Final Review
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
What is Diabetes?
‘Diabetes Mellitus’: inability to maintain glucose and insulin levels in the body. Diabetes is a group of metabolic conditions characterized by a failure to sustain carbohydrate and lipid homeostasis due to disturbances in insulin function, leading to impaired glucose and fat metabolism.
Type 1 Diabetes
(Previously: Juvenile Onset Diabetes/ IDDM) INSULIN DEFICIENCY
Insulin deficiency due to pancreatic β-cell death results in decreased glucose uptake in the tissues and increased hepatic glucose output, as well as increased lipolysis in the adipose tissue.
Type 2 Diabetes
(Previously: Adult Onset Diabetes/ NIDDM) INSULIN RESISTANCE
Insulin resistance that results in decreased glucose uptake in the tissues and increased hepatic glucose output, as well as increased lipolysis in the adipose tissue. DOESN’T MEAN THEY ARE OVERWEIGHT
Type 1 diabetes risk factors
Immune mediated (Genetic)
Type 2 diabetes risk factors
• Hereditary (2x risk if parent has type 2 diabetes)
• Obesity (80% are overweight or obese at onset)
• Abdominal fat distribution
• Age (over 45)
• Sedentary lifestyle
• Hypertension
• Dyslipidemia (inability to regulate blood trigliceride (fat) levels)
Metabolic Syndrome
1. Diabetes
2. Hypertension
3. Obesity
4. Dyslipidemia
Mechanisms that cause Type 2 diabetes
Primary cause: impairments in insulin signaling in the tissue
Insulin is present, but there is compensatory Hyperinsulinemia that eventually leads to β cell exhaustion and insulin deficiency (after many years )
Gradual onset – usually a few years until first symptoms appear
~10% of world population have T2D (many are undiagnosed)Associated with obesity
Prevalence rates are constantly on the rise
Mechanisms that cause Type 1 diabetes
• Primary cause: Immune system attacks the pancreas, causing β-cell death
