Ch.22 - Respiratory System (Part 1)
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
Respiration
refers to ventilation of the lungs (breathing)
gas exchange
8 Functions of Respiration:
Gas Exchange
O2 and CO2 are exchanged between blood and air
gases move independently of each other
Communication
involved in production of speech and sound
Olfaction
sense of smell
Acid-Base Balance
influences pH of bodily fluids by eliminating CO2
Blood Pressure Regulation
by helping make angiotensin II (BP regulation hormone)
Blood and Lymph Flow
breathing creates pressure gradients between thorax and abdomen that promote flow of lymph and blood
Blood Filtration
lungs filter small clots
Expulsion of abdominal contents
holding your breath helps with urination, defecation, and childbirth (called valsalva maneuver)
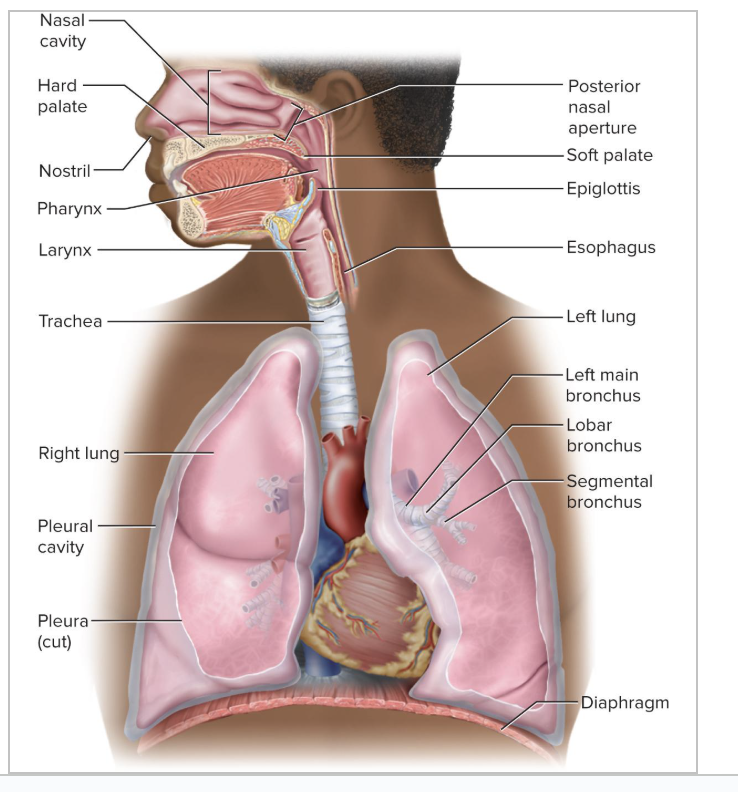
Principle Organs of the Respiratory System
nose, pharynx, larynx, trachea, bronchi, and lungs
alveoli stops incoming air
Conducting Zone of the Respiratory System
zone made for moving air
Includes those passages that serve only for airflow
NO gas exchange in this zone
lined with a mucous membrane,
filters, humidifies, and heats the air
Goes from the nostrils through the major bronchioles
Respiratory Zone of the Respiratory System
Where we have gas exchange
Consists of alveoli and other gas exchange regions
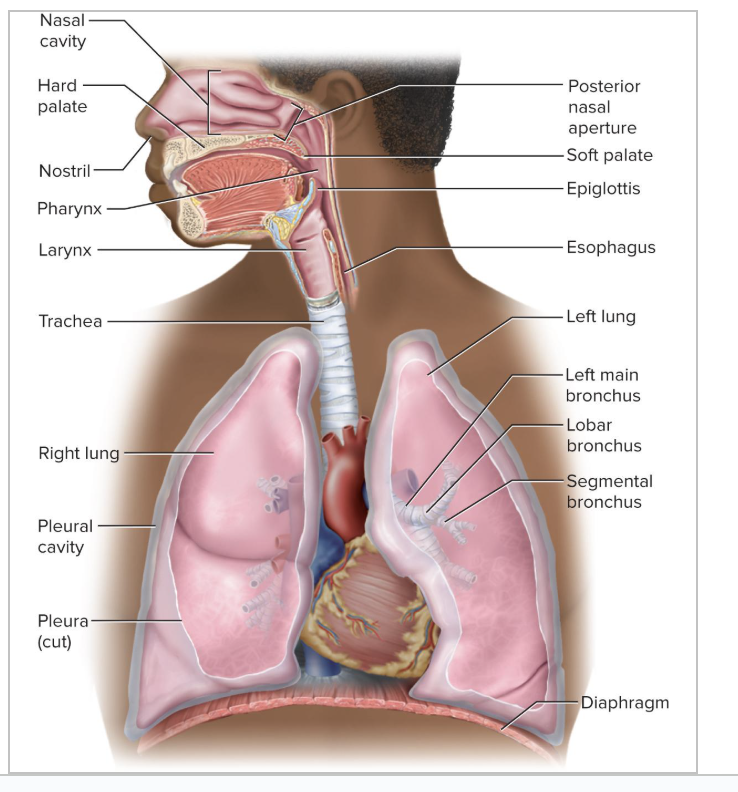
Upper Respiratory Tract
is in head and neck
more specifically, it goes from the nose to the larynx
Lower Respiratory Tract
includes the organs of the thorax
goes from trachea to lungs (neck down)
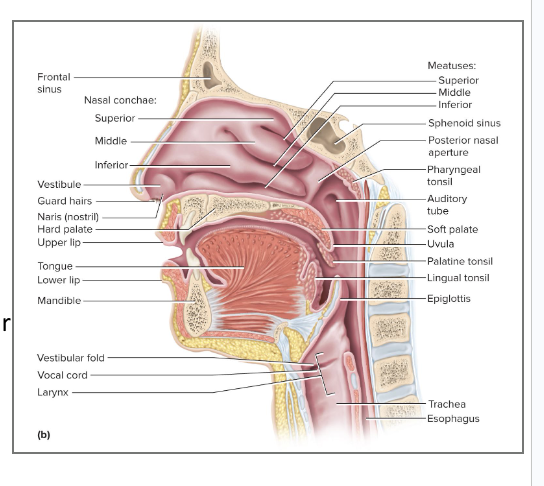
Functions of the Nose
Warms, cleanses, and humidifies inhaled air
Detects odors
Serves as a resonating chamber that amplifies voice
Structure of the Nose
Nose extends from the nostrils (nares) to the posterior nasal apertures (choanae / posterior openings)
Structures include:
Nasal Fossae
Vesibule
Nasal Conchae
Meatus
Olfactory Epithelium
Respiratory Epithelium
Erectile Tissue
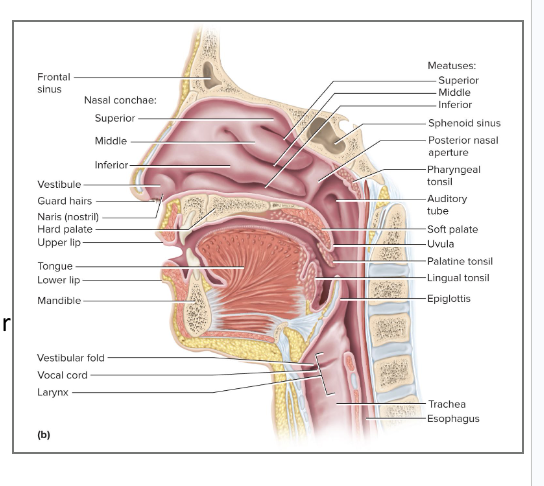
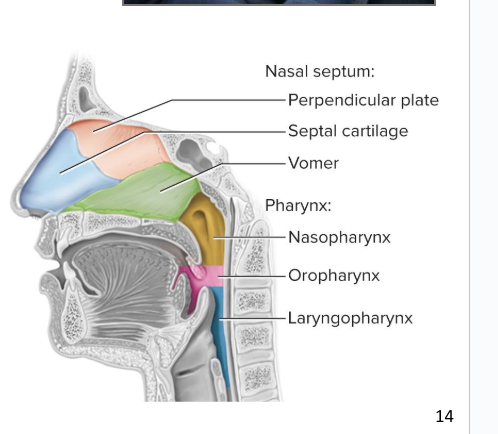
Nasal Fossae
right and left halves of nasal cavity
Nasal septum divides the nasal cavity into the 2 halves
Ethmoid and sphenoid bones form the roof of the nasal cavity
Hard palate forms the floor of the nasal cavity
Separates the nasal cavity from the oral cavity and allows you to breathe while you chew food
Where do the paranasal sinuses and nasolacrimal ducts drain into?
