HCR 240: Neurology Part 2
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
what is hypotonia
decreased muscle tone (flabby, no strength)
what is hypertonia
increased muscle tone
what are the three types of hypertonia
- spasticity: hyperexcitability of stretch reflexes leading to uncontrolled spastic movements
- dystonia: increased voluntary muscle contraction leading to uncontrolled repetitive movements (happens involuntary)
- rigidity: firm and tense muscles that resist movement
what are upper motor neurons, what do injuries lead to, and clinical manifestations
- originate in the brain and travel down to brainstem and spinal cord
- upper motor injuries will lead to hypertonia
- clinical manifestations: hypertonia (spasticity, dystonia, rigidity)
what are lower motor neurons, what do injuries lead to, and clinical manifestations
- originate in spinal nerves and travel to muscles
- lower motor neurons injuries will lead to hypotonia
- clinical manifestations: hypotonia (impaired movements, paresis or paralysis), muscle atrophy and develop fasciculations (involuntary, brief, localized, visible muscle contractions)
what is Parkinson disease and what does it lead to
- exact pathology is Parkinson disease is unknown but disease progression leads to loss of neurotransmitter dopamine
- dopamine has a crucial of inhibiting excess movements in the basal ganglia (part of the brain responsible for controlling voluntary movement)
what are symptoms of Parkinson disease
- loss of dopamine causes hypertonia - hallmark sign: resting tremors, cogwheel rigidity, and bradykineasa (slow movements due to loss of ability to control voluntary movements)
- increased tone leads to difficulty walking (hallmark sign: slow shuffling gait)
- other common symptoms: frequent drooling, unblinking stare with immobile facial muscles (masked facies)
what is Parkinson’s disease also associated with and treatment
- Parkinson’s disease is also associated with dementia
- treatment: place dopamine (medications carbidopa and levodapa), drugs that improve dopamine activity (amantadine), rehabilitation, physical therapy, occupational therapy, speech language therapy
what are spinal cord injuries
most causes of spinal cord injuries are traumatic due to falls, motor vehicle accidents, sports, or violence (its an upper motor neurons, CNS injury)
- shearing, compression, or penetrative forces leading to spinal cord tissue injury
- important to immediately immobilize the spine when cervical, thoracic, or lumbar vertebral trauma is suspected
what are clinical manifestations for spinal cord injuries
- normal activity of spinal cord cells cease at and below the level of spinal cord injury leading to loss of sensation and movement on the ipsilateral or contralateral side (depends on location of spinal cord injury)
- initial hypotonia followed by development of hypertonia
what is spinal shock (spinal cord injury complications)
initial loss of all motor and sensory function as wells as reflexes at or below the level of spinal cord injury
- some motor and sensory function may return and patient may experience return of normal reflexes or develop hypertonia
(*temporary, sustained significant spinal shock)
what is neurogenic shock (spinal cord injury complications)
- typically occurs with spinal cord injury at T6 or higher
- occurs due to loss of sympathetic activity, patient develops hypotension and bradycardia
(*real shock, low bp - there is injured flight or fight response so you can’t bring up heart rate or bp)
what is autonomic dysreflexia (spinal cord injury complications)
- typically occurs with spinal cord injury at T6 or higher and develops several days to weeks after initial injury
- hyperreactivity of sympathetic activity leads to extreme hypertension and reflex bradycardia with flushing of skin
