Neuroanatomy 7 -- the brainstem & cerebellum 1
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
The brainstem
Small structure — 8 cm length, 2-3 cm width
Direct continuation of the spinal cord (begins above C1 root exit)
Lies on the anterior border of the foramen magnum of the occipital bone and then on its clivus
Forms the floor of the 4th ventricle — on the top of the 4th ventricle there is the cerebellum —
Connected physically with the 3 brainstem subdivisions
3 subdivisions (caudal to rostral —)
Medulla oblongata
In continuity with the spinal cord — lies where anterior margen of foramen magnum opens, continuing with the pons and the midbrain
Pons
Midbrain/mesencephalon
Although it is small — contains huge # of vital pathways — thus, if damaged (especially caudally), we will die.
Moreover, all pathways connecting spinal cord & bran have to pass through the brain stem
Contains nuclei of cranial nerves
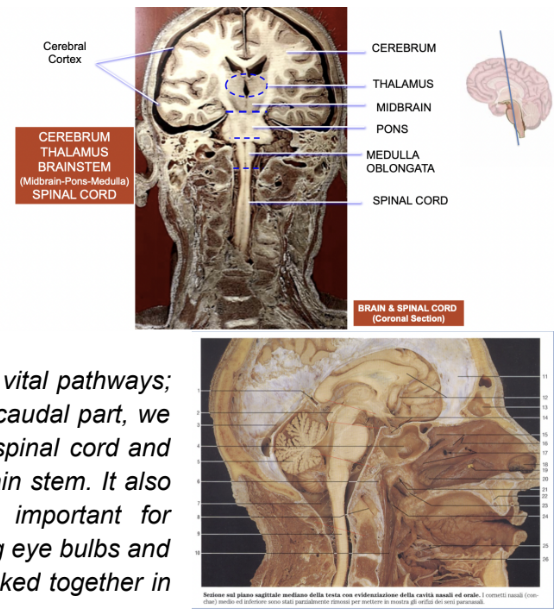
Medulla oblongata general division
Can be divided into a closed & opened part
Close portion —
Not part of the wall of the 4th ventricle
Open portion —
Undergoes the book-like opening and is part of the wall of the 4th ventricle
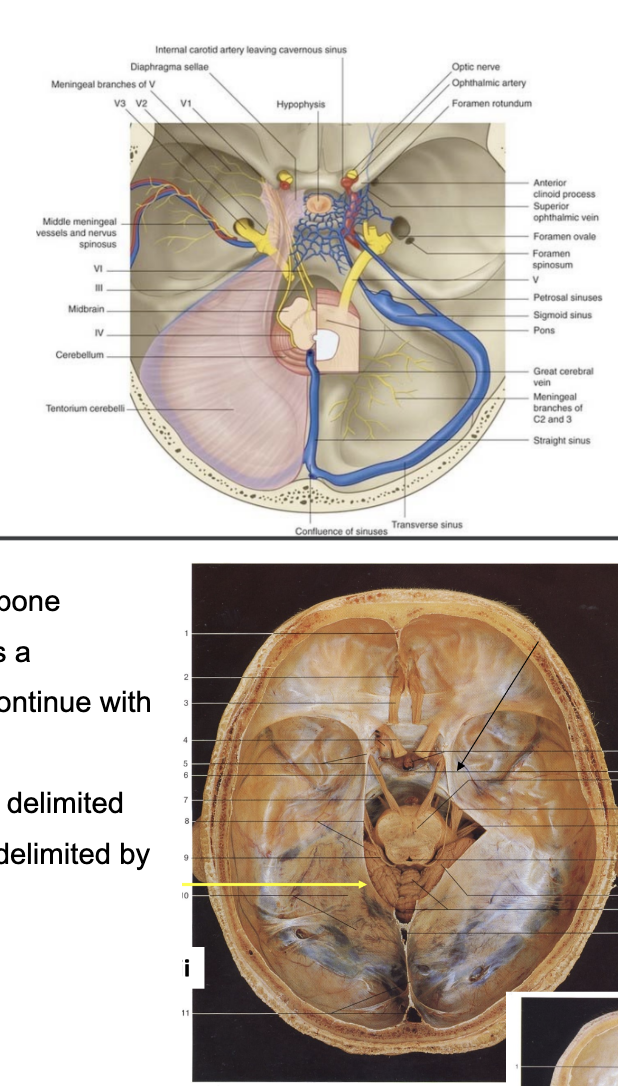
Brainstem’s position in posterior cranial fossa — revision of the endocranial fossae and relation with the base of the skull & foramina
As is lies on the anterior margin of the foramen magnum and on the clivus of the occipital bone — it lies on the base of the skull in the posterior cranial fossa (forming the floor of the 4th ventricle)
Every cranial nerve originating from the brainstem has to pass through the foramina characterizing the base of the skull
Base of skull division —
Can be divided into an anterior, middle, and posterior fossa
Surface of the brain structure that lies in the specific fossa has been colored with the same color of the fossa (image)
Blue —
Posterior cranial fossa — where brainstem & cerebllum lie
Due to its position, the nerves of the brainstem exit inthe different foramina
Oculomotor nerves & ophtalmic division of trigemnius use the superior orbital fissure
More caudally, there are the foramen ovale & foramen rotundum frm which maxillary & mandibular divisions of the trigeminal nerve pass
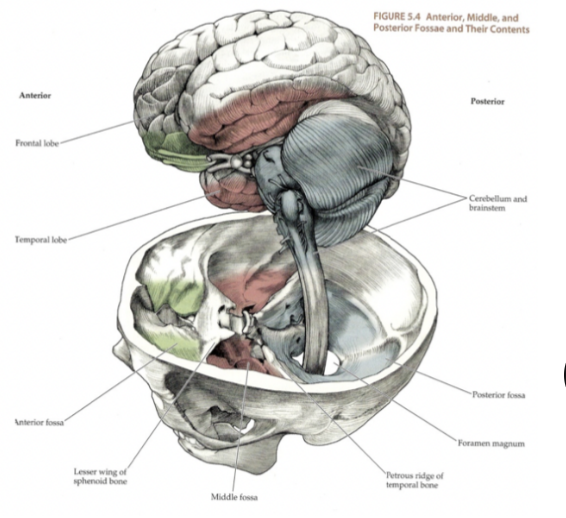
Fossae of base of skull image
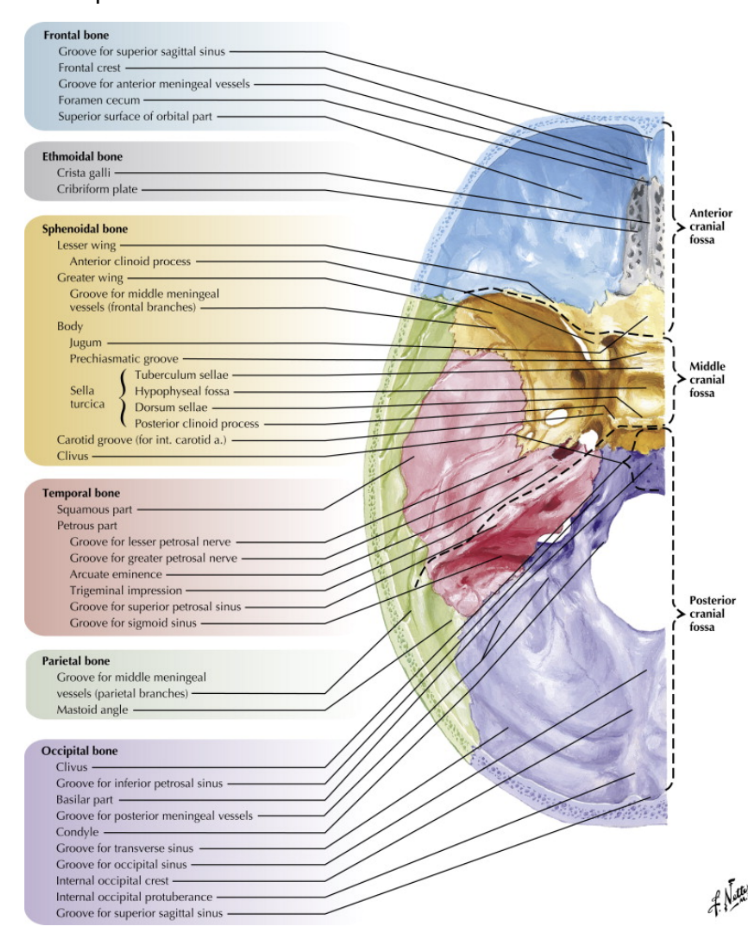
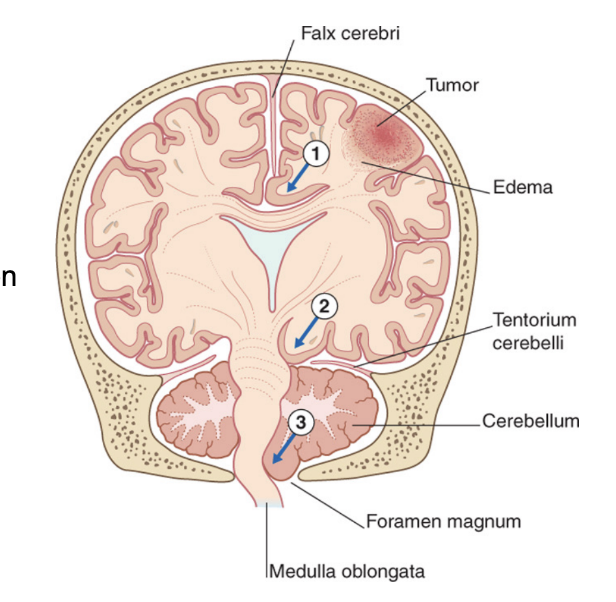
Insertions of the tentorium cerebelli –
The brainstem with the cerebellum is located in the posterior cranial fossa – a very “tight” compartment
Delimited inferiorly by the occipital bone
On left side – lamina of dura mater – the tentorium cerebelli
Attaches posteriorly to the transverse groove of the occipital bone & attaches on the surface of the petrous portion of the temporal bone. It continues its attachment anteriorly at the clinoid processes of the sphenoid bone
This attachment of the tentorium cerebelli leaves a passageway/opening so that the midbrain can continue with the diencephalon
*** Not only tight because posteriorly & inferiorly delimited by the bones – but also because superiorly it is delimited by the tentorium cerebelli.