the nasal cavity
Vestibule
beginning of the nasal cavity
small, dilated chamber/open space just inside the nostrils
Lined with stratified squamous epithelium
Have vibrissae
nasal cavity gets bigger as we move posteriorly, and then gets narrow again
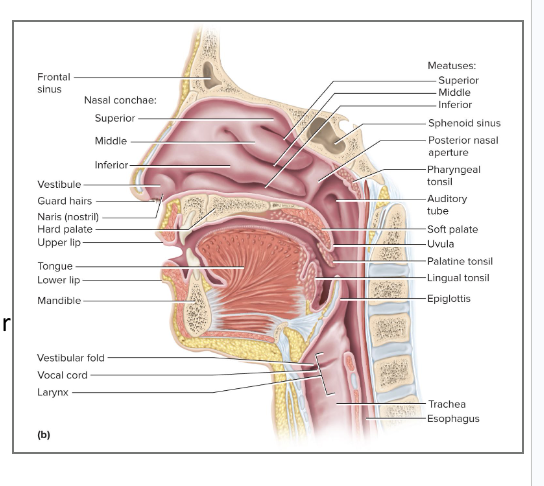
Vibrissae
stiff guard hairs that block insects and debris from entering nose
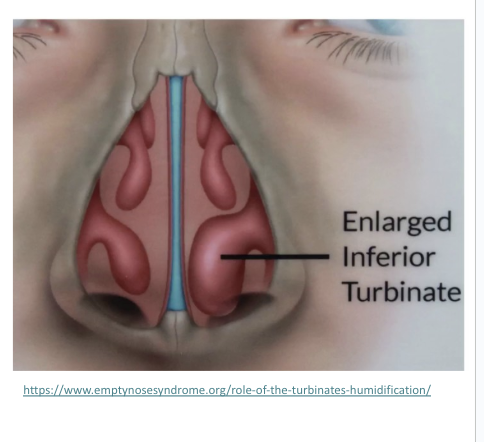
Nasal Conchae
3 folds of tissue that occupy the chamber behind the vestibule
consists of the superior, middle, and inferior nasal conchae (turbinates)
Project from lateral walls toward the septum
Each concha has a meatus
a narrow air passage beneath each concha
Narrowness and turbulence ensure that most air contacts mucous membranes
Cleans, warms, and moistens the air
most humidity is made with the nasal conchae
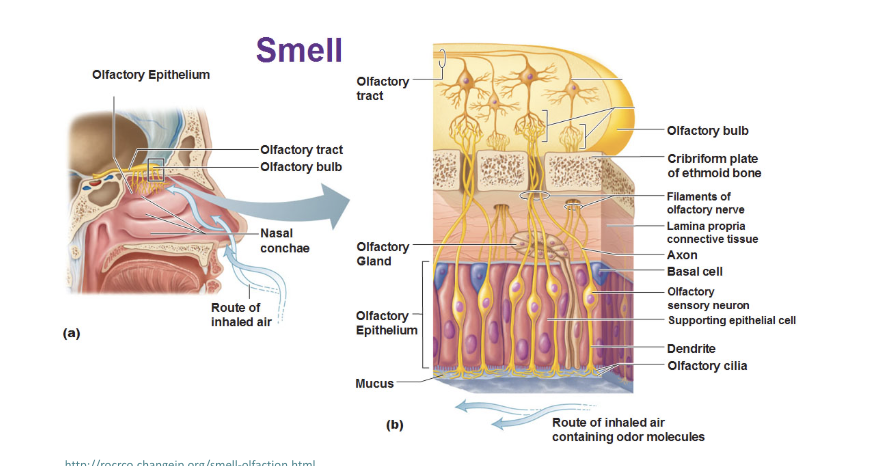
Olfactory Epithelium
detects odors
Covers a small area of the roof of the nasal fossa and neighboring parts of the septum and superior concha
there are immobile cilia on sensory cells that bind to odorant molecules
Respiratory Epithelium
lines the rest of nasal cavity except the vestibule
has ciliated pseudostratified columnar epithelium with goblet cells
Cilia are motile
Goblet cells secrete mucus and the cilia propel the mucus back toward the pharynx
mucus is swallowed into the digestive tract
Erectile Tissue (Swell Body)
tissue that swells as it absorbs more blood
In the nose, this tissue is located in the epithelium of the inferior concha
Every 30 to 60 minutes, tissue on one side swells with blood
This restricts airflow through that fossa, so most air is directed through the other nostril
This allows the engorged side time to recover from drying
Pharynx
The throat
a muscular funnel extending about 5 inches from the choanae to the larynx
part of body that can have food and air traveling through it
3 regions of pharynx
Nasopharynx
Oropharynx
Laryngopharynx
Nasopharynx
Receives auditory tubes and contains the pharyngeal tonsil
its 90° downward turn traps large particles
we don’t usually get food or water in the nasopharynx
passes only air and is lined by pseudostratified columnar epithelium
has mucous membrane
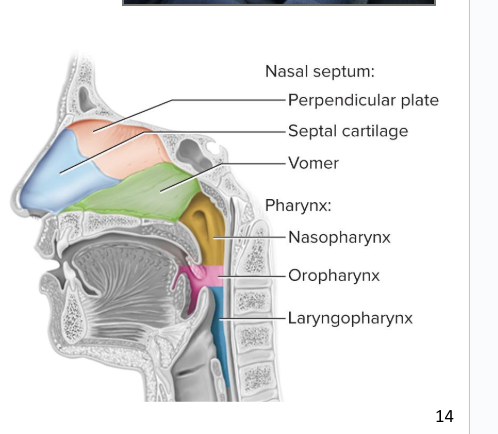
Oropharynx
Space between soft palate and epiglottis
Contains palatine tonsils
passes air, food, and drink
is lined by stratified squamous epithelium (non-keratinized)
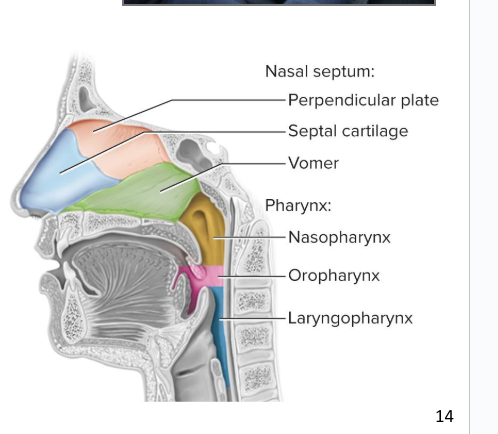
Laryngopharynx
space from the epiglottis to the cricoid cartilage
