patho (Fluid, Electrolyte, & Acid-Base Homeostasis)
1/154
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
155 Terms
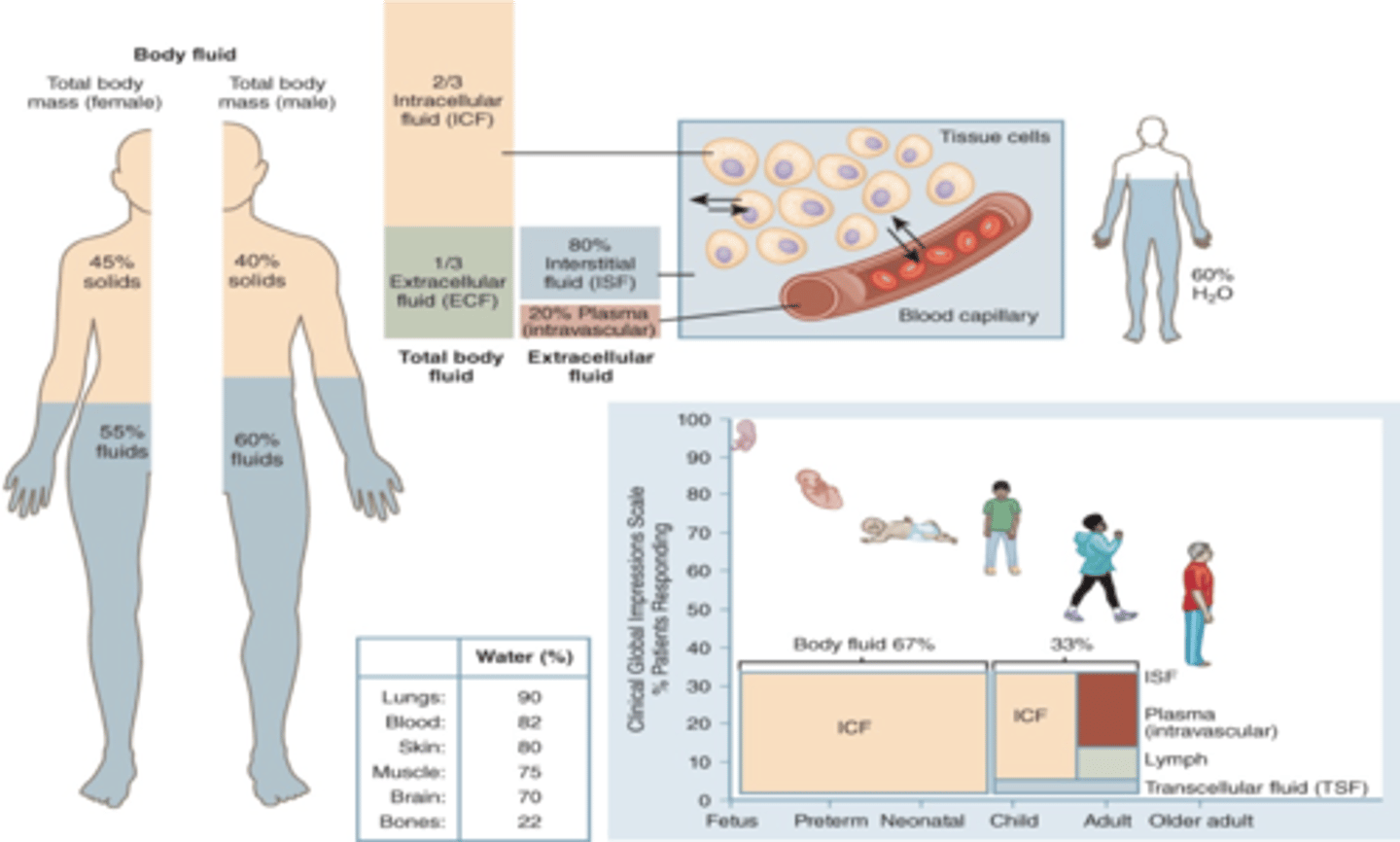
males compared to females have ________% more solids and ________% less fluids
5; 5. men total 40 solid 60 fluid. (remember this bc men have more muscle than fat compared to women and muscle cells store water unlike fat cells
Fluids, electrolytes, and pH all share a dynamic relationship in which imbalances in one area can cause imbalances in the other two. Additionally, the other areas can serve to ________ for those imbalances. When compensatory mechanisms fail to reestablish homeostasis, many bodily functions are impaired, and serious consequences can result. In such a case, medical interventions will be necessary to reestablish stability.
compensate
Newborns and infants have less body fat, so they have higher amounts of water compared to adults. While water levels may be high in this age group, their compensatory mechanisms are immature, so water losses (e.g., vomiting and diarrhea) can have serious consequences. The amount of body water decreases as the child ages until ______, at which time adult ratios are reached. With ____, both adipose tissue and muscle mass often decrease. Additionally, compensatory mechanisms decline with ____. ______, regardless of age, results in lower body water. Due to all of these factors, those individuals who are obese, very young, or very old are more susceptible to fluid imbalances, especially dehydration.
puberty, age, age, obesity
____________ fluid: fluid inside the cells primarily defined as _____
The ________________ _______ serves as a barrier through which substances and water must pass to move to or from this component
Intracellular fluid (ICF), cytoplasm
plasma membrane
____________ fluid: fluid outside the cells
Interstitial fluid (ISF): _____ the _____
Intravascular fluid: _____ the ______ ______
Transcellular fluid (TSF): (i.e., CSF; pleural/pericardial/peritoneal cavities; joint spaces, lymph, eyes, GI tract)
Extracellular fluid (ECF)
between the cells
inside the blood vessels
___ is 40% of body weight and is rich in potassium, magnesium, and proteins. ___ is rich in sodium, chloride, and bicarbonate (80% of this is ___ 20% is ____ composed of plasma) transcellular fluid is 1% of body fluid
intracellular fluid (ICF), extracellular fluid (ECF), interstitial fluid (ISF), intravascular fluid (IV)
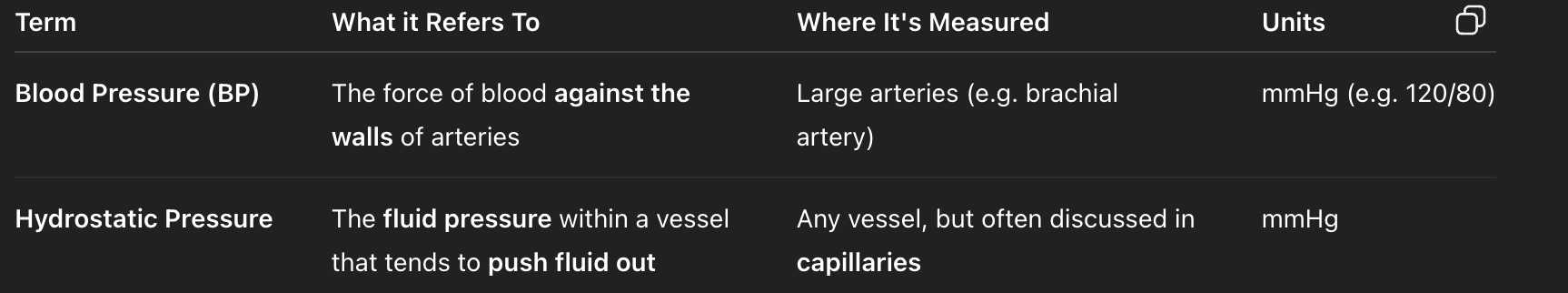
osmolarity vs osmosis
Osmolarity is the concentration of solute particles in a solution, it affects
osmosis which is the process of water diffusion from an area of low solute concentration to an area of high solute concentration.
