Chapter 15: Microbial Mechanisms of Pathogenicity
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
Pathology
study of the cause of disease
Etiology
study of disease
Pathogenesis
multiplication of any parasitic organisms
Infection
development of disease
disease
Disturbance in the state of health where
the body can’t carry out all of its normal
functions
Signs of disease
Objective and measurable
Directly observed by a clinician
Changes in any vital signs may be indicative of disease
Symptoms of Disease
• Subjective
• Felt or experienced by a patient but cannot be confirmed or measured.
• Changes in any vital signs may be indicative of disease
Syndrome
A specific group of signs and symptoms
Infectious disease
caused by infectious agents
Noninfectious disease
caused by some other factor - for example a poison
Communicable or contagious diseases
Can be spread from host to host - measles, hepatitis
Non-communicable disease
cannot be spread from host to host - food poisoning, tetanus, Legionellosis
Iatrogenic disease
contracted as the result of a medical procedure
Nosocomial disease
acquired in hospital settings
Zoonotic disease
transmitted from animals to humans
Subclinical disease
no noticeable signs or symptoms
(inapparent infection)
stages in the course of an infectious disease
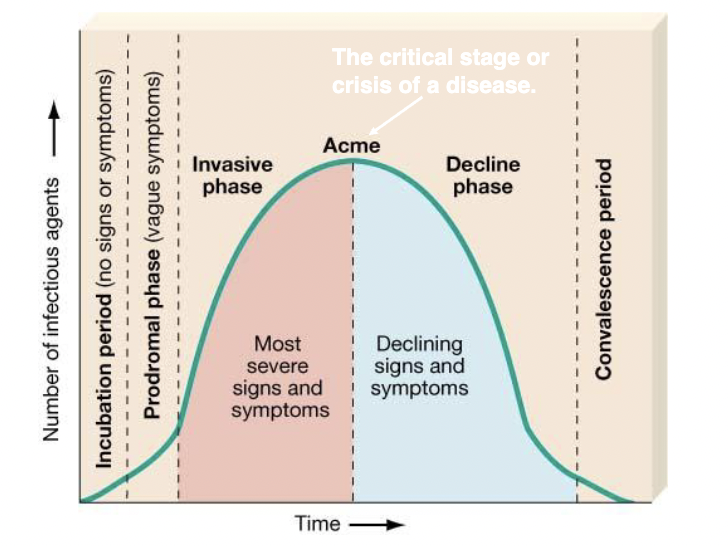
acute disease
disease where symptoms that develop rapidly
chronic disease
disease develops slowly
subacute disease
symptoms between acute and chronic
latent disease
disease with a period of no symptoms when the causative agent is inactive
Koch’s postulates
**cannot be applied to all pathogens
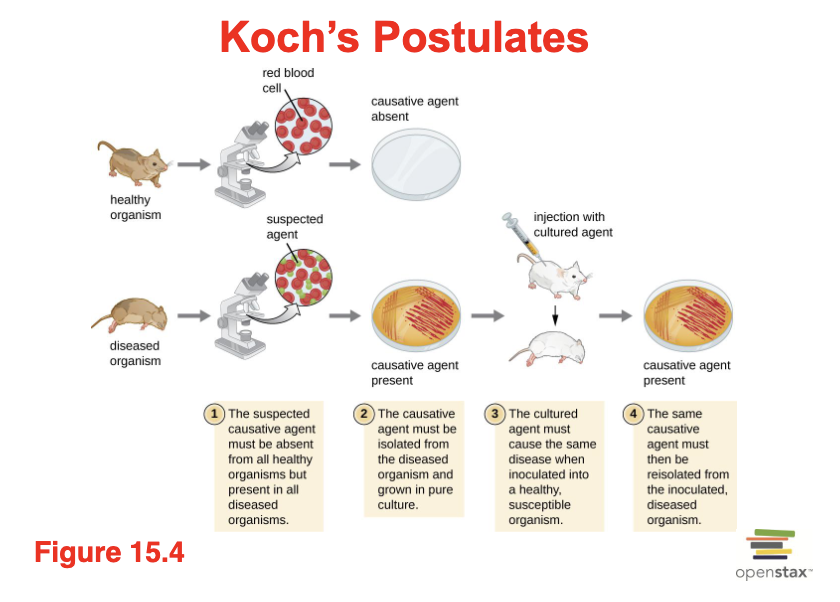
Limitations to Koch’s postulates
Postulate 1, assumes that pathogens are only found in diseased, not healthy, individuals