• Complete insulin deficiency (within a few months)
• In fact, without exogenous insulin, the patient would die within a year
• Acute and fast onset – usually symptoms appear within a few weeks
• ~1% of world population have T1D (~10% of all diabetes cases)
• Prevalence rates are constantly on the rise
What is insulin resistance?
An impaired response of the body to insulin, resulting in elevated levels of glucose in the blood (a key component of type 2 diabetes and metabolic syndrome).
Insulin
Anabolic Hormone
Secreted from pancreatic β cells (Islets of Langerhans) in response to increased blood glucose
High sugar intake stimulates release; no food inhibits release
Effects stomach, liver, skeletal muscle
Major Diabetes Complications
As a result of extended hyperglycemia (uncontrolled diabetes), damage to vessels, nerves, and other cells results in:
• Cardiovascular disease
• Hypertension
• Stroke
• Kidney disease
• Blindness
• Nerve damage
• Amputation
What are the three pillars of diabetes treatment?
Medication, Diet, Physical Activity (all play off on each other and affect one another)
Medications for Type 1 Diabetes
Insulin
MDI (Multiple Daily Injections)
Insulin Pump
Hyperglycemia
Blood glucose > 250 mg/dl
Too little insulin
Polydipsia, Polyuria, Weakness, Impaired Vision, Changes in Mood, ‘Acetone Breath’
Catabolic process utilizing protein as an energy substrate
Ketoacidosis (the body does not have enough insulin to use glucose (sugar) for energy)
Might induce a diabetic coma
Hypoglycemia
• Blood glucose < 60 mg/dl
• Too much insulin
• Confusion, Weakness, Tremor, Cold Sweat, Impaired Vision, Unresponsiveness
• Neuroglucopenia (brain doesn’t have enough glucose)
• Might cause loss of consciousness and death
• Must consume sugar ASAP in order to increase blood glucose levels
Insulin stimulated glucose uptake