Esophagus begins at that point
passes air, food, and drink
lined by stratified squamous epithelium (non-keratinized)
Larynx
aka voice box
chamber made of hyaline cartilage about 4 cm (1.5 in.) long
Very sensitive structure
Primary function is to keep food and drink out of the airway
Addition role of phonation
the production of sound
9 cartilages make up the larynx
Ligaments suspends larynx from hyoid and hold it together
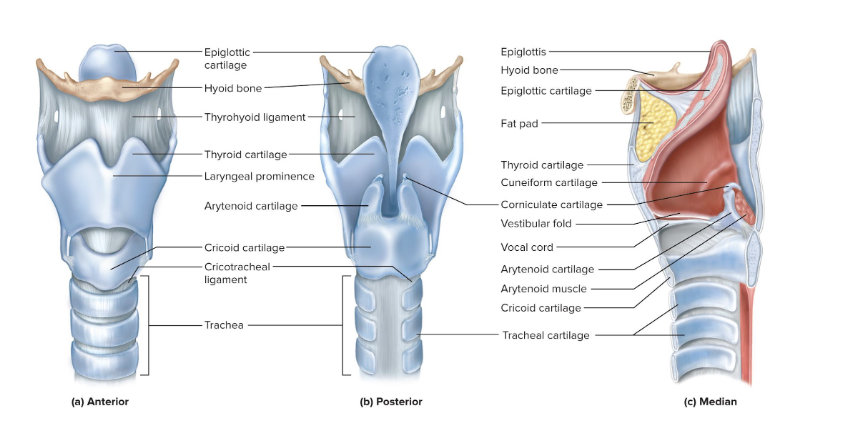
9 cartilages that make up the framework of the larynx:
3 are solitary and relatively large:
Epiglottic cartilage
Thyroid cartilage
Cricoid cartilage
3 smaller, paired cartilages
Arytenoid cartilages (2)
Corniculate cartilages (2)
Cuneiform cartilages (2)
Epiglottis
flap of tissue that guards the superior opening of the larynx (the glottis)
At rest, it stands almost vertically
During swallowing, extrinsic muscles of larynx pull the larynx upward
Then, the tongue pushes the epiglottis down to meet the larynx
This closes the airway and directs food to the esophagus behind it
Vestibular folds of the larynx play a greater role in keeping food and drink out of the airway
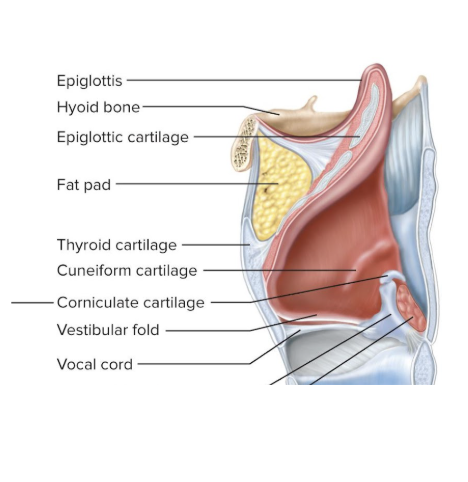
Epiglottic Cartilage
a spoon-shaped supportive plate in the epiglottis
most superior one
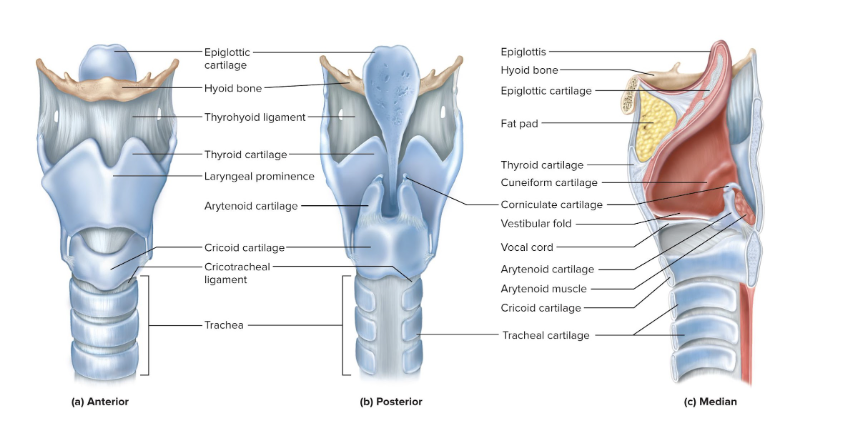
Thyroid Cartilage
is the largest cartilage of the larynx
makes a laryngeal prominence called the Adam’s apple
shield-shaped
Testosterone stimulates its growth, so it is larger in males
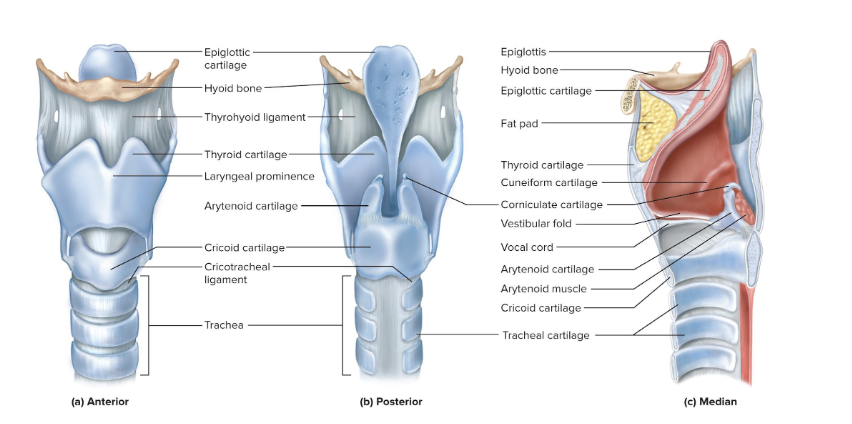
Cricoid Cartilage
connects the larynx to the trachea
ring-like
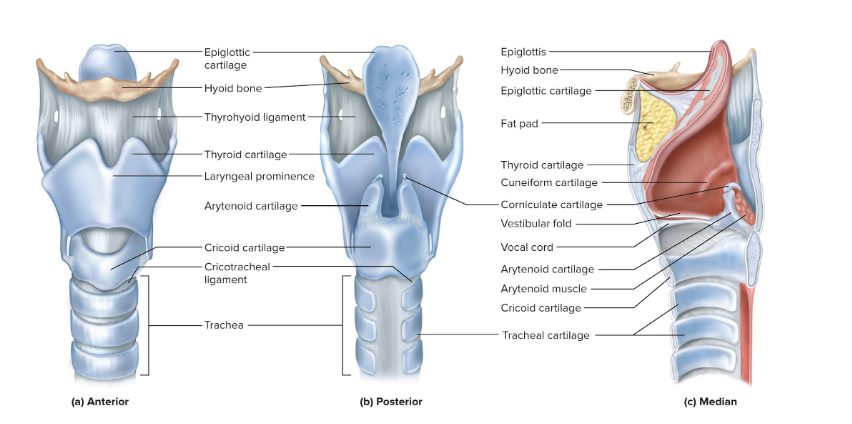
Arytenoid cartilages (2)
posterior to the thyroid cartilage
a pair
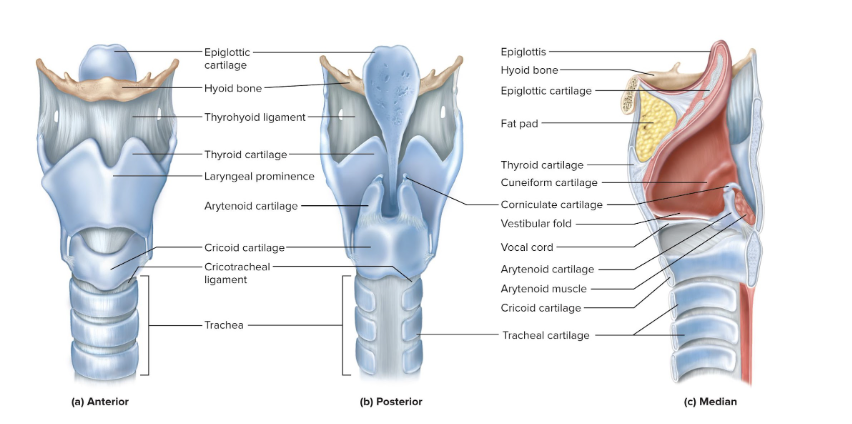
Corniculate cartilages (2)
attached to arytenoid cartilages like a pair of little horns
a pair
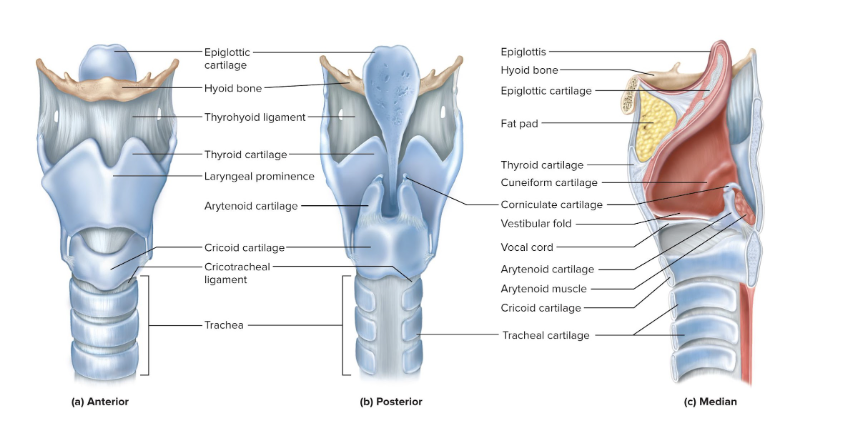
Cuneiform cartilages (2)
supports the soft tissue between the arytenoids and epiglottis
a pair
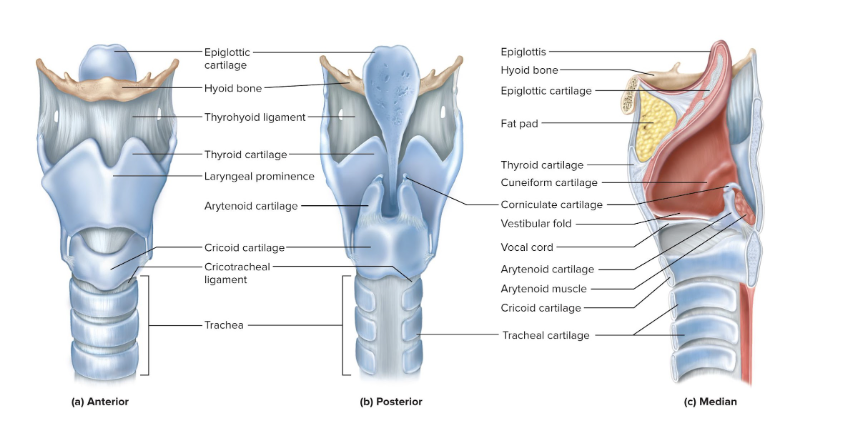
Thyrohyoid Ligament
suspends the larynx from the hyoid
starts at thyroid cartilage and goes to the hyoid bone
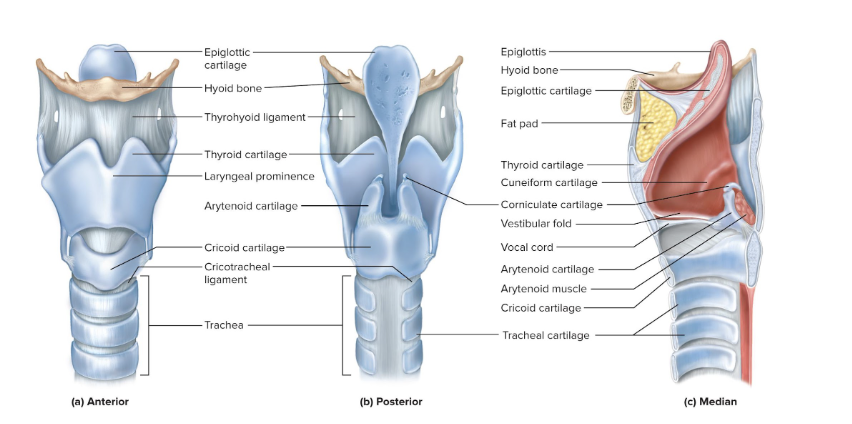
Cricotracheal Ligament
suspends trachea from larynx
starts at cricoid cartilage and goes to the trachea
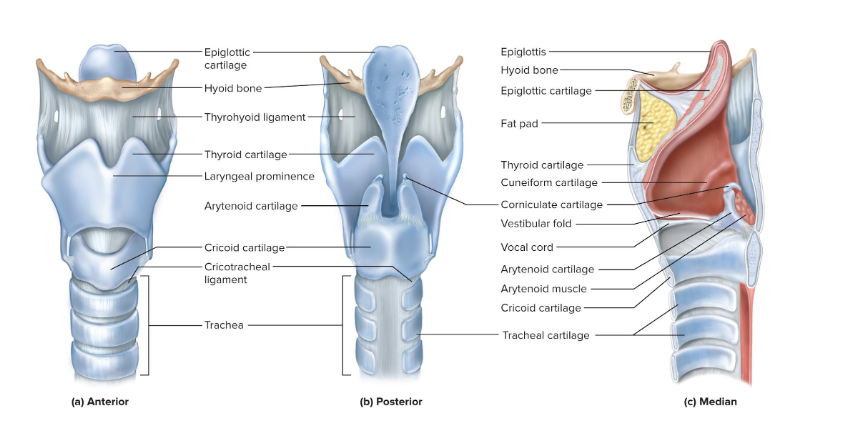
Superior Vestibular Folds
Called false vocal cords
Close the larynx during swallowing
Play no role in speech
have a mucous membrane
Vocal Cords
Produce sound when air passes between them