Koch’s postulate made the assumption that all healthy test subjects are equally susceptible to disease
Koch also assumed that all pathogens are microorganisms that can be grown in pure culture (postulate 2) and that animals could serve as reliable models for human disease
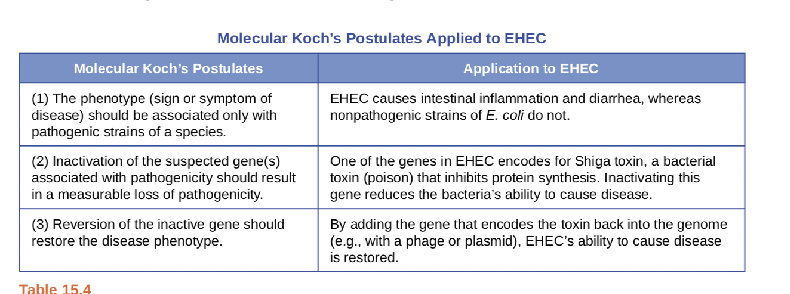
Molecular Koch’s postulates applied to EHEC
created by Stanley Falkow - 1988
• Premise is not the ability to isolate a particular pathogen but rather to identify a gene that may cause the organism to be pathogenic
Pathogenicity
Capacity to produce disease – what does it depend on?
Virulence
intensity of the disease produce by the pathogen
Attenuation
weakening of the disease-producing ability of the pathogen
Virulence factors
Have a negative impact on the host
enable a host to replicate and disseminate within a host in part by subverting or eluding host defenses.
Lead to an increase of mortality rate
Enable competition between microorganisms
Median infectious dose (ID50):
is the number of pathogen cells or virions required to cause active infection in 50% of inoculated animals
Median lethal dose (LD50):
the number of pathogenic cells, virions, or amount of toxin required to kill 50% of infected animals
Primary pathogen
pathogen that always causes disease
Opportunistic pathogen
can only cause disease when the host’s defenses are compromised
Steps of pathogenesis
exposure or entry
adhesion (tissue attachment and colonization)
invasion
infection/ host damage
pathogen exit
**pathogens are characterized by the presence of virulence factors
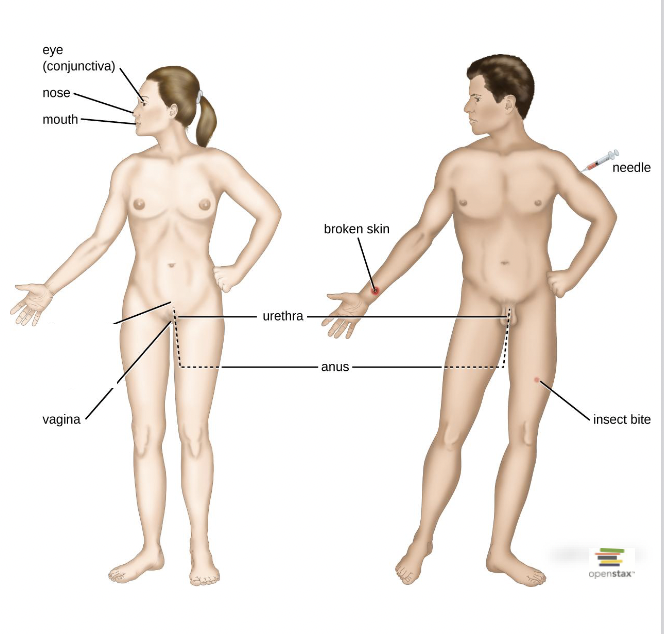
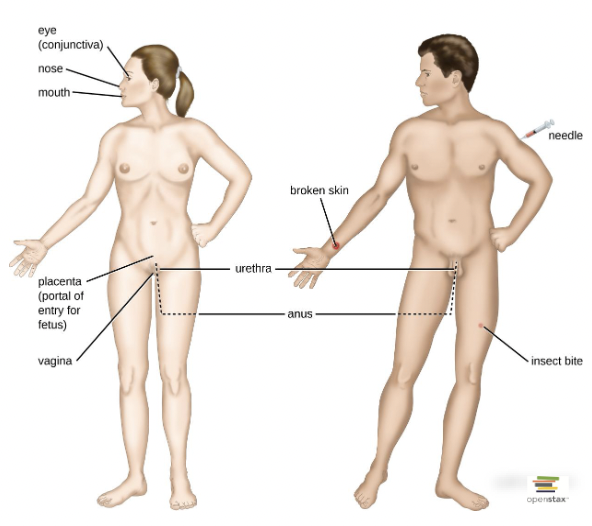
Portals of entry into the host
How do organisms cause disease once they enter the host?
