IB Biology Topic 6
1/180
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
181 Terms
alimentary canal
organs through which food actually passes (oesophagus, stomach, small & large intestine)
accessory organs
aid in digestion but do not actually transfer food (salivary glands, pancreas, liver, gall bladder)
Stomach
A temporary storage tank where food is mixed by churning and protein digestion begins
It is lined by gastric pits that release digestive juices, which create an acidic environment
Pancreas
Produces a broad spectrum of enzymes that are released into the small intestine via the duodenum
Also secretes certain hormones (insulin, glucagon), which regulate blood sugar concentrations
Small Intestine
A long, highly folded tube where usable food substances (nutrients) are absorbed
Large intestine
Final section of alimentary canal, where water and dissolved minerals are absorbed
Consists of the ascending / transverse / descending / sigmoidal colon, as well as the rectum
Liver
Takes the raw materials absorbed by the small intestine and uses them to make key chemicals
Its role includes detoxification, storage, metabolism, bile production and haemoglobin breakdown
Peristalsis
the process of wave-like muscle contractions of the longitudinal muscles that moves food along
Segmentation
Bidirectional mixing of food in the small intestine caused by circular muscles
How does food move through the gut?
contraction of circular longitudinal musces of the small intestine
Chemical digestion : stomach acids
- Contain gastric glands which release digestive acids = low pH environment
- Acidic environment denatures proteins and other macromolecules
- Stomach epithelium = mucous membrane = prevents acids damaging gastric lining
- Pancreas releases alkaline compounds = neutralises the acids as they enter the intestine
Chemical digestion : bile
- Liver produces
- Stored and concentrated in gall bladder
- Released into the intestine
-Contains bile salts = emulsification of fat
- The emulsification of fats increases the total surface area available for enzyme activity (lipase)
Enzymes digest most...
macromolecules in food into monomers in the small intestine e.g. lipase breaks down fat
Digestion of Carbohydrates
- Begins in the mouth with the release of amylase from the salivary glands
- Amylase is also secreted by the pancreas in order to continue carbohydrate digestion within the small intestine
- Enzymes for disaccharide hydrolysis are often immobilised on the epithelial lining of the small intestine, near channel proteins
digestion of proteins
-Begins in the stomach with the release of proteases
- Smaller polypeptide chains enter the small intestine where they are broken down by endopeptidases released by the pancreas
- These endopeptidases work optimally in neutral environments as the pancreas neutralises the acids in the intestine
digestion of lipids
- Occurs in the intestines, beginning with emulsification of fat by bile
- The smaller fat droplets are digested by lipases released from the pancreas
digestion of nucleic acids
Pancreas releases nucleases = digest nucleic acids (DNA, RNA) into smaller nucleosides
What secretes enzymes into the lumen of the small intestine?
the pancreas
how many layers in the small intestine structure?
4
Serosa
protective outer layer
Muscle layer
outer layer of longitudinal muscle (peristalsis) and inner layer of circular muscle (segmentation)
Submucosa
connective tissue seperating the inner mucosa and the muscles
mucosa
a highly folded inner layer which absorbs through its surface epithelium
Villi
Fingerlike extensions of the intestinal mucosa that increase the surface area for absorption
Villi absorb
monomers formed by digestion and mineral ions and vitamins
Features of Villi
Mnemonic: MR SLIM
- Microvilli
- Rich blood supply
- Single layer epithelium
- Lacteals
- Intestinal glands
- Membrane proteins
Different types of membrane transport for digestion:
Endocytosis, Simple Diffusion, Osmosis, Facilitated Diffusion, Co-Transport/Active transport
Glucuoe and amino diffuse through...
co-transport
monosaccarides and hydrophillic diffuse through...
facilitated diffsuion
water diffuses through...
osmosis
hydrophopic substances transport through...
simple diffusion
Pinocytosis
A type of endocytosis in which the cell ingests extracellular fluid and its dissolved solutes.