osmosis depends on hydrostatic (push or pull?) like BP and osmotic (push or pull?) pressures like water moving from low to high solute conc
Hydrostatic pressure () fluid out of the capillary, osmotic pressure draws () it back in
push, pull
Hydrostatic pressure PUSHES fluid out of the capillary, osmotic pressure draws PULLS it back in
___________: osmotic pressure of two solutions separated by a semipermeable membrane; capability of a solution to modify the volume of cells by altering their water content. The effect of a solution on cell volume
____________ solutions: same conc in and out the cell no fluid shift
In ________ osmolality, extracellular fluid (blood/plasma) having equal solute as inside the cells
____________ solutions: lower solute concentrations outside the cell, causing fluids to shift out of the intravascular compartment into intracellular space
In ________ osmolality, solute concentration in cells is greater than in blood aka extracellular fluid (blood/plasma) having less solute than inside the cells
___________ solutions: higher solute concentration outside the cell compared to inside the cell. This causes fluid to shift out of the cell, into the intravascular space
In _______ osmolality, solute concentration in cells is less than in blood aka extracellular fluid (blood/plasma) having more solute than inside the cells
Tonicity
isotonic
hypotonic
Hypertonic
iso,hyper,hypo
difference between osmosis and diffusion?
osmosis is water going across a semipermeable membrane from low to high to dilute for equilibrium. diffusion is particles going from high to low for equilibrium
Osmotic pressure is regulated by the plasma protein ________
Albumin. read the image!
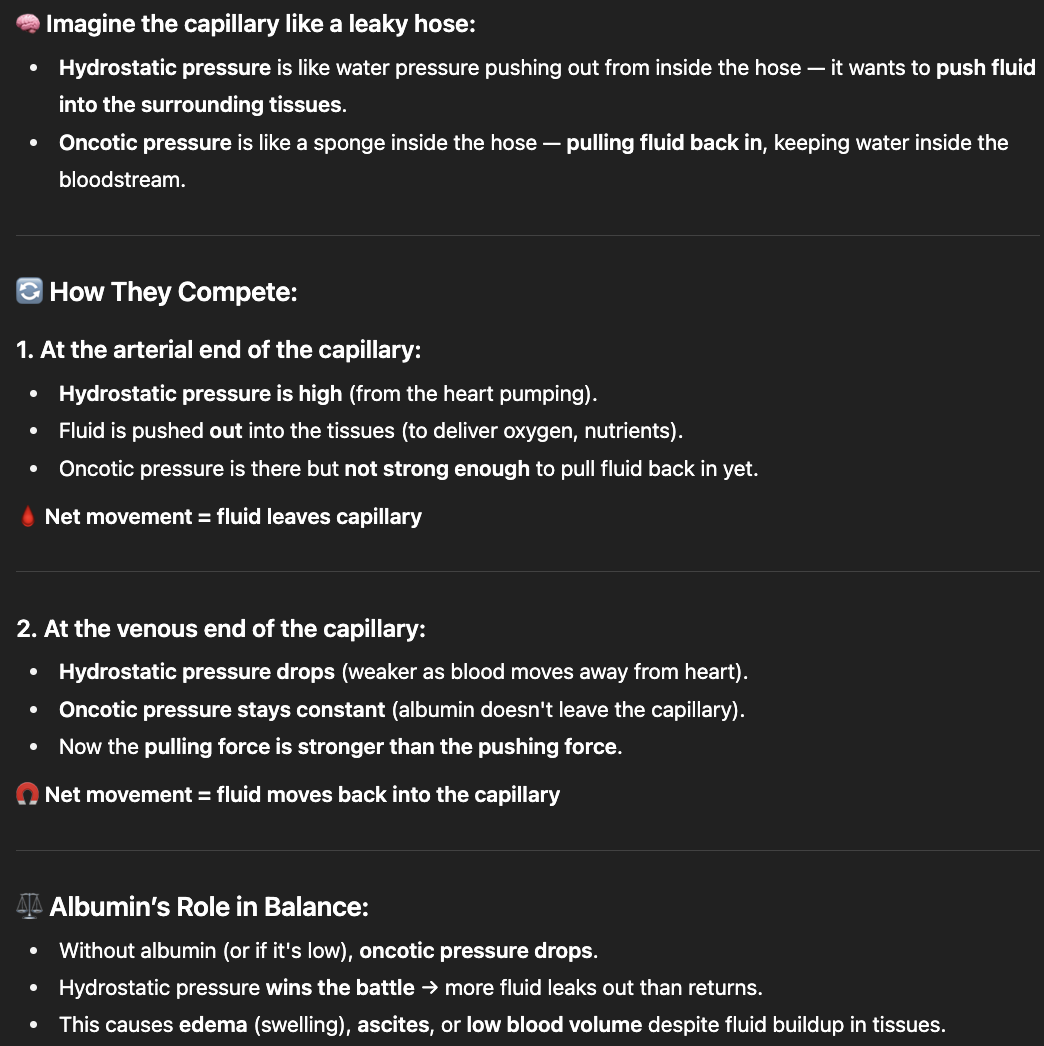
in the _______ end, blood pressure is higher than osmotic pressure bc it is close to the strongly pumping heart and net pressure is pushing OUT away from heart
At this end of a capillary, blood pressure (hydrostatic pressure) is higher than osmotic (oncotic) pressure because the blood is freshly pumped from the heart — it's still under the strong pressure wave generated by ventricular contraction
oncotic pressure is a type of osmotic pressure specific to proteins(ex albumin sponges for capillary
Arterial
in the _______ end, osmotic pressure is higher than blood pressure and net pressure is IN toward the heart
At this end, low blood/hydrostatic pressure allows oncotic/osmotic pressure to dominate, so fluid returns to the capillary.