vocal cords vibrate when air goes out of respiratory tract
Contain vocal ligaments
Covered with stratified squamous epithelium
Suited to endure vibration and contact
Vocal cords produce crude sounds that are formed into words by actions of pharynx, oral cavity, tongue, and lips
Glottis
the vocal cords and the opening between them
Male Vs. Female Vocal Cords
Male vocal cords are usually:
Longer and thicker
Vibrate more slowly
Produce lower-pitched sound
Loudness
Determined by the force of air passing between the vocal cords
Pitch
Higher tension results in higher pitch and lower tension in lower pitch
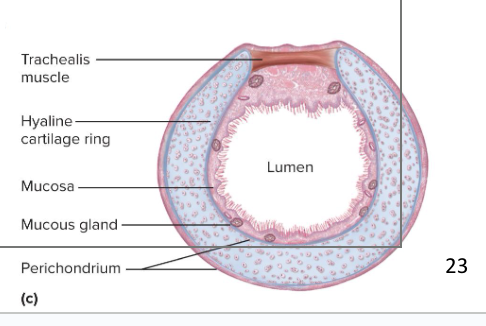
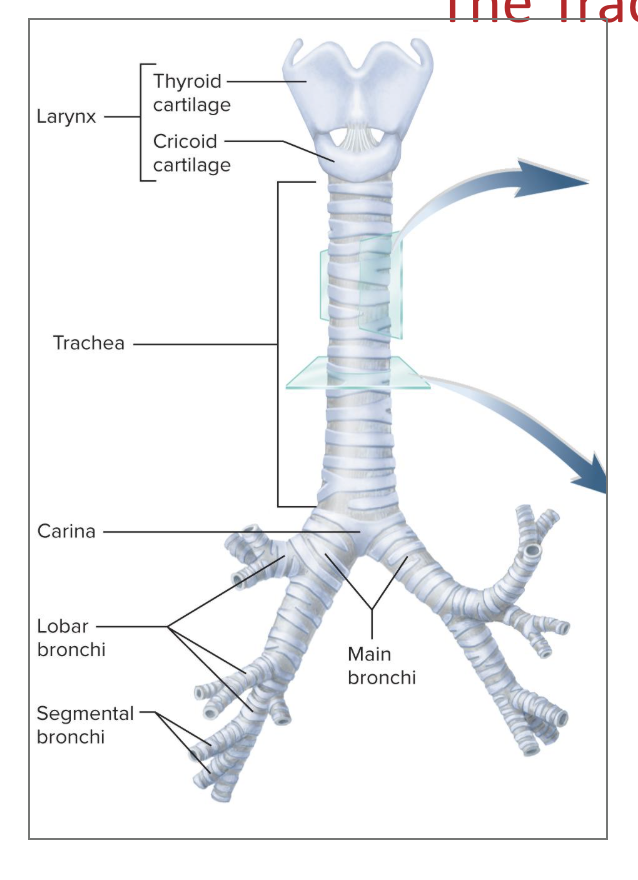
Trachea
the windpipe (a rigid tube)
is a conducting zone structure (moves air, no gas exchange)
anterior to the esophagus
16-20 C-Shaped hyaline cartilage rings prop trachea open and prevent collapse during inhalation
Trachealis muscle goes across the opening in the rings
the gap in the rings allow room for the esophagus to expand as food passes by
Contracts or relaxes to adjust airflow
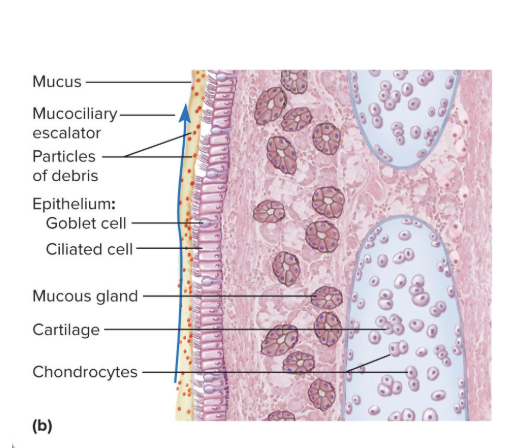
Inner lining
has ciliated pseudostratified columnar epithelium
secretes a ton of mucus
has a mucociliary escalator
Trachea branches off into the right and left main bronchi
Mucociliary Escalator
mechanism for debris removal in the trachea
Mucus traps inhaled particles
Upward beating cilia drives mucus toward the pharynx where it is swallowed
Middle Tracheal Layer
connective tissue beneath the tracheal epithelium
Contains lymphatic nodules, mucous and serous glands, and the tracheal cartilages
Right and Left Main Bronchi
the trachea branches off at the level of sternal angle to form the main bronchi
the ridge between the left and right bronchi forms the carina
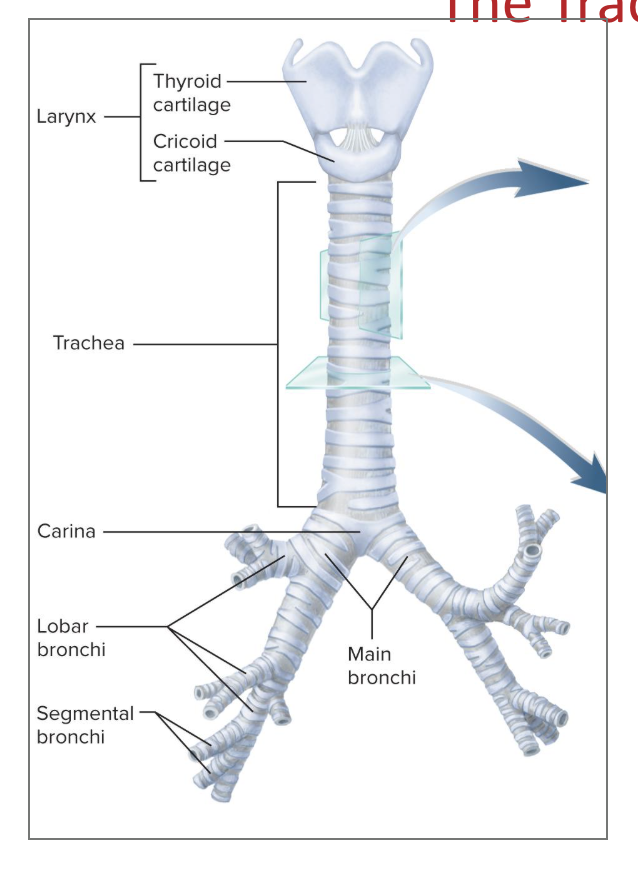
Carina
the internal medial ridge in the lowermost tracheal cartilage
Directs the airflow to the right and left
has lots of pressure receptors (built in panic button)
pressure on it causes violent coughing
if the particles go past the carina, it is much more difficult to get out of the lungs
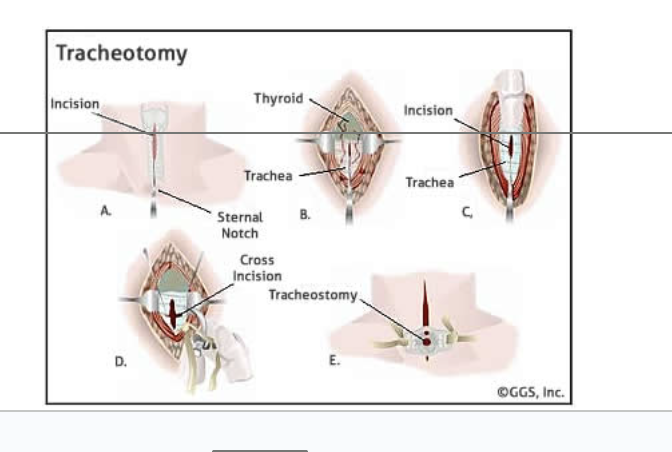
Tracheostomy
procedure where one makes a temporary opening in the trachea and inserts a tube to allow airflow
Prevents asphyxiation due to upper airway obstruction
Inhaled air bypasses the nasal cavity and is hot humidified
If tube is left in for too long, it will dry out mucous membranes of the respiratory tract