- any stimulation can trigger dysreflexia but it is most commonly due to distended bladder or rectum
(*neurons are not lost but injured)
what is multiple sclerosis (demyelinating disorders)
- autoimmune disorder leading to progressive inflammatory demyelination of nerve fibers in the CNS
- injured myelin becomes sclerosed (hardens into plaques) which disrupts axon activity
- partial recovery of myelin sheaths can lead to relapsing-remitting symptoms
- MRI brain will demonstrate lesions that vary in time and space
*tends of affect females more than males
what are symptoms and treatment for multiple sclerosis (demyelinating disorders)
- patients will typically have varying focal neurological deficits that come and go: weakness, paralysis, sensory deficits, impaired gait, visual disturbances, urinary incontinence, vertigo, ataxia, speech difficulties…
- no cure for multiple sclerosis but can try to control symptoms
what is guillain-barre (demyelinating disorders)
- also known as acute inflammatory demyelinating polyneuropathy
- typically occurs after a gastrointestinal or respiratory tract infection, can also occur after surgery or vaccination
- molecular mimicry leads to cross-reactive antibodies that target axonal myelin sheaths in peripheral motor nerves
(*one moment you’re fine, the next you’re not)
what are clinical manifestations and treatment for guilain-barre (demyelinating disorders)
- clinical manifestations: ascending flaccid paralysis starting from legs and eventually leading to quadriparesis or quadriplegia, hypotonia and loss of reflexes, respiratory failure, and autonomic nervous system instability
- most patients will slowly recover after treatment although recovery may be incomplete and typically take several months

what is myasthenia gravis (neuromuscular junction disorder)
chronic autoimmune disease caused by production of IgG antibodies against acetylcholine receptors in the post synaptic cleft of the neuromuscular junction

what does myasthenia gravis lead to (neuromuscular junction disorder)
leads to destruction of acetylcholine receptor sites and causes decreased transmission of nerve impulse
(*the more they move, the weaker they become - provider tells patients to keep blinking and at a point, they can no longer open their eyes but after a while they will be able to open again)

what is myasthenia gravis characterized by and symptoms (neuromuscular junction disorder)
- characterized by insidious onset of exertional fatigue and muscular weakness that improves with reset and worsens again with ongoing activity
- some types of myasthenia autoantibodies may selectively affect muscles of eye, face, mouth, throat, and neck - these syptoms are oftentimes the first symptoms to appear: diplopia (double vision), ptosis (drooping eyelids), difficulty talking, swallowing, and chewing

what are treatments for myasthenia gravis (neuromuscular junction disorder)
- treatment is individualized based on severity of disease and typically includes more than 1 drug
- immunosuppressant drugs (corticosteroids)
- acetylcholinesterase inhibitor (anti-acetylcholinesterase) medications are the basis for outpatient treatment
(*this happens over a long period of time)

what is myasthenic crisis (neuromuscular junction disorder)
uncontrolled myasthenia leading to severe muscle weakening and respiratory distress
- requires ICU admission and plasmapheresis

what is botulism (neuromuscular junction disorder)
- caused by ingestion of toxins released from bacteria Clostridium Botulinum (most commonly seen in improperly canned foods)
- toxins act to inhibit the release of acetylcholine vesicles from the presynaptic cleft
(*happens suddenly)

what are symptoms of botulism and what can ingestion of it lead to (neuromuscular junction disorder)