oncotic pressure is a type of osmotic pressure specific to proteins(ex albumin sponges for capillary
Venous
In health care, the external solution described in relation to tonicity is an intravenous solution—specifically, IV solutions containing electrolytes (crystalloids) and other solutes (e.g., glucose) that are used to treat a variety of patient conditions (e.g., dehydration and shock). These solutions are classified based on their tonicity as either isotonic, hypotonic, or hypertonic
yay
fluid sources (oral intake or IV solutions) can be iso-, hypo-, or hypertonic
oooo
2 Sensible fluid losses
2 Insensible fluid losses
Urine and stool (measurable)
Sweat and respiration (immeasurable)
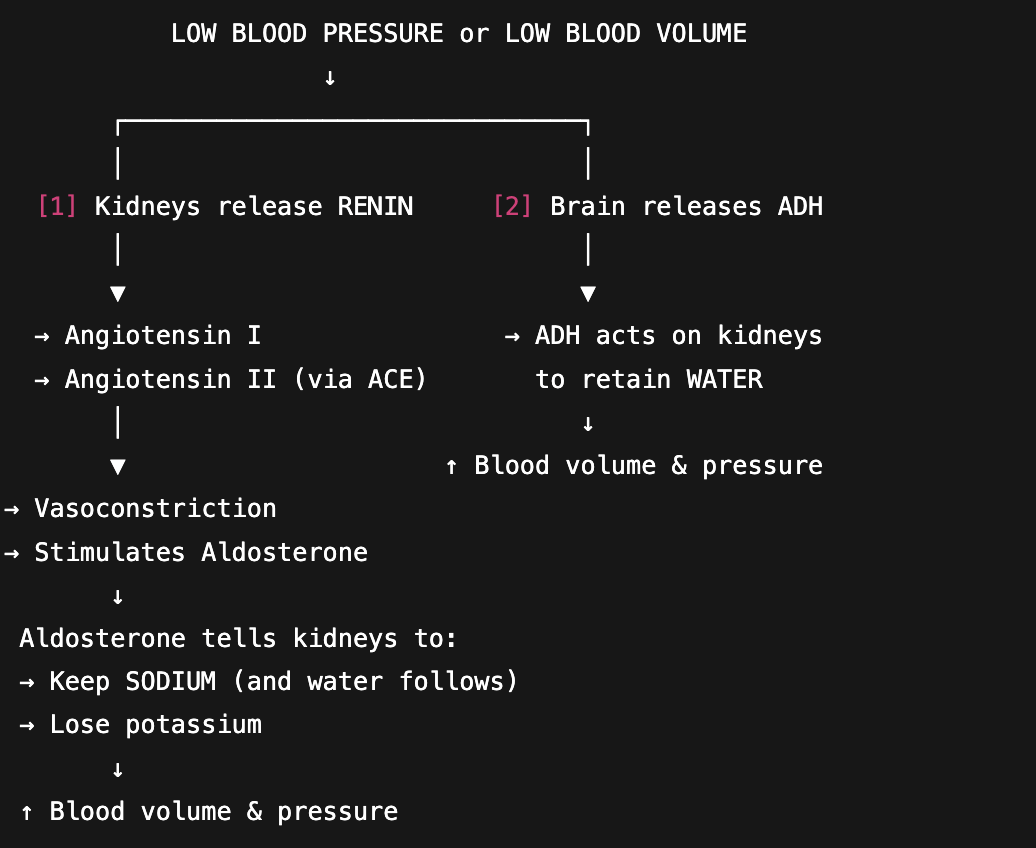
ADH keeps water
Aldosterone thus RAAS keeps sodium and dumps potassium
ADH stops water losses through urine. Released from the pituitary gland in times of decreased fluid volume and increased osmolarity, ADH promotes the reabsorption of water into the blood from the renal tubules.
aldosterone hormone tells kidneys to increase reabsorption of sodium … increases blood volume bc water stays as well to balance the salty conc
aldosterone is part of RAAS (left side of image chart) ADH is not
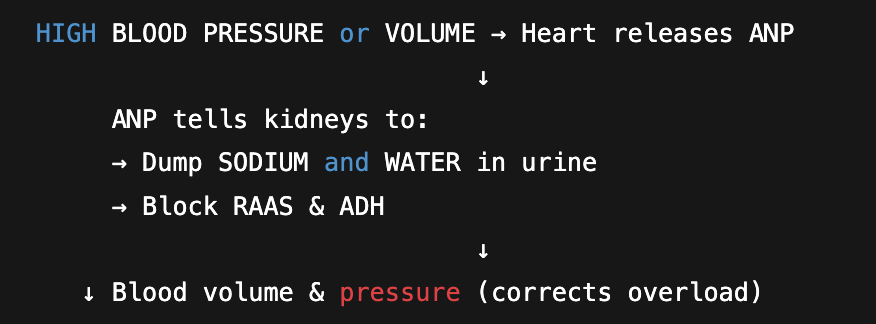
ANP is released when the atria of the myocardium become overstretched, indicating increased fluid volume. This peptide stimulates renal vasodilation, thereby increasing urinary output. Additionally, atrial natriuretic peptide suppresses aldosterone secretion and STOPS RAAS, further increasing urinary output.
Decreased fluid volume or increased osmolarity (solute concentration) triggers the thirst mechanism in the (), which prompts the individual to increase oral intake of fluids.
-one of the best regulators of water balance
This thirst sensation can decrease with age, a phenomenon called ()
hypothalamus
hypodispia
Fluid excess is referred to by several names depending on the compartment affected by poor fluid distribution. when it is excess fluid in interstitial space ______ this is an issue with fluid distribution not always overload and anasarca is the word for generalized this, excess fluid in intravascular space _______ this is from excessive sodium or water intake w insufficient water losses to compensate, in intracellular space ______ this may lead to lysis of cell w cerebral cells being most sensitive to this
edema; hypervolemia; water intoxication
what causes Hypervolemia? Excessive _______or______ intake and insufficient _______or______ losses
Excessive sodium/water intake and insufficient sodium/water losses
Polydipsia
excessive thirst
What can cause excessive sodium or water intake?
-High-sodium diet
-Psychogenic polydipsia (drinking too much water bc anxiety or ocd or schizophrenic bc your mind thinks u need it not bc any somatic reason)
-Hypertonic fluid administration
-Free water
-Enteral feedings
-High-sodium diet
-Psychogenic polydipsia (drinking too much water bc anxiety or ocd or schizophrenic bc your mind thinks u need it not bc any somatic reason)
-Hypertonic fluid administration
-Free water
-Enteral feedings
What can cause inadequate sodium/water elimination? (3 ____ failure and 3 conditions
-Hyperaldosteronism
-Cushing's syndrome (a condition w excessive corticosteroids, which act like aldosterone)
-Syndrome of inappropriate antidiuretic hormone (excessive ADH)
-Renal failure (kidney unable to eliminate fluid or waste)
-Liver failure (less albumin→fluid leaks out of blood vessels into tissues causing edema→low blood volume so RAAS is activated→fluid overload but poor distribution→worse edema
-Heart failure (unable to pump effectively so less blood to kidney)
Manifestations of fluid excess
Rapid weight _____
Anasarca/Peripheral/periorbital/cerebral ___
______ fontanelles (in infants)
🫁
____pnea
_______ thus pulmonary _____
❤
______ pulse
_____cardia
____JV (flat or distended)
____BP
___heart sound
🚽
____uria
anorexia
nausea
🧠
changes in LOC (level of consciousness)
confusion
headaches
seizures
🦵 Edema / Swelling:
Rapid weight gain
Anasarca/Peripheral/periorbital/cerebral edema
Bulging fontanelles (in infants)
🫁 Respiratory:
Dyspnea (shortness of breath)
Crackles (fluid in lungs) thus pulmonary congestion
❤ Cardiac:
Bounding pulse
Tachycardia
Jugular vein distension (JVD)
Hypertension
S3 heart sound
🚽 Kidneys / Output:
Polyuria (pale, high-volume urine)
anorexia
nausea
🧠 Neuro:
changes in LOC (level of consciousness)
confusion
headaches
seizures
What are some cardiovascular effects that can happen from fluid excess?