membrane will become encrusted and interfere with clearance of mucus from tract, promoting infection
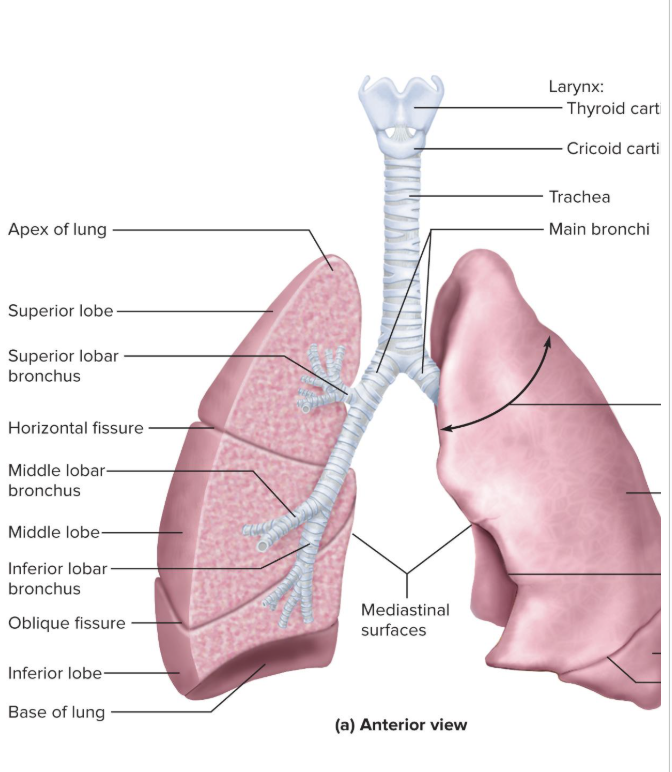
Anatomy of the Lung
Base: broad concave portion resting on diaphragm
Apex: tip that projects just above the clavicle
Costal surface: pressed against the ribcage
Mediastinal surface: faces medially toward the heart
has the hilum
Lungs are asymmetrical because of surrounding organs and major blood vessels
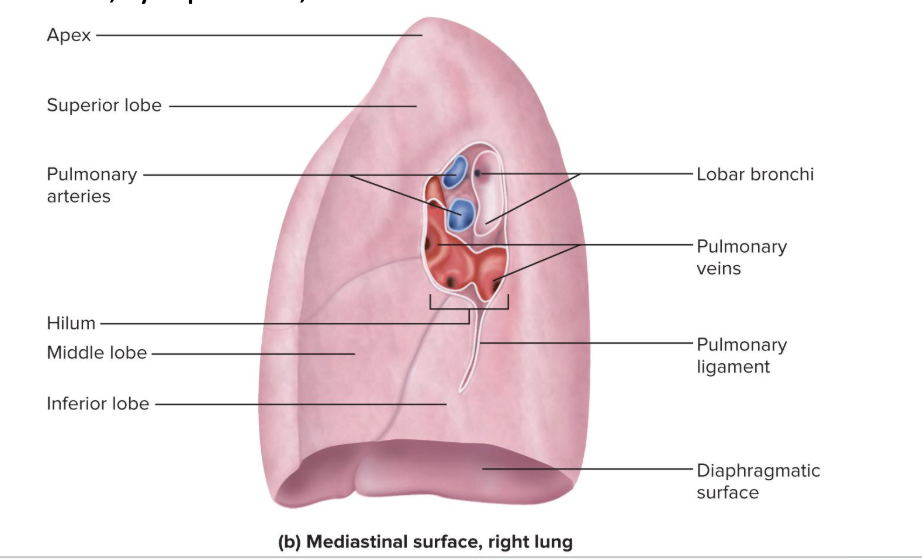
Hilum
slit through which the lung receives the main bronchus, blood vessels, lymphatics, and nerves
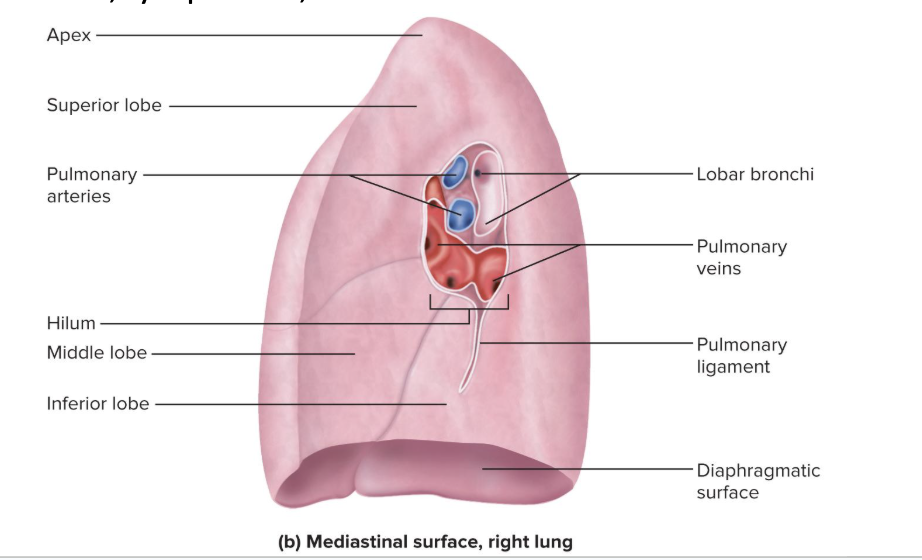
Right Lung Vs. Left Lung
Right lung
Shorter than the left lung because liver rises higher on the right
Has 3 lobes: superior, middle, and inferior
separated by horizontal and oblique fissure
Left lung
Tall and narrow because the heart tilts toward the left and occupies more space on this side of mediastinum
Has indentation called the cardiac impression
where the heart extends and presses into the left lung
Has 2 lobes: superior and inferior
separated by a single oblique fissure
Bronchial Tree
a branching system of air tubes in each lung
goes from the main bronchus to 65,000 terminal bronchioles
3 types of bronchi:
Primary Bronchi
Secondary Bronchi
Tertiary Bronchi
All bronchi are lined with ciliated pseudostratified columnar epithelium
Cells grow shorter and the epithelium thinner as we progress distally
All divisions of the bronchial tree have a large amount of elastic connective tissue
Contributes to the recoil that expels air from lungs
Bronchi have cartilage propping them open
Main (primary) Bronchi
the two main branches off of the trachea
are supported by C-shaped hyaline cartilage rings
Lobar (secondary) Bronchi
branches that send air to an individual lobe of the lung
supported by crescent-shaped cartilage plates
One for each lobe of lung: 3 in the right lung and 2 in the left
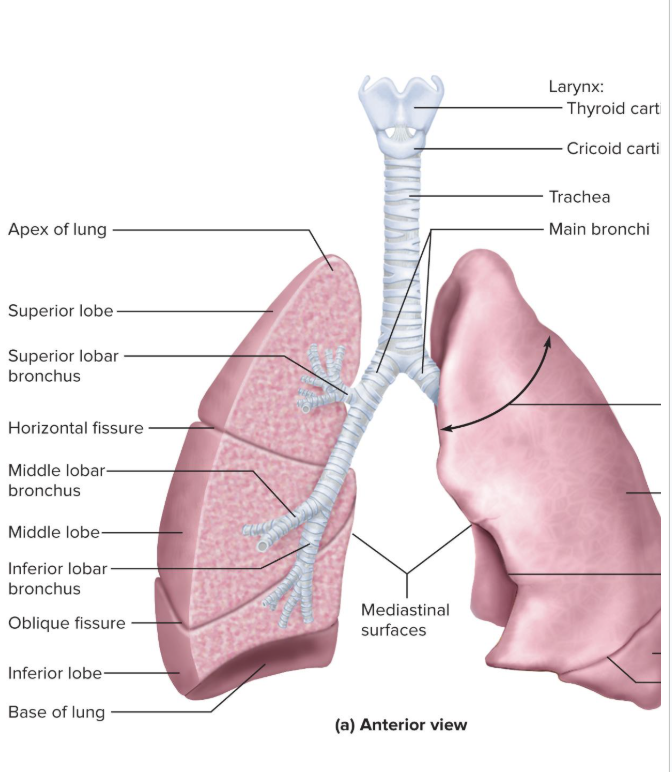
Segmental (tertiary) Bronchi
branches within the lobe of a lung
supported by crescent-shaped cartilage plates
10 on the right, 8 on the left
tertiary bronchi supply a specific bronchopulmonary segment
functionally independent unit of the lung tissue
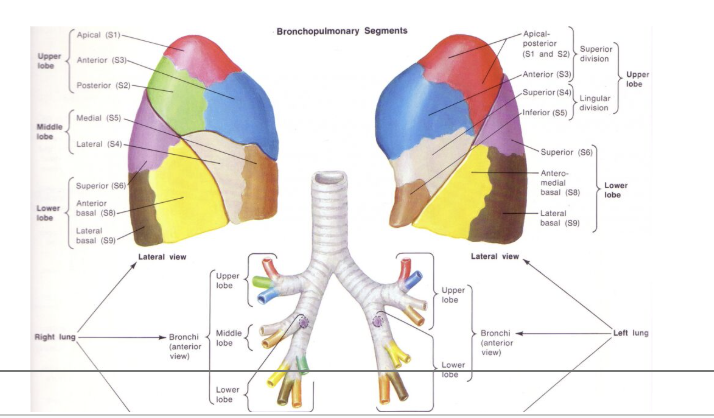
Bronchioles
smaller tubes in the lungs that move air around
don't have or need cartilage holding them open
1 mm or less in diameter
Have ciliated cuboidal epithelium
Well-developed layer of smooth muscle
Divides into 50 to 80 terminal bronchioles
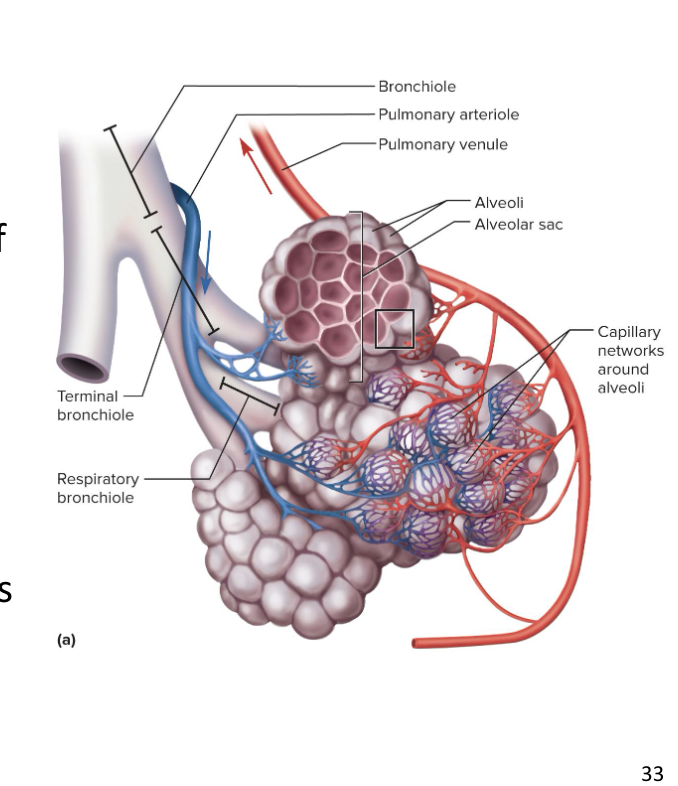