- symptoms may begin with diplopia, difficulty with speech and swallowing however rapidly progress to severe flaccid paralysis, respiratory failure, and dead (looks like myasthenia gravis)
- ingestion of C. botulinum can also lead to colonization of the intestine and production of toxins in people who have impaired intestinal microflora or low levels of bile acid
what is glasgow coma scale (traumatic brain injury - TBI)
- assessment of a trauma patient with suspected neurological injury started with the glasglow coma scale (GCS)
- the gcs was developed to quantify the severity of a person’s traumatic brain injury and allow for clinical tracking of injury progression
what are the 3 factors that are assessed in the GCS (traumatic brain injury - TBI)
- eye opening
- verbal response
- motor response
(these are based on the patient’s best response)
what is the lowest score and highest score of the glasglow coma scale and what do the points mean (traumatic brain injury - TBI)
- the lowest score is 3 and the highest score is 15
- a GCS of 3 to 8 is considered severe TBI and needs emergence treatment
- minor brain injury: 13-15 points
- moderate brain injury: 9-12 points
- severe brain injury: 3-8 points
what is posturing (traumatic brain injury - TBI)
- the term used for certain abnormal movements of the skeletal muscles in response to stimulation
- posturing occurs when there is severe injury to brain
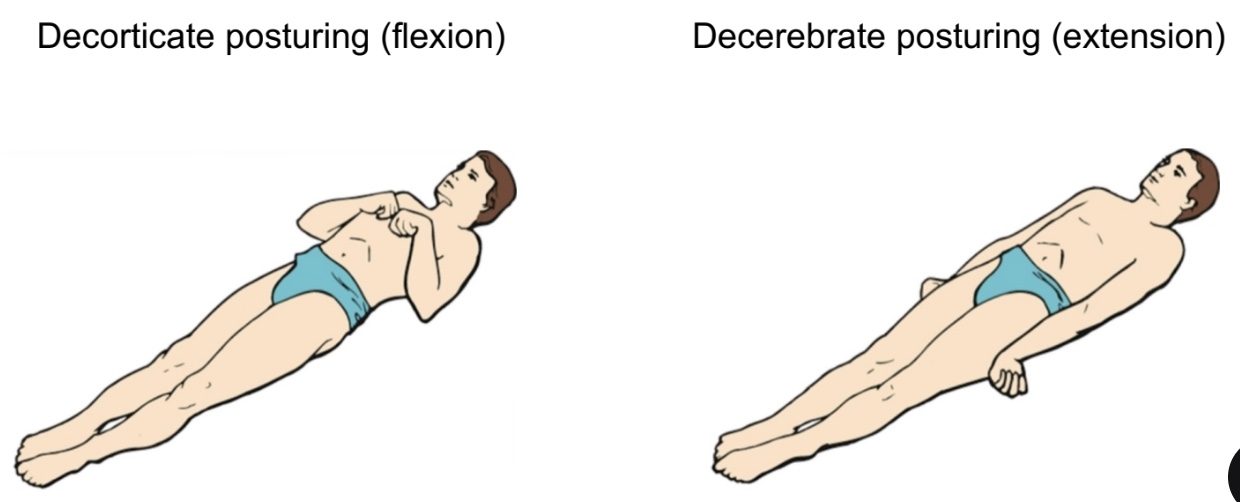
what are the 2 main types of posturing (traumatic brain injury - TBI)
- decorticate posturing (flexion): suggests injury to cerebral cortex → flexion of upper extremities at elbow with extension of lower extremities
- decerebrate posturing (extension): suggests injury to cerebrum and brainstem → all four extremities are in rigid extension with the forearms in hyperpronation
what is traumatic epidural hematoma, what is it associated with, and what does it need (traumatic brain injury - TBI)
- hemorrhage below the skull but above the dura matter
- typically associated with skull fractures, especially at the temporal fossa (site of meningeal artery and vein)
- needs emergent evaluation by neurosurgery for potential cranietomy and evacuation of hematoma; surgery is typically indicated
what are symptoms of traumatic epidural hematoma (traumatic brain injury - TBI)
- characteristic symptoms include initial loss of consciousness following by lucid periods (brief periods in which the patient regains consciousness)
→ following lucid periods, symptoms will occur and may progress to nausea, vomiting, lethargy, and coma
→ epidural hematoma expansion is immediately life-threatening
what is traumatic subdural hematoma, what is it associated with, and symptoms (traumatic brain injury - TBI)
- hemorrhage below the dura matter but above the brain tissue
- most SDH are associated with venous bleeding
- symptoms occur due to compression of brain tissue and depending on site of hemorrhage: nausea, vomiting, headache, confusion, weakness, coma
what is needed in a traumatic subdural hematoma and treatment (traumatic brain injury - TBI)
- needs emergent evaluation by neurosurgery for potential craniectomy and evacuation of hematoma
→ surgery is not always required if the subdural hematoma is small or if the symptoms are mild
→if hematoma is not removed, acute subdural hematoma will progress to subacute and then chronic
what is subarachnoid hematoma and symptoms (traumatic brain injury - TBI)
- hemorrhage below the arachnoid matter but above brain tissue (and pia matter)
- symptoms occur due to compression of brain tissue and depending on site and size of hemorrhage: nausea, vomiting, headache, confusion, coma
what is needed in a traumatic subarachnoid hematoma and treatment (traumatic brain injury - TBI)
needs emergent evaluation by neurosurgery
→ surgery is typically not indicated unless there are complications with cerebral edema
