flashcards physiology exam 2
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
What are the main functions of the cardiovascular system?
circulates gases (carbon dioxide & oxygen)
circulates nutrients
circulates antibodies
circulates hormones
circulates wastes
circulates electrolytes, etc.
regulates temperature
regulates pH
clotting
immune response
What are the two main components of blood?
plasma (liquid part)
formed elements (blood cells & platelets)
What type of tissue is blood?
vascular connective tissue
What is hematocrit?
the percent (%) of whole blood composed of red blood cells (RBCs)
female (♀): 38–45%
male (♂): 43–51%
What does temperature regulation involve?
taking heat to the skin → radiate out → sweat (540 cal/gram H20).
water acts as a “heat sink” with high specific heat (heat capacity).
What is the specific heat of water compared to metals?
H₂O (water) = 1 cal/g°C
Fe (iron) = 0.1 cal/g°C
Al (aluminum) = 0.1 cal/g°C
What is the normal blood pH range and how is it maintained?
pH = 7.35–7.45
Maintained by a buffer system.
What are the three layers seen when blood is centrifuged?
Plasma (top layer)
Buffy coat (white blood cells + platelets)
Erythrocytes (bottom layer)
What are two examples of blood’s role in homeostasis?
Regulating pH via buffers
Regulating temperature via heat distribution
What are leukocytes?
White blood cells that defend the body against infection and disease.
What are the two main categories of leukocytes?
Granulocytes
Agranulocytes
What are the three types of granulocytes?
-neutrophils
-eosinophils
-basophils
What are neutrophils also called?
Polymorphonuclear leukocytes (PMNs)
Describe neutrophils:
60-65% of white blood cells (WBCs)
Lysosome-rich and very phagocytic
Very migratory
Poorly stained granules
Faint in blood smears
Describe eosinophils:
Granules stain red with eosinophils (acidic dye)
Bilobed nucleus
Contain lysosomes
Active in allergic reactions and parasitic infections
Describe basophils:
Approximately 0.5% of white blood cells (WBCs)
Granules contain histamine (vasodilator, increases capillary permeability) and heparin (anticoagulant)
Granules are not lysosomes
What are the two types of agranulocytes?
Monocytes
Lymphocytes
Describe monocytes:
Largest of all white blood cells
15-20 µm (micrometers)
Become macrophages in tissues
Very active phagocytes
Describe lymphocytes:
Smallest of white blood cells
Two main types:
T lymphocytes- cellular immunity
B lumphocytes- humoral immunity (produce antibodies)
What are platelets?
cytoplasmic fragments with no nucleus
Live about 10 days
Count: 150,000-300,000 per mm³ of blood
Important in hemostasis (prevention of bleeding)
What determines blood type?
The presence of surface antigens A and/ or B on red blood cells.
