week 7- equality & diversity, electrolytes, acid-base, kidney stones
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
differentiate between diversity and the legal notion of equality
Diversity is to do with acknowledgement of alterity among people in terms of their community, culture, beliefs, life experiences, individuality (we are NOT the same).
Equality is to do with fairness of opportunity and observing the rights of people so that their alterity is not discriminated against.
give an account of how diversity informs the ethical notion of equity
Treat equals equally, and unequals unequally.
Treating people justly does not mean treating everyone identically, if it disregards features of diversity that can place people at an unfair advantage in society
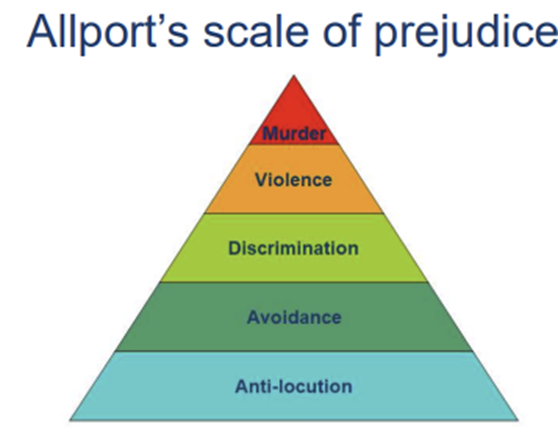
outline the link between prejudice and discrimination
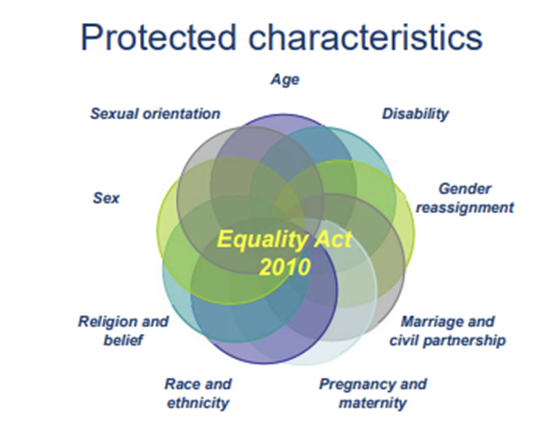
list the 9 diversity strands protected in law
discuss the definition of disability
“…has a physical or mental impairment and the impairment has a substantial and long-term adverse effect on his or her ability to carry out normal day-to-day activities.”
summarise forms of discrimination
• Direct discrimination– treating people less favourably because of a protected characteristic
• Indirect discrimination– putting people with a protected characteristic at an unfair disadvantage
• Associative discrimination– because of another person’s protected characteristic
• Perceived discrimination– when it is believed that a person has a protected characteristic
• Harassment – through violating a person’s dignity, or a degrading, humiliating, hostile, intimidating, or offensive environment
• Victimisation– detriment to a person who is making use of the Equality Act 2010 or is thought to be doing so
• Instruction to discriminate
what pathology occurs when the kidney start dysfunctioning?
•Acute pulmonary oedema - fluid
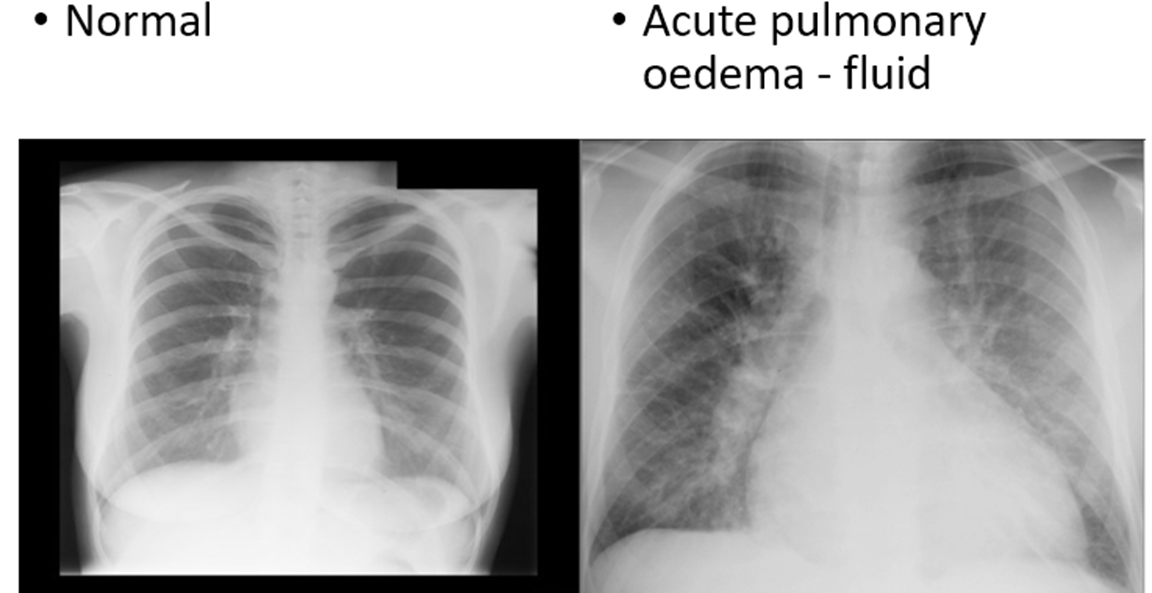
(salt and water imbalance)
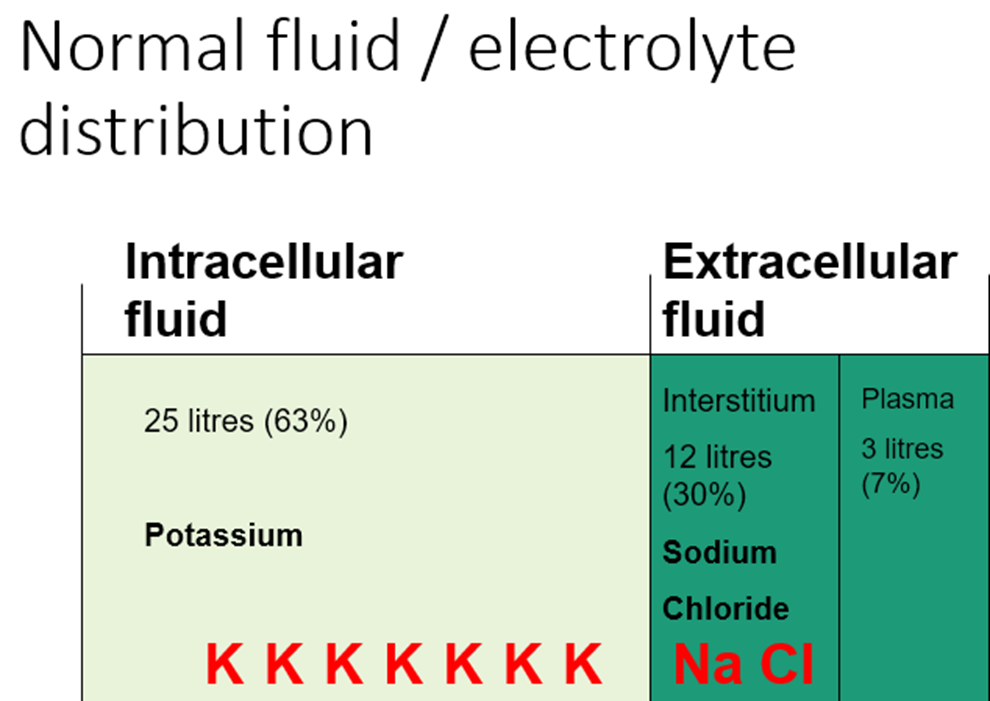
where is potassium, sodium and chlorine found?
what controls the afferent arteriole and what controls the efferent arteriole?
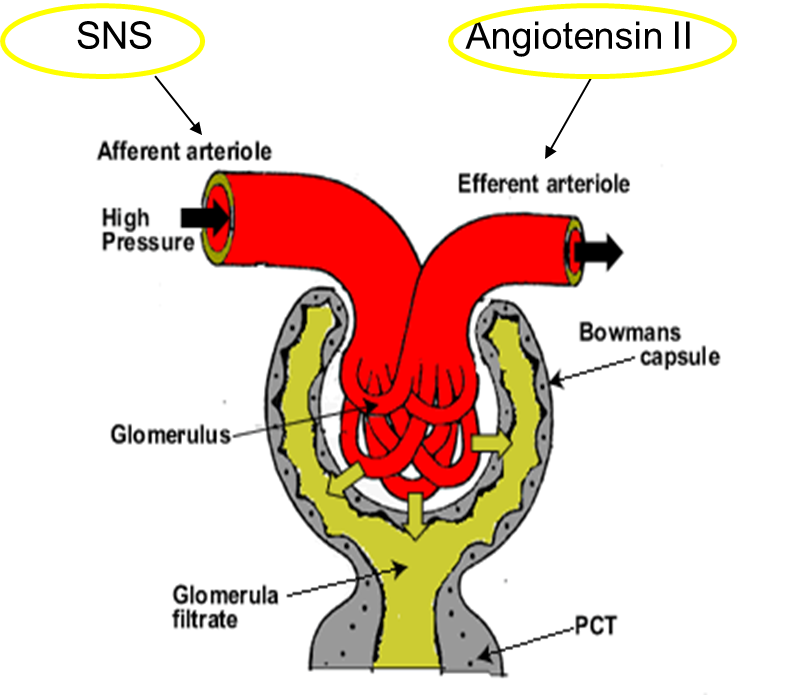
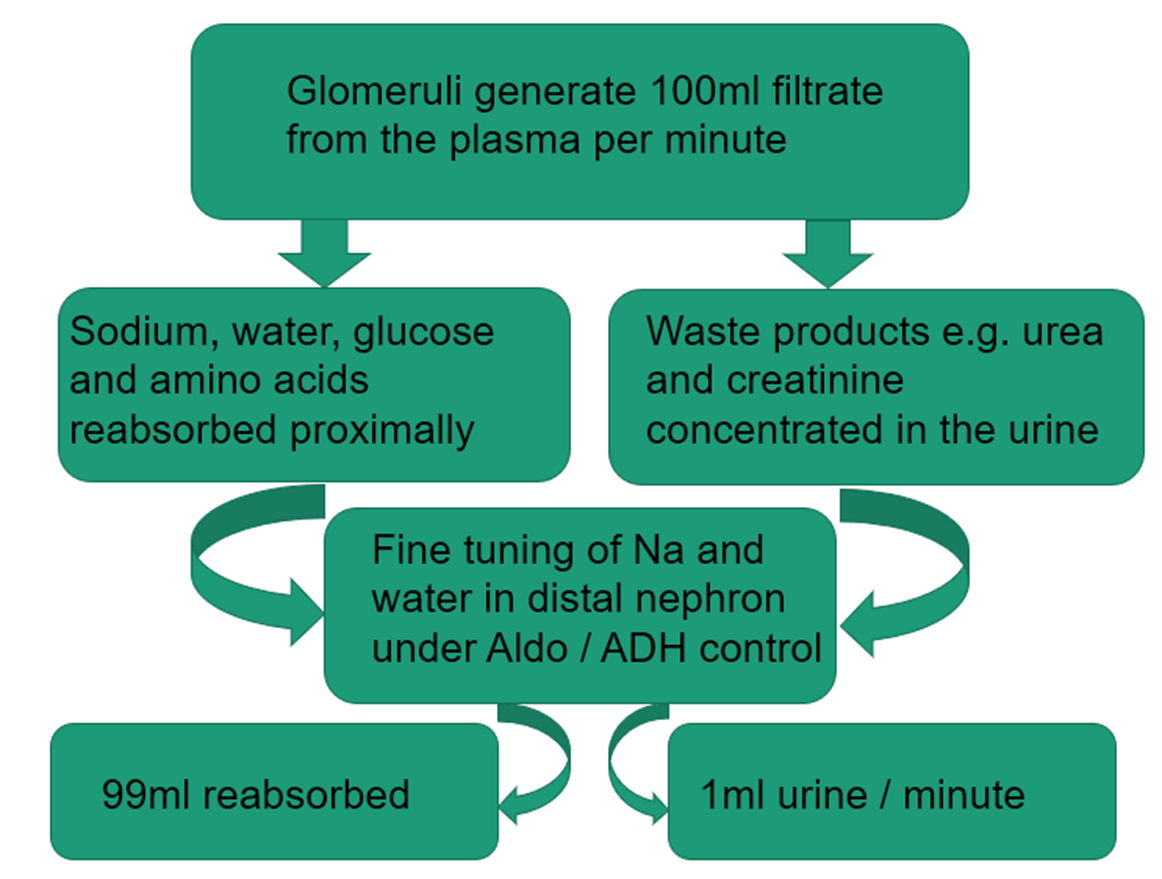
how does the kidney filter?