Occipital lobe lies over the tenrotium cerebellum because the posterior fossa is occupied by the cerebellum & brainstem, meaning that the superior surface of the cerebellum is in communication with the occipital lobe via this lamina of dura mater called the tentorium cerebellum
The presence of the tentorium cerebellum divides the neurocranium into a supratentorial & infratentorial compartment –
Cerebral hemispheres – supratentorial
Brainstem & cerebellum – infratentorial
Supratentorial is divided into 2 parts (lobes) by the great cerebral falx
Clinical drop — Herniation – (occur after compression)
Structures of the posterior cranial fossa can herniate through the occipital foramen
/Foramen magnum – mainly cerebellar tonsils, patient may die immediately due to compression of medulla oblongata
Structures of the supratentorial compartment can herniate through the incisura tentorii
Usually herniation of the temporal lobe – problems with oculomotor nerve, parasympathetic fibers inhibited, only sympathetic fibers work – the ones involved in pupil dilation (3rd cranial nerve)
Supratentorial compartment —
The great cerebral falx attaches anteriorly to the frontal crest & to the cresta galli, then continues on the sagittal groove and attaches to the tentorium cerebelli on the midline
Characrerized by the great cerebral falx into 2 other subdivisions —
Right & left cerebral hemispheres
The falx cerebri attaches anteriorly to the crista galli, then on the squamous portion of the frontal bone, then to the parietal bone, then to the occipital bone, and then it attaches on the midline of the tentorium cerebelli, where we have formation of one of the venous sinuses of the skull
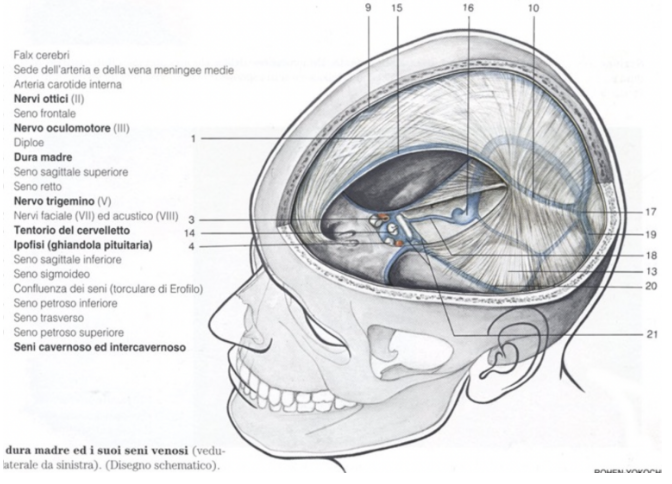
Meninges & headache –
Headache – the most common symptom in meningitis and is found in more than 80% of the patients
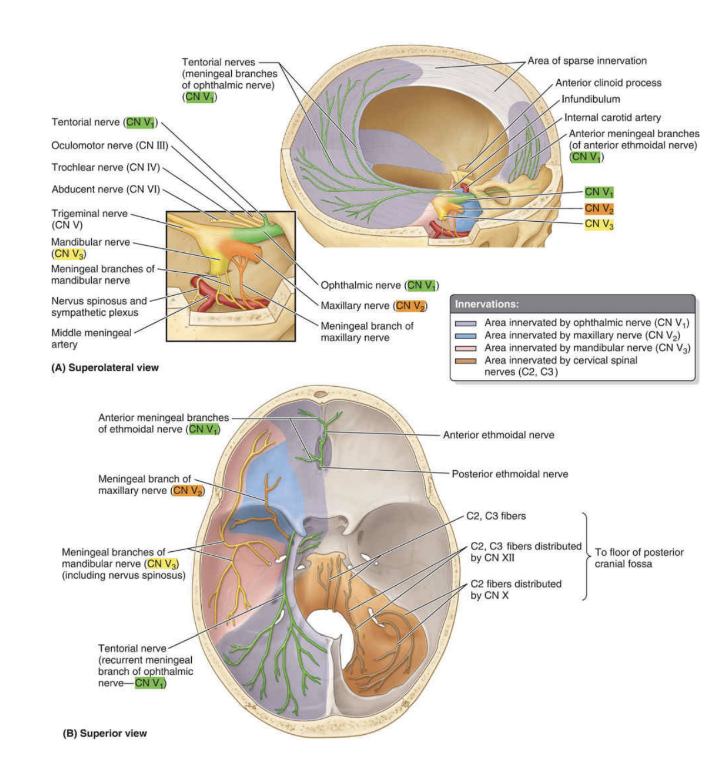
Meninges are innervated (mostly) by the 3 branches of the trigeminus –
The branch with the largest territory of innervation is the Ophthalmic division of the trigeminal – innervates all of the supratentorial compartment
Vasodilation of meningeal vessel in supratentorial compartment – usually leads to headache in frontal or parietal headache
Occipital nerves innervate infratentorial compartment
If we have vasodilation of meningeal vessel in the infratentorial compartment, – occipital spinal nerves
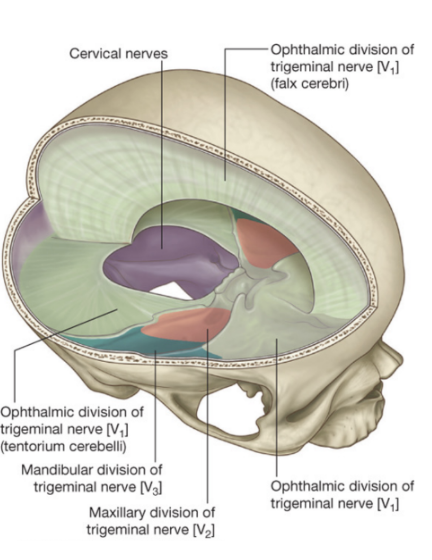
meninges & headache continuation image
Posterior cranial fossa – orange
The meninges of the infratentorial compartment (covering floor of posterior cranial fossa) are mostly innervated by sensory branches of the spinal nerves
Some of these branches reach directly as proper CII CIII branches –
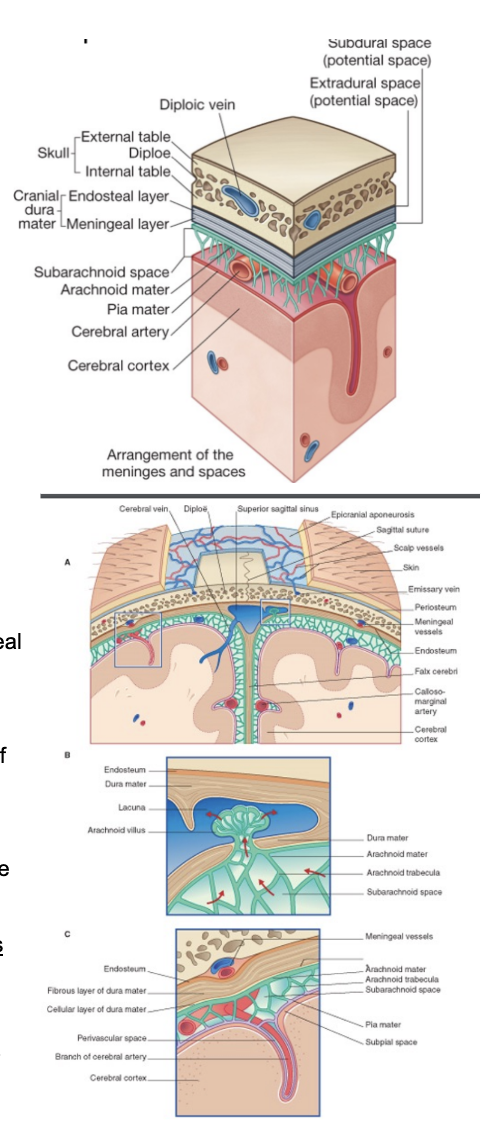
Arrangement of the meninges in the cranial cavity
In the spinal cord, between the meninges and the bone there was a space — at the level of the cranium, the epidural space is virtual
Attached to the surface of the brain, we can see the pia mater, then right above it, the subarachnoid space, full of trabeculae extending from the arachnoid mater to the pia mater
The dura mater —
Above/attached to the arachnoid mater — divided into 2 layers (separating where we have venous sinuses)
Meningeal layer
On the side of the other meninges
In regards to venous sinuses — Endosteal layer attached to the bone, meningeal detaches allowing blood to flow
Endosteal layer
On the side of the bone
Very attached to the bone, causing the epidural space to only be virtual — can become real if there is a pooling of blood between the endosteal layer and the skull
Some areas more easily detachable from the bone (typically below parietal bone & squamous portion of temporal bone – thus why easier to have a collection of blood here than in other places
Epidural layer can also be called extradural space
Subdural space —