what is traumatic intraparenchymal hemorrhages/intraparenchymal confusions and symptoms - other traumatic brain injuries (traumatic brain injury - TBI)
bleeding within the brain tissue, symptoms are based on size and location of hemorrhage
what is coup-contre-coup injuries - other traumatic brain injuries (traumatic brain injury - TBI)
bleeding of the opposite site of impact; caused by abrupt shaking of the brain within the skull
what is diffuse axonal injury - other traumatic brain injuries (traumatic brain injury - TBI)
shearing injury to the axons of the brain causing mild to severe cognitive impairments
what are the other types of traumatic brain injuries (traumatic brain injury - TBI)
- traumatic intraparenchymal hemorrhages/intraparenchymal confusions
- coup-contre-coup injuries (injury is so strong it pushes brain into other side)
- diffuse axonal injury (doesn’t show up on CAT scan, need MRI)
- skull fractures (epidural)
- concussions
(*multiple types of traumatic brain injuries tend to occur at the same time)
what are TBI considerations (traumatic brain injury - TBI)
- all neuro trauma patients with acute hemorrhage need to be monitored in an ICU setting with frequent neurological examinations and serial CT scans
→ high risk of post-traumatic seizures within the first 7 days
→ concern for hematoma expansion
→ concern for secondary injury: indirect injury to brain that occurs hours to days after primary injury due to inflammation and release of cytotoxic cell contents
→ concern for development of cerebral edema and high intracranial pressure: tends to peak at days 5-7 and can become life-threatening
what is cerebrobascular accident (CVA) and risk factors (cerebrovascular diseases)
- strokes are referred to as cerebrovascular accidents (CVA)
- CVAs are the leading cause of disability and one of the top 10 causes of mortality in US
- risk factors for CVA: smoking, diabetes, obesity, high blood pressure, cholesterol, atrial fibrillation, hypercoagulable states, positive family history
what are symptoms of cerebrovascular accidents and common assessments by family/ER staff (cerebrovascular diseases)
- symptoms of a stroke depends on the size and location of the stroke
- common symptoms: loss of sensation, weakness or paralysis of contralateral limbs, speech disturbances (aphasia and dysarthria)
- common assessment for stroke by family members or EMS: FAST
- common assessment for stroke by ER staff and neurologists: NIHSS
what are the different types of cerebrovascular accidents and what do all stroke patients need (cerebrovascular diseases)
- ischemic stroke (something blocking off intracranial: thrombotic and embolic
- hemorrhage stroke (spontaneous hemorrhage in brain)
- all stroke patients need an emergent CT scan to see what type of stroke is occurring prior to initiating treatment
what is thrombotic ischemic strokes (cerebrovascular diseases)
- atherosclerosis or inflammation causes formation of thrombi within intracranial arteries (clot start in intracranial artery)
- thrombi can grow large enough to block arteries directly which causes arterial occlusion and stenosis
- insufficient arterial blood flow can lead to brain tissue hypoxia and eventually cell death
what can also be injured in thrombotic ischemic strokes
surrounding cells in nearly brain tissue may also be injured and progress to death or may be saved with adequate treatment (penumbra)
what is embolic ischemic strokes and typical sources (cerebrovascular diseases)
- thrombus is formed extracranially and breaks off to become an embolus
- typical sources: heart with atrial fibrillation, endocarditis, prosthetic valve, or rheumatic heart disease
- common to have secondary stroke or multiple stokes at once
what is treatment for embolic ischemic strokes