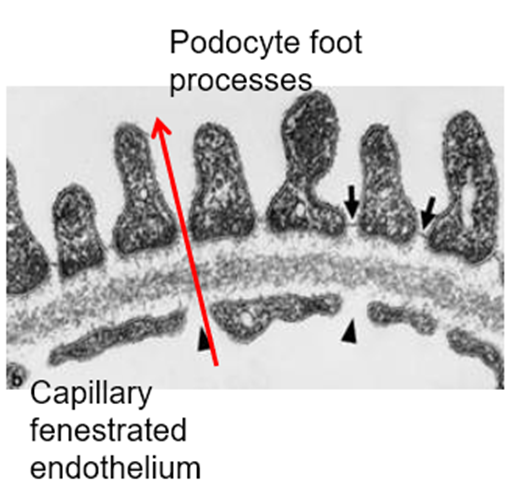
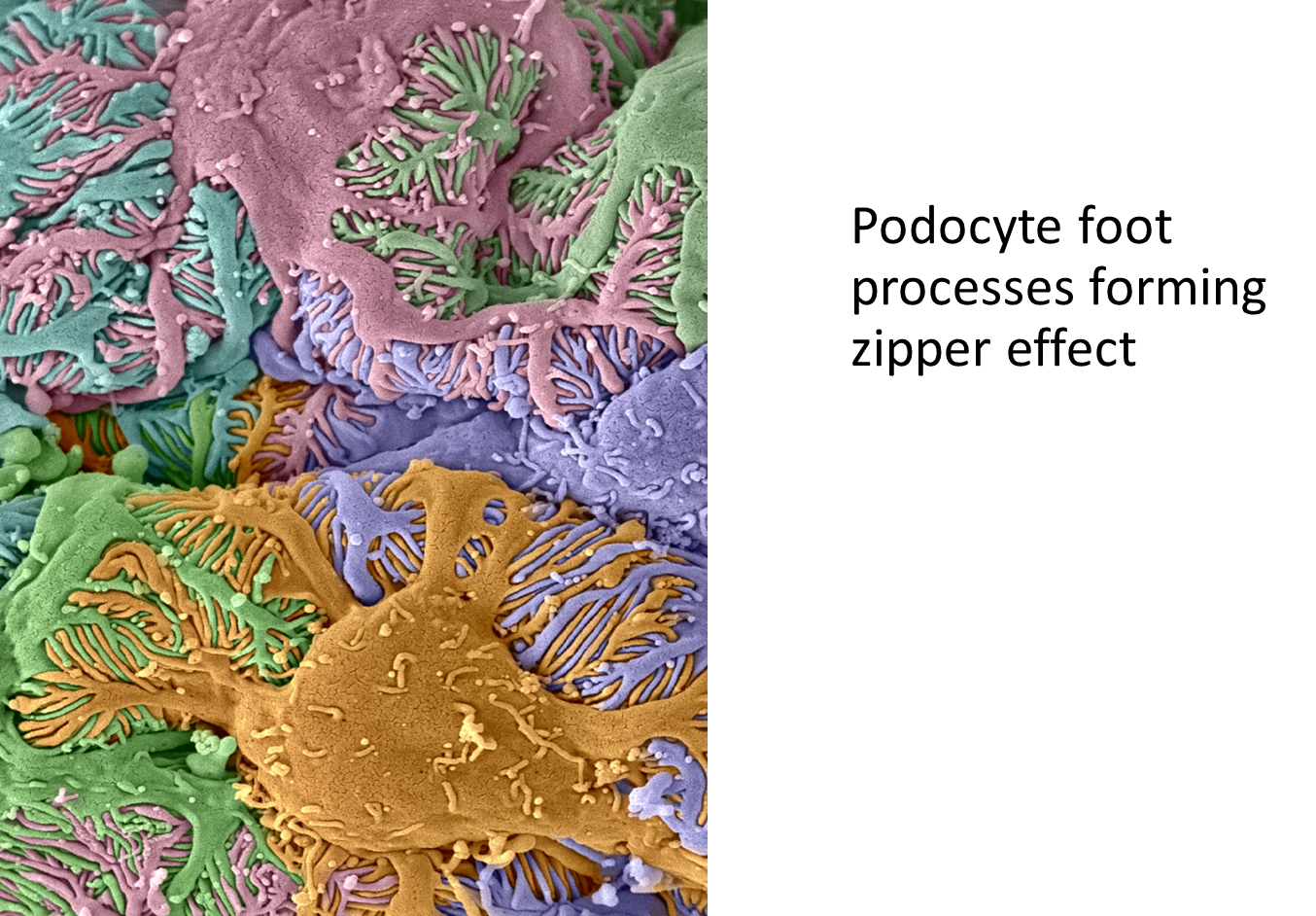
outline The 2 ways the kidney controls fluid / electrolytes
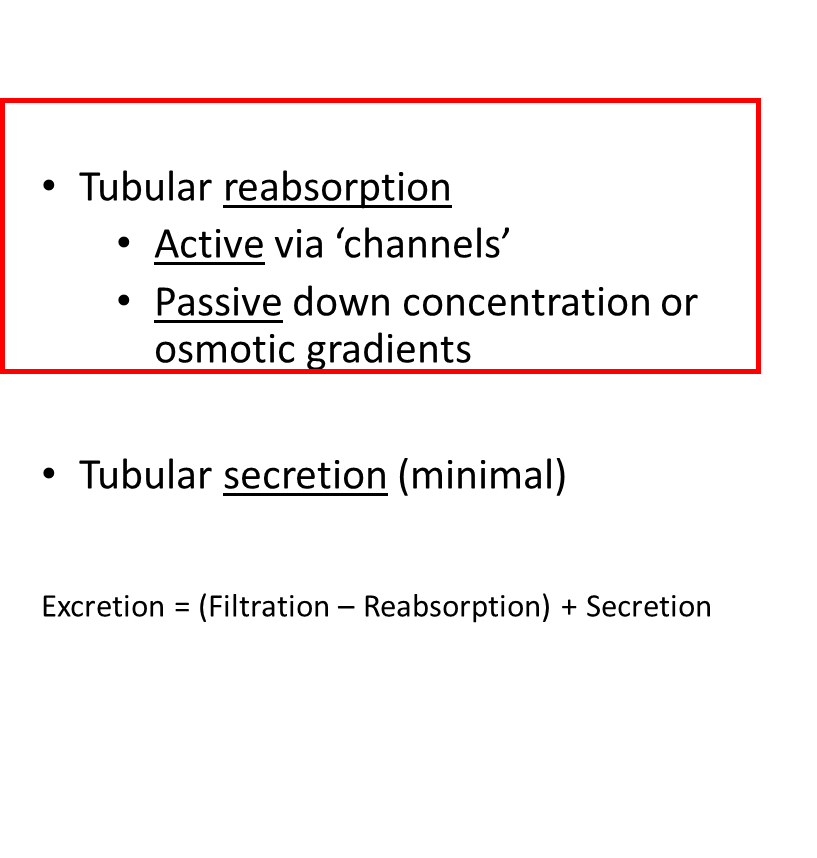
99% of filtrate
(180 litres/day)
is reabsorbed
differentiate between osmole, osmolarity and osmolality
•Measuring the concentration of a solute
•Osmole
•Osmolarity = [osmole] / unit volume (litre)
•Osmolality = [osmole] / unit mass (mosm/Kg)
•Temperature independent
•The measure which is used routinely
•Concentration of solutes in plasma 285-295mosm/Kg
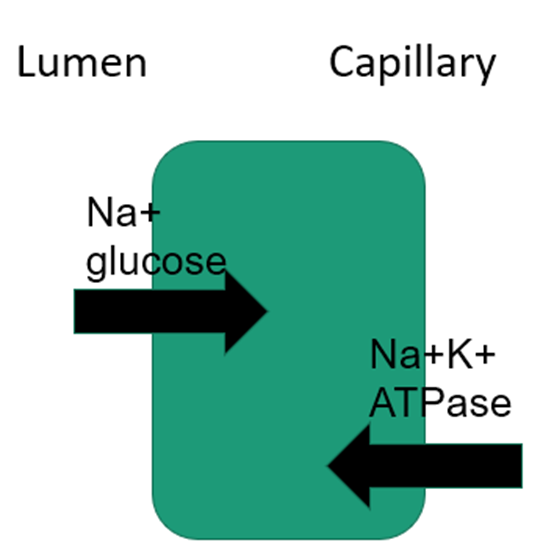
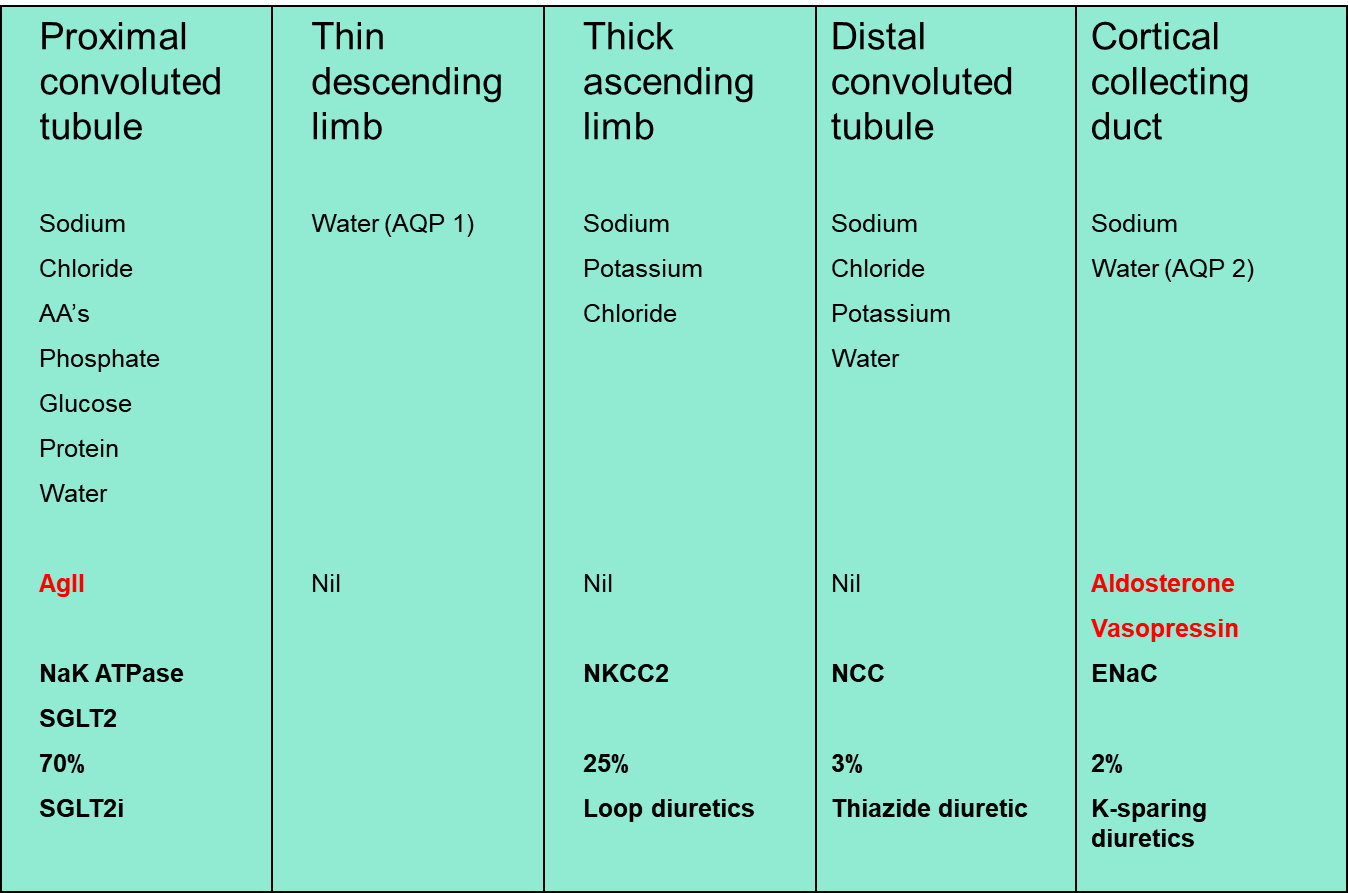
describe the proximal convoluted tubule
The powerhouse
14mm
•70% reabsorption