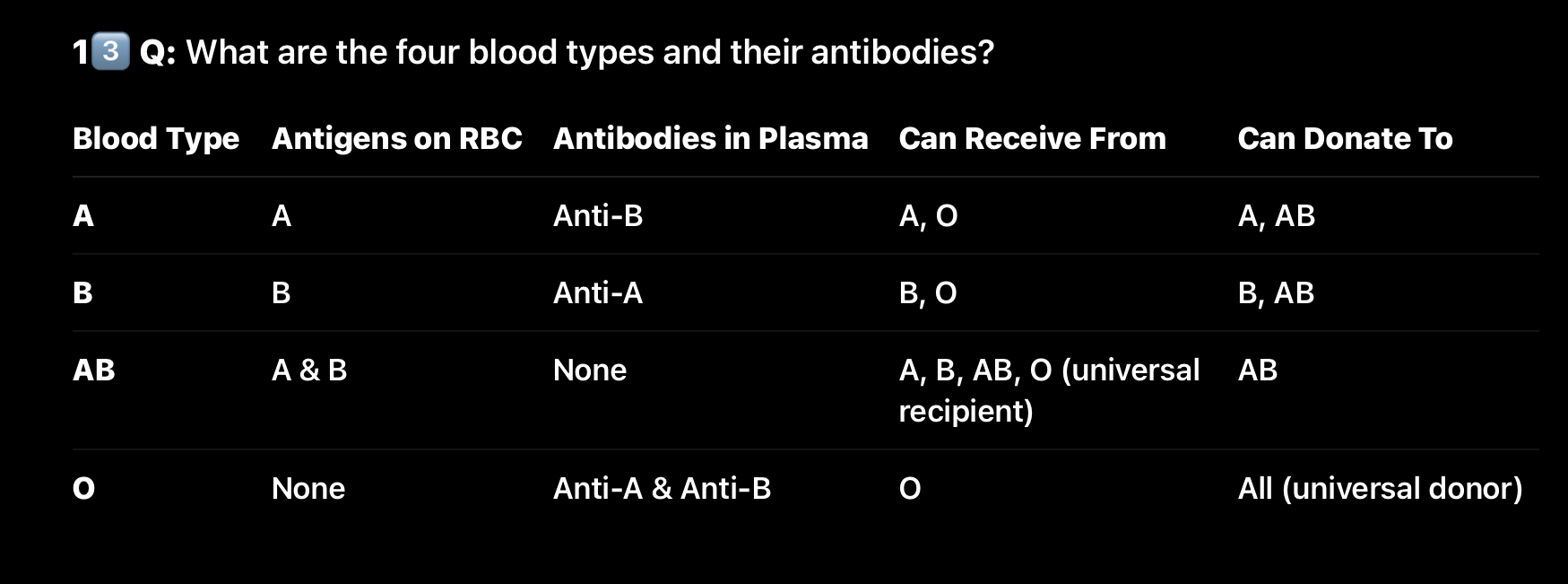
What are the four blood types and their antibodies
What is the Rh factor?
An antigen found on red blood cells
Rh⁺: has the antigen
Rh⁻: lacks the antigen
What happens if an Rh⁻ mother carries an Rh⁺ baby?
She may produce anti-Rh antibodies that cross the placenta during a second pregnancy, causing hemolytic disease (erythroblastosis fetalis).
What is RhoGAM used for?
To prevent Rh⁻ mothers from forming anti-Rh antibodies
What are the genetic alleles for the ABO blood group system?
IA, IB, and i
IA and IB are codominant (both expressed → type AB)
i is recessive (only shows when homozygous ii → type O)
What are the possible genotypes for each ABO blood type?
Type A: IAIA or IAi
Type B: IBIB or IBi
Type AB: IAIB
Type O: ii
What are the Rh factor genotypes?
Rh⁺: RR or Rr (has the Rh antigen)
Rh⁻: rr (no antigen)
What dye stains acidic cell structures red or pink?
Eosin, an acidic dye that binds to basic (alkaline) components in cells.
What dye stains basic structures blue or purple?
Methylene blue, a basic dye that binds to acidic components like DNA or granules.
Why are neutrophil granules faint in blood smears?
Because their granules stain poorly with common blood dyes, giving a light or faint appearance under the microscope.
What does hemostasis mean?
Hemostasis means the prevention of bleeding — literally “static blood.” It’s the process the body uses to stop bleeding after injury.
What are the three main steps of hemostasis?
Vasoconstriction
Platelet plug formation
Clot formation (with retraction and resolution)
What happens during vasoconstriction?
Blood vessels constrict to reduce blood flow.
Platelets release thromboxane, which acts as a vasoconstrictor.
Von Willebrand factor (vWF) attracts platelets to the site of damage and helps them stick, starting the platelet plug.
What is the role of von Willebrand factor?
It acts like a bridge — it binds exposed collagen fibers at the injury site and attracts platelets, triggering them to attach and start the platelet plug.