-bounding pulse
-high BP
-jugular vein distention
-S3 heart sound
-Tachycardia
What are some neurologic effects that can happen from fluid excess?
-changes in LOC (level of consciousness)
-confusion
-headaches
-seizures
What is a respiratory side effect of fluid excess?
Pulmonary congestion
________ and ______ are side Gastrointestinal side effects of fluid excess
Anorexia and nausea
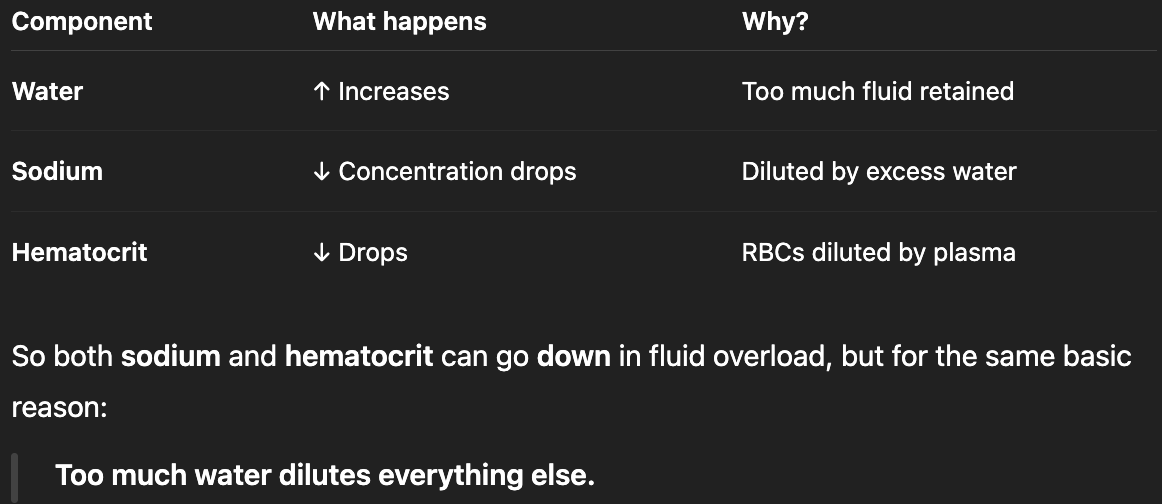
Why would a hematocrit (% of blood that is made up of RBC) on a patient with fluid excess be reduced?
plasma volume (the liquid part of blood) increases.
But # of RBCs stays the same.
So the RBCs become diluted in all that extra fluid.
This makes the percentage of RBCs (hematocrit) go down — even though the actual number of RBCs hasn’t changed.
bc of all the excess fluid, there is more water than sodium, so sodium concentrations will be reduced too
_______ _______: when total body fluid levels are insufficient to meet the body's needs
fluid deficit results in () which is when body loses more fluid than it takes in
Fluid deficit
dehydration
Decreased fluid in the intravascular space
Hypovolemia
does fluid deficit only occur from electrolyte defect?
no, it can also occur independently without electrolyte defects
Decrease in fluid level leads to... (3)
___BP
______conc of blood solutes
cells _____
-increase in level of blood solutes
-cell shrinkage
-hypotension (low BP
what are the 2 causes of inadequate fluid intake? (one is the obvious dietary the other is … in the hospital… the nurse has to do what to IV fluid?
-poor oral intake
-inadequate IV fluid replacement
Excessive fluid or sodium losses can occur from...
GI how?
from skin how?
respiratory how?
bloodhow?
renal how?
🧻 1. Fluid Loss from the GI Tract
Gastrointestinal losses (vomiting, diarrhea, suction)
💦 2. Loss from the Skin or Respiratory System
Excessive diaphoresis (sweating)
Burns
Open wounds
Prolonged hyperventilation (water loss through breathing)
🩸 3. Blood/Plasma Loss
Hemorrhage
Ascites (fluid shifts into the abdomen)/ Effusions (fluid shifts into pleural or pericardial spaces)
These are examples of third-spacing. Fluid shifts out of the vasculature into spaces like the abdomen or pleura. Even though total body water is still present, it’s not in the right place and cannot be used for perfusion thus—your body acts like it's dehydrated
🧠 4. Renal Losses (Kidneys)
Nephrosis (loss of protein and fluid in urine)
Diabetes mellitus (glucose pulls water → osmotic diuresis)
Diabetes insipidus (loss of water due to lack of ADH)
Excessive use of diuretics
Osmotic diuresis
Manifestations of fluid deficit
Neuro(3): _____, altered ____, mood? Cardio: ____BP, ____cardia, ____JV (flat or distended) Resp: _____resp (increased or decreased resp) Renal: ___guria Edema: weight _____, _____fontalles (sunken or bulging), _____ mucous membranes, ____skin turgor aka ________ |
Neuro | Thirst, altered LOC, confusion/restless |
Cardio Resp | low BP, tachycardia, weak pulse, flat JVs increased resp |
Renal | Oliguria |
Edema | Weight loss, sunken fontanelles, Dry mucous membranes, ↓ skin turgor so tenting |
Positively charged electrolytes () negatively are ()
what 3 functions/roles do electrolytes have?
Cations (na,mg,k,ca) anions (chloride and bicarb)
role in homeostasis, muscle and neural activity, acid-base and fluid balance
does the kidney eliminate or reabsorb sodium?
where is sodium found?
what 2 major roles does sodium play as an electrolyte?
reabsorbs
extracellular fluid (ECF)
it regulates fluid volume and neurological function
what 2 major roles does potassium play as an electrolyte?
where is potassium found?
does the kidney eliminate or reabsorb potassium?
-muscle contraction, cardiac conduction
intracellular fluid (ICF)
eliminate
3 major roles of calcium as an electrolyte:
insufficiency in calcium leads to
-bone health, neuromuscular function, cardiac function
osteoporosis
5 major electrolytes
sodium, potassium, chloride, calcium, magnesium
where is magnesium found?
magnesium plays a role in (2)
intracellular fluid (ICF) & in bone tissue
keeping bone healthy and many cellular functions
alcoholism leads to low levels of electrolytes, which one is most affected/decreased
Magnesium
where is chloride found?
chloride binds to
chloride is essential for
extracellular fluid (ECF)
other ions
HCL production (hydrochloric acid)
normal range of sodium
135-145 mEq/L
the most significant cation and prevalent electrolyte in ECF
sodium
what controls serum osmolality and water balance?