•Almost everything goes with sodium
•Only hormone particularly involved is angiotensin II which partially controls sodium
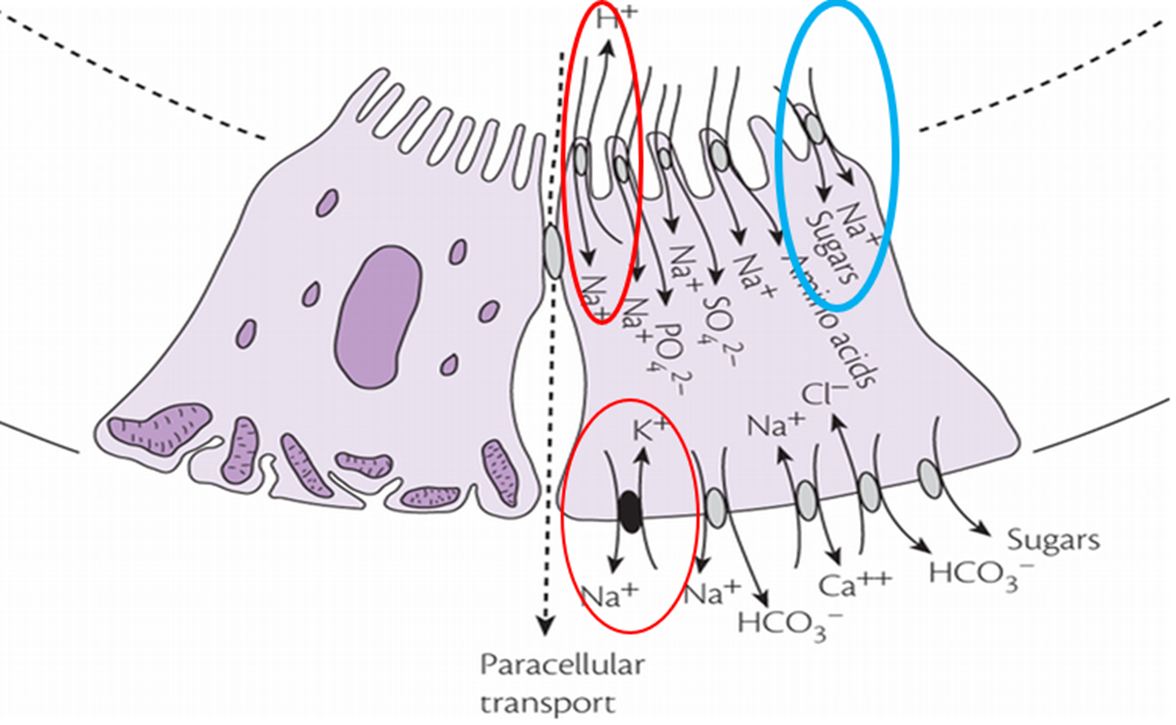
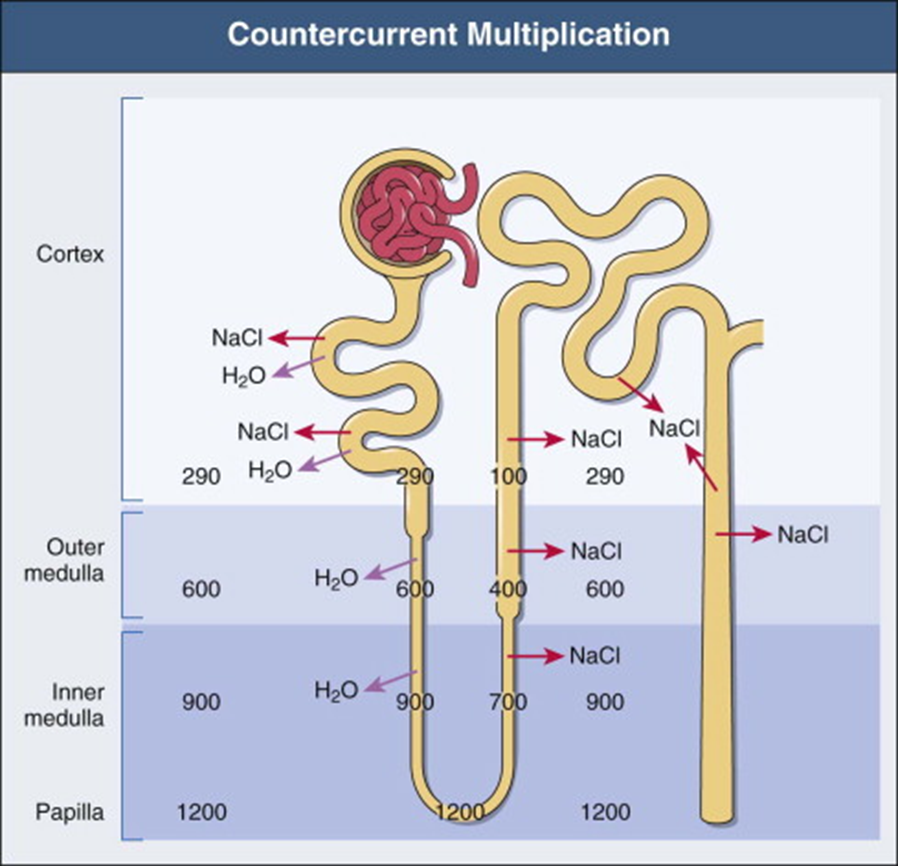
explain the loop rules
1. Thick ascending limb is impermeable to water, but actively transports sodium, potassium and chloride
2. Thick ascending limb provides the concentration gradient to promote water reabsorption from the thin DLH
3. Thin descending limb is freely permeable to salt and water
4. Vasa recta doesn’t wash away the gradient by using countercurrent exchange
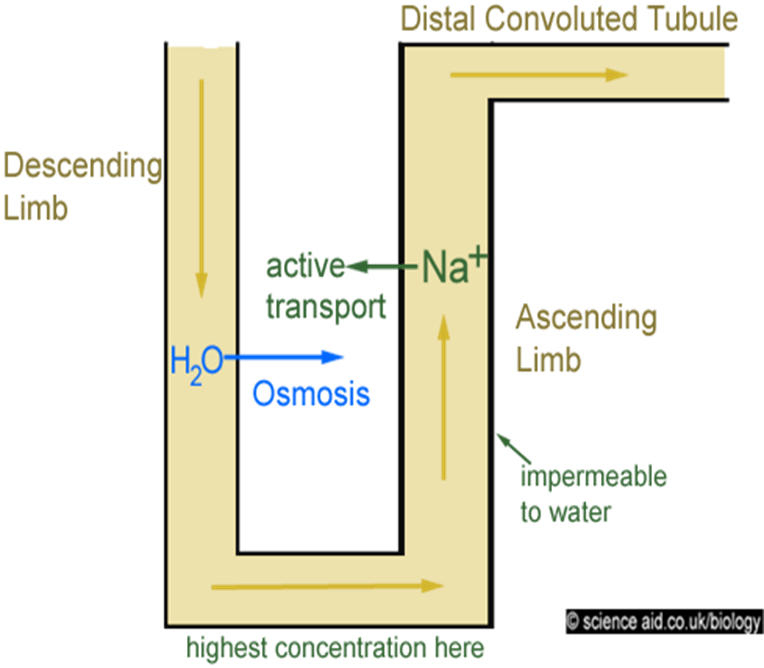
Water follows sodium (osmosis)
hypotonic fluid is delivered to the distal tubule.