Process of the digestion of starch in small intestine:
1. salivary amylase and pancreatic amylase are the enzymes which digest
2. Ammylose into maltose subunits
3. Amylopectin into dextrins
4. The hydrolysis of dextrins and maltose = production of glucose
5. This can be used to make ATP or stored as glycogen
6. The hormone insulin and glucagon regulate the concentration of glucose
Insulin
A hormone which lowers blood glucose levels
Glucagon
A protein hormone secreted by pancreatic endocrine cells that raises blood glucose levels
Dialysis tubing
Plastic-like cellulose tubing with tiny holes to allow small molecules to pass through, it models absorption of food in the intestine
WIlliam Harvey discovered the blood system
were a combined network, blood flows continusouly, the heart is the pump (arteries from hear) (veins to heart), Blood flow is unidirectional
pulmoary circuit
on the right side of the heart
systemic circulation
on the left side of the heart
Arteries
Blood vessels that carry blood away from the heart
Characteristics of arteries
blood at high pressure, walls are thick, wales stretch or contract with a pulse, walls contain muscles cells and elastic fibres
Capillaries
Microscopic vessel through which exchanges take place between the blood and cells of the body
Characteristics of capllilaries
blood at low pressure, walls made of a single layer, extremly narrow lumen, facilatate material exhange
Cappliaries absorb
cell waste e.g. carbon dioxide and urea
Veins
Blood vessels that carry blood back to the heart
Characterisitc of veins
blood at low pressure, wide lumen, have valves, walls are thin, small amounts of muscles
Role of valves in the blood system
prevent backwards blood flow
heart structure
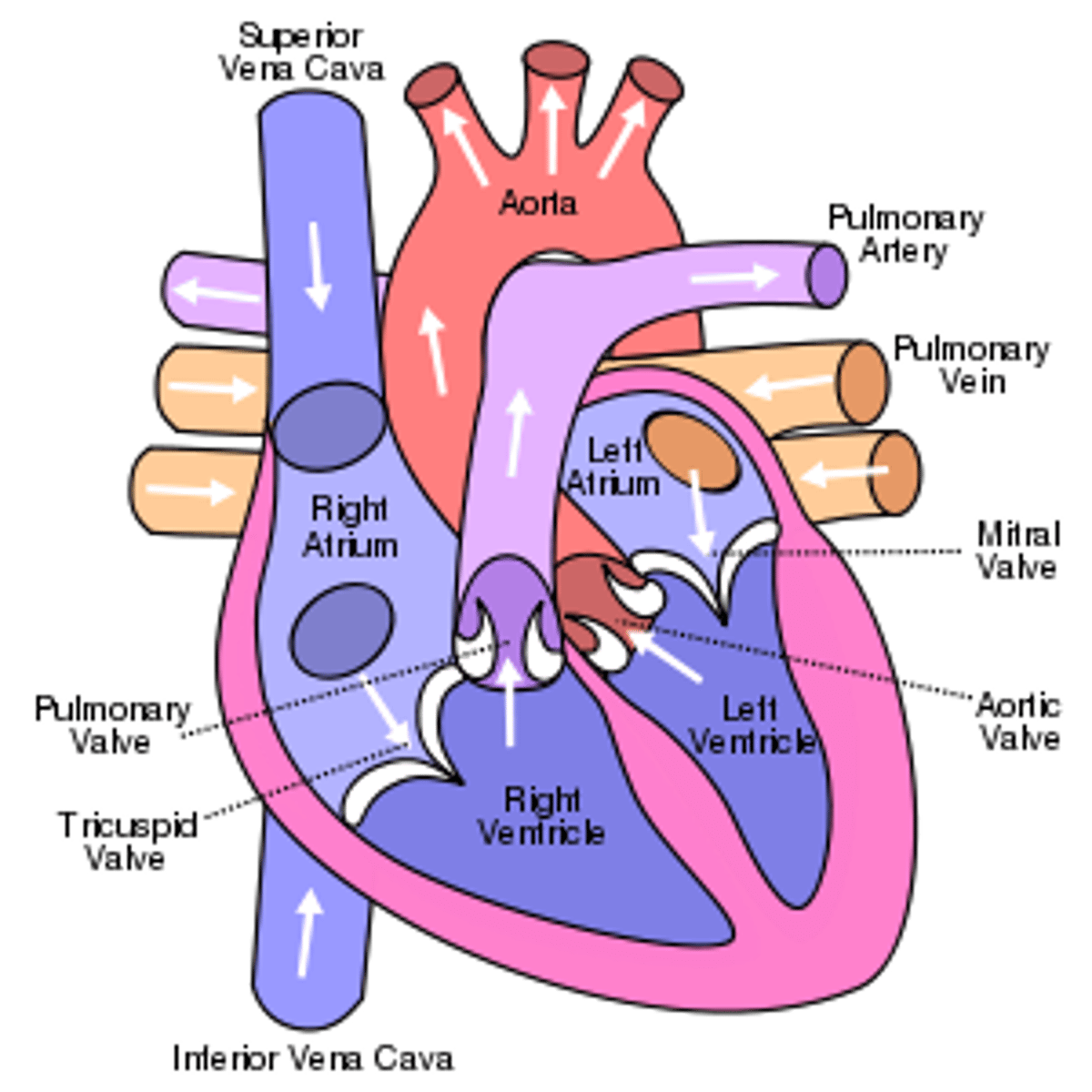
Pathway of deoxygenated blood through the heart
-Vena Cava (veins) from body
-Right Atrium
-Tricuspid valve
-Right Ventricle
-Pulmonary valve
-Pulmonary (artery)
-Lungs
Pathway of oxygenated blood
-from lungs
-Pulmonary veins
-Left Atrium
-bicuspid valve
-Left ventricle
-aortic semilunar valve
-aorta
-body
Sinotorial node
pacemaker on right atrium of heart
Describe the electrical events that trigger the contraction of the heart muscle fibres
- The heart beat is myogenic
- Electrical signals are initiated by the sinoatrial (SA) node
- It stimulates the atria to contract and also relays signals to an atrioventricular node
- The atrioventricular node sends signals via the Bundle of His to Purkinje fibres