Sodium
sodium facilitates muscles and nerve impulses through the ___________________
sodium-potassium pump
main source for sodium is
sodium is excreted through the _____ and ______
does sodium play a role in the acid-base balance?
dietary intake
kidneys and GI tract
yes
__________: increase in membrane potential / less polar
__________: restoration of resting potential / more polar
Depolarization
Repolarization
resting membrane potential
-70mV
really helpful action potential video link
https://www.youtube.com/watch?v=W2hHt_PXe5o
Hypernatremia is when sodium levels are greater than _______ mEq/L
145
2 causes of Hypernatremia. which is more common?
-excessive sodium
-deficient water
usually from water loss not sodium gain. sodium gain is from more unusal things like (too much dietary sodium, cushings, hypertonic IV saline, corticosteroid use)
what are 4 examples of causes that could cause excessive sodium?
-too much dietary sodium
-hypertonic IV saline
-Cushing's
-corticosteroid use
what are 6 examples of causes that could cause hypernatremia from deficient water?
answer me this…. one of the options is either diabetes mellitus or diabetes insipidus… which is it?
-insufficient intake
-third spacing
-excessive output
-prolonged hyperventilation
-diuretic use
-diabetes insipidus
manifestations of hypernatremia:
C- cardiac (____cardia, ____ pulse, BP____,
H- head (fever, flushed skin, headache, seizure)
F- fluid (___(thirsty or dehydrated?), ____ urine output, _____fluid retention, edema, ___ mouth, _____ mucous membranes, ___phagia)
M- mood (______________ at first while neurons start to _________ this can lead to _______ in extreme then ____________ as the neurons _______ this leads to ____in extreme)
cardiac head fluid mood
C- cardiac (tachycardia, thready pulse, BP changes,
H- head (fever, flushed skin, headache, seizure)
F- fluid (thirsty, decreased urine output, increased fluid retention, edema, dry mouth, dry/sticky mucous membranes, dysphagia)
M- mood (restless/irritable/agitated at first while neurons start to excite/shrink this can lead to seizure in extreme then slow/lethargy/weakness as the neurons shut off/lose function this leads to coma in extreme)
hypernatremia pic
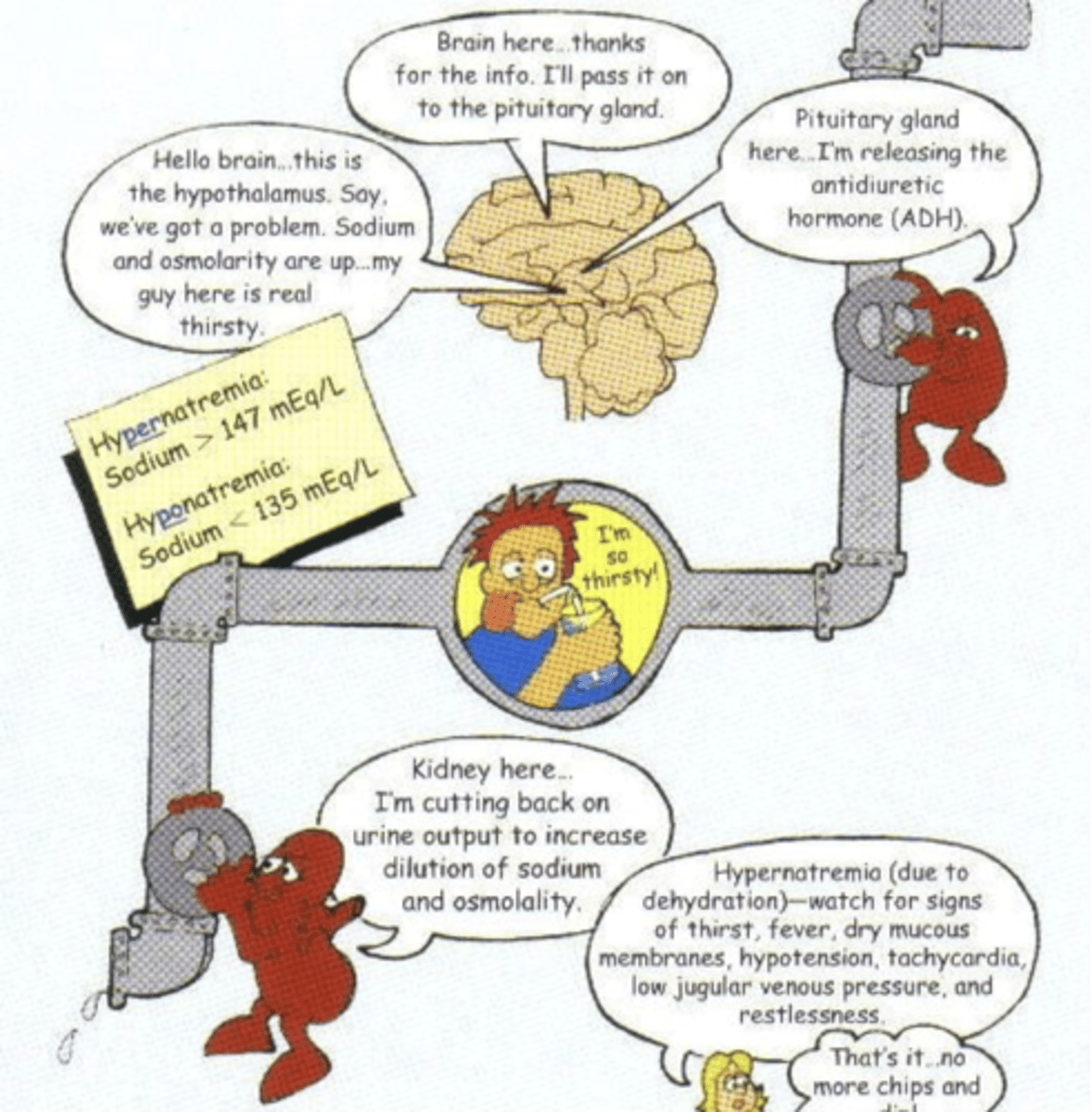
when a patient has hypernatremia, the __________ ________ releases ADH (antidiuretic hormone) to
pituitary gland;
recover water from urine in kidneys to put water back in blood
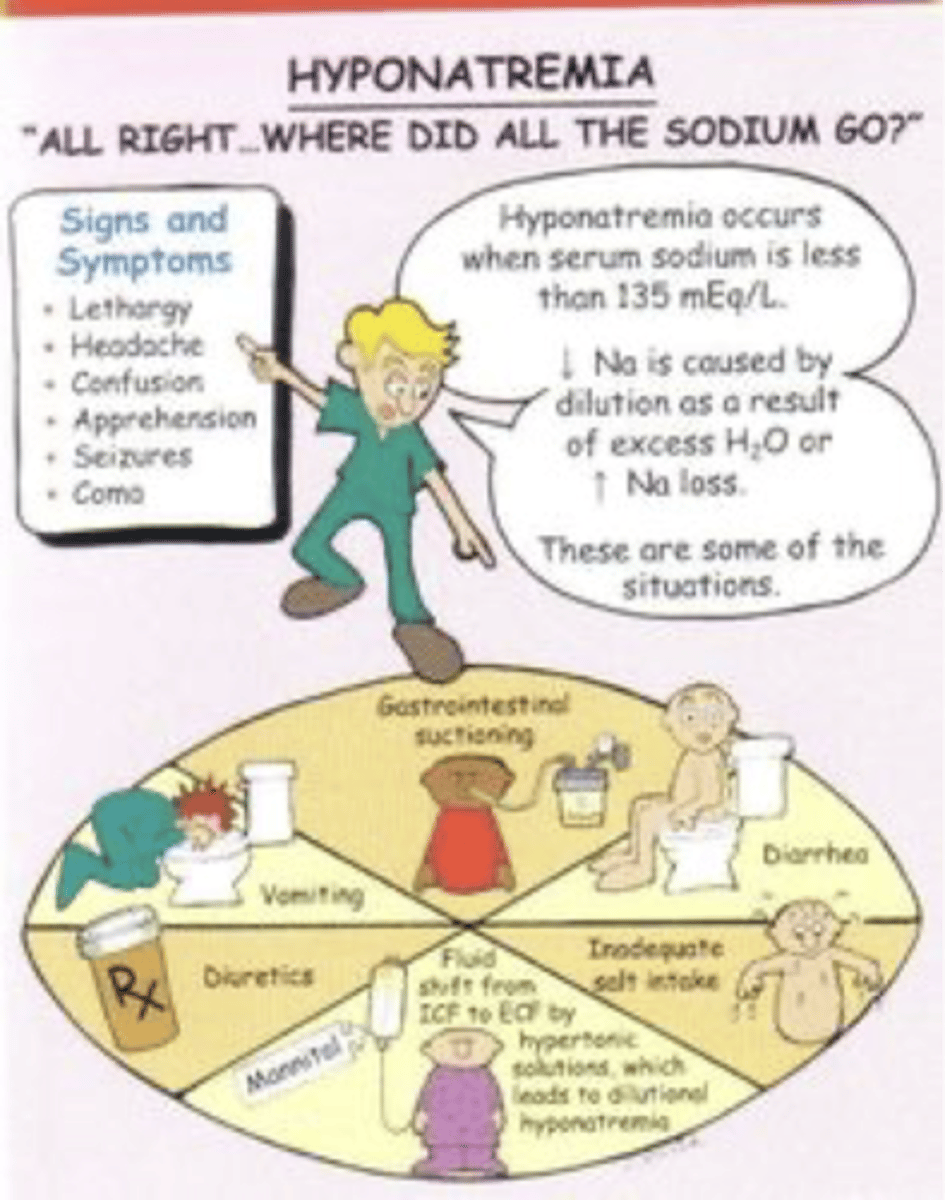
Hyponatremia is when sodium is less than
135 mEq/L
serum osmolarity ___________ in hyponatremia
decreases
2 casues of hyponatremia:
-deficient sodium
-excessive water
Hyponatremia related to deficient sodium can be a result of...
diuretic use,
gastrointestinal losses,
diaphoresis,
insufficient aldosterone,
adrenal insufficiency,
dietary sodium restrictions