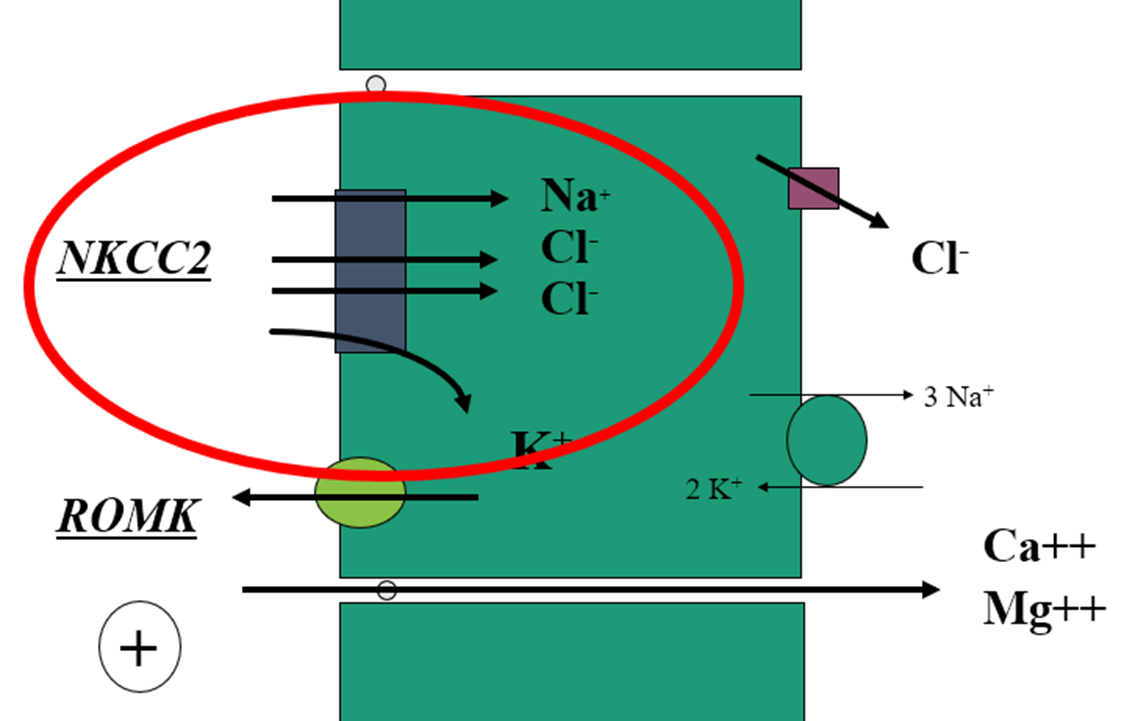
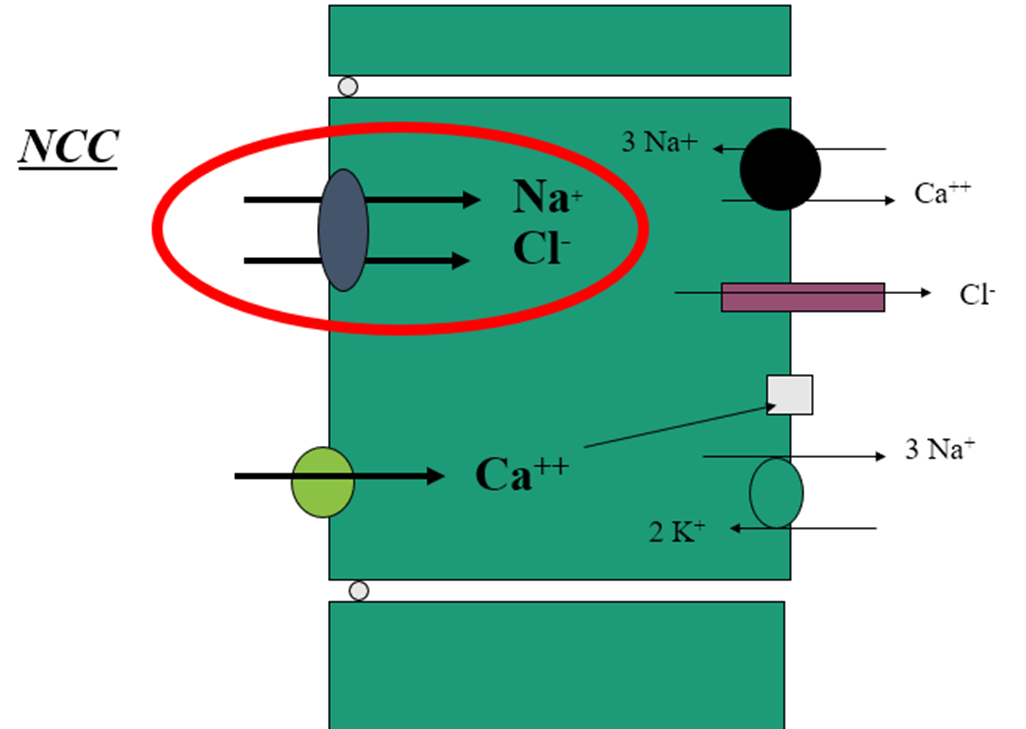
what channel is found in the thick ascending limb of the loop of henle and its function?
what channel is found in the distal convoluted tubule and its function?
1mm long
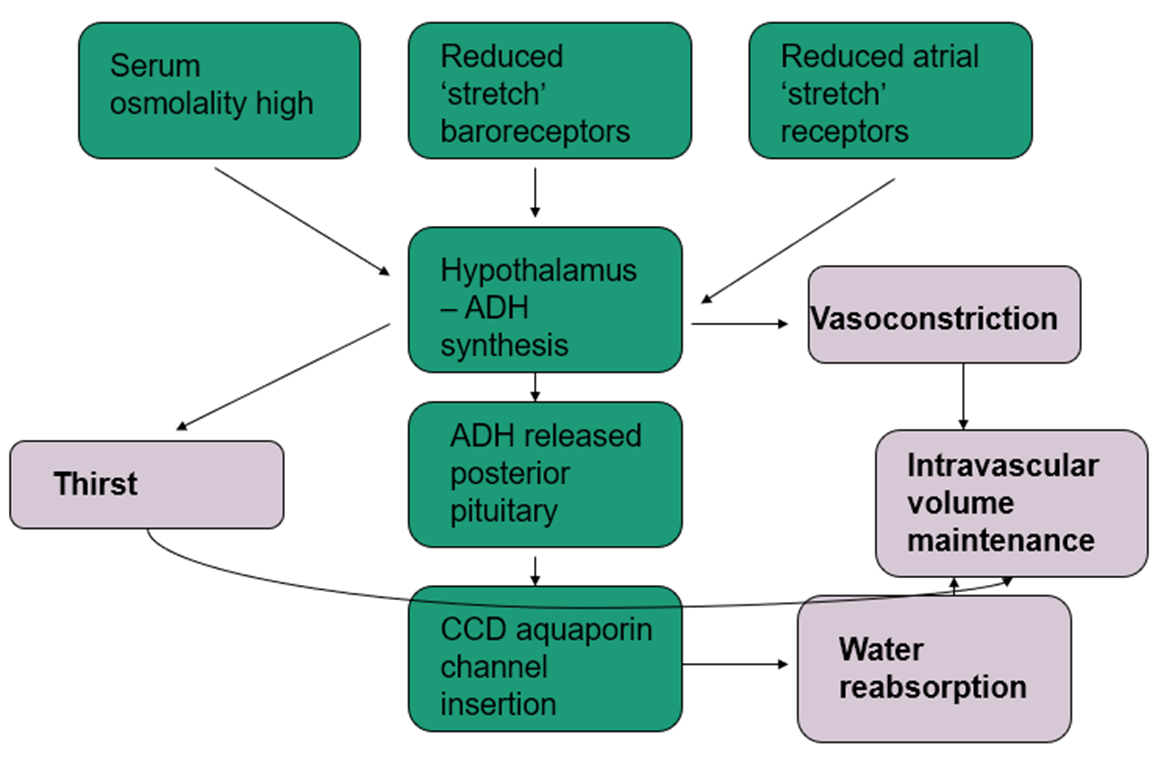
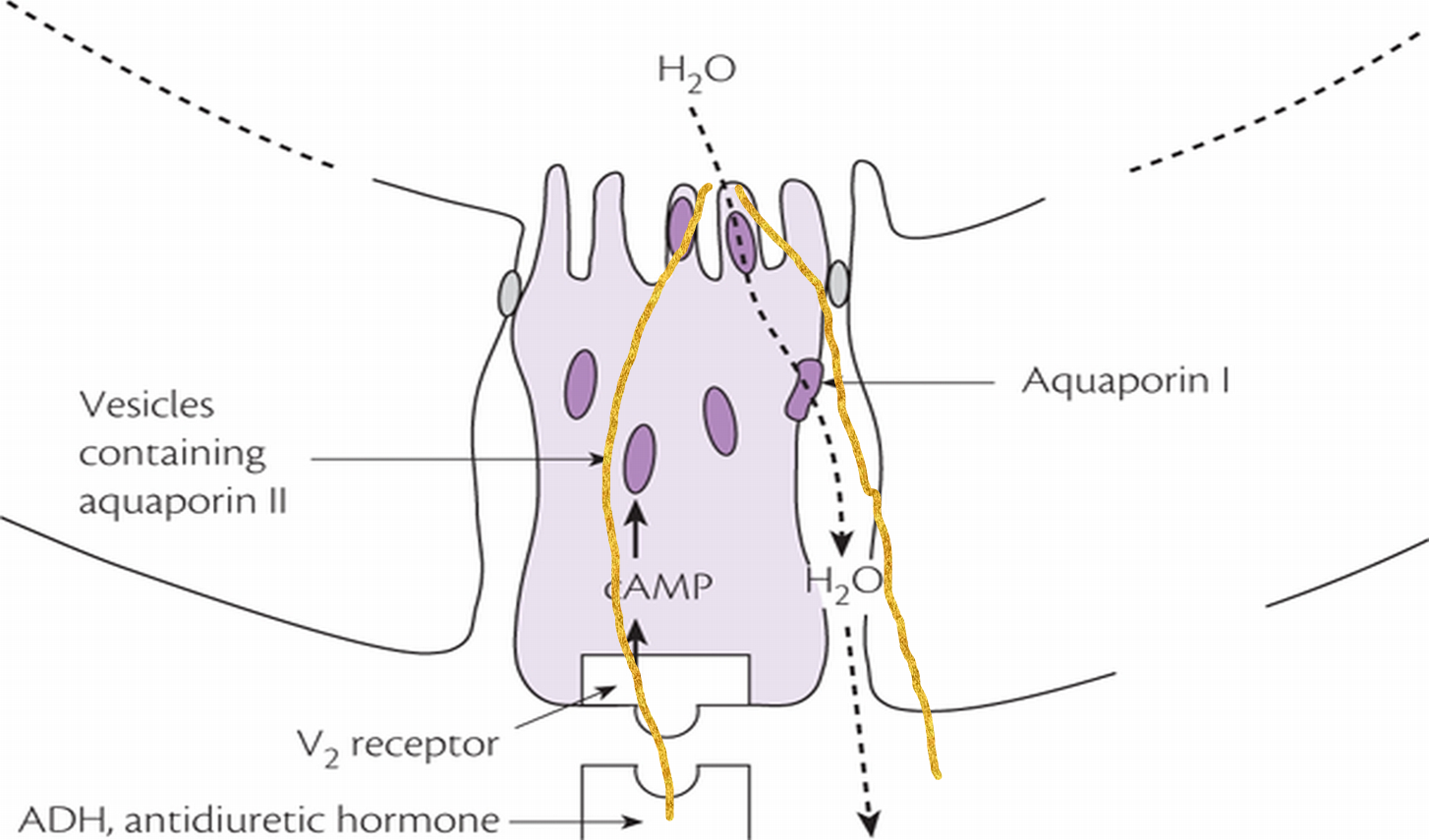
what’s the function of the cortical collecting duct, and link it to the hypothalamus?