Between the dura & the arachnoid — also a potential space
Can be opened by the separation of the arachnoid mater from the dura mater as a result of trauma, pathologic process, or the absence of cerebrospinal fluid as seen in a cadaver
Potential spaces — normally not there, but can become real if something starts to pool there (ex. due to haemorrhage)
Arachnoid —
A layer (arachnoid mater) with many strands of collagen fibers that extend towards the pia mater
The space between the trabeculae is called the subarachnoid space – contains cerebrospinal fluid, cerebral arteries , and meningeal vessels
Close to the venous sinuses, the arachnoid forms granulations (of Pacchioni) that extroflect inside the venous sinuses (especially the superior sagittal sinus) – and here, our CSF moves from the subarachnoid spaces into the venous sinuses and from there the general circulation
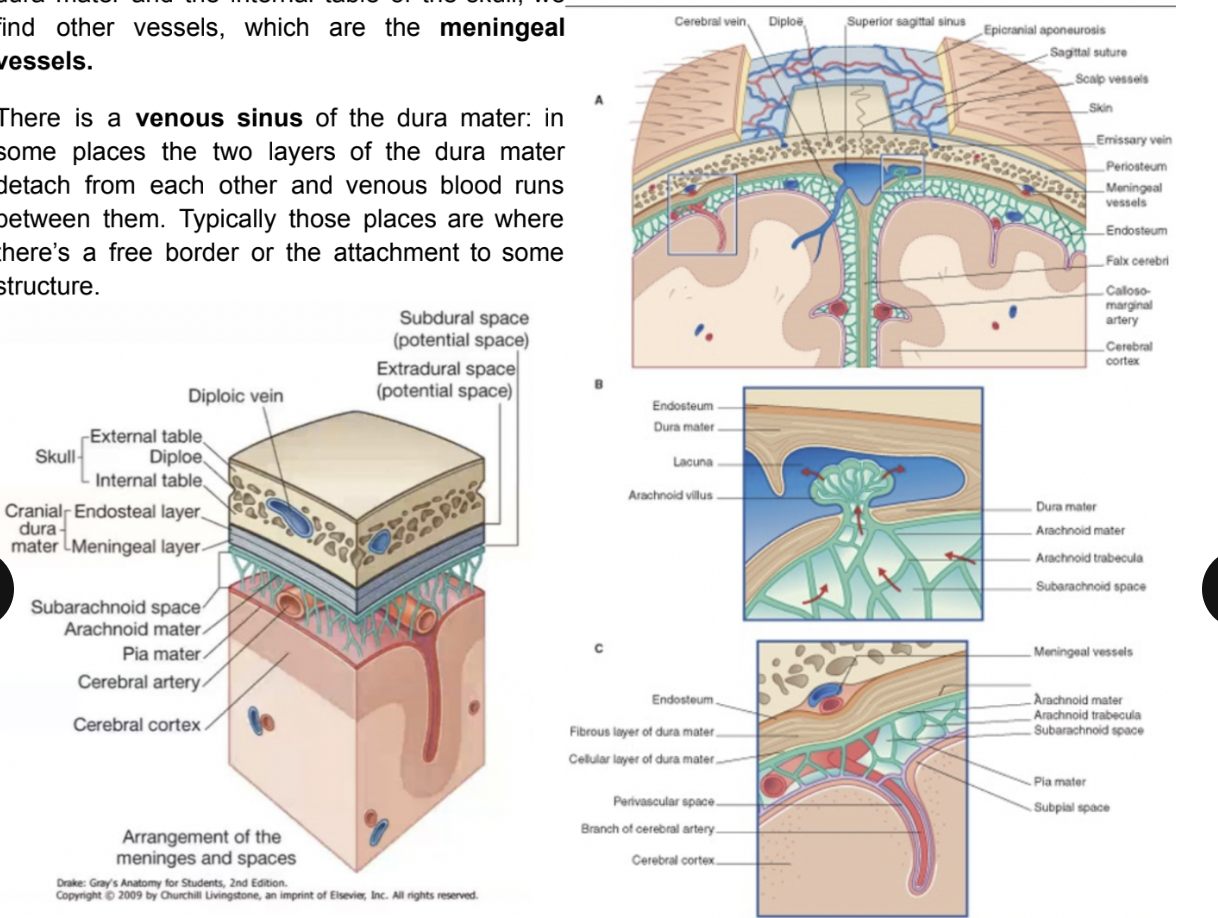
Meningeal blood supply (outline)
Looking in the subarachnoid space — we find the cerebral arteries
Between the endosteal layer of the dura mater and the internal table of the skull, we find other vessels, which are the meningeal vessels
There is a venous sinus of the dura mater —
In some places the 2 layers of the dura mater detach from each other & venous blood runs between them
Typically those places are where there’s a free border or the attachment to some structure
Granulation of pacchioni
Granulations formed by the arachnoid in some places that protrude inside the venous sinuses
Where the CSF is drained in the venous plexus — produced in the ventricular cavity
At the level of the 4thventricle the CSF enters in the subarachnoid spaces — the fluid is then reabsorbed in the venous system — the majority reabsorbed at the level of the Pacchioni’s granylations
Meningeal arteries
Embedded in the endosteum of the skull
Most important/largest — middle meningeal artery
Branch of the maxillary artery & enters into the skull via the foramen spinosum in the middle cranial fossa
Runs very close to the bone, over the inner surface of the parietal & temporal bones
Due to its proximity to the bone, in case of fracture of the skull, there is a high risk of damaging the middle meningeal artery — especially if the fracture is near the Pterion
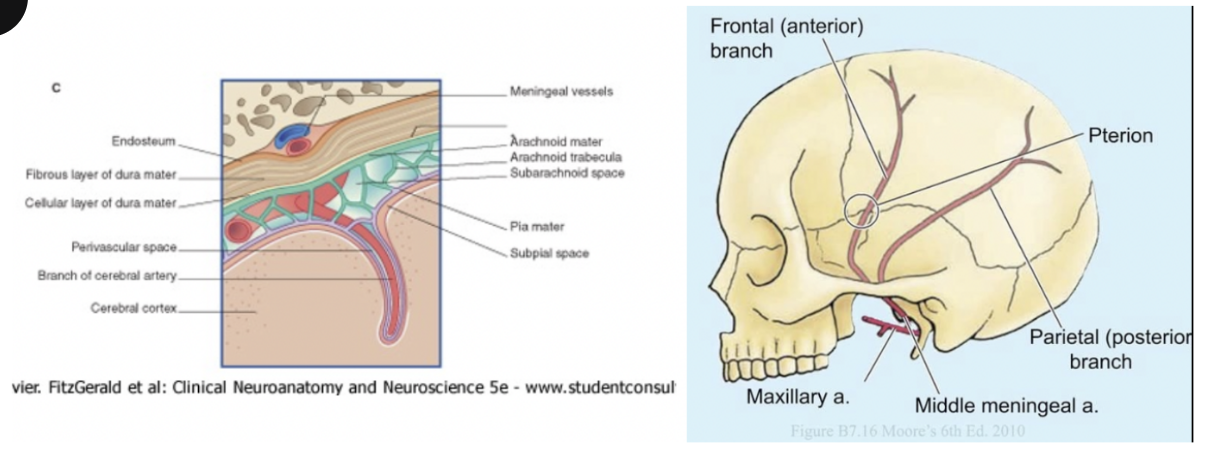
Clinical drop — Epidural hematoma
Epidural/extradural hematoma — between the bone & endosteal layer of the dura mater, caused by a blow to the side of the head (probably caused by a lesion in the middle meningeal artery)
Initial loss of consciousness due to the concussion
Trauma to reticular formation
May be followed by a lucid period of some hours (lucid interval)
Can be the time in which blood starts to pool, leading to compression of the brain
Onset of increasing drowsiness and headache
Due to the intracranial compression
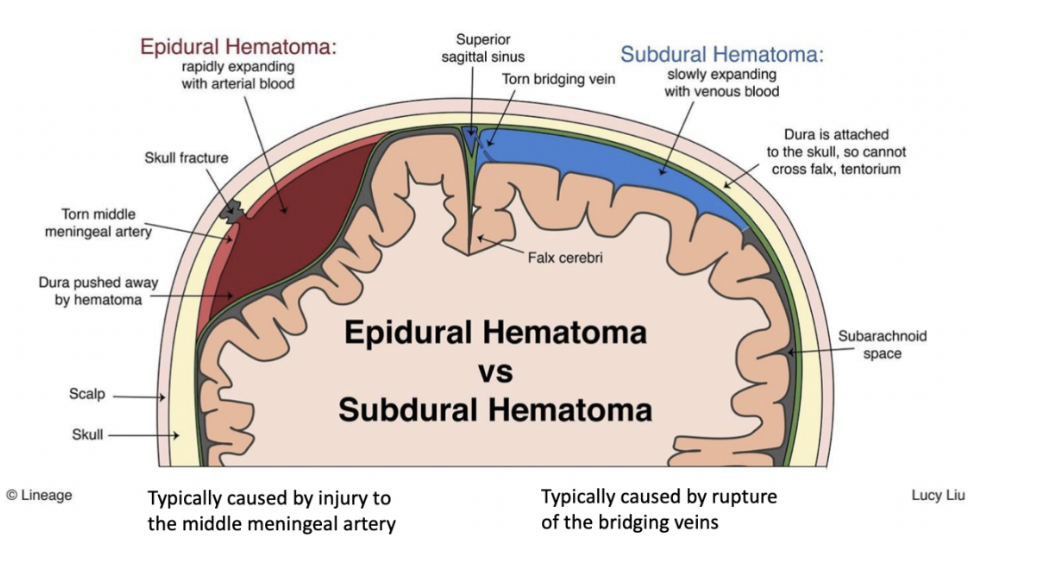
Subdural hematoma
Distinguished from a epidural hematoma — takes place between the innermost place of the dura mater & the arachnoid
In this case, the blood is typically venous & it comes from a fracture of the bridging vein
Bridging veins —
Drain the venous blood from the cerebral cortex into the superior sagittal sinus & in doing so they bridge the subdural space (subdural haemorrhages/hematomas)
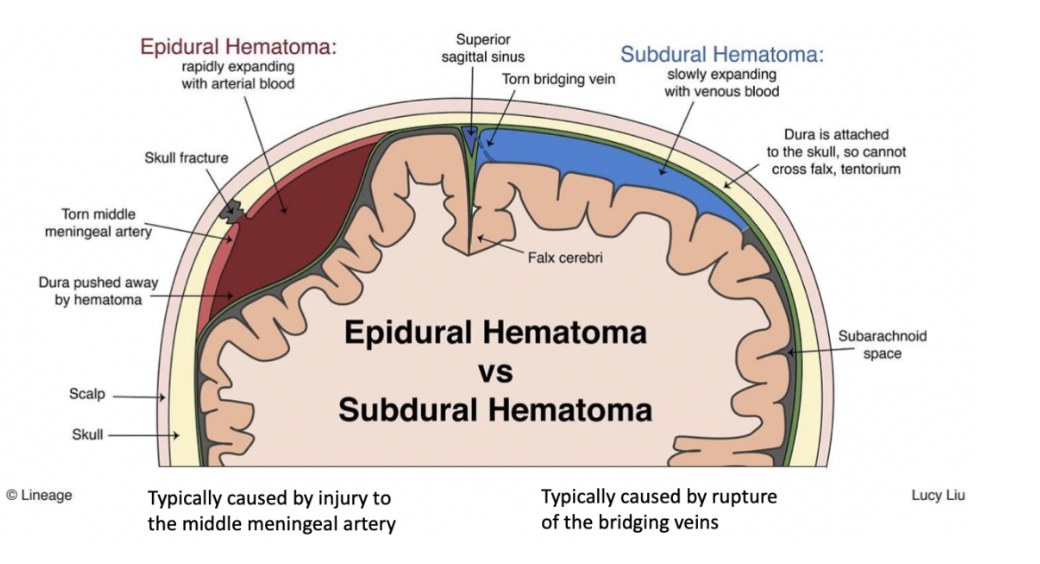
DO NOT CONFUSE BRIDGING VEINS WITH EMISSARY VEINS
Bridging veins — bridge the cerebral vessels in subarachnoid space to the venous sinuses in the dural space
Emissary veins — bridge veins of scalp to the sinuses
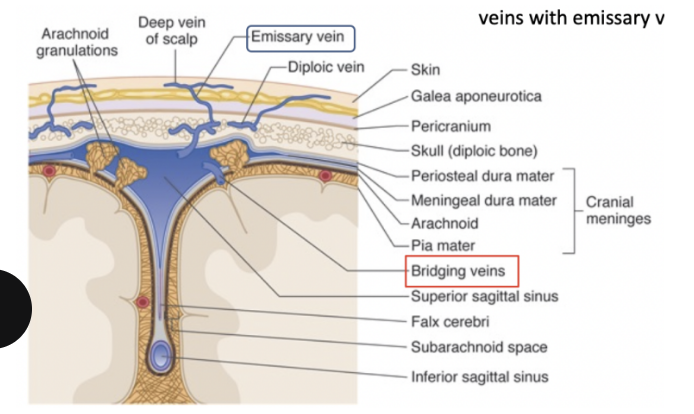
Types of cerebral haemorrhages
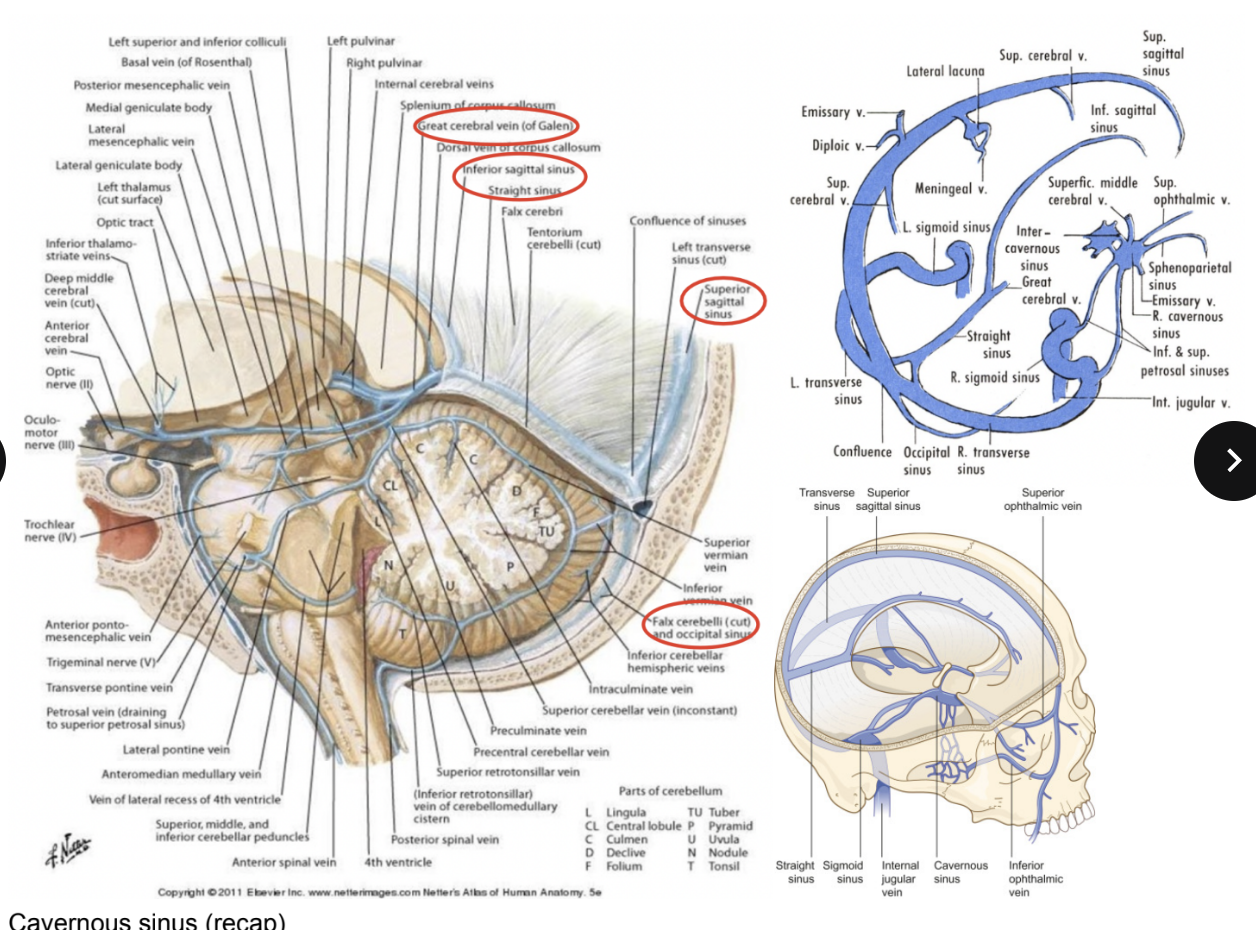
Venous sinuses of the dura mater
Form in between the endosteal & meningeal layer — lined by the endothelium — found where the dura mater attaches to the skull or along its free margins
Wall – made of dura mater lined by endothelium