what is diaphoresis,
sweating excessively from disease or drug side effect
Hyponatremia related to excessive water can be a result of...
hypotonic IV saline,
hyperglycemia,
water intake,
renal failure,
syndrome of inappropriate antidiuretic hormone,
heart failure
manifestations of hyponatremia:
C- cardiac (_____ BP/pulse)
R- resp (_____ respiration
G- GI (anorexia, abdominal cramping/GI upset
M- muscle weak/spasm/diminished deep tendon reflexes,
F- fluid (edema, dry mucous membranes, skin turgor bad)
N- neuro (coma, seizure, headache, confusion, lethargy)
C- cardiac (changed BP/pulse)
R- resp (shallow respiration
G- GI (anorexia, abdominal cramping/GI upset
M- muscle weak/spasm/diminished deep tendon reflexes,
F- fluid (edema, dry mucous membranes, skin turgor bad)
N- neuro (coma, seizure, headache, confusion, lethargy)
hyponatremia pic
normal chloride electrolyte range
98-108 mEq/L
which electrolyte is a mineral electrolyte and major extracellular anion?
Chloride
__________ can bind and travel with cations (sodium, potassium, calcium)
Chloride
how does chloride assist in fluid distribution?
where is chloride found? (4)
by attaching to water or sodium
-gastric secretions, pancreatic juices, bile, cerebrospinal fluid
what is the main source for chloride?
where is chloride excreted?
chloride plays a role in the acid-base balance when it is bound to
dietary intake;
through the kidneys
hydrogen
hyperchloremia is when chloride levels are greater than ________ mEq/L
2 causes of hyperchloremia:
manifestations of hyperchloremia:
108
-increased chloride intake, decreased chloride excretion
reflect the underlying causes manifestations
hypochloremia is when chloride levels are less than ______ mEq/L
2 causes of hypochloremia:
manifestations of hypochloremia
98
-decreased chloride intake, increased chloride excretion
reflect the underlying causes manifestations
causes of decrease chloride intake (4)
causes of increased chloride intake: (4)
DECREASED CHLORIDE INTAKE
Hyponatremia,
administration of 5% dextrose in water intravenous solution,
water intoxication,
hypokalemia
INCREASED CHLORIDE INTAKE
hypernatremia,
hypertonic intravenous solution,
metabolic acidosis,
hyperkalemia
causes of increase chloride excretion (4)
causes of decreased chloride excretion: (3)
INCREASED EXCRETION
Diuretics, vomiting,other gastrointestinal losses, metabolic alkalosis,
DECREASED EXCRETION
hyperparathyroidism, hyperaldosteronism, renal failure
normal potassium range
3.5-5 mEq/L
The primary intracellular cation
Potassium (K+)
Plays a role in electrical conduction (nervous, musculoskeletal, cardiovascular), acid-base balance, and metabolism
Potassium
main source of potassium
dietary intake
where is potassium excreted?
-kidneys
-GI tract
Serum __________ cannot fluctuate much without causing serious issue.