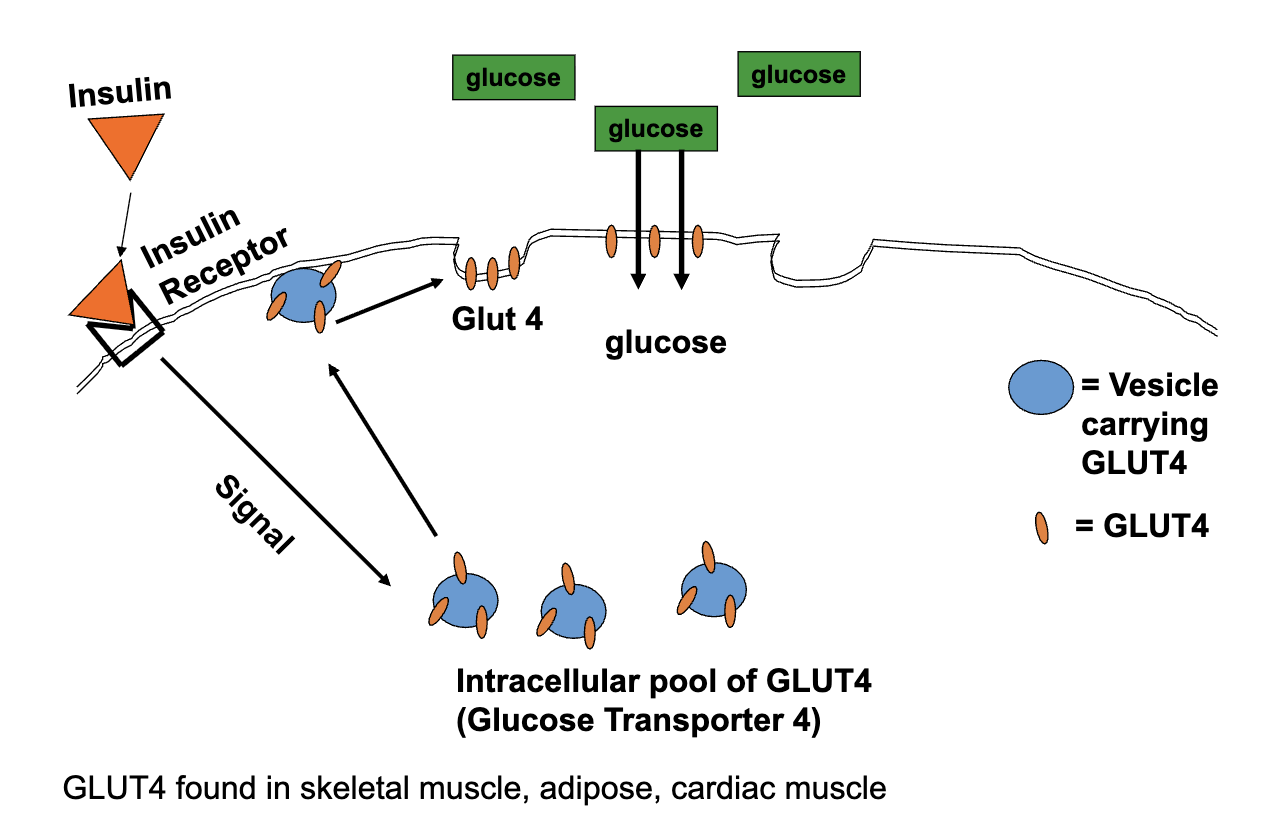
With no Insulin, can tissues uptake glucose?
YES
Glut 1 – continuous low-level uptake
Contraction-mediated Glut 4 Translocation (during skeletal muscle contraction)
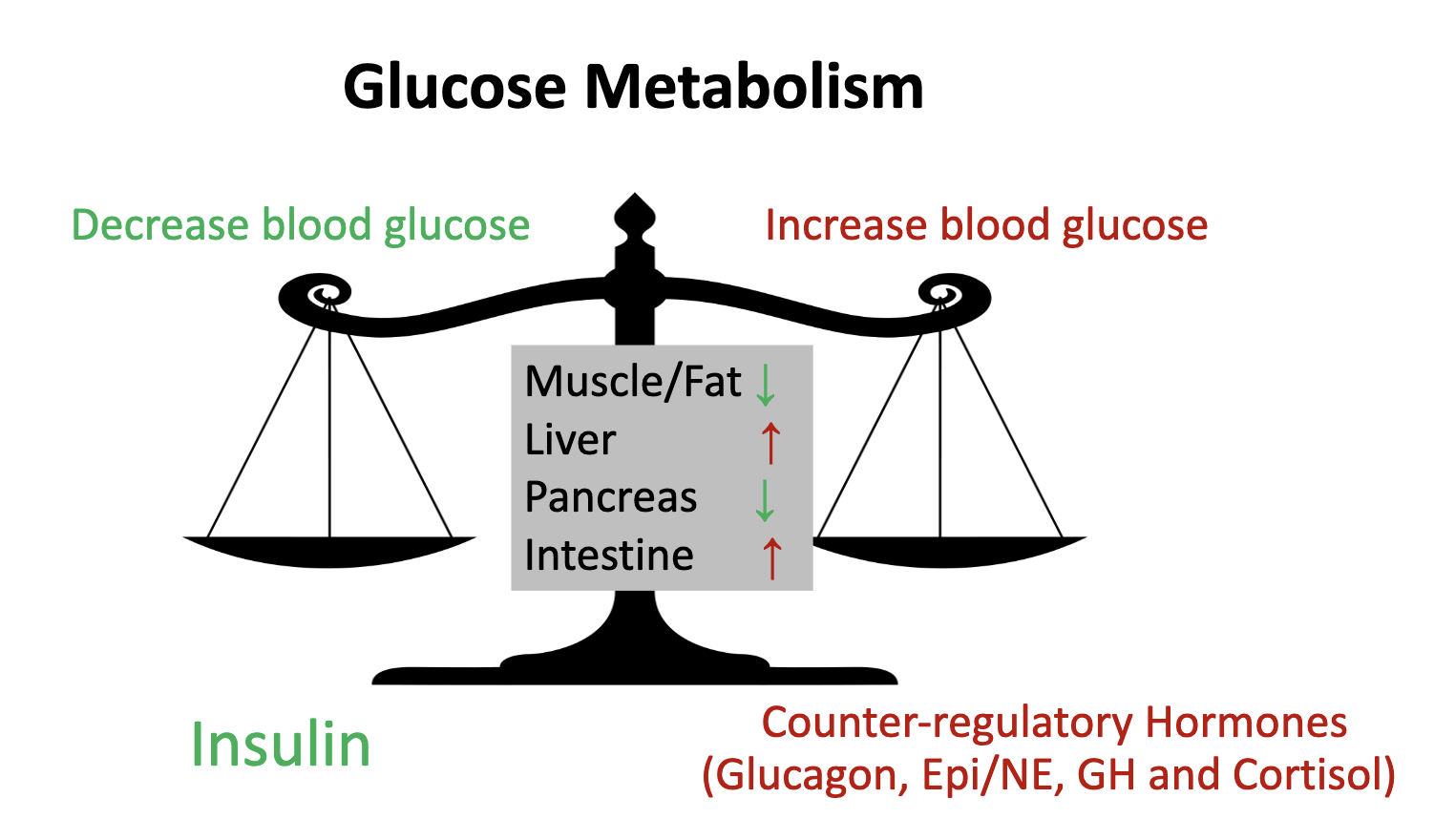
Counter-regulatory Hormones:
• Epinephrine/Norepinephrine (fight or flight response) (mobilize glucose)
• Glucagon (mobilize glucose)
• Growth Hormone
• Cortisol
• Catabolic, so their primary function is to mobilize substrates
• ↑ Lipolysis and FFA output from adipose tissue
• ↑ Hepatic glucose output
• ↓ Glucose Uptake
What Happens During Exercise
In order to maintain blood glucose: insulin levels DECREASE while counter-regulatory hormone levels INCREASE
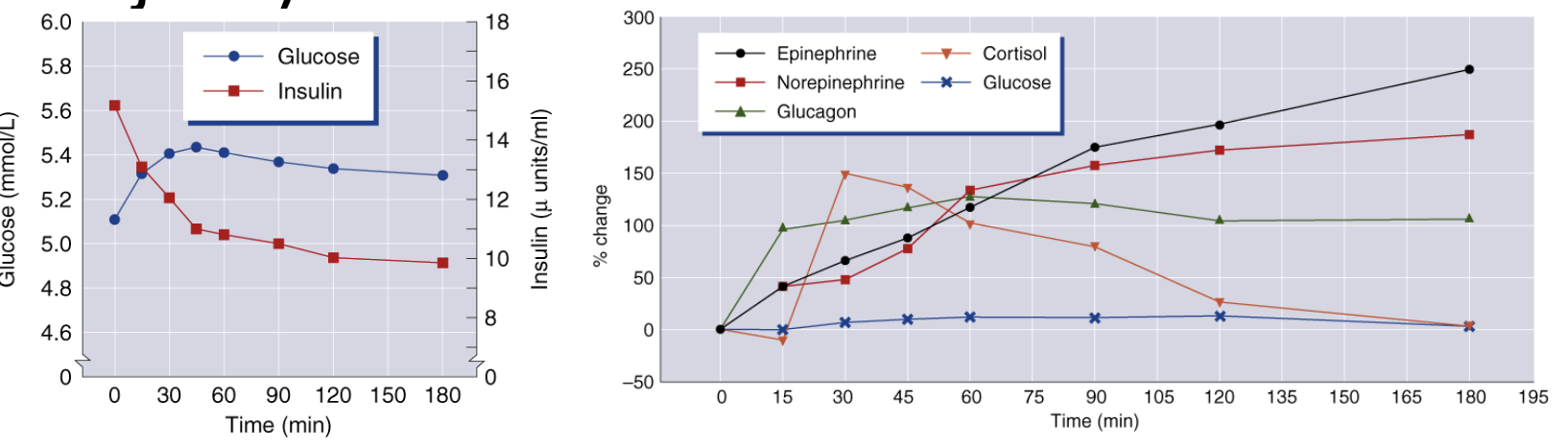
Which are the main effectors in blood glucose regulation, and how do they change
during exercise? (Think about insulin vs. counter-regulatory hormones and how they
maintain blood glucose levels in exercise)
Main effectors:
Insulin → lowers blood glucose.
Counter-regulatory hormones: glucagon, epinephrine, cortisol, and growth hormone → raise blood glucose.
During exercise:
Insulin ↓ → limits glucose uptake in non-active tissues.
Glucagon, epinephrine, cortisol, GH ↑ → increase hepatic glucose output and promote fat use.
Muscle glucose uptake ↑ via insulin-independent (contraction-mediated) pathways.
➜ Result: Blood glucose maintained despite increased
What are the primary factors that increase glucose uptake, and what is the primary transporter molecule that facilitates glucose uptake by the skeletal muscle?
Exercise increases glucose uptake in active muscles, as well as insulin sensitivity. (Exercise has an insulin-like effect. Muscle contraction DIRECTLY promotes glucose uptake (insulin is not necessary). Glut4 Transporters are responsible for facilitating glucose into the skeletal muscle.