- These fibres innervate the ventricles and cause them to contract
how is heart rate increased and decreased?
by impulses brought to the heart through two nerves from the medulla of the brain.
Describe the role of the medulla and epinephrine (adrenaline) in regulating heart rate
- The SA node maintains the heart's normal sinus rhythm (60 - 100 bpm)
- The SA node may be regulated by the medulla, with sympathetic nerves increasing heart rate, by releasing noradrenaline and parasympathetic nerves decreasing the heart rate by releasing acetylcholine
- Heart rate may also be increased by the release of epinephrine (a.k.a. adrenaline) into the bloodstream
Outline the pressure changes in the heart during the cardiac cycle
Blood returning to the heart will flow into the atria and ventricles as the pressure in them is lower
As ventricles fill, atria contract (atrial systole), increasing pressure in atria and forcing blood into ventricles
As ventricles contract, ventricular pressure exceeds atrial pressure and AV valves close to prevent back flow
When ventricular pressure exceeds pressure in aorta, the aortic valve opens to release blood into the aorta
As blood exits the ventricle, ventricular pressure falls below aortic pressure, so the aortic valve closes
When ventricular pressure drops below atrial pressure, the AV valve opens and cycle begins again
Causes of Coronary Occlusion
- Fatty deposits develop in the arteries and reduce the lumen
- The restricted blood flow increases pressure in the artery, = damage to the arterial wall
- The damaged region is repaired with fibrous tissue which significantly reduces the elasticity of the vessel wall
- As the smooth lining of the artery is degraded, lesions form called atherosclerotic plaques
- If the plaque ruptures, blood clotting is triggered, forming a thrombus that restricts blood flow
- If the thrombus is dislodged it becomes an embolus and can cause a blockage in a smaller arteriole
Risk Factors for Coronary Heart Disease
Age
Genetics
Obesity
Diseases
Diet
Exercise
Sex
Smoking
First line of defence
prevent the entry of pathogens into the body
- intact skin
- mucous membranes
Blood clots
1 - Platelets : form a sticky plug at the damaged region (primary haemostasis)
2 - Fibrin strands form an insoluble mesh of fibres that trap blood cells at the site of damage (secondary haemostasis)
Coagulation Cascade
1- Platelets to become sticky and adhere to the damaged region = solid plug