Venous sinuses drain the deep & superficial veins of the brain into the sigmoid sinus into the internal jugular vein — Before final drainage they are in communication with outside via emissary veins
Superior sagittal sinus
Where the falx cerebri attaches to the skull
Inferior sagittal sinus —
At the level of the free margin of the falx cerebri
Straight sinus —
Where the tentorium attaches to each other, in front of the transverse groove, attaches in back to transverse
Transverse sinus — where the tentorium attaches to the transverse groove
Sigmoid sinus —
In the sigmoid groove which drains (from the transverse sinus) in the internal jugular vein, at the level of the jugular foramen
Superior & inferior petrous sinuses — continue forward from sigmoid sinus along petrous portion of temporal bone, connecting to cavernous sinus
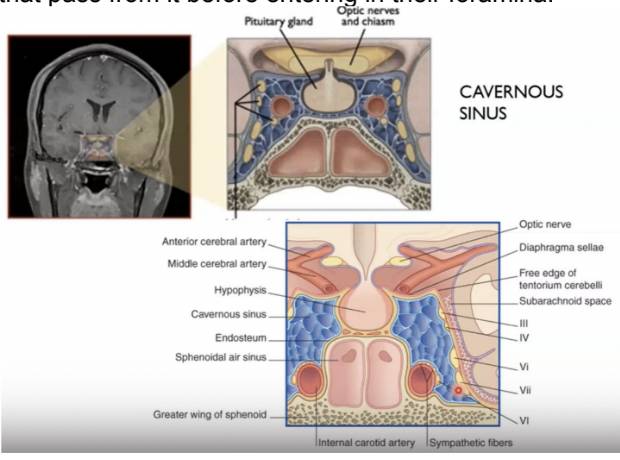
Cavernous sinus —
On the sides of the sella turcica
Occipital sinus —
Where there is a lamina of dura mater that inserts in between the 2 cerebellar hemispheres (cerebellar falx or falx cerebri) and on the other part, attaches on the inferior part of the straight crest (going down from transverse sinus)
Confluence of the sinuses —
Where the transverse, occipital, straight, & superior sagittal sinuses come together
Cavernous sinus (recap)
Found on the side of the body of the sphenoid bone —
Made by a plexus of veins delimited by dura mater
Contains many relavent strucutrs passing from it before entering in their foramina
Occlusion, inflammation, or thrombosis of the cavernous sinus —
Very commonly the nerves running in it are affected aswell — causing paralysis of the eye muscles (cavernous sinus syndrome)
CN 3, 4, V1, V2, & 6
Thrombosis — caused by injuries in the face (esp. danger triangle)
Inflammation of this area, even if not treated, can be transported into the cavernous sinus, where it can lead to inflammation or thrombosis and then it can spread to other sinuses
Initially it would give rise to symptoms related to the paralysis of the muscles of the eyes due to the inflammation of the nerves that pass in the cavernous sinus `
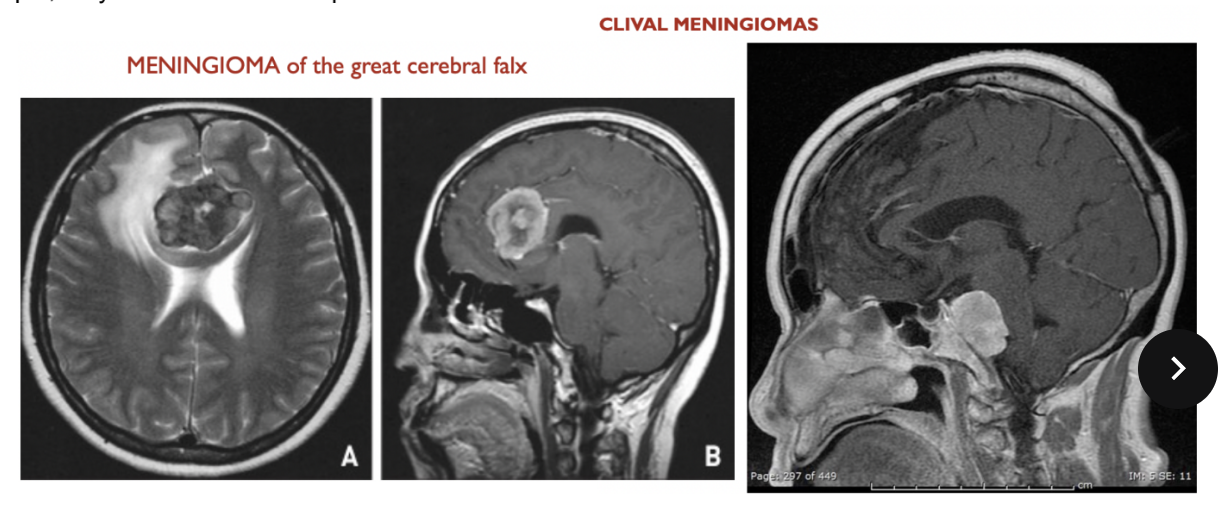
Meningiomas
In the Us comprise about 32% of all primary intracranial tumours, with an annual incidence of 5.2 per 100000 population
Twice as common i women, with regional variation
Patients with multiple meningiomeas generally comprise less than 10% of cases
Most are beneign
However, while they grow, can compress nervous tissue
In generall, atypical & anaplastic meningiomas comprimse less than 10%
Can be meningiomas of the great cerebrl falx, clival meningiomas, etc.
Clival meningiomas are at the level of the clivus of the occipital bone, which can cause problems for the brainstem
Meningiomas are often benign growths, but depending on their position can cause damage (ex. compressing brain structures)
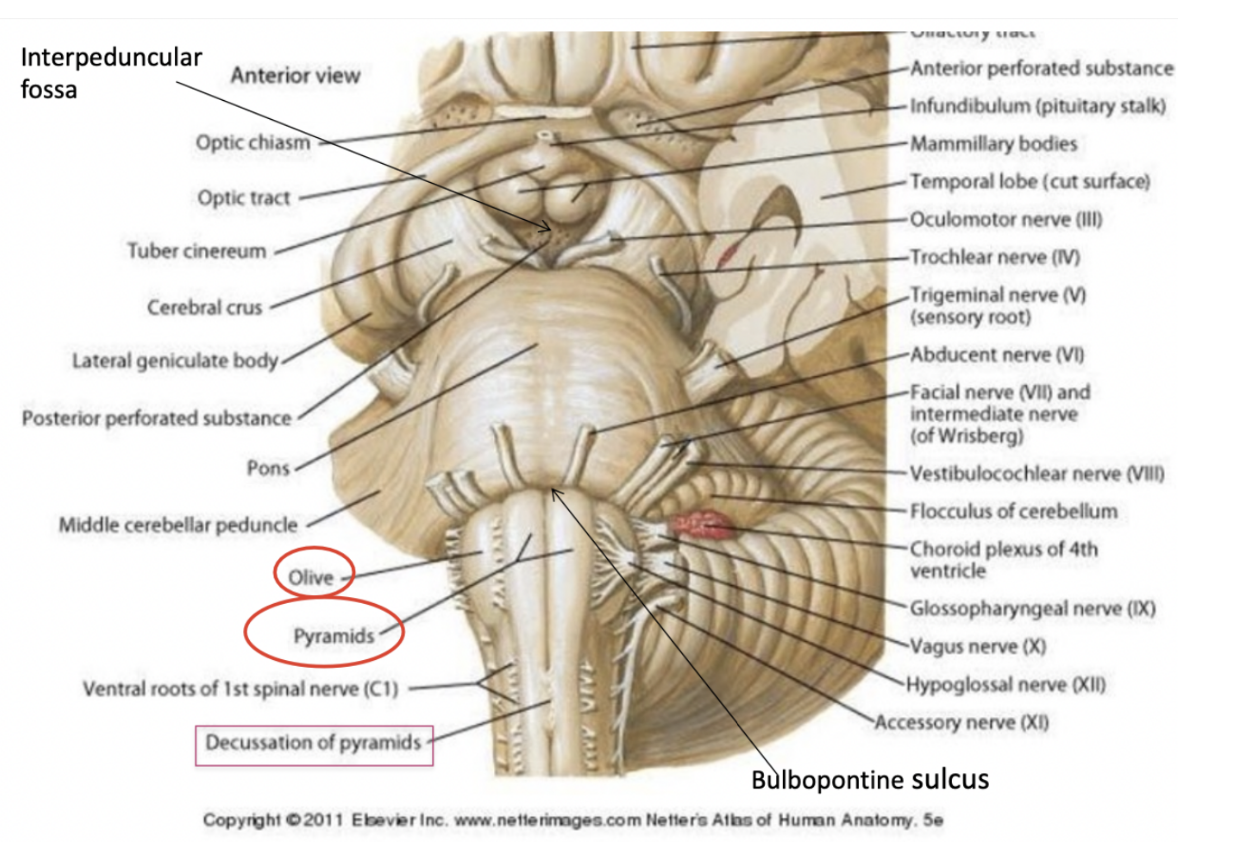
Gross anatomy of the brainstem–
Not segmented
Nerves do not emerge in the same position – do not come out organized such as in the spinal cord (ventral & dorsal root, anterolateral & posterolateral sulci, etc)
On the surface, can observe –
Grooves, fissures, peduncles, bulges, elevations, depressions
Most cranial nerves that originate from the brainstem exit venterolaterally
Ventral side of the brainstem —
In caudal → rostral direction – starting with medulla oblongata
Close to the midline/anterior median fissure, we see two large structures called the pyramids of the medulla oblongata
These 2 elevations correspond to the corticospinal tract –
all fibers coming from the cortex will come down to the medulla oblongata & are collected together to form the medullary pyramids
Caudally, there is a decussation of pyramids – meeting together
This is where 90% of the fibres of the pyramidal tract will cross on the other side - the fibres of the lateral corticospinal tract become contralateral.