Exercise Increases Insulin Sensitivity Effects
Insulin-stimulated glucose uptake and glycogen synthesis were markedly increased post-exercise.
Increased uptake in the absence of Insulin (up to 1h post-exercise).
Increase uptake only in the presence of insulin (from 2h post exercise).
This effect could last up to 72h post-exercise
Primarily due to increased Glut 4 protein levels
How to prevent exercise-induced hypoglycemia?
If blood glucose < 100 mg/dl – Elevated risk for hypoglycemia
Ingest Carbs before exercising and postpone the exercise 15-30 min
In order to prevent hypoglycemia
Inject Insulin in a non-active site
DO NOT EXERCISE 2 hrs after insulin injection
Reduce insulin dose by 20-50% (up to 90% reduction if using an insulin pump)
Exercise Benefits – T2DM
Improves glucose uptake – less glucose in blood (immediate effect)
Increases insulin sensitivity (short-term effect)
Weight/fat loss improves insulin sensitivity (long-term effect)
Reduced CVD risk factors, chronic illnesses
Stress reduction
Physical activity plays an important role in preventing and treating T2DM
Exercise Benefits – T1DM
• Increases insulin sensitivity (can use less insulin)
• Helps maintain a healthy weight
• Reduced CVD risk factors, chronic illnesses
• Stress reduction
• Improves overall quality of life
Physical activity presents quite a few challenges in the treatment of T1DM. However, the potential benefits of well-planned exercise outweigh them.
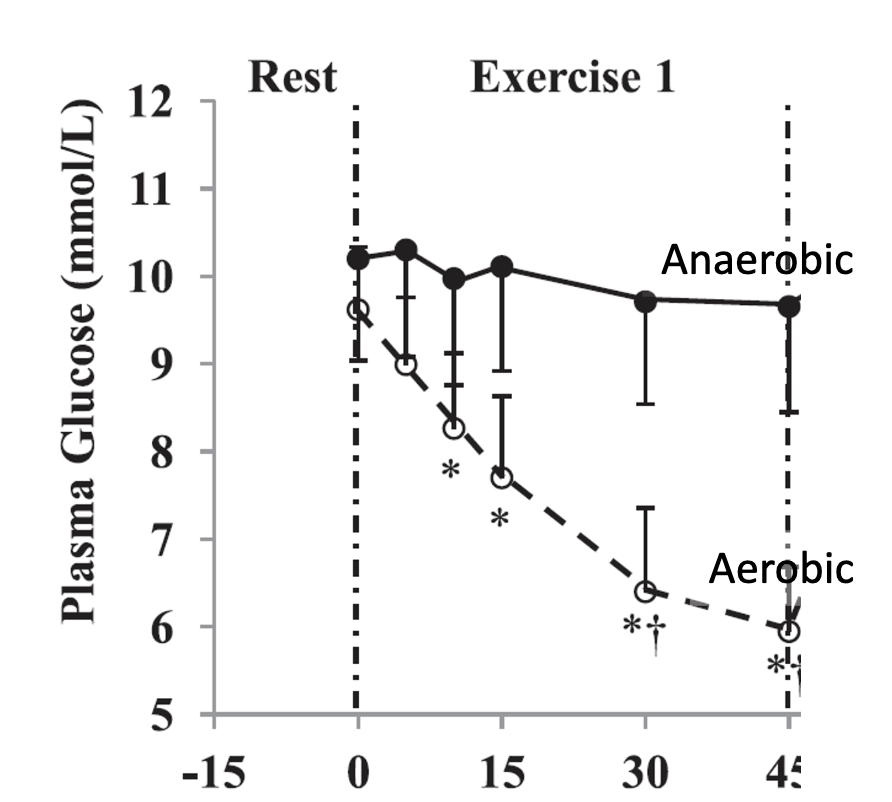
Study the graphs that show plasma glucose response to aerobic vs resistance exercise
• A massive increase in counter-regulatory hormones
• results in increased hepatic glucose output
• with rates that surpass glucose uptake by the skeletal muscle
• So...
• Blood glucose does not drop as it does during aerobic exercise
• and might actually even increase
ADA Recommendation for PA in Diabetes
• at least 150 min/wk of moderate aerobic activity.
• 3 days/week, with no more than 2 consecutive days without activity.
• Alternatively, at least 75 min/week of vigorous intensity
• 2–3 sessions/week of resistance exercise on nonconsecutive days.
• Additionally, decrease the amount of time spent in daily sedentary behavior. Prolonged sitting should be interrupted every 30 minutes
• Finally, Flexibility training and balance training are recommended 2–3 times/week for older adults with diabetes.