Terminal Bronchioles
Final branches of the conducting zone
Have no mucous glands or goblet cells
Have cilia that move back mucus draining into them using the mucociliary escalator
Each terminal bronchiole gives off two or more smaller respiratory bronchioles
Respiratory Bronchioles
have gas exchange with blood stream,
have simple squamous epithelium
Have alveoli budding from their walls
Considered the beginning of the respiratory zone since alveoli participate in gas exchange
Divide into 2 to 10 alveolar ducts
End in alveolar sacs
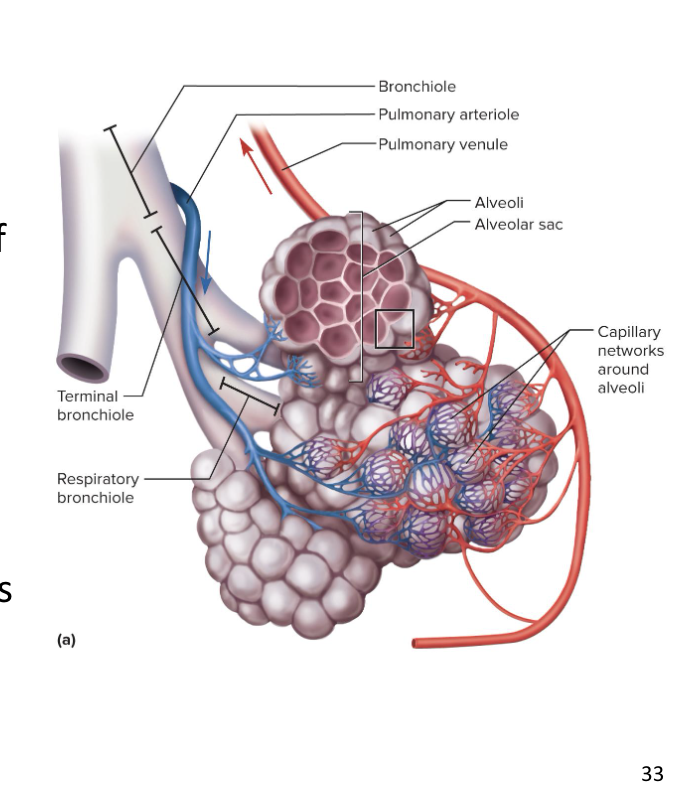
Alveolar Sacs
clusters of alveoli arrayed around a central space called the atrium
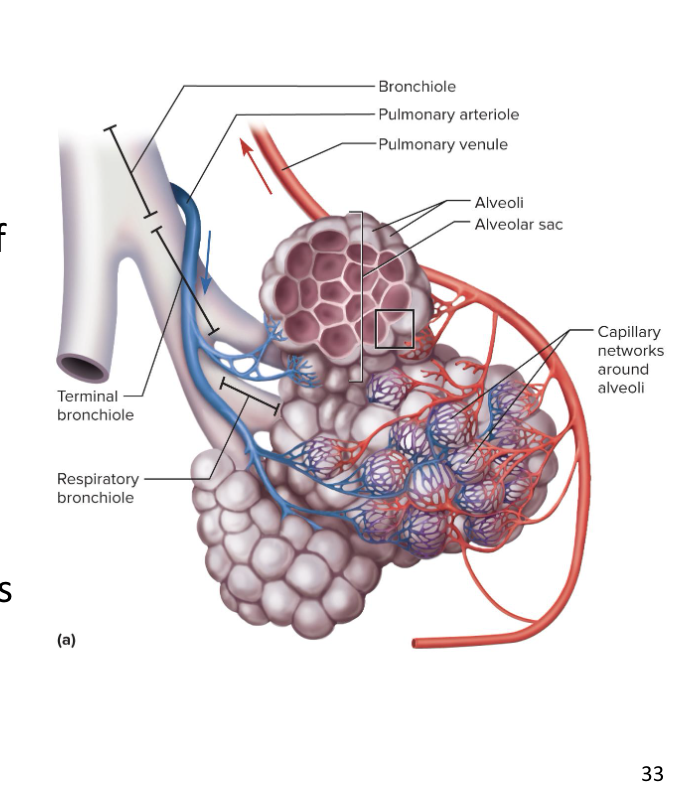
Alveoli
are respiratory zone structures that make up the alveolar sacs
there are 150 million alveoli in each lung, providing lots of surface area for gas exchange
simple squamous epithelium to maximize diffusion
no mucus and no structures to remove the mucous
3 types of cells that make up the alveoli:
Squamous Alveolar Cells (Type 1)
Great Alveolar Cells (Type 2)
Alveolar Macrophages (Dust Cells)
Each alveolus is surrounded by a basket of capillaries supplied by the pulmonary artery
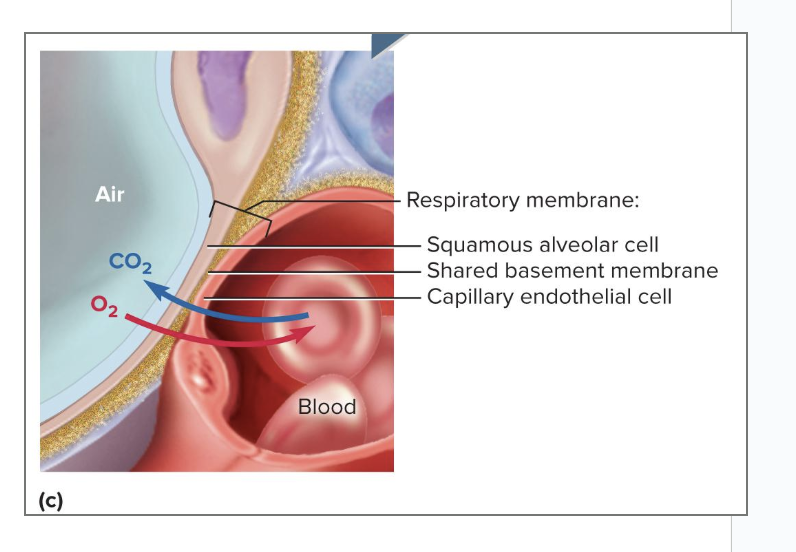
Squamous Alveolar Cells (Type 1)
Thin, broad cells that allow for rapid gas diffusion between the alveoli and the blood
most common
covers 95% of alveoli surface area
Great Alveolar Cells (Type 2)
Round to cuboidal cells that cover the remaining 5% of alveolar surface
Repair the alveolar epithelium when the squamous (type I) cells are damaged
Secrete pulmonary surfactant (soap)
makes it easier for us to open up the airways
have a polar region and nonpolar region (amphipathic)
this allows them to H bond to water and reduce the amount of H bonds present when walls collapse
Alveolar Macrophages (Dust Cells)
Cells that wander through the lumens of alveoli and the connective tissue between them
Keep alveoli free from debris by phagocytizing dust particles
100 million dust cells die each day as they ride up the mucociliary escalator to be swallowed and digested with their load of debris
Respiratory Membrane
thin barrier between the alveolar air and blood
where gas exchange occurs
gases move independently
the simple squamous alveolar cells and capillaries share a basement membrane that glues them together
CO2 goes from blood to alveolar air
Oxygen goes into the blood from the alveoli
How do we prevent fluid from accumulating in alveoli?