•Anti-diuretic hormone (ADH = vasopressin)
•Acts via aquaporin channels
•Prominent role in acute stress / volume depletion
how is aldosterone released?
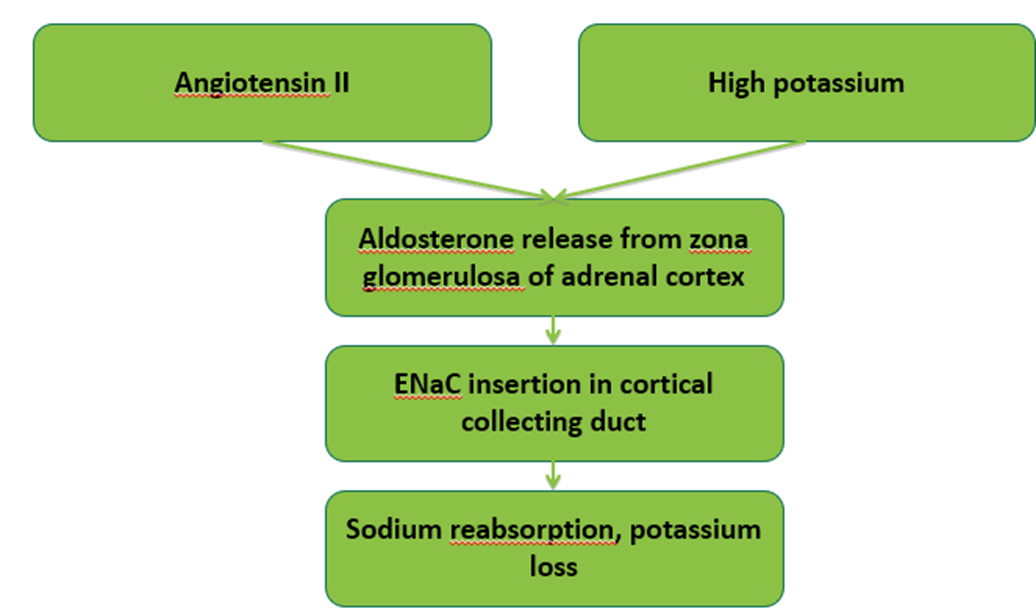

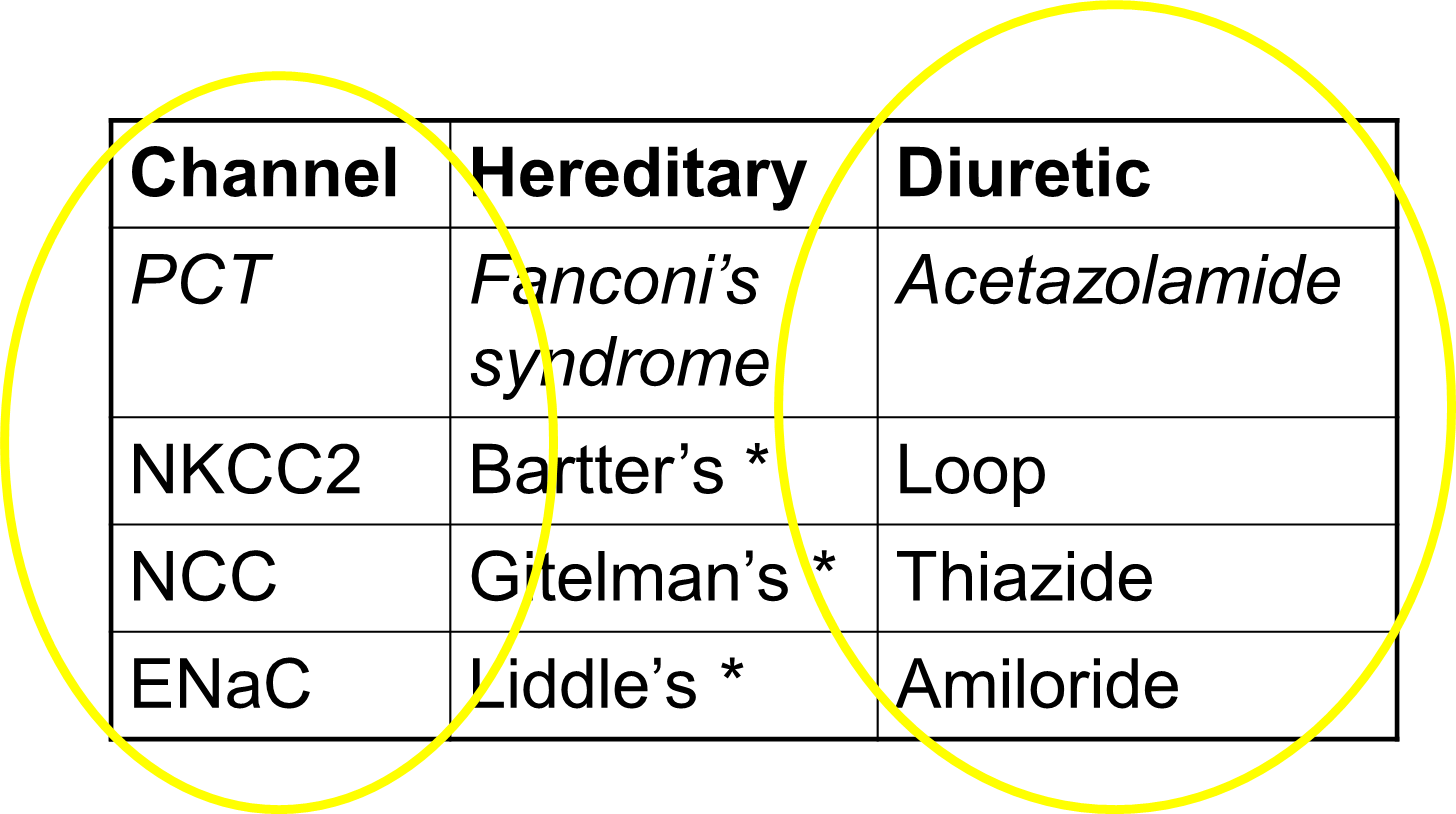
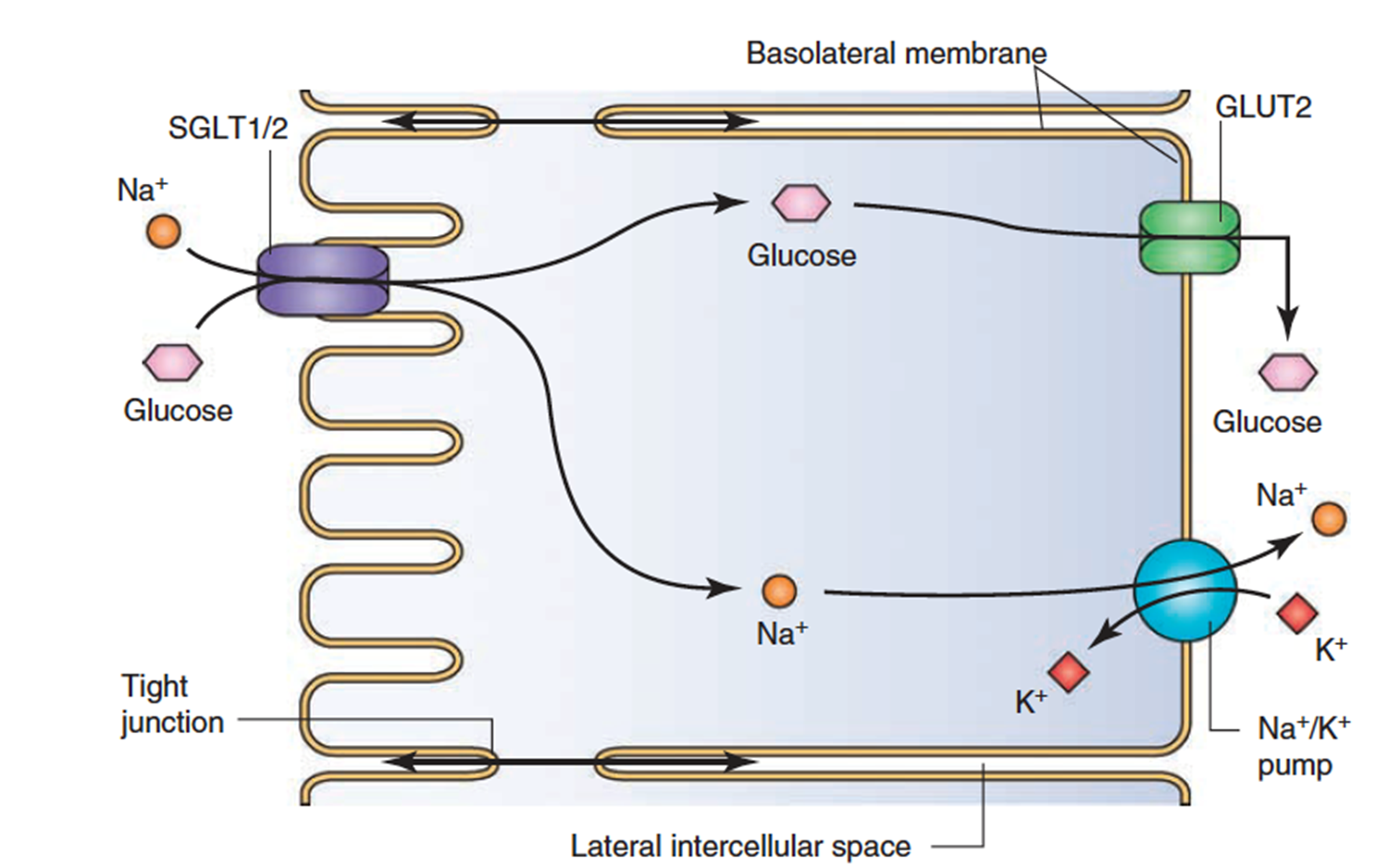
what are the main channels in the nephrons and where are they found?