General Exercise Plan for Type 1 Diabetes
Aerobic Exercise
Intensity:
50-90% of HRR
RPE 11-16
Frequency: 3-7 d/wk
Duration:
20-60min total
5-10min – Warmup
5-10min – Cool down
Resistance Exercise (initial)
Intensity:
40-50% 1RM
Max weight at 20-10 reps
Frequency: 2-3 d/wk
Duration:
5-10min –Warmup
1-3 exercises per muscle group
1-3 sets per exercise
15-8 reps
General Exercise Plan for Type 2 Diabetes
Aerobic Exercise
Intensity:
50-90% of HRR
RPE 11-16
Frequency: 3-7 d/wk
Duration:
20-60min total
5-10min – Warmup
5-10min – Cool down
Resistance Exercise (initial)
Intensity:
40-50% 1RM
Max weight at 20-10 reps
Frequency: 2-3 d/wk
Duration:
5-10min –Warmup
1-3 exercises per muscle group
1-3 sets per exercise
15-8 reps
Circuit type training is recommended
Target large muscle groups
Use compounded movements (multi-joint)
Beware of Isometric exercises
BMI
Body Mass Index — weight / height²
No distinction between overweight and overfat
Body fatness and BMI are only weakly related
Relationship differs in different groups
Old vs. YoungOld vs. Young
Men vs. WomenMen vs. Women
Weight trained vs.Weight trained vs. Non-weight trainedNon-weight trained
BMI IS NOT A BODY COMPOSITION MEASURE
A disadvantage is that it cannot distinguish between fat and muscle so a muscular person could be labeled as “obese”
Normal BMI
<25 kg/m²
Overweight BMI
25-29 kg/m²
Obese BMI
≥ 30 kg/m²
Fat mass (FM)
The absolute amount of body fat
Includes all extractable lipids from adipose and other tissues
Fat-free mass (FFM)
Lipid-free chemicals and tissue
Water, muscle, bone, connective tissue, organs
Basically, everything else that is not fat.
Relative body fat percentage (%BF)
FM expressed as a percentage of total body mass (TBM)
Indirect Assessment of Body Comp Measures – Densitometry-based
Densitometry: assess the density of the body
Density = Mass / Volume
Archimedes’ Principle: an object repels water in a direct relation to its density
MRI / DXA
break body into components of muscle, bone, and fat and estimate their volumes (know body mass, can estimate density)
Indirect Measures – Densitometry based
Dual-Energy X-Ray Absorbptiometry
Theory
Transmit photons (X-rays) at 2 different energy levels and get different attenuation levels by fat, lean tissue, and bone
What does it measure?
Bone mineral density
Fat
Fat-free soft tissue
3 Component Model