Alveoli are kept dry by absorption of excess liquid by blood capillaries
Lungs have more extensive lymphatic drainage than any other organ in the body
Low capillary blood pressure also prevents the rupture of the delicate respiratory membrane
Pleural Membrane
serous membrane of the lungs (double membrane)
Has a parietal pleura and a visceral pleura
Has a pleural cavity in-between the two pleura
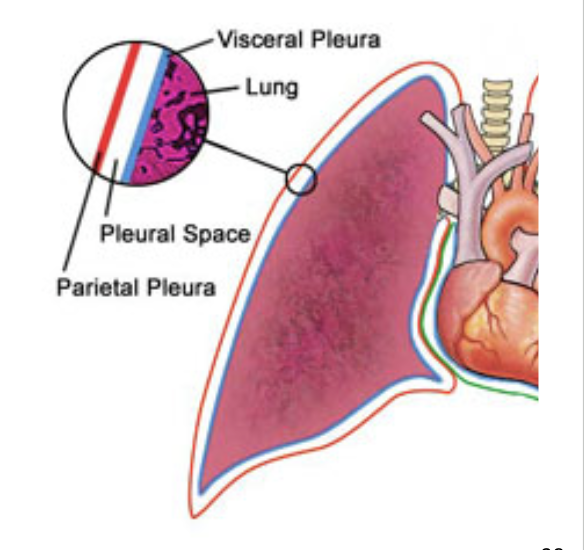
Visceral Pleura
serous membrane that covers the lungs
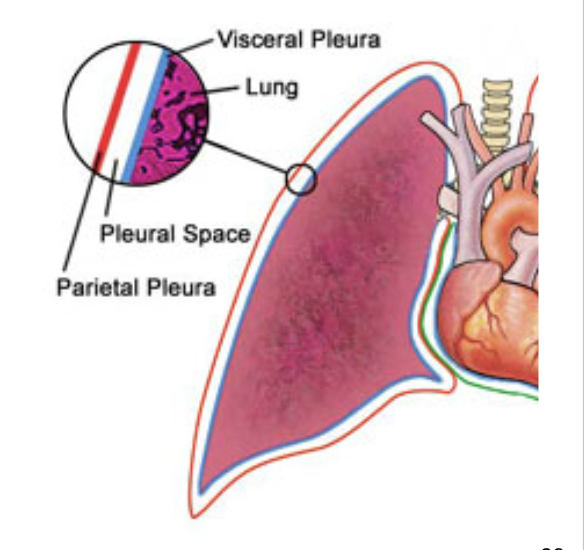
Parietal Pleura
attaches to the mediastinum, the inner surface of the rib cage, and the superior surface of the diaphragm
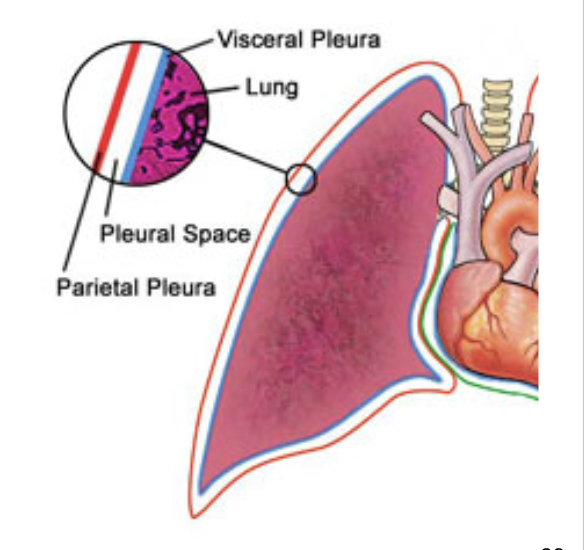
Pleural Cavity
the potential space between the pleurae
Normally no room between the membranes, but contains a film of slippery pleural fluid
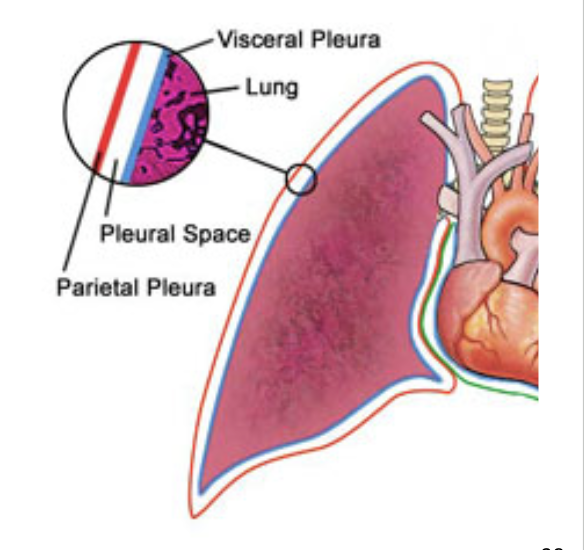
Functions of the Pleurae and Pleural Fluid
Reduces friction
pleural fluid is slippery, causing less friction
Creates a pressure gradient
Lower pressure than atmospheric pressure
assists lung inflation
Creates a pressure gradient to help the pleura hydrogen bond to each other
Compartmentalization
Prevents spread of infection from one organ in mediastinum to others
Pulmonary Ventilation
consists of a repetitive cycle of inspiration (inhaling) and expiration (exhaling)
Flow of air in and out of lung depends on a pressure difference between air within lungs and outside body
Respiratory muscles change the lung volume and creates differences in pressure relative to the atmosphere
pressure and volume are inversely proportional
Respiratory Cycle
one complete inspiration and expiration
Quiet respiration: while at rest, effortless, and automatic
Forced respiration: deep, rapid breathing, such as during exercise
happens with sympathetic activation or high metabolic needs
Diaphragm
most important muscle for inspiration
Prime mover of respiration
located below the lungs
Contraction flattens the diaphragm and pulls the abdominal organs down, making the thoracic cavity larger and pulling more air into the lungs
Relaxation allows diaphragm to bulge upward again, compressing the lungs and expelling air
Accounts for two-thirds of airflow
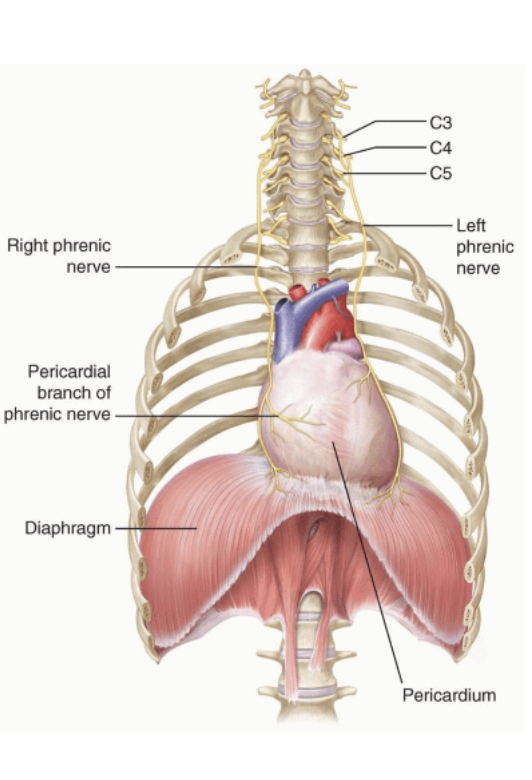
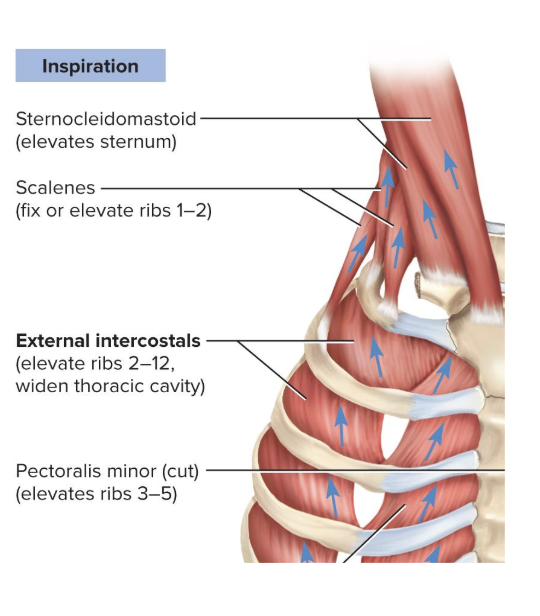
External Intercostal Muscles
used to elevate the ribs to make thoracic cavity larger
Stiffen the thoracic cage during respiration
Prevent it from caving inward when diaphragm descends
Contribute to enlargement and contraction of thoracic cage