•NaK ATPase / NaH antiporter (PCT)
•SGLT2 (PCT)
•Sodium dependent glucose co-transporter
•98% filtered glucose is reabsorbed in PCT by SGLT2
•If the amount of filtered glucose is high, the co-transporter is saturated and glucose excreted in the urine
•NKCC2 (Thick ALH)
•NCC (DCT)
•Aquaporin (CCD)
•ENaC (Cortical collecting duct)
which diretic is best for when each of the nephron’s channels don’t work?
describe waste products
•Main measured ones are urea and creatinine
UREA-•By product of amino acid metabolism in liver
•Reabsorbed in inner medullary collecting ducts (passively)
•Involved in countercurrent exchange and maintaining concentration gradient
CREATININE-•Creatinine (breakdown product of creatinine phosphate, muscle metabolism)
•Freely filtered at the glomerulus
•Not reabsorbed
•Minimal tubular secretion (10%)
•Give an estimate in blood of how well kidneys working
•Attributed to the ‘uraemic syndrome’ when levels are high
outline urinary electrolytes
•Urinary sodium
Dietary intake in steady state
Induced natriuresis (diuretics)
Assess cause of hyponatraemia
•Urinary chloride
Suspected diuretic abuse
•Urinary calcium
Differentiate between Bartter’s / Gitelman’s
•Urinary potassium / urea rarely used
describe urine and its volumes