Potentially more accurate b/c it accounts for individual differences in 3 components
Accuracy ± 3%Accuracy ± 3
Magnetic Resonance Imaging
High Accuracy ~ 1%
Issues:
ExpensiveExpensive
Labor intensive
Skinfold Thickness
assess subcutaneous fat at various places
Indirect Measures – Densitometry based
Bioelectrical Impedance
Predict comp from resistance to the flow of electrical current
Indirect Measures – Densitometry-based
Resistance to current flow reflects the properties of different tissues
Tissues that contain a high level of water (blood, muscle) are highly conductive
Fat, bone, and air-filled spaces are not.
Easy to use, appears sophisticated
Overweight vs Obese
When body weight exceeds the normal or standard weight for a particular person based on height and frame size.
Both involve having an excessive amount of body fat
Usually determined by BMI (Overweight: BMI >25, Obese: BMI >30)
What is the % of overweight and obese people in the USA?
Around 70% of US adults are overweight (BMI>25) and 33% are obese (BMI≥30)
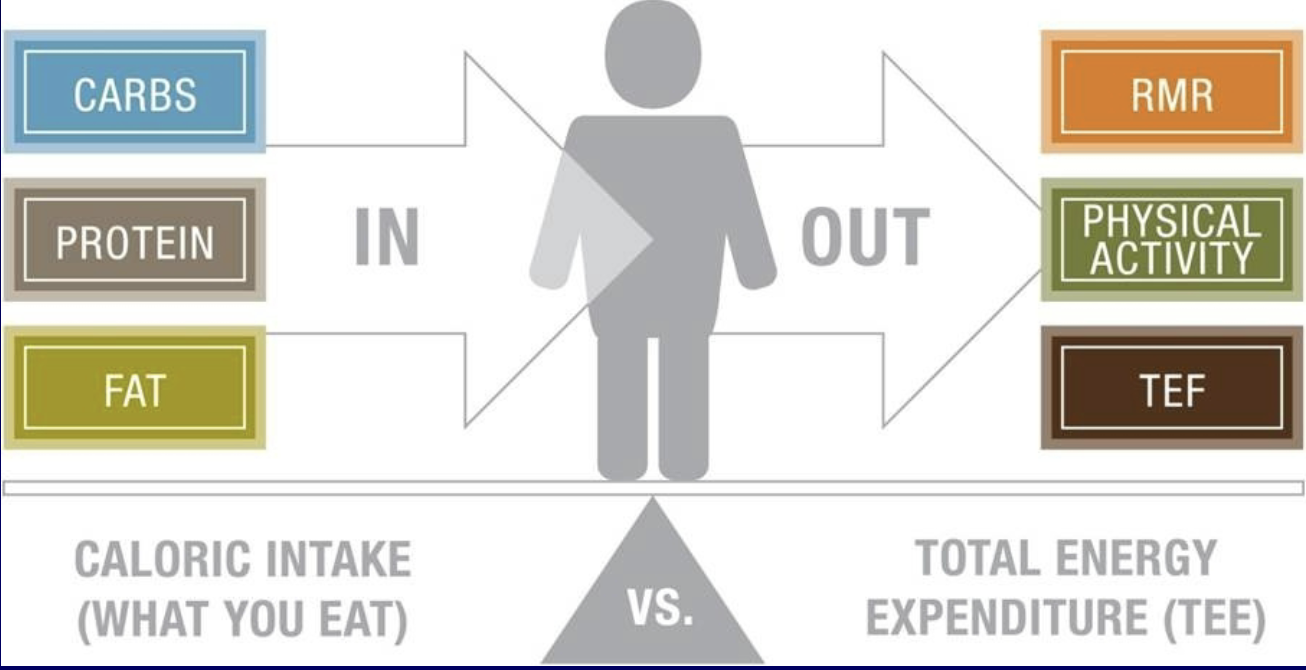
Body Weight Regulation
Energy Balance = (Intake – Expenditure)
If intake and expenditure are equal, then weight will remain stable
If intake exceeds expenditure, then weight will increase
If intake is less than expenditure, then weight will decrease
Expenditure
RMR (60-75%)
Activity - exercise, non-exercise activity (15-30%)
Thermic effect of feeding – energy required for digestion (10%)
Measuring Energy Expenditure
Substrate + ADP + Oxygen (O2) = ATP + Carbon Dioxide (CO2) + Heat
Measure Directly = measure heat
Measure Indirectly = measure other metabolic by-products (O2 and CO2)
These measures only estimate energy from AEROBIC METABOLISM
Indirect Calorimetry: Measuring Gas Exchange
Respiratory Exchange Ratio (RER)
Respiratory quotient (RQ) is the ratio of CO22 production to O2 consumption at the cell (VCO2/VO2)
When measured using expired gases, this ratio is called the respiratory exchange ratio (RER)
RER provides an index of energy derived from fat and carbs
RER = 1.0: 100% of the energy is derived from carbohydrates
RER = 0.7: 100% of the energy is derived from fats
RER = 0.85: ~50% of energy from CHO and 50% from fats
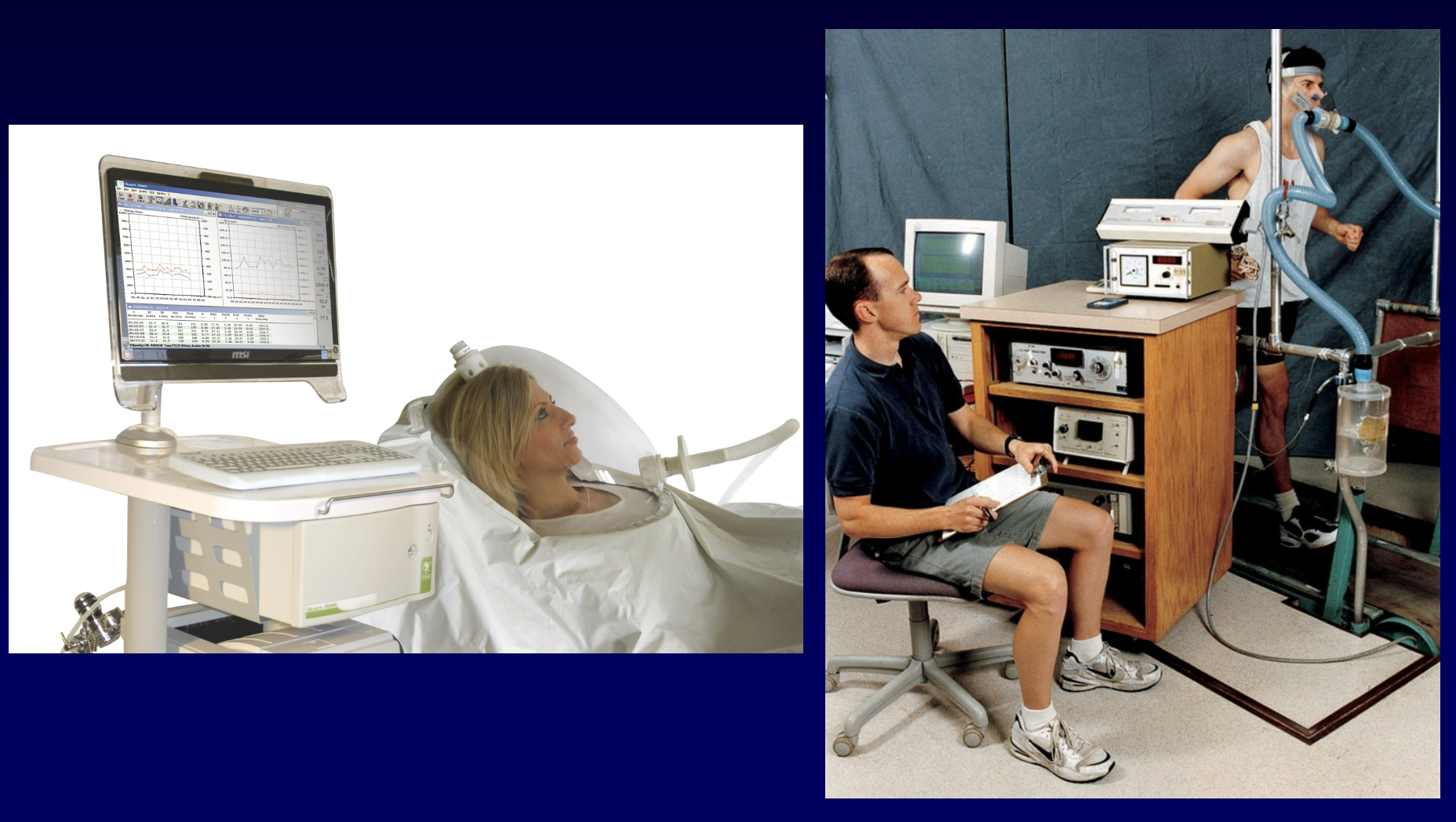
Caloric Equivalent for Oxygen
• Caloric value per liter of O2 depends on the substrate being oxidized.