potassium
Hyperkalemia pic
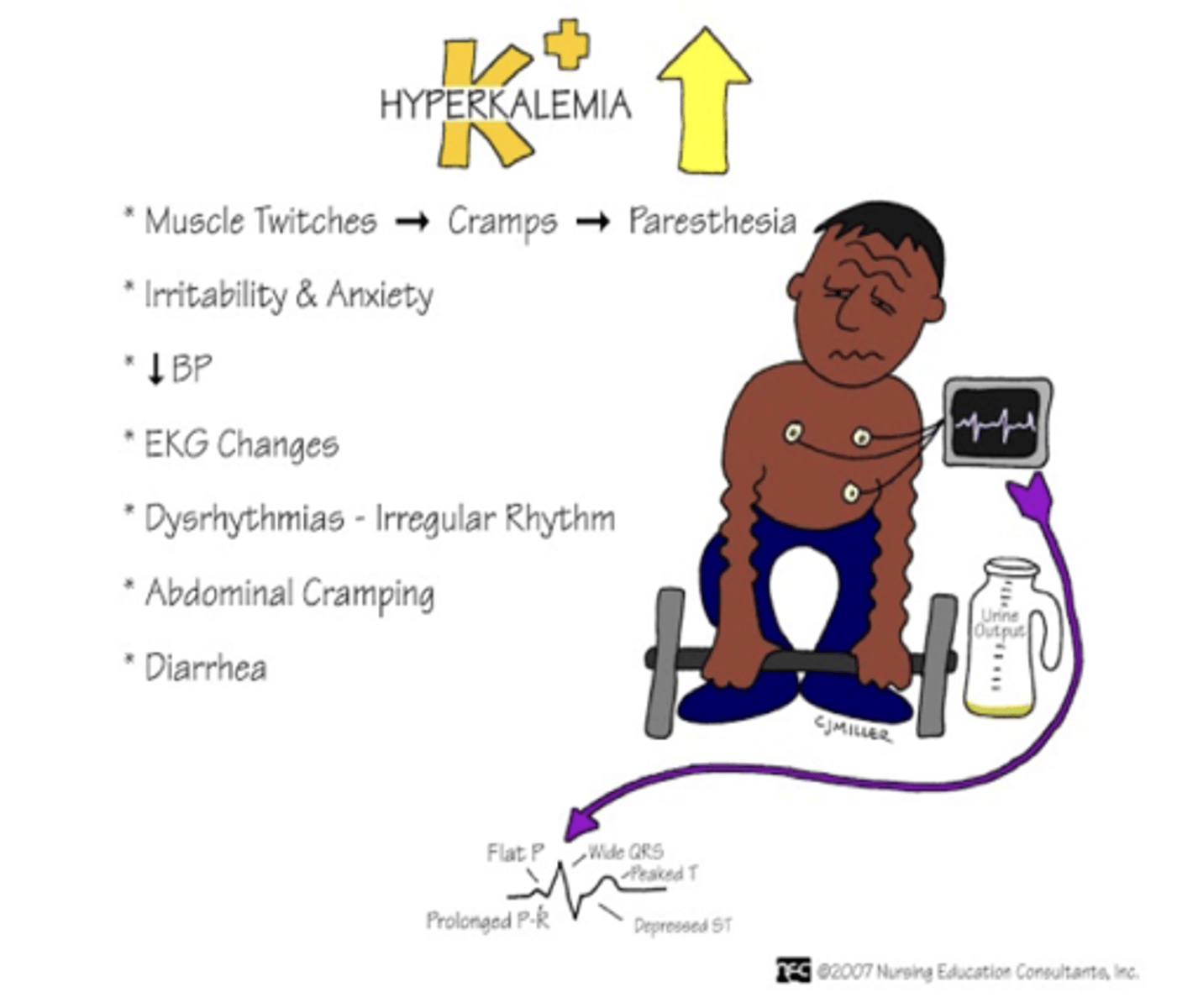
>5 mEq/L
hyperkalemia
3 main causes of hyperkalemia:
-deficient excretion
-excessive intake
-increased release from cells
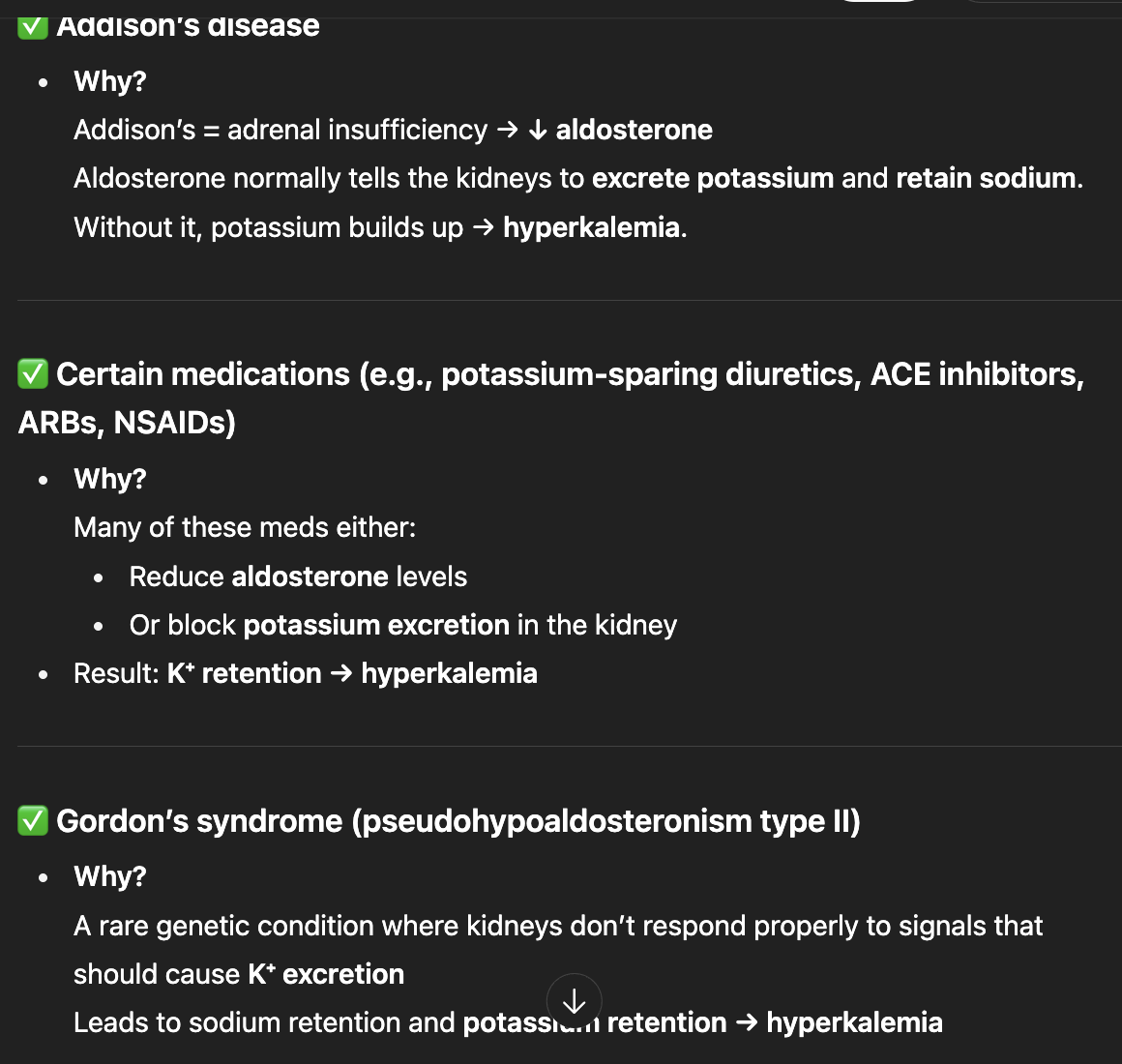
causes of Hyperkalemia through deficient potassium excretion:
renal failure,
Addison’s disease,
certain medications,
Gordon’s syndrome
oral potassium supplements, salt substitutes, rapid intravenous administration of diluted potassium
these are causes of __________ through ______________
excessive potassium intake
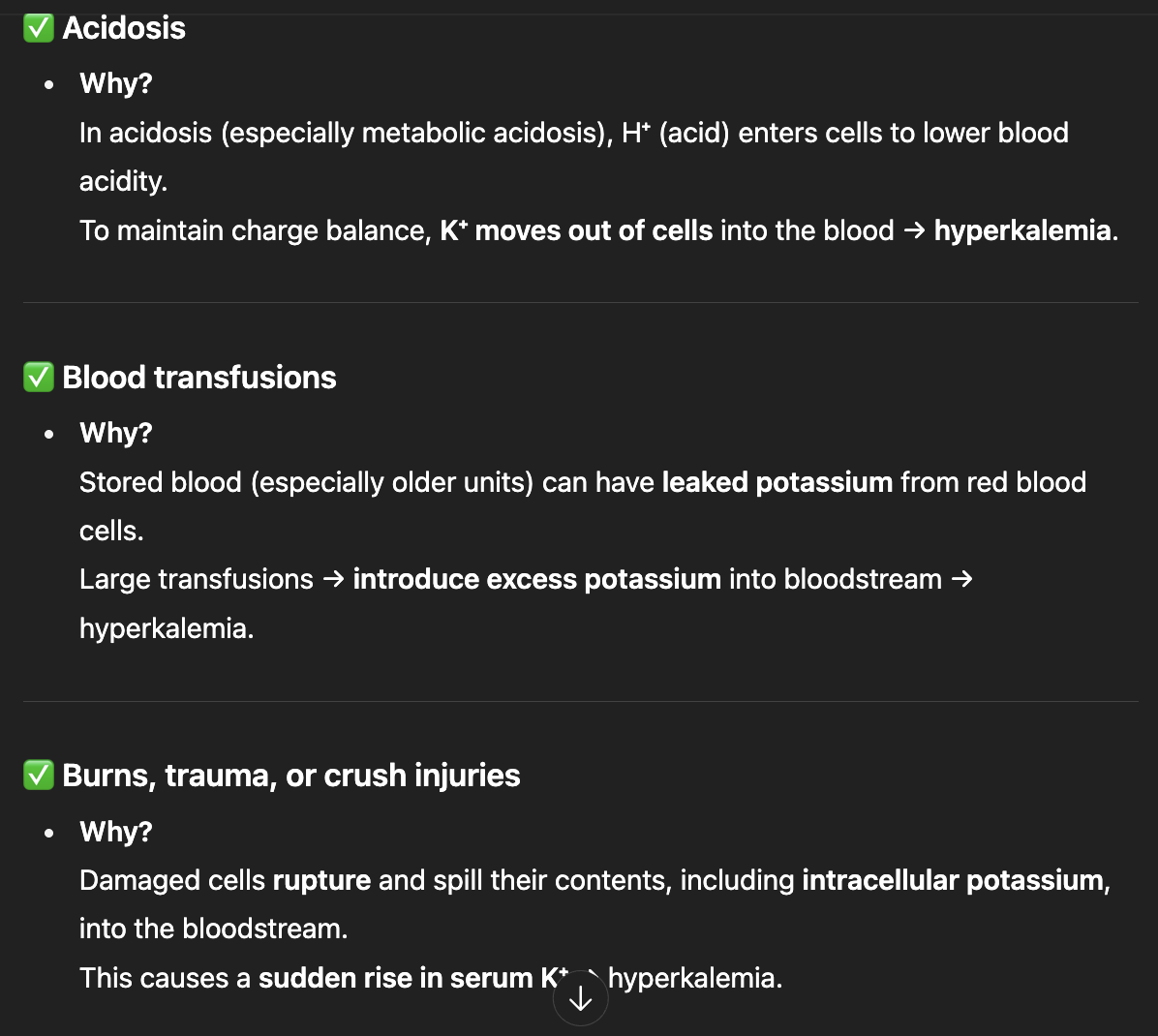
causes of Hyperkalemia through increased release from cells:
acidosis,
blood transfusions,
burns or any other cellular injuries
manifestations of Hyperkalemia:
muscle, resp, cardio, urine, nerve, gastro
M- muscle weakness
R- respiratory rate decrease
C- heart (bradycardia,dysrhythmias, cardiac arrest, EKG changes)
U- urine (oliguria/anuria)
N- nerve(paresthesia,flaccid paralysis, reflexes)
G- gastro (abdominal cramping, nausea, diarrhea)
Potassium <3.5 mEq/L
hypokalemia
3 main causes of Hypokalemia:
-excessive loss
-deficient intake
-increased shift into the cell
some causes of Hypokalemia related to excessive loss:
some causes of Hypokalemia related to deficient intake (3):
causes of Hypokalemia related to increased shift into the cell (2):
vomiting, diarrhea, nasogastric suctioning, fistulas, laxatives, potassium-losing diuretics, Cushing’s syndrome, and corticosteroids
malnutrition, extreme dieting, and alcoholism
alkalosis and insulin excess
manifestations of Hypokalemia:
gut cant move normally
G- GI (contipation, abdomen distended, decrease bowel sound, ileus
C- cardiac (hypotension, thready pulse, arrhythmia, ECG changes, cardiac arrest)