At the limit between the brainstem and spinal cord,
On right & left of pyramids – large ovoidal structure – olive
Correspond to a very important nuclear complex of the medulla oblongata – inferior olivary nucleus/complex, that give rise to the olive
Passageway anteriorly to the olive is marked by a groove that is a continuation of the anterolateral groove
Upper portion of medulla oblongata is marked by the bulbopontine sulcus – marks the passageway between the medulla oblongata & the pons
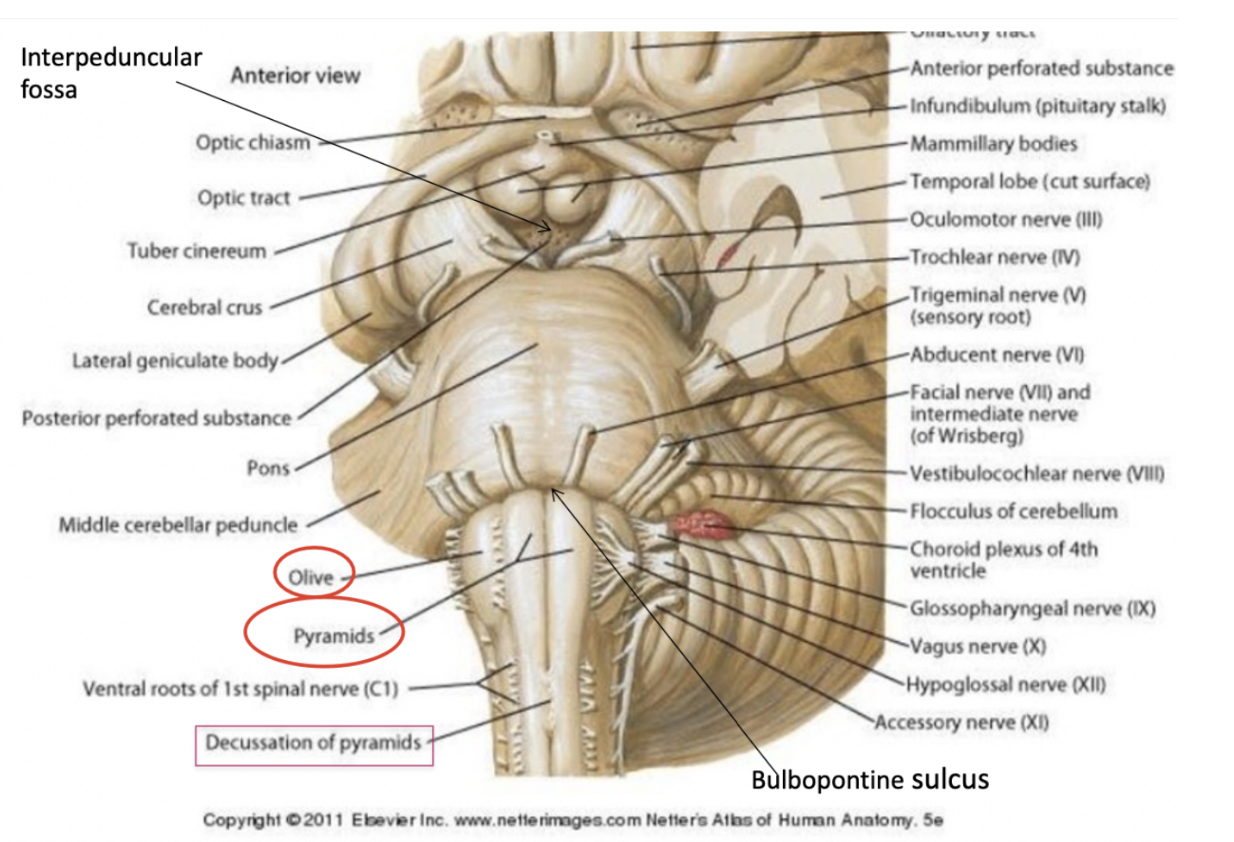
Emergence/exit of cranial nerves (ventral surface) –
Close to the midline – emergence of the hypoglossus (CN 12) – motor (innervates muscle of branchial or paraxial mesoderm origin (emerges between olive & triangle)
The 11th CN – caudal to the exit of hypoglossus (exception – everything else dorsal)
Behind the olive, in the retroolivary groove, the emergence of the glossopharyngeal nerve, the vagus nerve, and some of the roots of the accessory nerves can be found (9, 10, & some 11)
Then, in the bulbupontine sulcus, there is also the emergence of the abduchens (CN 6) (nerve innervating occulomotion – motor)
More laterally in the bulbupontine sulcus (3 things either side, starting medially )- facial nerve proper (7) (motor component), intermediate component of the facial nerve (7) (visceromotor & sensory component), and the vestibulocochlear nerve (VIII)
Largest root – sensory root of the trigemius - Trigeminal nerve (V), while thinner root (on the left side) – contains the motor root — comes out of sides of pons
Infundibulum & mammillary bodies – part of the hypothalamus
Close to the midline, in the interpeduncular fossa (enlargement of the subarachnoid space) – exit of oculomotor nerves
3 nerves of oculomotion in cavernous sinus & superior orbital fissure – then goes down to follow others in orbital cavity – trochlear nerve
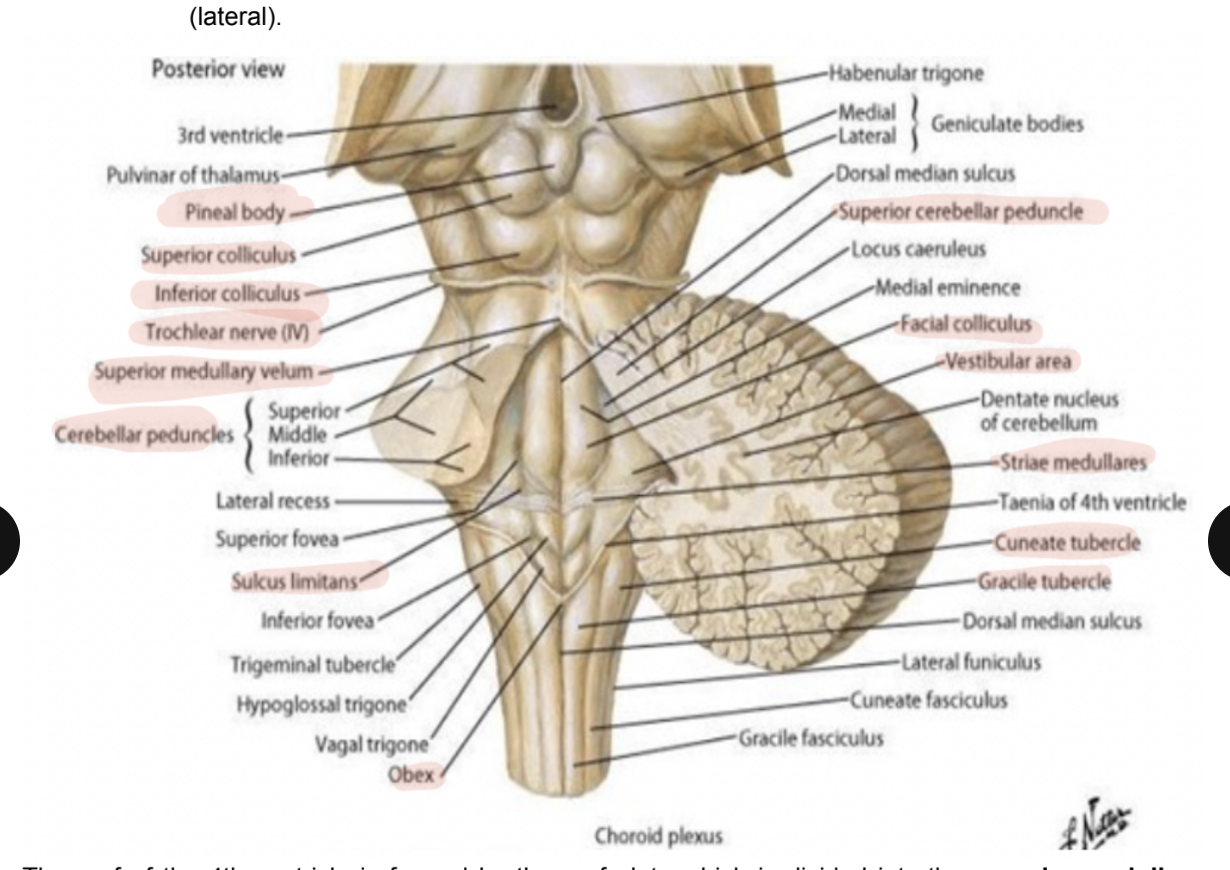
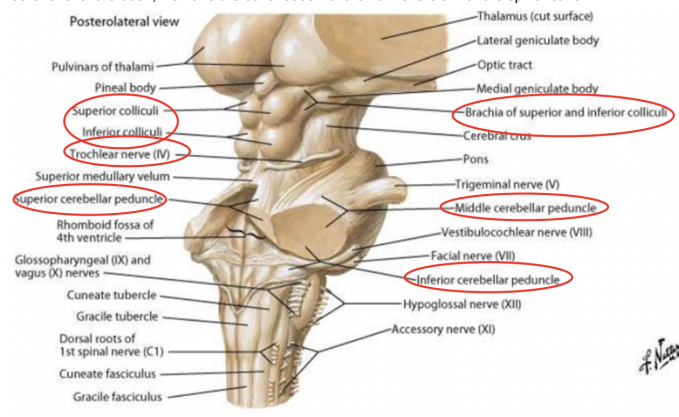
Dorsal side of the brainstem
To see it, cerebellum (covering most of 4th ventricle & pons) has to be removed
Rhomboidal fossa — corresponds to floor of 4th ventricle — here we can recognize —
Inferior triangle —
Representing the open portion of the medulla, due to the booklike opening of the mesencephalic vesicle
Superior triangle —
Formed by the pons
Non-smooth surface — various protruberances & grooves including the —
Facial colliculus, medial eminence, lateral recess, sulcus limitans, trigeminal tubercle, hypoglossal trigone, striae medullaris, etc
All of these structures represent the fact that there are some structures evident to the point of protruding from the lfoor of the fourth ventricle in the tegmentum of the medulla & pons