What is the function of thromboxane?
Thromboxane is released by platelets and causes vasoconstriction to limit blood loss.
What is platelet plug formation?
The second step of hemostasis — platelets stick to the damaged vessel wall and to each other, forming a temporary seal over the injury.
What chemical makes platelets “sticky”?
ADP (adenosine diphosphate) released by activated platelets makes other platelets sticky, promoting aggregation.
What other chemical activates more platelets during plug formation?
ATP — it helps activate surrounding platelets, creating a positive feedback loop.
How do platelets stick together?
Via fibrin connections — fibrin strands form a mesh that holds platelets together.
What happens in the clot formation stage?
Fibrinogen (soluble) is converted into fibrin (insoluble).
This reaction is catalyzed by the enzyme thrombin.
The fibrin forms a net-like structure that traps red blood cells and platelets, forming a clot.
What enzyme converts fibrinogen to fibrin?
Thrombin
Why is fibrin important in clot formation?
Because it forms the structural mesh of the clot that physically seals the injury.
What happens during clot retraction?
Actin and myosin in platelets contract, causing the clot to shrink.
This pulls the wound edges closer together and helps expel serum from the clot.
What happens after the clot retracts?
The vessel begins healing and repair; smooth muscle cells reproduce, helping restore the vessel wall.
Why does the clot eventually need to be removed?
Because once the vessel is healed, the clot becomes unnecessary and could block flow — so it must be dissolved.
What enzyme dissolves the clot?
Plasmin — formed from the inactive precursor plasminogen.
What converts plasminogen into plasmin?
Plasminogen activators, such as tissue plasminogen activator (tPA).
What is the function of plasmin?
It digests fibrin, breaking down the clot (fibrinolysis).
What is thrombosis?
An inappropriate or abnormal clot that forms inside a blood vessel, usually a vein, without injury.
What is a thromboembolus?
A clot that breaks free and travels through the bloodstream — it can block vessels elsewhere, leading to serious conditions like stroke or pulmonary embolism.
What could happen if one of the hemostatic factors is missing?
A bleeding disorder may occur (e.g., hemophilia), since the chain reaction for clot formation cannot complete.
Which proteins and cells are most active during hemostasis?
Platelets, clotting factors, and fibrinogen — all work together to form a stable clot.
What is the myocardium?
The muscular layer of the heart responsible for contracting and pumping blood.
What are the main characteristics of myocardial tissue?
Striated like skeletal muscle
Small, uninucleated cells
T-tubules are present
Sarcoplasmic reticulum (SR) is similar to skeletal muscle
Calcium (Ca²⁺) comes from both the SR and interstitial fluid
Composed of autorhythmic and contractile cells
Myogenic (generates its own action potential)
Cells connected by gap junctions at intercalated discs
Cells are branched
Why is the myocardium said to be striated?
Because it has sarcomeres (repeating actin and myosin filaments) like skeletal muscle.
What is the difference between autorhythmic and contractile cells?
Autorhythmic cells (1%): Generate their own action potentials (pacemaker cells).
Contractile cells (99%): Respond to action potentials by contracting and pumping blood.
What makes cardiac tissue myogenic?
It can generate its own electrical impulses without stimulation from the nervous system.
What are intercalated discs?
Specialized junctions that connect cardiac cells; they include gap junctions (for electrical signals) and desmosomes (for mechanical strength).
What is the function of gap junctions in the heart?
They allow ions to flow between cells, enabling synchronized contractions (functional syncytium).
What is the function of desmosomes?
They anchor cardiac cells together so they don’t pull apart during contraction.
They are stronger than the cell itself.
What percentage of myocardium is autorhythmic?
About 1%.
What percentage of myocardium is contractile?
About 99%.
List the main parts of the heart’s conduction system.
SA (sinoatrial) node
AV (atrioventricular) node
Bundle of His (AV bundle)
Bundle branches
Purkinje fibers