M- muscle (weakness, leg cramp,
N- nerve (paresthesia, light reflexes hyporeflexia, weak, confused, irritable)
normal range of calcium:
4–5 mEq/L
main source of calcium
where is calcium absorbed?
calcium is excreted in
5 roles of calcium
dietary intake
GI tract (small intestine
urine and stool
(5) blood clotting, hormone secretion, receptor functions, nerve transmission, muscular contraction
calcium has an inverse relationship with ___________ and a synergistic relationship with _____________
______________________ aids calcium absorption
what 3 things regulate calcium?
phosphorus;
magnesium
vit D
vitamin K, parathyroid hormone, calcitonin
Calcium >5 mEq/L
hypercalcemia
hypercalcemia causes related to increased intake or release:
hypercalcemia causes related to deficient excretion:
increased intake or release: calcium antacids, calcium supplements, cancer (esp bone but also others), immobilization, corticosteroids, vitamin D deficiency, hypophosphatemia
deficient excretion: renal failure, thiazide diuretics, hyperparathyroidism
manifestations of hypercalcemia
(reflect decreased cell membrane excitability and are often nonspecific. affect cardiac, nervous, musculoskeletal, gastrointestinal, and renal systems )
cardiac | dysrhythmias, EKG changes, high BP, arrest |
|---|---|
GI | Abdominal pain, nausea, vomiting, constipation, anorexia |
Musculoskeletal | Bone pain/weak, muscle weakness, , decreased deep tendon reflexes |
Renal | Renal calculi(kidney stones), polyuria ((high calcium levels interfere with ADH, resulting in increased water excretion), polydipsia, dehydration, pancreatitis |
Neuro | Lethargy, fatigue, malaise, confusion, depression, memory loss, headache, stupor, coma, |
hypocalcemia is levels less than _______ mEq/L
4