2- Initiate localised vasoconstriction = reduce blood flow. Triggers conversion of the inactive zymogen prothrombin into the activated enzyme thrombin
3 - Thrombin catalyses fibrinogen to fibrin
4 - The fibrin strands = mesh of fibres around the platelet plug and traps blood cells to form a temporary clot
5- When the damaged region is completely repaired, an enzyme (plasmin) is activated to dissolve the clot
Second line of defence
Innate immune system
- non-specific
- non-adaptive
Phagocytosis process
- Phagocytic leukocytes circulate in the blood and move into the body tissue in response to infection
- Histamine released which draw white blood cells to the site of infection via chemotaxis
- Pathogens engulfed when pseudopodia surround the pathogen and then fuse to form an internal vesicle
- The vesicle is then fused to a lysosome forming a phagolysosome and the pathogen is digested
- Antigens may be presented on the surface of the phagocyte in order to stimulate the third line of defence
Third line of defence
Adaptive immune system, which is specific in its response
B lymphocytes
are antibody producing cells that recognize and target particular antigens
T lymphocytes
are regulator cells that reslease chemicals to activate specfic B cells
Antibodies
Proteins produced by B cells that attach to antigens, keeping them from harming the body
Antigen
A protein that, when introduced in the blood, triggers the production of an antibody
Antigens are specific
to a antibody
Antibiotics can only work on
prokaryotic cells
Antibiotics targets
prokaryotic metabolism
Viruses lack a metabolsim and hence
can not be treated with antibiotics
Antibiotic resistance happens by ..
Genes degrade the antibiotic, block its entry, increase its removal or alter the target
Resistance increases due to....
Antibiotics are :
- Over-prescribed
- Misused
- Freely available
Penicillin
the first discovered antibiotic
Florey and Chain experiment
mice made sick with bacteria, half were given penicillin and teh other hald nothing, those who ingestied penicillin lived
Effects of HIV on the immune system
- HIV targets t cells
- the virus is inactive during when the t cells reproduce
- eventually, the virus is active and has spread
- antibodies can't be produced
- one is extremely susceptible to infection
ventialtion maintains
concentration gradients of oxygen and carbon dioxide between air in the alveoli and blood flowing in adjacent capllicaires
Ventilation
movement of air in and out of the lungs
gas exchange