Virulence Factors:
1. Adhesion molecules
2. Toxins and superantigens
3. Enzymes
Examples of Virulence factors
o Bacterial Pili
o Enzymes that harm the host or prevent detection
o Proteins that disrupt normal cellular function
o Capsules
o Enzymes that inactivate antibiotics
What happens once the microorganisms enter the host?
• In order to colonize or penetrate the body surfaces/organs, microorganisms first need to attach the surface (adhesion)
Adhesion
Ability of a pathogen to attach to the cells using adhesion factors (adhesins)
Where are adhesins/ ligands located on the pathogen?
Can be proteins or lipids and are present on:
• Pili
• Flagella
• Cilia
• Capsids
• Membranes of viruses
2. Can be hooks and barbs
3. Can be spike proteins on viruses
4. Can be glycocalyces – slime layers and capsules
5. Biofilm growth can also act as an adhesion factor.
Examples of adhesins on microorganisms
• Glycocalyx: Streptococcus mutans
• Fimbriae: Escherichia coli
• M protein: Streptococcus pyogenes
What happens once microorganisms attach to their target cells?
1. Remain attached to the cell surface – e.g. Taenia saginata
2. Fuse with the host cell membrane.
3. Be internalized into the host cell
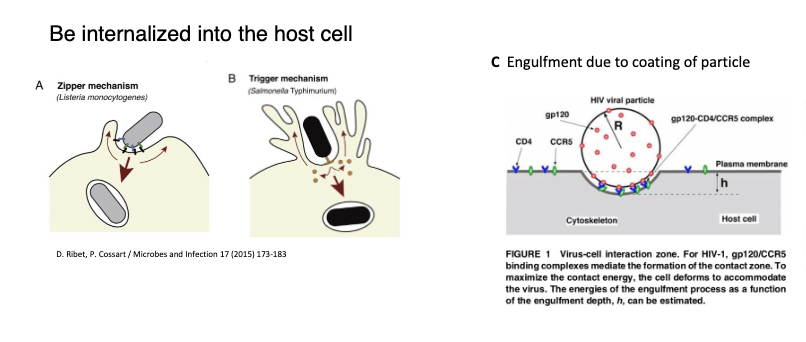
How are microorganisms internalized into the host cell?
Zipper mechanism
Trigger mechanism
engulfment due to coating of particles
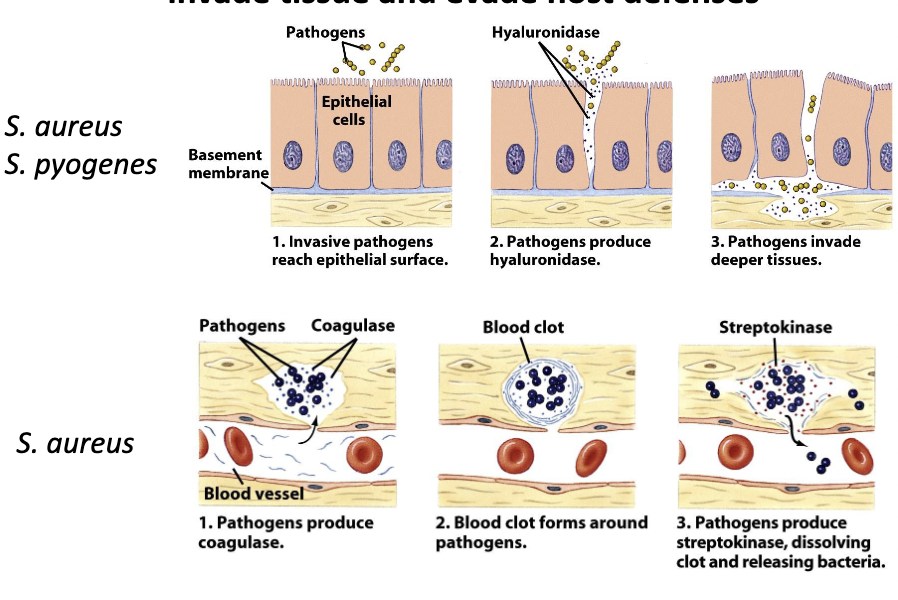
Exoenzymes
Enzymatic virulence factors help bacteria
invade tissue and evade host defenses
Examples of exoenzymes and their targets
Toxin
substance that contributes to pathogenicity
Toxigenicity
ability to produce a toxin
Toxemia
presence of toxin in the host’s blood
Toxoid
inactivated toxin used in a vaccine
Antitoxin