•Min / max output per day
Dependent on kidneys ability to concentrate urine (200-1400mosm/Kg)
Maximum urine osmolality 1400 mosm/Kg
Minimum urine osmolality 50 mosm/Kg
600 mosmol of waste products excreted /day
Minimum urine output = 600/1400 =
0.4 litres/day
Maximum urine output = 600/50 =
12 litres/day
name different diuretics and where they work in the nephrons.

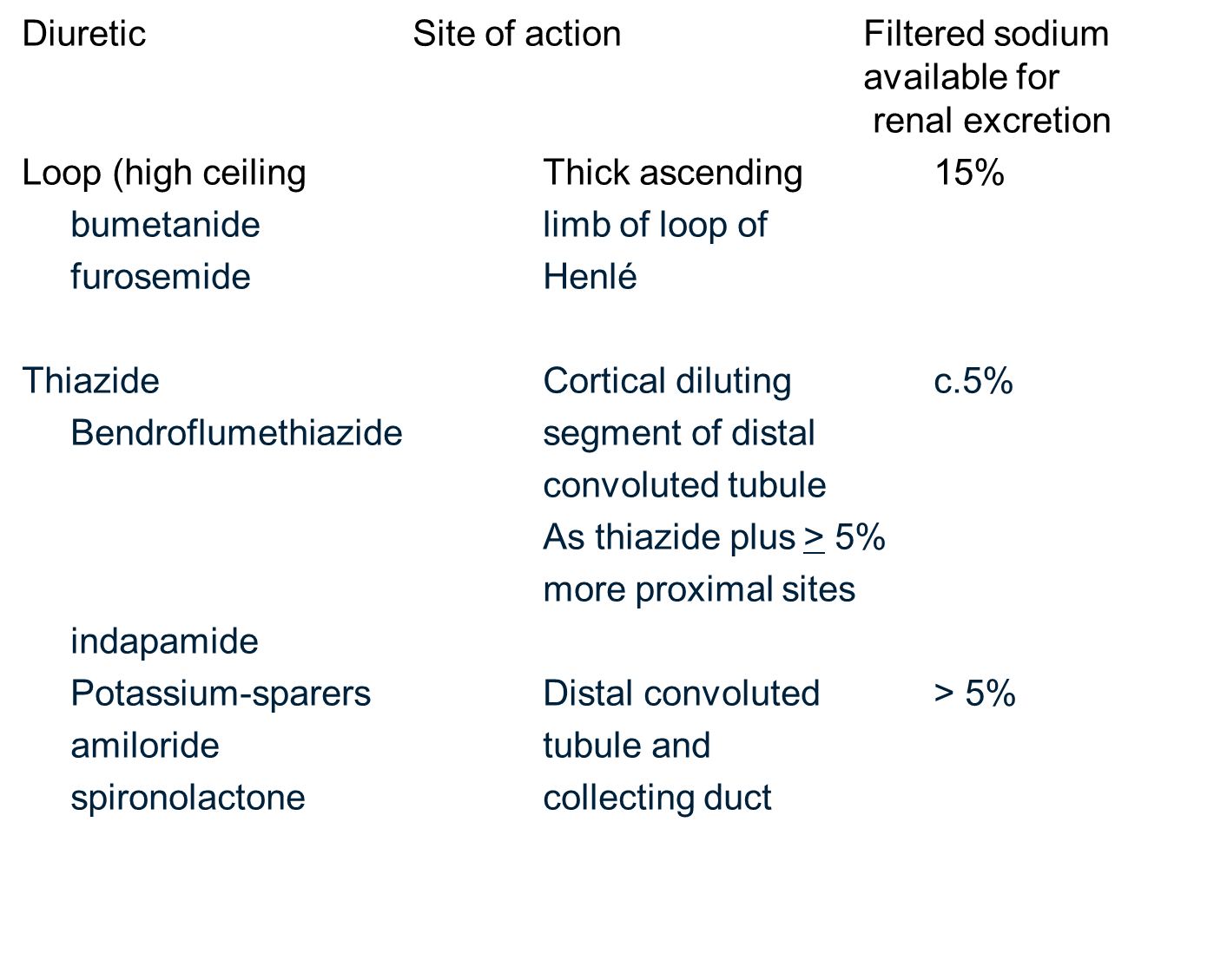
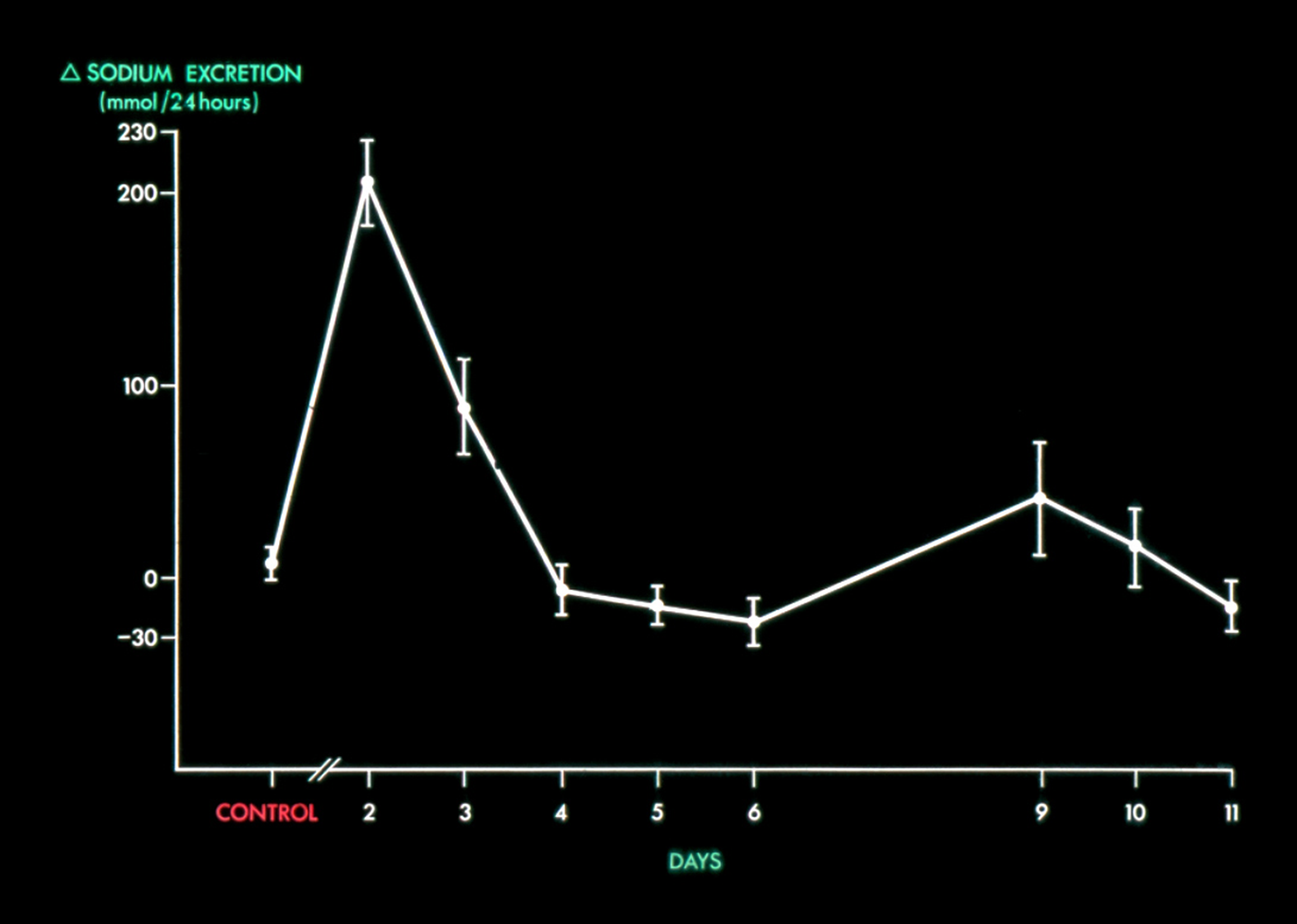
understand the sodium excretion levels when taking diuretics
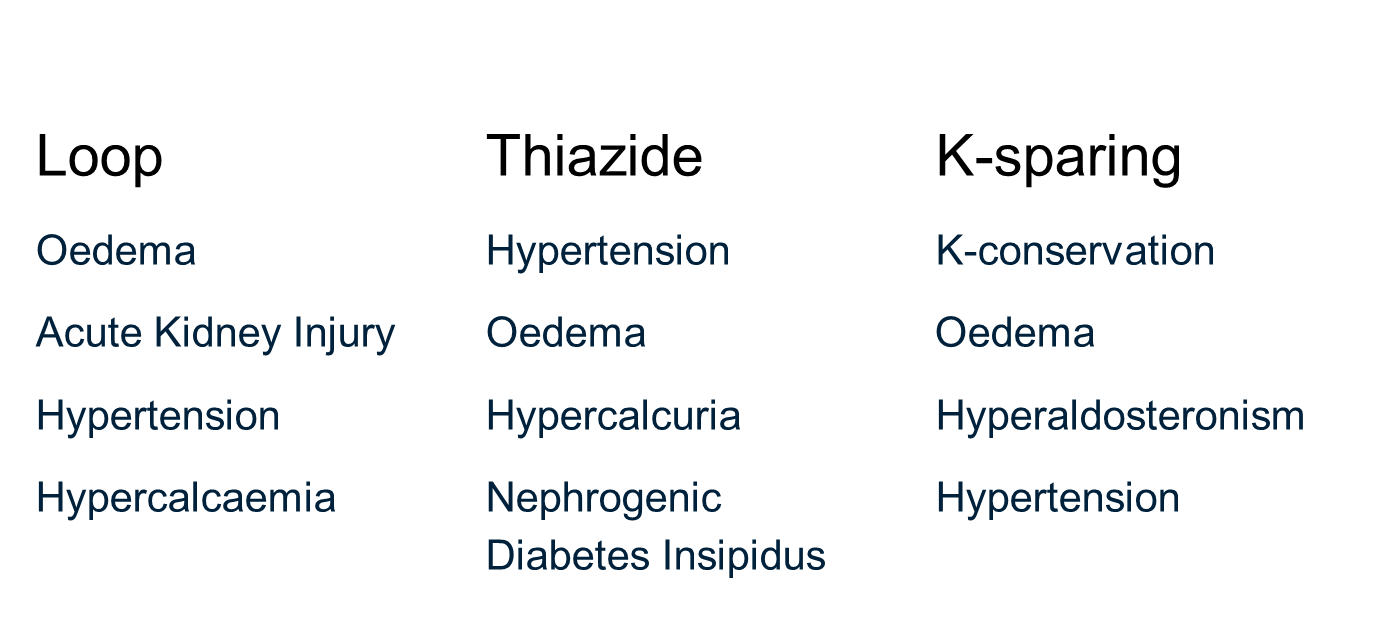
name the classes and in which conditions each one is used
name the potency, absorption, onset, duration, dose-response and effectiveness in advanced CKD of each type of diuretic:
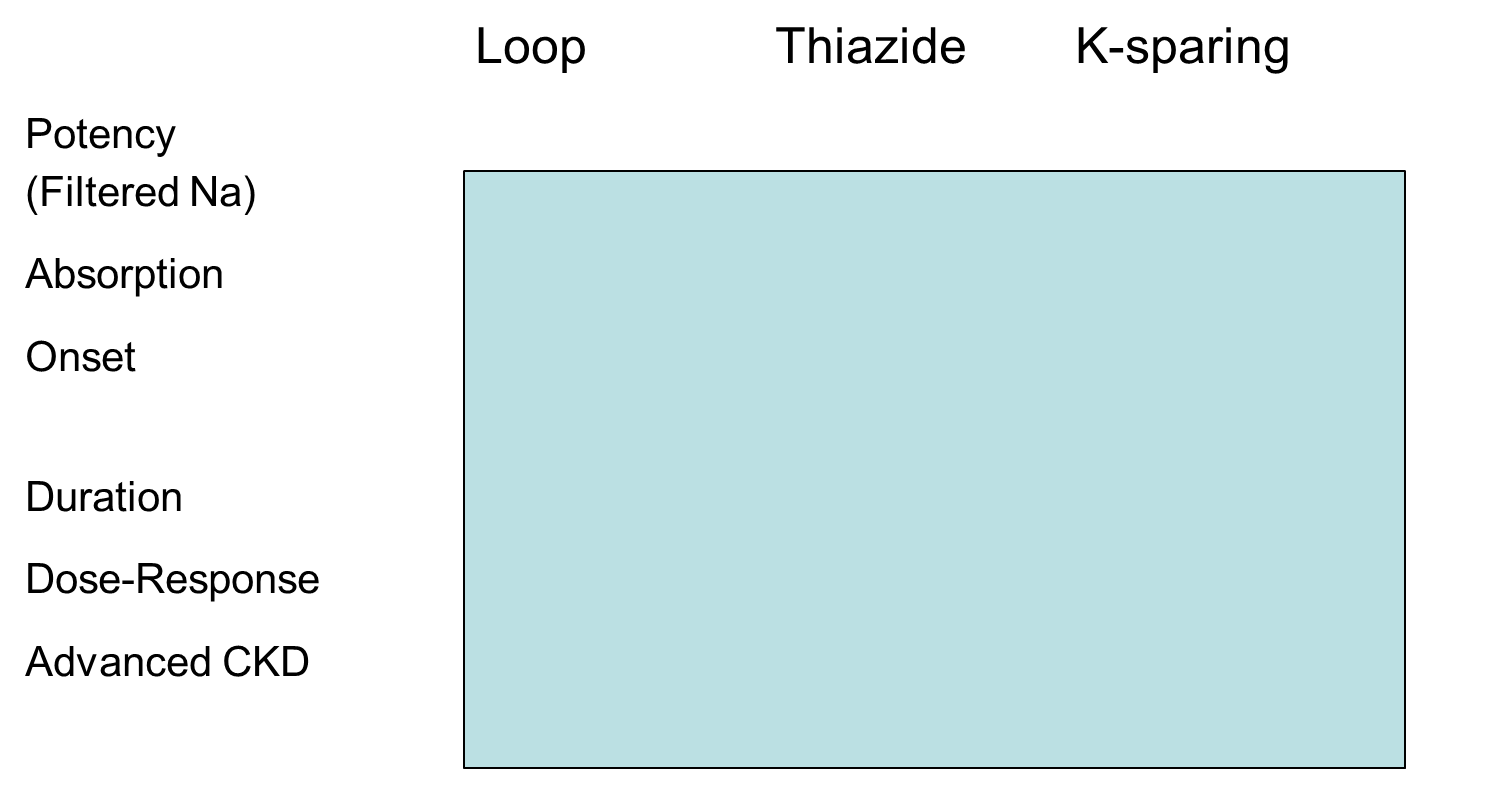
Hint!!
Loop= POWERFUL
Thiazide & potassium-sparing= WEAK
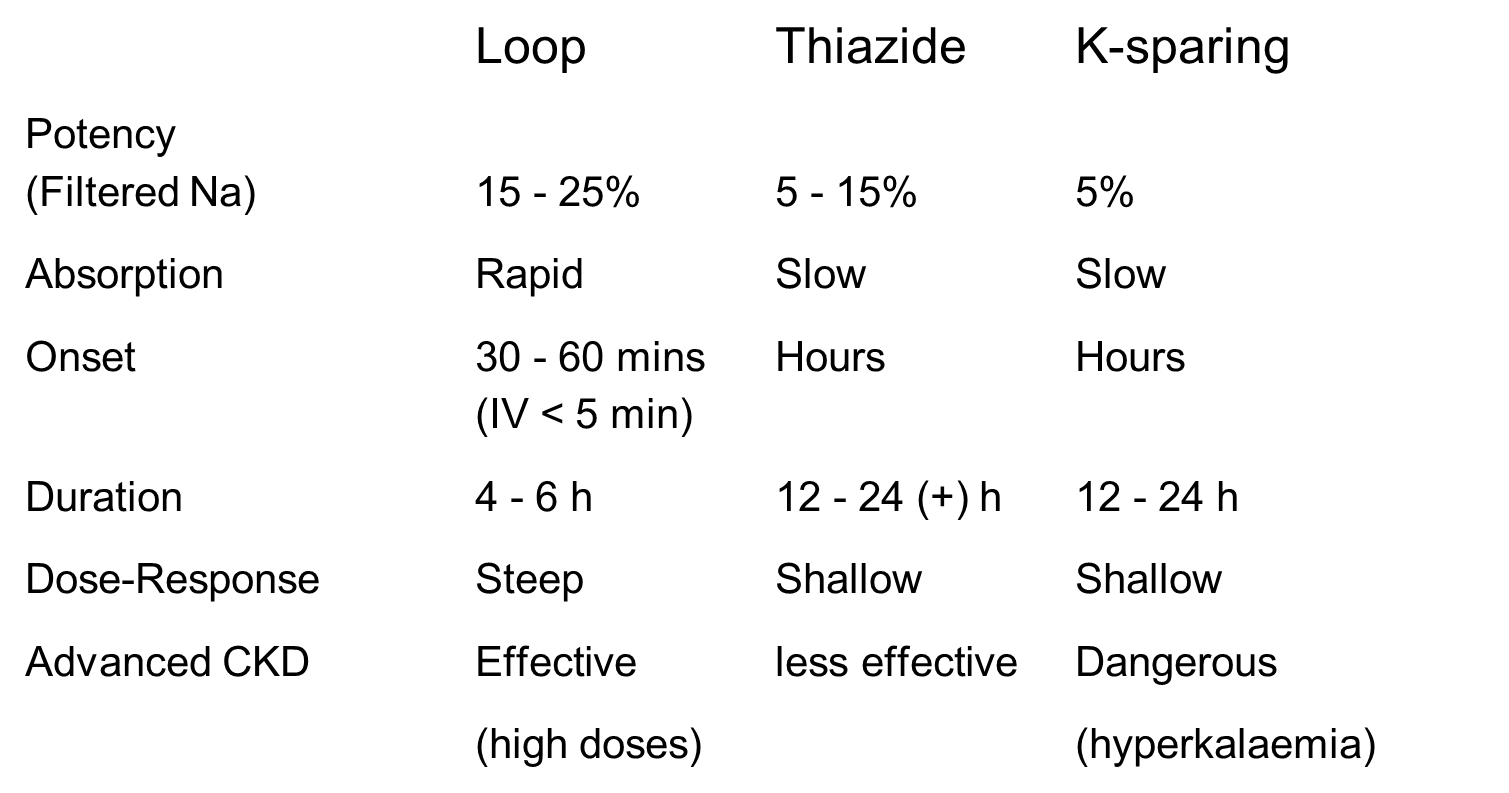
Loop= POWERFUL
Thiazide & potassium-sparing= WEAK
how do Loop diuretics (e.g. furosemide, bumetanide) work?
•Inhibit Na/K/2Cl co transporter in TALH (thick ascending limb of the loop of Henle)
•Increase K/Mg/Ca excretion
•Main use in heart failure and chronic kidney disease
•Metabolic alkalosis
•Ototoxicity in high doses
how do Thiazide diuretics (e.g. bendroflumethazide, metolazone, chlorothiazide) work?