• Glucose ~ 5 kcal/l O2
• Fat ~ 4.6 kcal/l O2
• RER can be used to determine the kcals per liter of O2 consumed, which is termed the caloric equivalent for oxygen.
Resting Metabolic Rate (RMR)
Rate at which the body expends energy at rest
Usually measured as whole body oxygen consumption
Basal Metabolic Rate (BMR)
The minimum energy required for essential physiological functions (varies between 1,200 and 2,400 kcal a day)
Directly related to the amount of muscle in the body
Daily Energy Use
1,800 to over 3,000 kcal a day
Higher than RMR b/c of the energy required to move
Factors Affecting RMR
Fat-Free Mass (FFM)
Muscle uses energy
More muscle = more energy use
Body surface area (different than mass)
More area = grater heat loss
More area = more energy required to maintain body temp
More area = higher metabolic rate
Other Factors
Body Temperature
Stress
Hormones
Calculating RMR – the Weir Equation
RMR (kcal/day) = 1440 (3.941 * VO2 (l/min) + 1.106 * VCO2(l/min)).
Energy Intake
Carbohydrates & Proteins = 4kcal/g
Fats = 9kcal/g
Alcohol= 7kcal/g
Energy Expenditure
Walking/Running= 1kcal/1km/1kg BW
Cycling = 0.25 kcal/1km/1kg BW
Swimming= 4 kcal/1km/1kg BW
What is Gait?
An acquired skill consisting of several movements
Getting up from a seated position
Propelling the body forward
Maintaining balance
Direction changes in response to a changing environment
Stopping
Gait Cycle – A Stride
Stance – 60%, Swing – 40%
Heel strike—>forefoot contact—>heel lift—>toe off
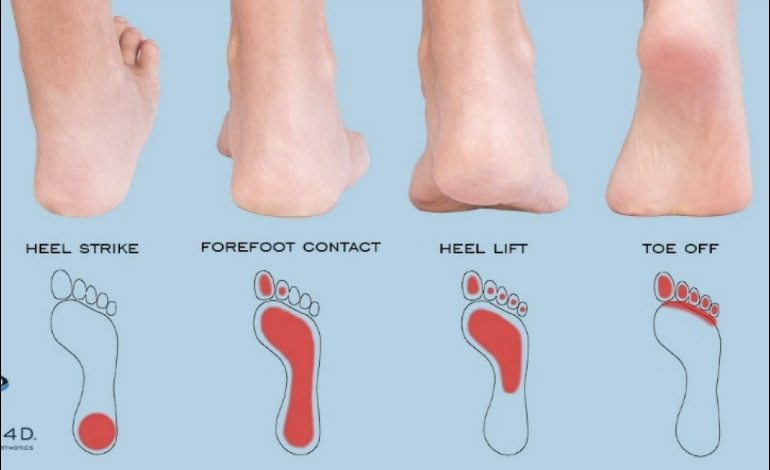
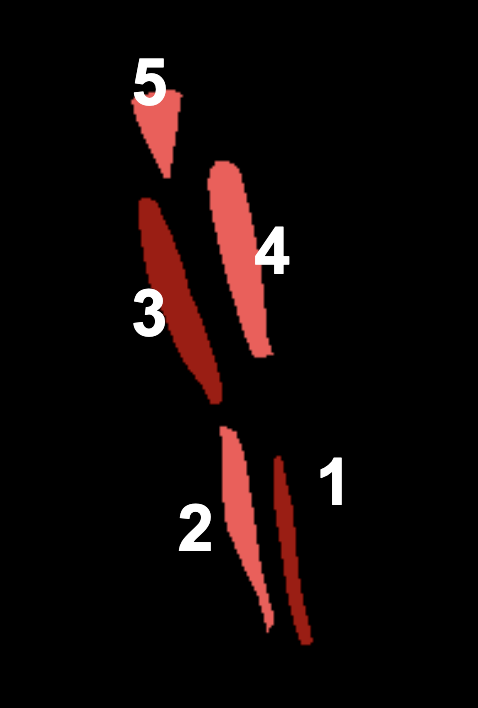
Walking/Gait Muscles
Tibialis Anterior (deceleration muscle—on shin, absorbs force)
Gastrocnemius
Hamstrings
Quadriceps
Gluteus Medius (Helps stabilize—not sway)
What to Look For in Gait
Difficulty rising from a chair (muscle weakness, balance problems)
Balance - do they veer off course? (cerebellar dysfunction)
Widened base - if base width approaches two feet, The likelihood of psychogenic gait disorder rises, unless the patient has morbid obesity or an obvious structural explanation
Shuffling gait
Postural sway
Rate of walking - start off slowly and then speed up or general slowness (joint degenerative disease, weakness)
Steppage gait -lifting the leg higher than normal when walking (peroneal nerve injury, fibular injury, multiple sclerosis)
Antalgic Gait
painful gait, a limp to avoid pain
Ataxic gait
An unsteady, uncoordinated walk, a wide base of support, is seen. normally due to cerebellar disease
Festinating Gait
short, accelerating steps are used to move forward, often seen in people with Parkinson's disease
Hemiplegic gait
involves flexion of the hip because of the inability to clear the toes from the floor at the ankle and circumduction at the hip—unable to lift toes—feet are always flat
Steppage gait
A weak anterior tibialis muscle causes foot drop, and you must lift your foot up high to clear your toes over the ground.—can lead to knee pain since it is taking all of the force
Trenelenurg gait
Weak hip and gluteal muscles causing leaning over sideways a bit while walking
spastic gait
increased muscle tone due to CNS impairments
What is a Normal Gait in Elderly?
Slowed speed (< 5 km/h)
slowed postural support responses