- treatment for ischemic strokes (thrombotic and embolic) is time sensitive
- limited window of opportunity to save brain tissue within the penumbra
what is transient ischemic attack (TIA) (cerebrovascular diseases)
- sometimes referred to as a mini stroke
- symptoms are transient (resolve within 1 hour of onset without treatment)
- neuroimaging may be positive or negative for infaction
- high risk of ischemic stroke within the next 90 days
(*symptoms go away on their own within 24 hours)
what is hemorrhage strokes (cerebrovascular diseases)
- spontaneous intracranial hemorrhage
- due to similar symptoms, it is impossible to distinguish between ischemic and hemorrhage strokes without CT scan
- treatment is based on preventing hematoma enlargement and treating cerebral edema
what is intracranial aneurysm, what may it be, and describe non-ruptured and ruptured aneurysms - other cerebrovascular abnormalities (cerebrovascular diseases)
- weak bulging area in a vessel wall
- may be congenital or caused by arteriosclerotic changes to the blood vessel, infections, or trauma
- non-ruptured aneurysms are typically asymptomatic unless they grow large enough to compress brain tissue
- ruptured aneurysms are emergently life-threatening
what is non-traumatic subarachnoid hemorrhage, what is produced, how is it characterized, risk factor, and mortality rate - other cerebrovascular abnormalities (cerebrovascular diseases)
- blood escapes from defective or injured vasculature into the subarachnoid space (commonly caused by ruptured aneurysm)
- blood produces an inflammatory response with high risk of vasospasm
- characterized by sudden onset thunderclap headache (described as “worse headache of my life”) and progressive loss of arousal/awareness
- greatest risk factor is family history
- mortality rate is 50%
what is meningitis, how is it caused, and what does it alter (intracranial infections)
- inflammation of the meninges
- most commonly caused by infection (bacteria, viruses, parasites, fungi)
- alters CNS function due to compression of brain tissue and inflammatory response
what are hallmark signs of meningitis, what may it need, and treatment (intracranial infections)
- hallmark signs: fever, headache, light sensitivity (photophobia), neck pain, neck stiffness/rigidity, lethargy
→ may have positive Brudzinski’s and Kernig’s sign on clinical exam
- need lumbar puncture for diagnosis
- treatment depends on underlying cause
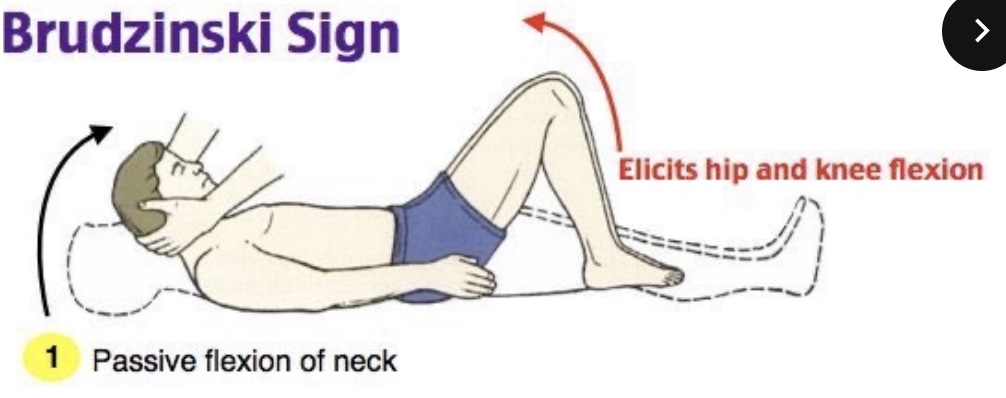
what are Brudzinski sign - meningitis (intracranial infections)
- Brudzinski sign is a finding on clinical examination that suggests meningeal irritation
- this test has relatively low sensitivity and high specificity (false negatives are common but if the test is positive then the patient likely has meningeal irritation)
(* high and knee flexion occurs when you do passive flexion of neck)
what are Kernig sign - meningitis (intracranial infections)
- Kernig sign is a finding on clinical examination that suggest meningeal irritation
- this test has relatively low sensitivity and high specificity (false negatives are common but if the test is positive, then the patient likely has meningeal irritation
(*when knee and hip is flexed 90 degrees, it elicits pain or limited extension)
what is encephalitis, what most commonly causes it, symptoms, and diagnosis (intracranial infections)
- inflammation of brain tissue
- most commonly caused by infection (bacteria, viruses, parasites, fungi) → Herpes Simplex type 1 is the most common sporadic cause of encephalitis
- patients may have similar symptoms as meningitis, but are more likely to develop focal neurological deficits and seizures
- need lumbar puncture for diagnosis → treatment depends on underlying cause
(*moves from meninges to brain, CSF fluid is white instead of clear)