss of consciousness.
Hypothalamic function declines as temperature drops.
Shivering ceases at core temperature <29°C (85°F).
Cold-induced vasodilation (final protective mechanism) delivers warm blood to prevent frostbite
Acclimatization
Acclimatization is the physiological adaptation to extreme temperatures over days to weeks.
Heat Acclimatization
Increased sweat production (earlier onset, more dilute).
Expanded plasma volume improves circulation.
Cardiovascular adaptations reduce strain.
Cold Acclimatization
Increased basal metabolic rate (BMR) due to thyroid hormone stimulation.
Greater shivering efficiency.
Enhanced brown adipose tissue (BAT) activity in infants and cold-adapted populations
Regulation of Body Temperature Within Exercise
During exercise, the body generates excessive heat (15-20 times resting levels).
Increased Sweating
Evaporative cooling becomes the primary heat loss mechanism.
Trained athletes sweat more efficiently (earlier onset, lower electrolyte loss).
Skin Blood Flow Redistribution
Vasodilation shunts blood to the skin, promoting heat dissipation.
However, excessive vasodilation can reduce blood supply to muscles, impairing performance.
Cardiovascular Adjustments
Increased heart rate and stroke volume maintain oxygen delivery despite increased skin perfusion.
Dehydration reduces plasma volume, impairing thermoregulation.
Core Temperature Set-Point Adjustment
During prolonged exercise, hypothalamic temperature threshold shifts higher.
This allows a higher operating temperature before sweating initiates