shorter step length
increased time in double limb support
Strength declines in leg and posture muscles
Declined aerobic capacity
Posture changes (stooped posture – increased pressure on posterior muscles)
Neuromuscular declines
Step Length
Count #of steps it takes to cover 5 meters
Calculate: 500cm/step# = Step length (cm).
Do it twice and take the average
Comfortable Walking Speed
Measure the time it takes to cover 10 meters
Calculate: 10m / time (sec) = Speed (m/sec)
Do it twice and take the average
To convert: m/sec * 3.6 = Km/hr
Daily Walking Distance
Measure daily step # (pedometer/ smart watch/ phone app)
Measure step length
Calculate: Daily step # * Step length (cm) = Daily walking distance (cm)
To convert: cm / 100,000 = Km
Aging of The Motor System (Neuromuscular changes)
Decreased muscle mass & strength
Decreased muscle function
Decreased dexterity
Increased falls
Increased disability
Sarcopenia
Decreased Muscle Mass
Decreased fiber size
Decreased fiber number
Large, weight-bearing muscles – more susceptible
results in systemic decrease in strength, so Grip strength will correlate with other muscles
Fiber Type Changes with Aging
Decreased Type 2 fiber number (fast twitch)
Aging of the skeletal system
Decreased bone density (osteoporosis)
Increased fracture risk
Decreased elasticity of connective tissue
Decreased ROM in the joints
Increased tendon stiffness
Increased risk of tendon injury
Most of these changes are due to disuse
Physical activity offers protection
Aging of the Neural System
Decreased neuron numbers
»» Ischemia, neurotoxins and apoptosis
Decreased reaction time
Decreased neural signal speed
Decreased coordination
Decreased dexterity
Reduced cognitive function
Greater strength loss
• Rarely used muscles
• Concentric contraction
• High contraction velocity
• Maximal strength
• Power activities
• Large angles in the joint
• Women
Moderate Strength loss
• Daily used muscles
• Isometric + Eccentric contraction
• Slow velocity
• Muscle endurance
• Small angles in the joint
• Men
Benefits of Resistance Training in Elderly
Improved mobility
Improved ability to perform ADL
Prolongs the period of functional independence
Lowers the risk of falling
Improved Bone Density
Improves metabolic health
Resistance Training in The Elderly
Most have chronic conditions – physician consent
Avoid the Valsalva maneuver
Longer warm up and cool down
Incorporate functional exercises
Multijoint, large muscle group exercises
Machines are preferred over free weights
»» Less skill is required
»» Greater support
»» More gradual resistance adjustment
Aging of The Aerobic System
VO2max ↓ 5ml/kg/min per decade
12-14 ml/kg/min – Functional Threshold
HRmax ↓ 10 bpm per decade
Vascular stiffness + atherosclerosis
Weakened respiratory muscles
Stiffness of the costal joints
Benefits of Aerobic Training in Elderly
Attenuates VO2max decline
Attenuates SV and CO decline
Improved mobility
Improved ability to perform ADL
Lowers the risk of falling
Improves metabolic health
Functional Tests
sit to stand test
timed get up and go
functional reach test
Berg balance test
timed one-legged stance
6 min walk test
grip strength test: 30 kg for Men and 20kg for Women