antibodies against a specific toxin
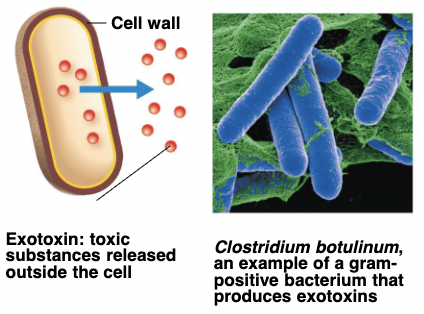
Exotoxins
proteins produced inside pathogenic bacteria, most commonly gram- positive bacteria, as part of their growth and metabolism. The exotoxins are then secreted into the surrounding medium during log phase
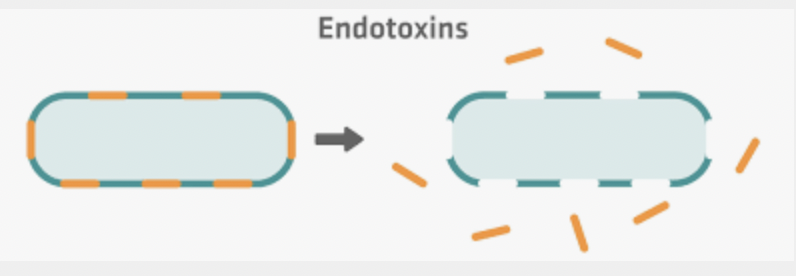
Endotoxin
Lipid portion of lipolysaccharides (LPS) that are part of the outer membrane of the cell wall of gram- negative bacteria- they are liberated when the bacteria die and the cell wall breaks apart. (ex. Salmonella typhimurium)
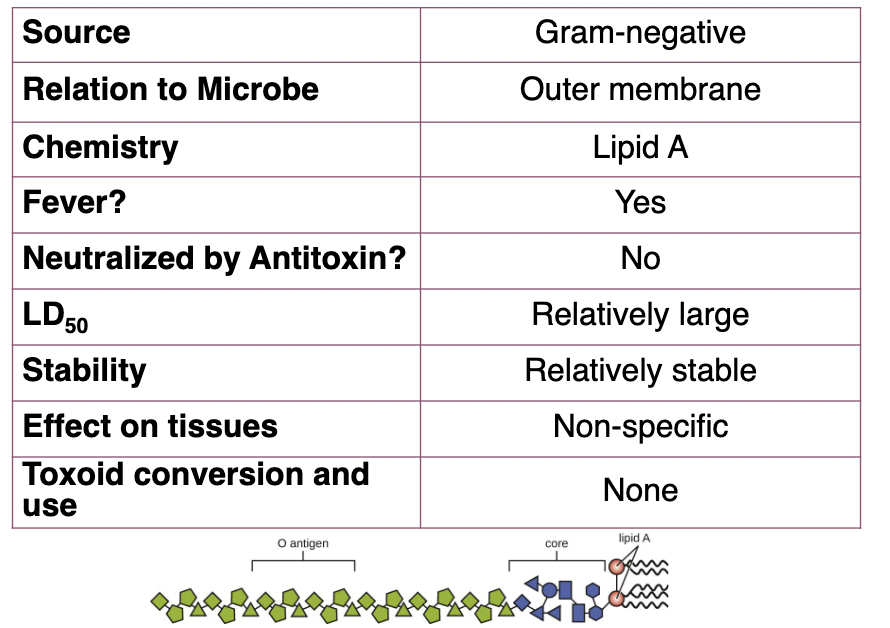
Characteristics of endotoxins
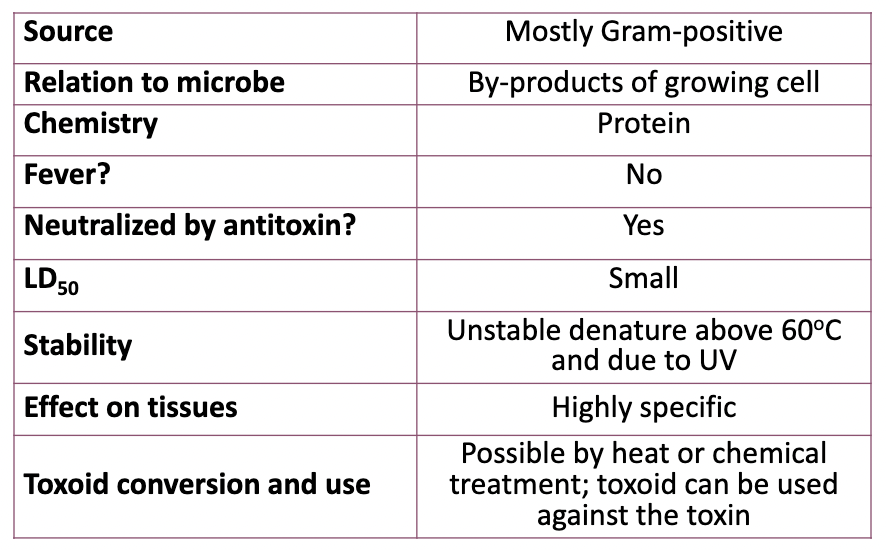
Characteristics of Exotoxins
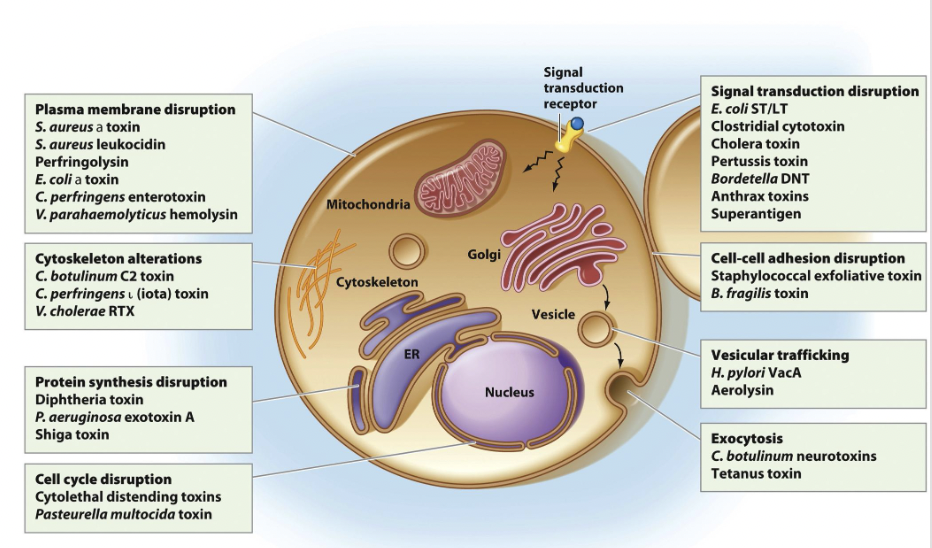
Examples of toxins and how they act
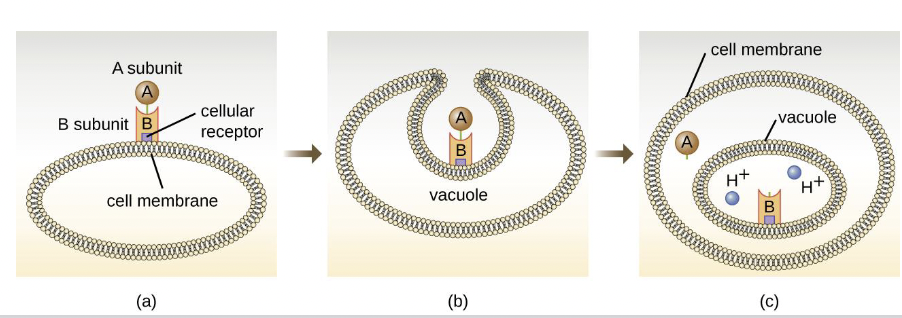
Two- Subunit AB Toxins
• A subunit is toxic.