the process of obtaining oxygen from the environment and releasing carbon dioxide
Gas exchange by pressure in lungs:
Occurs via diffusion
O2 concentration is higher in the lungs than in the blood, so O2 diffuses into blood.
CO2 concentration in the blood is higher than in the lungs, so CO2 diffuses out of blood.
cell respiration
the process in cells in which oxygen is used to release stored energy by breaking down sugar molecules
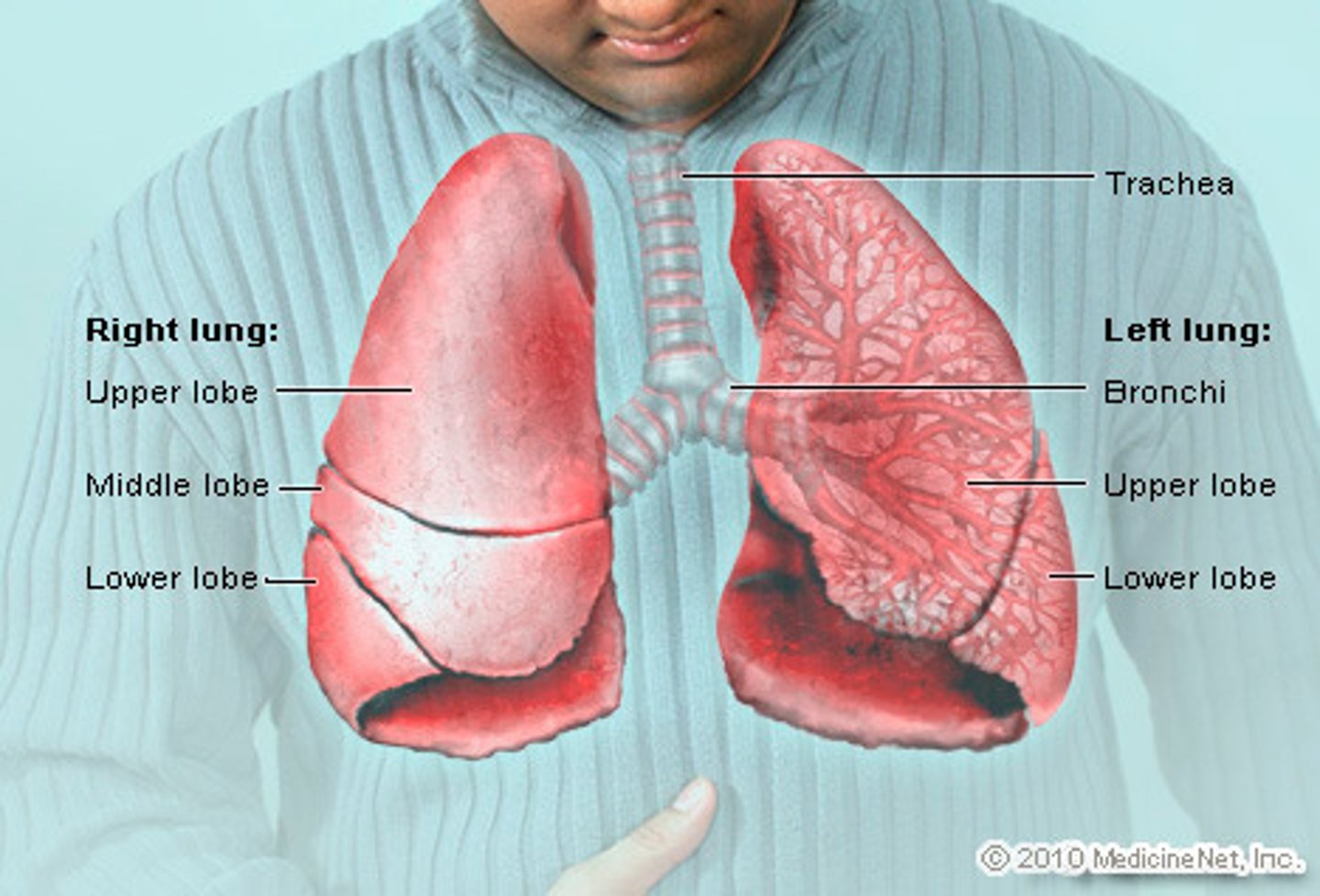
Lung structure
trachea, bronchi, bronchioles, alveoli
Alveoli structure
- Thin epithelial layer
- Rich capillary network
- Spherical
- Internal surface is covered with a layer of fluid
Type I pneumocytes
extremely thin alveolar cells that are adapted to carry out gas exchange
Type II pneumocytes
cuboidal cells that's produce surfactant which reduces surface tension in the alveoli
What does surfactant do?
It reduces surface tension inside the alveolar or respiratory membrane.
Muscle contrations in the lungs cause
pressure changes in the thorax that force air in and out of the lungs
When the volume of the thoracic cavity increases
pressure in the thorax decreases
When the volume of the thoracic cavity decreases
pressure in the thorax increases
When pressure in the chest is less than atmospheric pressure
inspiration will occur
When pressure in the chest is greater than atmospheric pressure
expiration will occur
Muscular process of inhalation:
1. diaphragm contracts
2. external intercostal muscles pull ribs up
3. this increases pressure in the thoracic cavity
4. pressure in the lungs decreases below atmospheric pressure
5. Air flows in the equalise
Muscular process of exhalation:
1. diaphragm muscles relax
2. internal intercostal muscles pull ribs down
3. abdominal muscles contract
4. decreases volume of thoratic cavity
5. pressure in lungs increases above atmospheric pressure
6. air flows out
Causes of lung cancer:
smoking, passive smoking, air pollution, radon gas, asbestos and silica
Consequence of lung cancer
death, metastasis, blood, wheezing etc.
Emphysema
a condition in which the air sacs of the lungs are damaged and enlarged, causing breathlessness.
causes of emphysema
smoking or second hand smoking
consequences of emphysema
reduced surface area in alveoli, difficulty breathing, volume of alveoli increases
Spirometery
measuring the volume and / or flow at which air can be inhaled or exhaled
Neuron
a specialized cell transmitting nerve electrical impulses; a nerve cell.