Add about one-third of the air that ventilates the lungs
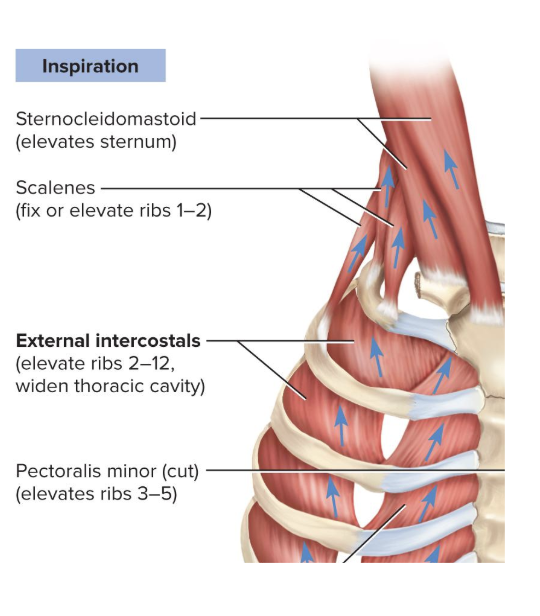
Scalenes
Synergist muscles to the diaphragm
Fix or elevate ribs 1 and 2
Normal Quiet Expiration
An energy-saving passive process
exhaling does not involve activation of muscles, instead we rely on elastic recoil of the lungs and thoracic cage
allows our lungs to naturally contract on themselves for exhalation
As muscles relax, structures recoil to the original shape and size of the thoracic cavity
results in airflow out of the lungs
Forced Expiration
uses muscles in addition to the elastic recoil
uses the rectus abdominis, internal intercostals, and other lumbar, abdominal, and pelvic muscles
the greatly increased abdominal pressure pushes the viscera up against the diaphragm, increasing thoracic pressure and forcing air out
Important for “abdominal breathing”
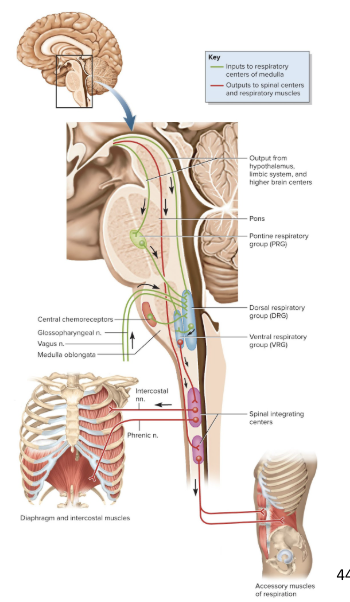
Brainstem Regulatory Centers
the brain stem regulates autonomic respiration using 3 regulatory centers:
Ventral respiratory group (VRG)
Dorsal respiratory group (DRG)
Pontine respiratory group (PRG)
Ventral Respiratory Group (VRG)
Primary generator of the respiratory rhythm
Produces a respiratory rhythm of 12 breaths per minute
located on anterior of medulla
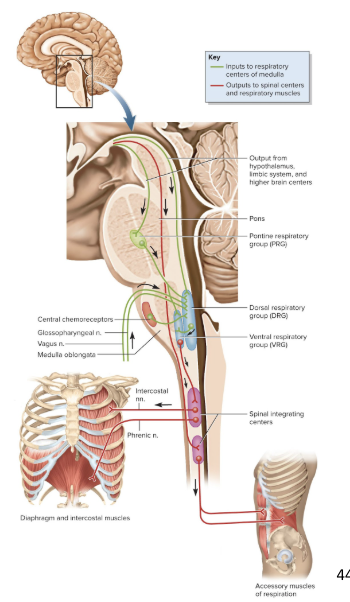
Dorsal Respiratory Group (DRG)
Modifies the rate and depth of breathing
Receives influences from external sources
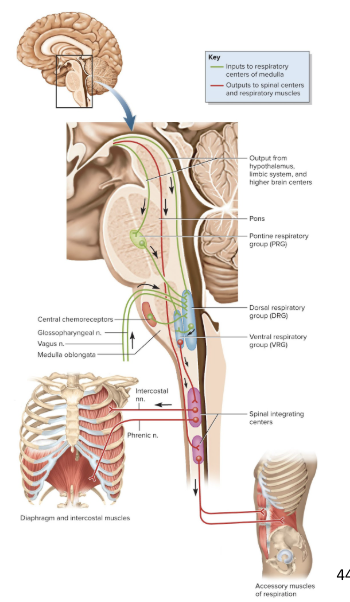
Pontine Respiratory Group (PRG)
Modifies the respiratory rhythm by outputs to both the VRG and DRG
modifies the respiratory rhythm in response to external stimuli
Adapts breathing to special circumstances such as sleep, exercise, vocalization, and emotional responses
Hyperventilation
anxiety-triggered state where breathing is so rapid that it expels CO2 from the body faster than it’s produced
As blood CO2 levels drop, the pH rises causing the cerebral arteries to constrict
makes blood pH more basic
this causes there to be less blood and O2 going to the brain, which may cause dizziness or fainting
Can be controlled by having the person rebreathe the expired CO2 from a paper bag
Voluntary Control of Breathing
Voluntary control over breathing originates in the motor cortex
signals bypass brainstem to respiratory neurons
voluntary control over breathing is temporary, the ANS will overrride
Breaking point: when CO2 levels rise and the blood pH get too low to a point where automatic controls override one’s will