Vestibular area is more lateral and corresponds to where we find the vestibular nuclei
The facial colliculus is more on the midline & we find the motor nucleus of the facial nerve and the fibers of the abducens on their way to exit from the brainstem & protrude below the surface of the floor of the 4th ventricle
The sulcus limitans — between the cranial nerve motor nuclei (medial) from the sensory nuclei (lateral)
Roof of the 4th ventricle —
Formed by the roof plate which is divided into the superior & inferior medullary velum
From the dorsal side of the dorsal view — 3 cerebellar peduncles
Caudally to the 4th ventricle, on the medulla oblongate we can recognize the gracile tubercle & cuneate tubercle
Rostral to the 4th ventricle, we find the territory of the midbrain
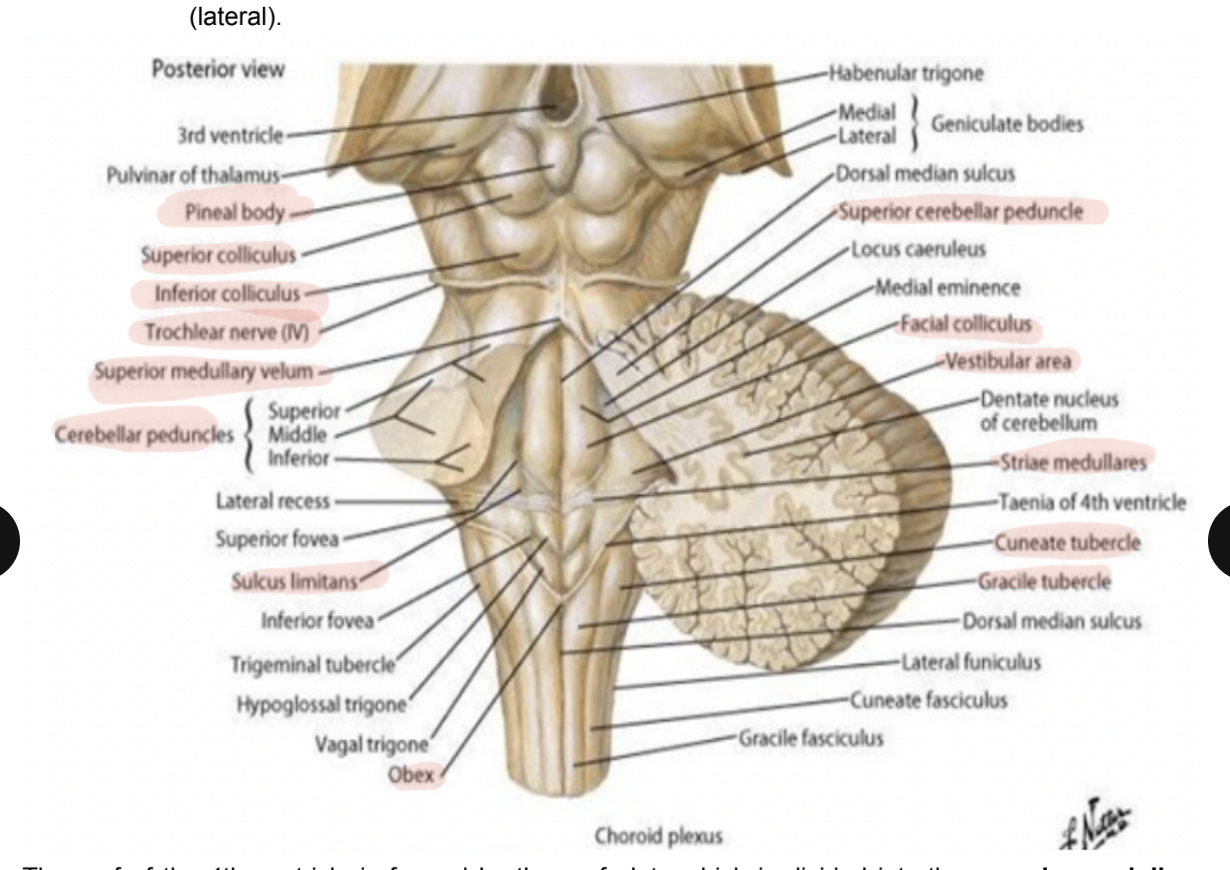
Cerebellar peduncles
Visible from the dorsal side of the dorsal view
Contain the axons putting the cerebellum in communication with each zone of the brainstem
With both afferent & efferent fibers
Divided into —
Superior peduncle — connects to the midbrain
Middle peduncle — connects to the pons
Inferior peduncle — connects to the medulla
The 3 converge to then enter the cerebellum
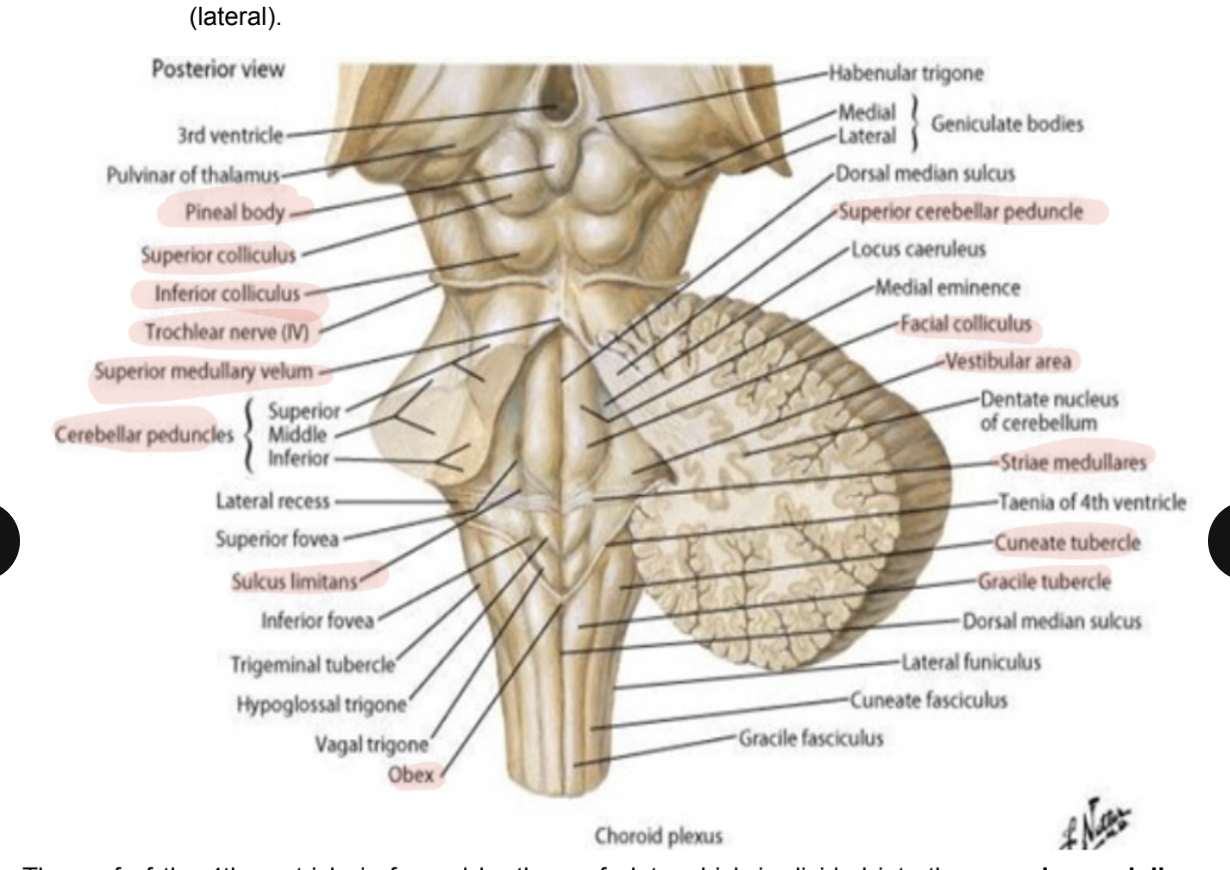
Tubercles of medulla oblongata
The gracile tubercle & the cuneate tubercle
In these tubercles, we find the gracilis nucles & the nucleus cuneatus — part of the closed portion of the medulla
The white matter of the spinal cord forms the dorsal column, which can be divided into a gracile & cuneate fasciculus, which will stop at the level of the nuclei, forming the tubercles
The obex represents the place where the ependymal canal communicates with the 4th ventricle
(At the beginning of the open portion of the 4th ventricle)
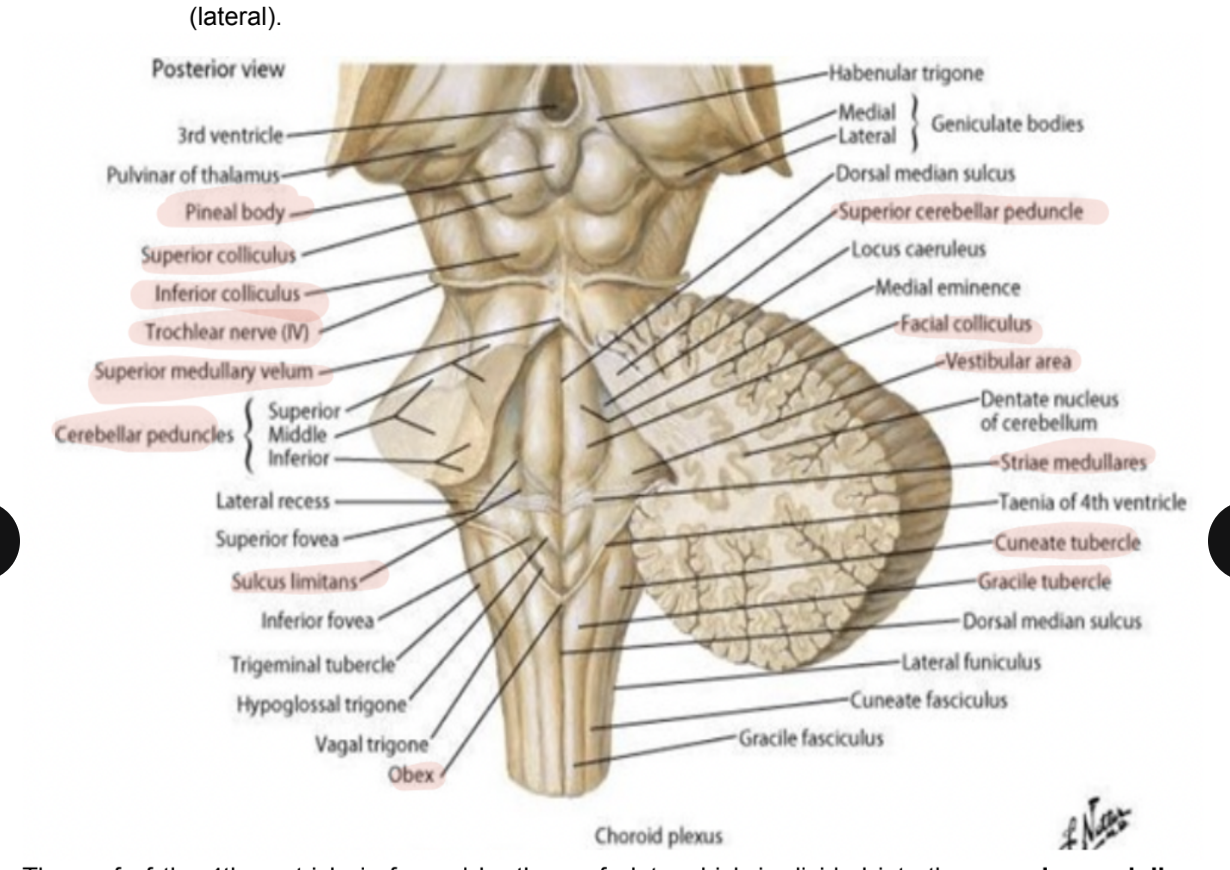
Midbrain territory
Rostral to the 4th ventricle — did not undergo the book-like opening
Characterised dorsally by the lamina quadrigemina (or tectum) (tectum = roof, tegmentum = floor of midbrain)
Characterised by the presence of 4 colliculi —
2 inferior & 2 superior
In between the superior colliculi we find the pineal gland
Part of the diencephalon
Between the tectum & the superior cerebellar peduncle (or superior medullar velum), we find the exit of the trochelar nerve (IV)
Runs along the superior medullary velum & crosses to the ventral surface
Roof of 4th ventricle & choroid plexus
To observe roof of 4th ventricle — sagittal view
Cerebellum lies over the roof, which consists of — 2 veli — thin structures made of thin transparent layer of white matter —
Superior medullary velum
Inferior medullary velum
Presence of choroid plexus — region enriched with capillaries pushing inside the ventricular cavities