• B subunit binds host cell receptors.
• Many B subunits are complexes of 5 units arranged as a ring.
• ADP-ribosyltransferase inactivates or alters target proteins.
Successful multiplication of the pathogen leads to
infection
Primary infection
acute infection that causes the initial illness
Secondary infection
opportunistic infection after a primary (predisposing) infection
Local infection
pathogens are limited to a small area of the body
Systemic infection
an infection throughout the body
Focal infection
systemic infection that began as a local infection
Sepsis
toxic inflammatory condition arising from the spread of microbes, especially bacteria or their toxins, from a focus of infection
Bacteremia
bacteria in the blood
Septicemia
growth of bacteria in the blood
Toxemia
toxins in the blood
Viremia
viruses in the blood
How pathogens survive within a host
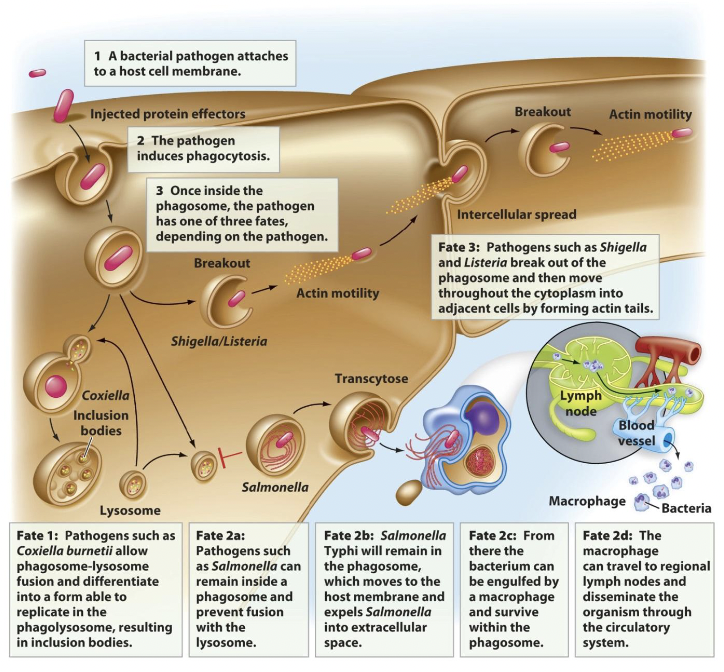
Examples of extracellular immune avoidance
capsules
cell-surface proteins
quorum sensing
Capsules
coat bacterial cell walls and can prevent
phagocytes from binding
Cell-surface proteins
components of the cell wall that prevent detection
• Bind to Fc region on antibodies
• Alter their antigens to avoid antibody binding
Quorum sensing
used to communicate with other pathogens about population size
Antigenic Variation (ex. rhinovirus)
100 known serotypes of rhinovirus; each virus has a unique capsid protein. Antibodies to one capsid protein are not effective on another
Antigenic shift (ex. influenza)
Two strains of influenza virus infect the same cell and the genomes get mixed. This makes a dramatically different virus
Antigenic drift
Random mutations can occur within the cell that a virus infects creating small changes in virus proteins
Latent Herpes Virus
Herpes virus goes into latency and incorporates it’s genome into the host cell.
During periods of stress, the virus re-circularizes and reactivates causing lesions.
• Small RNA molecules called microRNAs (miRNA) are made by herpes virus that interfere with the host cell’s apoptosis program.
• During this process, no viral proteins are made to avoid immune detection
Examples of protozoan pathogenesis
antigenic masking
antigenic variation
intracellular location
immunosuppression
antigenic masking
Some protozoans coat themselves in host antigens to avoid detection by the immune system
antigenic variation
Just like viruses and bacteria, some protozoans can alter their surface antigens to prevent antibody binding
Intracellular Location
Just like some bacteria, protozoans have found ways to live inside the host cell to prevent detection.
Immunosuppression
Some protozoans induce the secretion of anti-inflammatory cytokines to reduce the innate immune response
Exits pathogens use from host