At the level of the choroid plexus, we have filtration of blood inside the ventricular cavity to form CSF
The 4th ventricle communicated with the subarachnoid space through 3 openings
In the choroid plexus there are fenestrated capillaries to allow passage of blood components into the space separating the capillaries from the epithelial (ependymal) cells, then to a process of filtration to produce CSF
At the level of the choroid plexus — blood-CSF barrier
Endothelial & ependymal cells are part of a barrier that separates blood from the CSF produced in the ventricular cavity
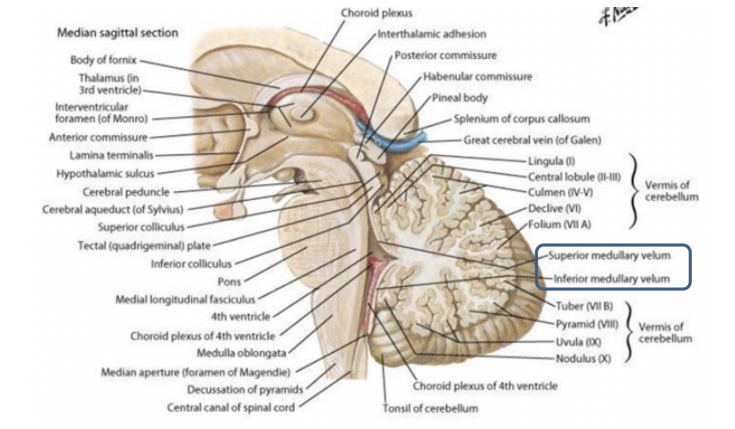
Openings through which the 4th ventricle communicates with the subarachnoid space
2 lateral — foramina of Luschka
At the level of the lateral recesses of the 4th ventricle
One median aperture — posteriorly — foramen of Magendie
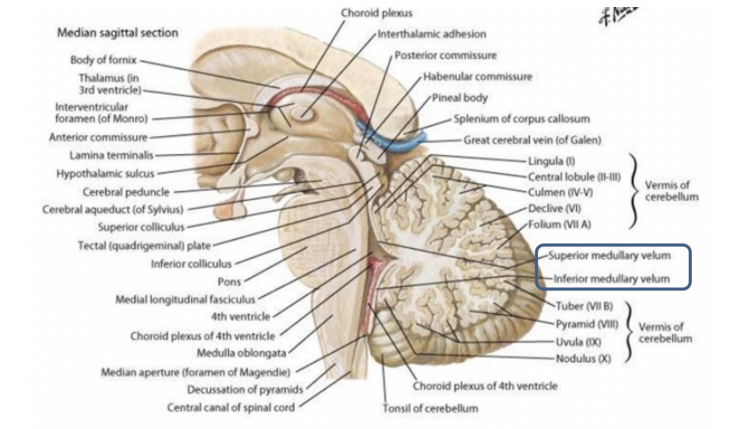
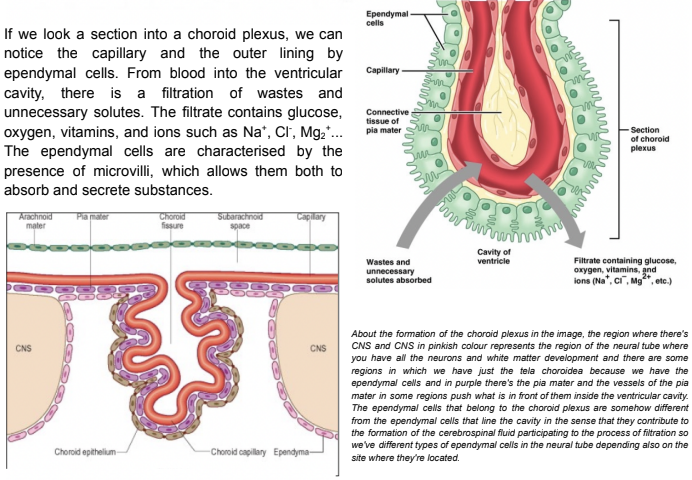
Image of blood CSF barrier
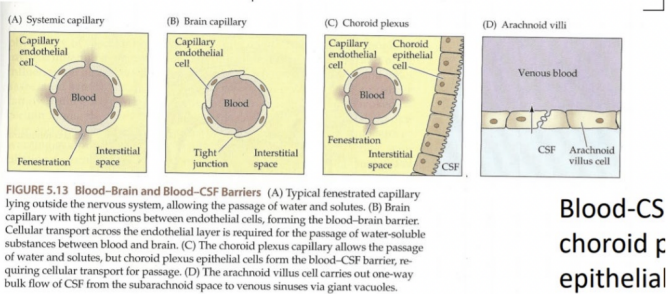
Looking into a section of a choroid plexus — image analysis
Notice the capillary and the outer lining by ependymal cells
From blood into the ventricular cavity, there is a filtration of wastes and unneccesary solutes —
Filtrate contains glucose, O2, vitamens, & ions (Na+, Cl-, Mg2+..)
Ependymal cells are characterized by microvilli —
Allows them to both absorb & secrete substances
Lateral side of the brainstem
Can notice most of the structures that we could from the dorsal side —
Check other flashcard
NOT SURE IF BELOW IS ALSO VISIBLE FROM DORSAL — CHECK
Superior & inferior coliculi have brachia conjuctiva — bundles of white matter connecting them to the diencephalon
Superior brachia conjuctiva —
Connects superior colliculus t the lateral geniculate body/nucleus of the diencephalon (major auditory nucleus)
Inferior brachia conjuctiva —
Connects inferior coliculus with the medial geniculate nucleus of the diencephalon (key to the visual pathway)
Thus, the tectum has to do with the acoustic & visual pathways
Some cranial nerves (facial, vestibulocochlear, & olive & rootlets emerging dorsally & ventrally to it) exit
Accessory nerve (IX) — tricky — classified as cranial nerve due to its exit from the jugular foramen and then distribution to its destinations, but some of the fibers originate from the medulla oblongata, while most of them originate from the cervical segment of the spinal cord
At the level of the obex, we have the continuation of the 4th ventricle with the spinal canal
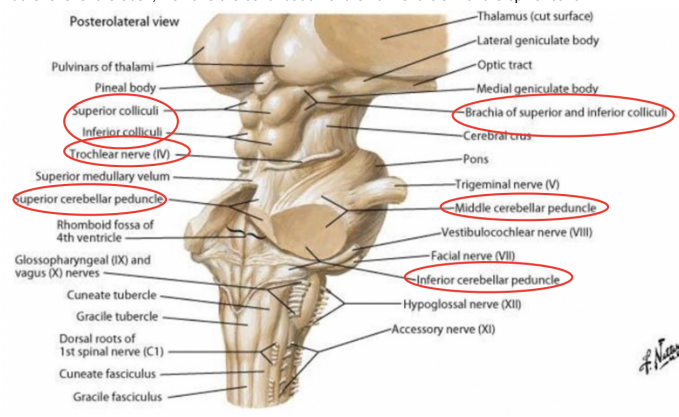
Structures we can see from the lateral side that we also can from the dorsal side of the brainstem
Cerebellar peduncles (esp. middle p.)
Exit of 4th cranial nerve — trochlear (originates caudally to the inferior coliculi
Fibers exiting from the tegmentum of the midbrain enter in the superior medullary velum, cross, & exit from it
The 2 trochlear nerves contain the fibers coming from the contralateral motor nucleus of the trochlear nerve — don’t remain dorsal, but embrace on the side of the midbrain, continuing ventrally & then anteriorly
The lamina quadrigemina
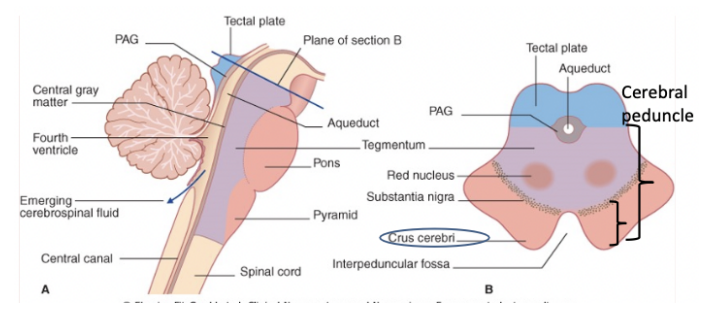
Basic organization of the brainstem
Can be divided into 3 “longitudinal strips” — 2 of which are present everywhere & one of which is only present in the midbrain
Ventral region of the brainstem — base (or foot), dorsal to where we find the tegmentum
In midbrain only — tectum — involved in auditory & visual pathways
Cerebral peduncle
(B) in the image
Refers to the midbrain — some authors state it only consists of the base (in the midbrain), and for others also the tegmentum
Anterior portions of the cerebral peduncle (corresponding to base of midbrain) are also called the crus cerebri, in between which there is the interpeduncular fossa
This fossa contains enlargement of the subarachnoid space — interpeduncular subaachnoid space
In the midbrain we find the Aqueduct of Silvius
Since it doesn’t undergo the book-like opening
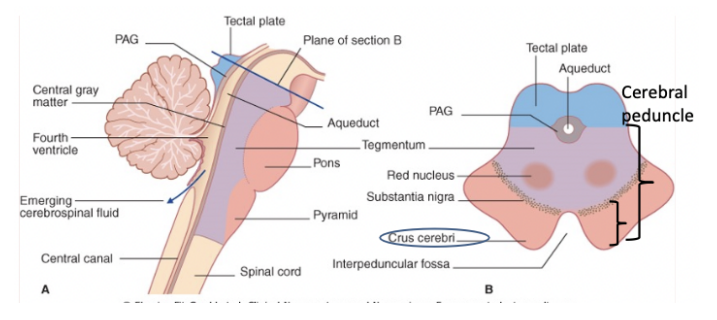
Base of the brainstem
The phylogenetically newest part
Only made of white matter & the newest descending pathways —
The corticopontine cerebellar tract & the pyramidal tract
Exception is in the pons — specifically where in addition to the white matter we find the basilar nuclei of the pons (C)

Tegmentum of the brainstem
We find the rest — the old descending pathways, ascending pathways, nuclei of the cranial nerves and the specific nuclei of the brainstem
Contains the reticular formation —
Important because it is both the oldest part of the brainstem but also contains all our vital centers
Here we can also find the cranial nerve nuclei, the specific nuclei, the sensory & motor pathways (except the pyramidal & corticopontine tracts)
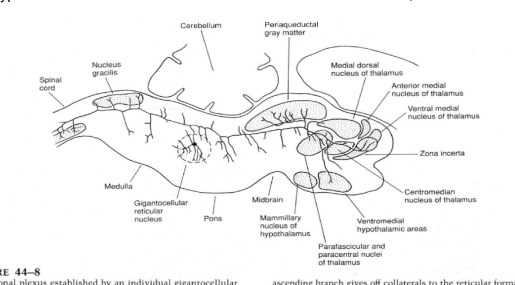
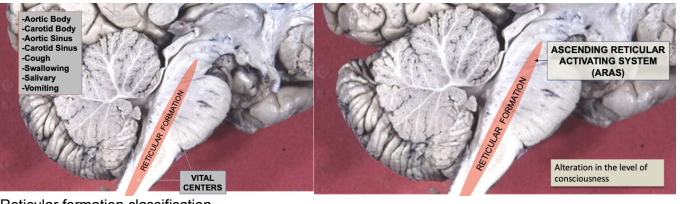
Reticular formation
Oldest part of the brain — diffuse, multisynaptic, netlike meshwork (reticulum) of widely interconnected neurons in the tegmentum
Due to it being the phylogenetically oldest, — functions to support ex. survival of the individual — has to do with the vital centers of the brainstem
Involved in nearly every aspect of brain function including homeostasis, consciousness, arousal (waking up), pain, primitive motor control (descending motor pathways from RF), muscle tone (function of final reticular descending pathway & vestibulus final descending pathway) and behavioral mechanisms
Vital centers are located in the medulla & pons and control cardiovascular, respiratory, and other homeostatic mechanisms — lesions here are fatal
Ex. of reticular formation mediated reflexes:
Aortic body, carotid body, aortic sinus, carotid.sinus, cough, swallowing, salivary, & vomiting
Most rostral part of the reticular formation (in midbrain) — involved in beforementioned mechanisms (ex. pain control) — but not respiration or cardiovascular control — due to this part mostly concerning bombarding of cerebral cortex with a lot of excitatory inputs —
Midbrain reticular formation gives rise to a tonic ascending barrage of diffuse, non-specific sensory data calld the ARAS (ascending reticular activating system)
Reticular formation extends in the midbrain, pons, medulla, & also cervical segment of spinal cord
ARAS
Ascending reticular activating system — tonic ascending barrage of diffuse, non-specific sensory data
Acting as a batter, it stimulates the cerebral cortex & maintains the conscious state —
Midbrain lesions of the ARAs result in coma, incomplete lesions may result in stupr
Called ascending because it projects rostrally, reticular because comes from RF, & activating because it activates the cerebral cortex
Linked to the sleep cycle & circadian cycles
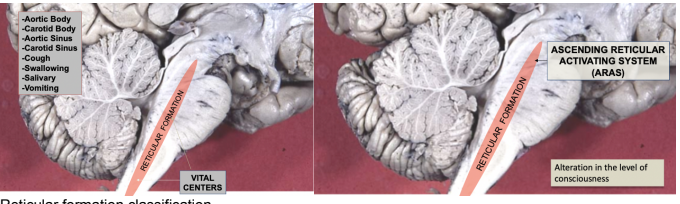
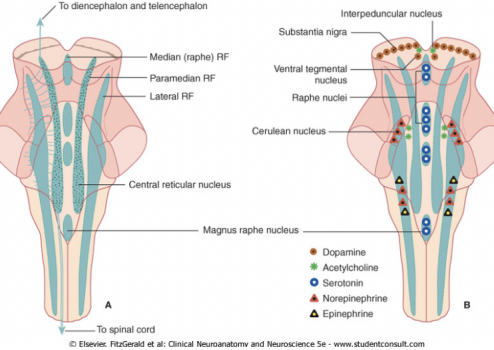
Reticular formation classification
A cytoarchitectonic & a neurochemical division —
Cytoarchitectonic division of reticular formation —
Based on cytological characteristics (shape & size) of neurons — 3 regions
Median region (raphe component) —
Contains raphe nuclei & a region where fibers exchange between sides
Medial/paramedian region —
Lateral region —
Extends in the cervical segment of the spinal cord
Basically if we go from midline of brainstem (medial → lateral) we find 3 subdivisions with cells differing in size & shape
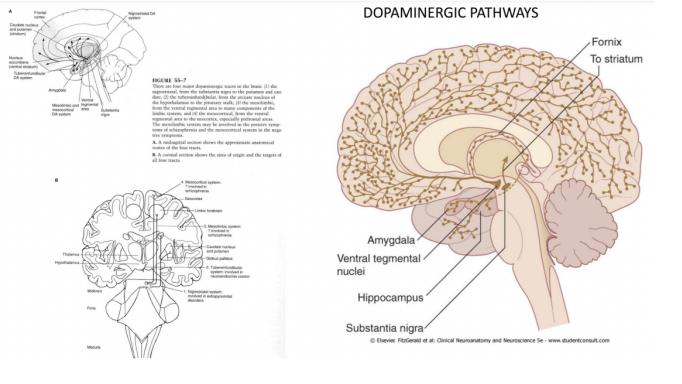
Neurochemical division of reticular formation —
Characterized by the type of neurotransmitter used — divisions according to production of dopamine, serotonin, acetylcholine, epinepherine & norepinepherine
A dopaminergic region (red) mostly located in the midprain — produces dopamine
Substantia nigra — (in midbrain) most important dopaminergic center of our brain
Dopamine — important (ex. Parkinson disease occurs because substantia nigra isn’t producing dopamine anymore, leading to motor, behavioural, and cognitive problems
Seratoninergic division (coloured in blue) — formed by the nuclei closer to the midline — seratoninergic centers can be found in the midbrain, as well as in pons & in the medulla — regions involved in several functions —
Ex. pain control, behavioral & homeostatic mechanisms, etc.
Chlonergic’s division’s nuclei (green) — mostly located in the pons
Noradrenergic (ex. nucleus cerulea) and adrenergic divisions (red & black)
Neurochemical division — important from a neuropsychiatrist pov — connected with mood, thought, consiousness etc. disorders due to arrangement of the neurotransmission of the reticular formation
For this reason many drugs act upon the reticular formation
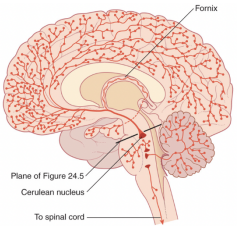
Noradrenergic pathways
Some of the noradrenergic nuclei project rostrally (ex. →cerebral cortex), some caudally (spinal cord), some to the cerebellum (pre-cerebellar nuclei)
Noradrenergic pathways — involved in —
Modulation of attention
Attention deficit disorders respond to noradrenergic drugs
Sleep wake cycle modulation
Mood modulation & consequently involved in mood disorders
Lots of neuropsychiatric disorders are related to problems in the reticular formation
In pain modulation
Seratoninergic pathways —
Involved in several psychiatric syndroms (disorders of mood) like depression, anxiety, OCD, aggressive behaviors, eating disorders, — modulaton: temperature regulation, motor control, arousal
Link between seratoninergic centers & sudden infant death syndrome (SIDS) —
40% SIDS have abnormalities in 5HT in centers of the medulla involved in homeostatic regulation of hypercarbia & hypoxia during sleep — meaning that when we sleep our breathing pattern changes & is regulated by CO2 & O2 quantities in our bloodstream —
If sueratoninergic centers don’t function correctly they cannot regulate the response to increases in CO2 during sleep — normally if face is against pillow in sleep, amount of CO2 increases, with this info brought to the CNS causing us to autonomously move around — in case of malfunctioning of the seratoninergic nuclei, this mechanism doesn’t work, so the baby can die
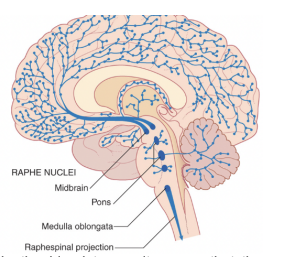
Dopaminergic pathways
Most dopaminergic centers are directed rostrally and the source of dopamine is mostly at the midbrain level
Can be divided into —
Mesostriatal (movement disorders)
Mosolimbic (reward, addiction, positive signs of schizophrenia)
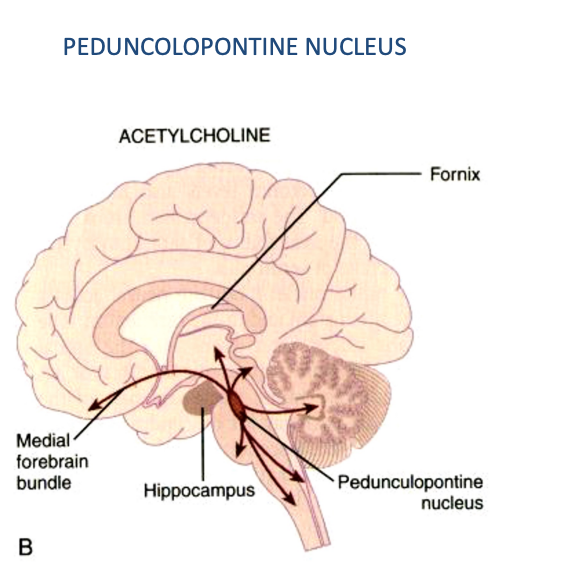
Cholinergic pathways — pedunculopontine nucleus
Nucleus that extends both in the pons & in the midbrain
Has several projections — among them — one projection to the intralaminar nuclei of the thalamus — part of the arousal mechanism of the cortex
Cholinergic group of neurons — involved in locomotion —
In the tegmentum of the midbrain there is a region called the mesencephalic locomotor region
Moreover, also projects to the motor nuclei of the brainstem & of the spinal cord
In continuity via the medial forebrain bundle with a group of cholinergic neurons located in the basal forebrain
Consiousness & coma
To have consciousness — we need an aroused cortex
Consiousness — has a content & a level
(Alertness, attention, awareness)
The reticular formation (especially the pedunculopontine nucleus) projects to the intralaminar nucleus of the thalamus, which then projects to the cortex, to the basal forebrain (specifically with the septal nuclei), and to the posterior nuclei of the hypothalamus
The pontomesencephalic reticular formation —
The one most responsible for cortex activation as it receives a lot of inputs —
The sensory pathways that ascend the brainstem, the limbic & cingulate cortex, the thalamic reticular nucleus, the limbic system, and the fronto-parietal association cortex
Consequentally, lesions in the upper region of the reticular formation (& bilateral extensive lesions of the cortex) result in coma
RF neurons can influence distant sites —
Axons of the RF neurons have a typical behavior —
Very long & can bifurcate along the brainstem’s longitudinal axis with one rostral & one caudal branch —
Meaning that one neuron can affect structures located very rostral (cerebral cortex), and neurons located caudally —
Ex. one single neuron can reach with one branch the cerebral cortex & with the other the caudal-most neuron of the spinal cord —
Thus, neurons of the RF are able to affect a lot of systems
Not pseudounipolar neurons — have dendrites & both branches are output portions
Structure in image belongs to a very typical neuron of the RF but not to all of them — many neurons that either project rostrally or caudally