•Act on Na/Cl cotransporter in DCT
•Main use is in hypertension
•Increase K/Mg excretion but reduce Ca excretion
•Can be used to reduce hypercalcuria (renal stones)
how do Potassium sparing diuretics (e.g. spironolactone, amiloride) work?
•Spironolactone- mineralocorticoid receptor antagonist
•Useful for hyperaldosterone states (heart failure, cirrhosis)
•Amiloride – sodium channel blocker – blocks ENaC in collecting duct
•Useful in states of low potassium
what are side effects of Thiazide and loop diuretics?
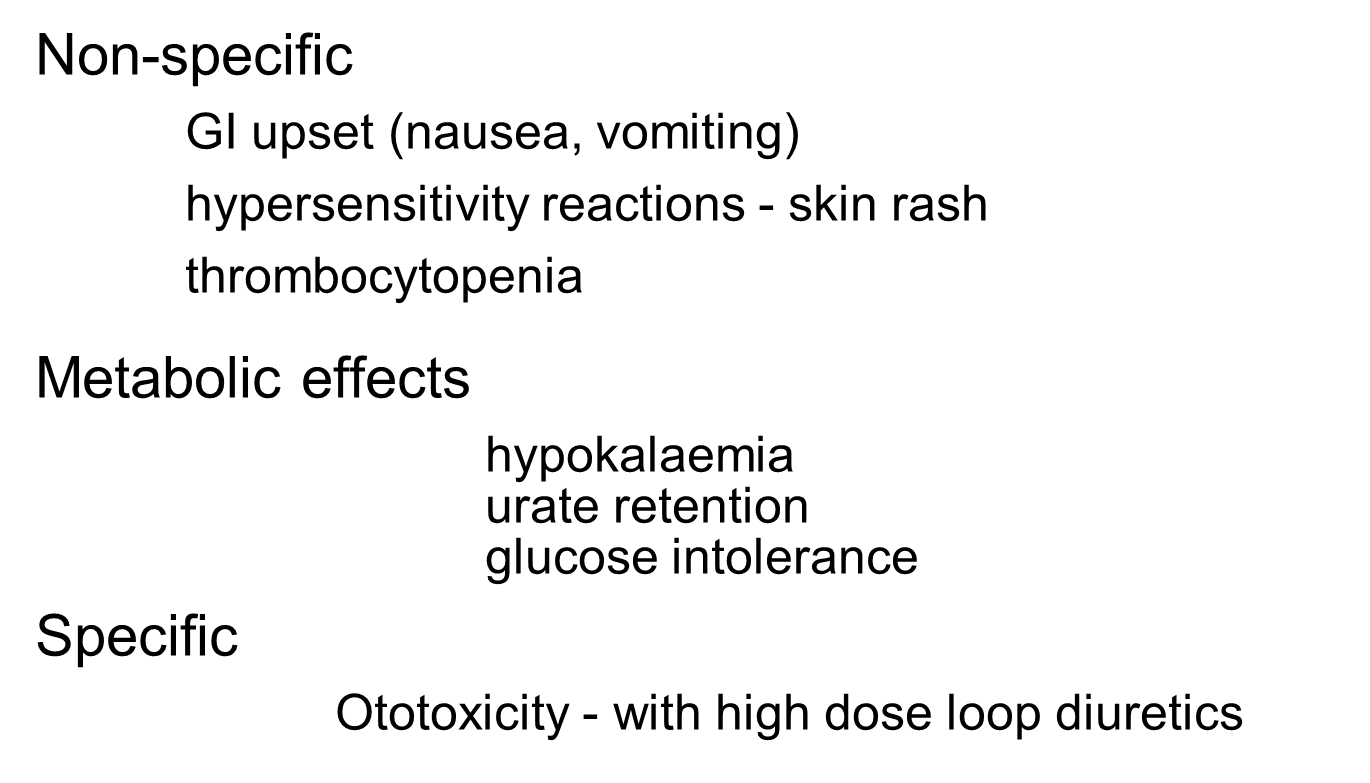
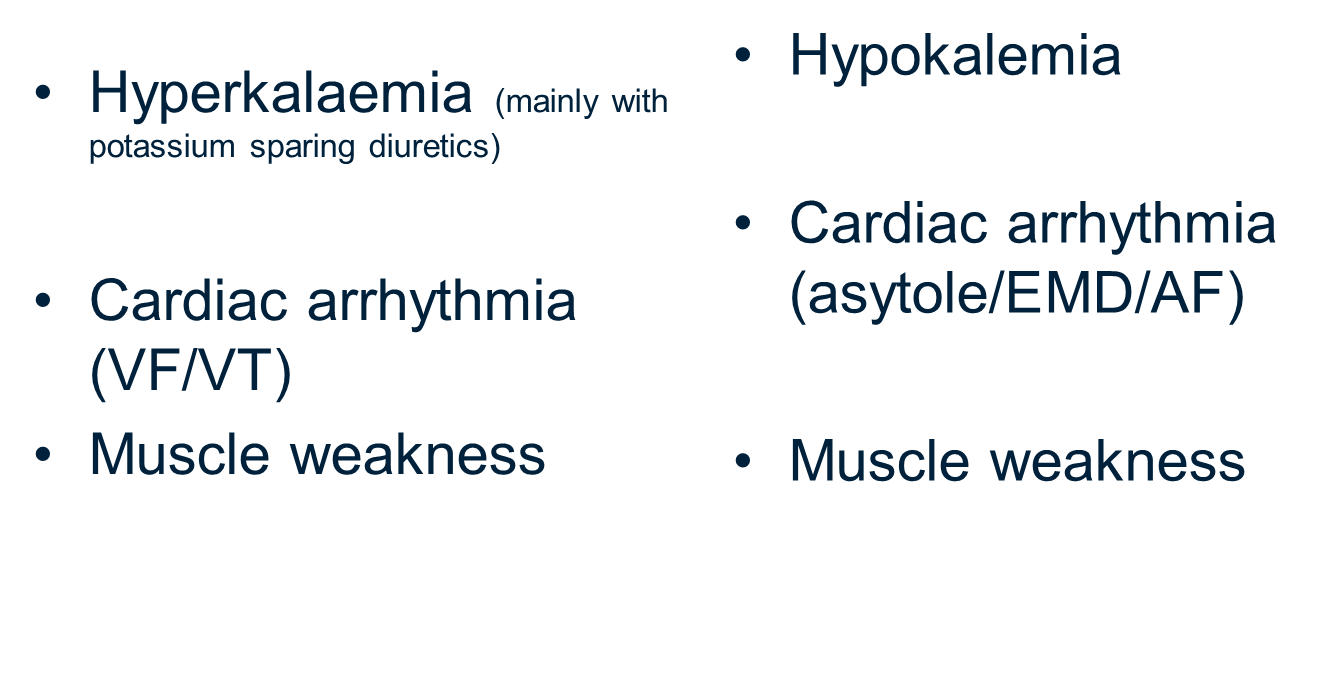
what are major electrolyte concerns with diuretics?
[Medicines which protect kidneys]
correlate Angiotensin converting enzyme (ACE) inhibitors and Angiotensin receptor blockers –e.g. losartan and kidney function
•Effective antihypertensive effect mediated by reduction of Ang II
•Therefore frequently nephroprotective in renal disease especially if proteinuria
•However potential to cause acute drop in GFR if dehydrated or in patient with renal artery stenosis
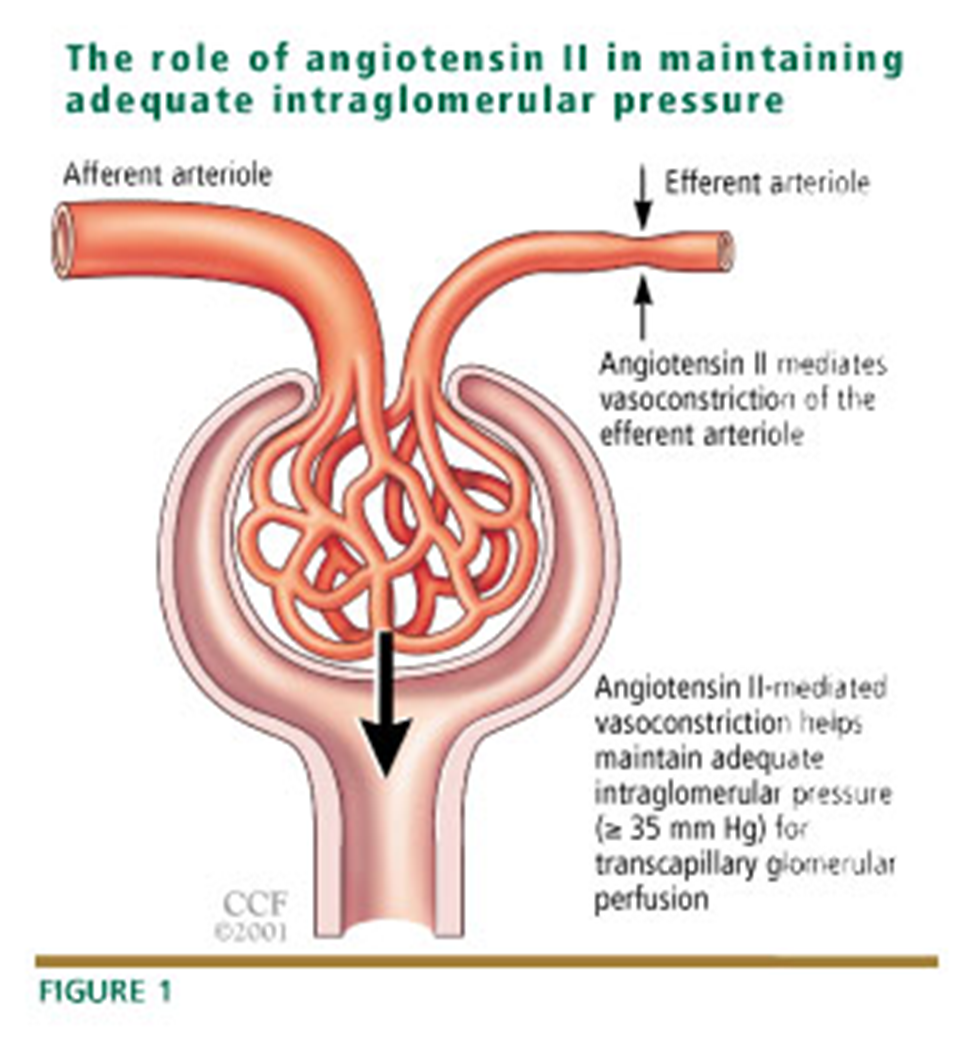
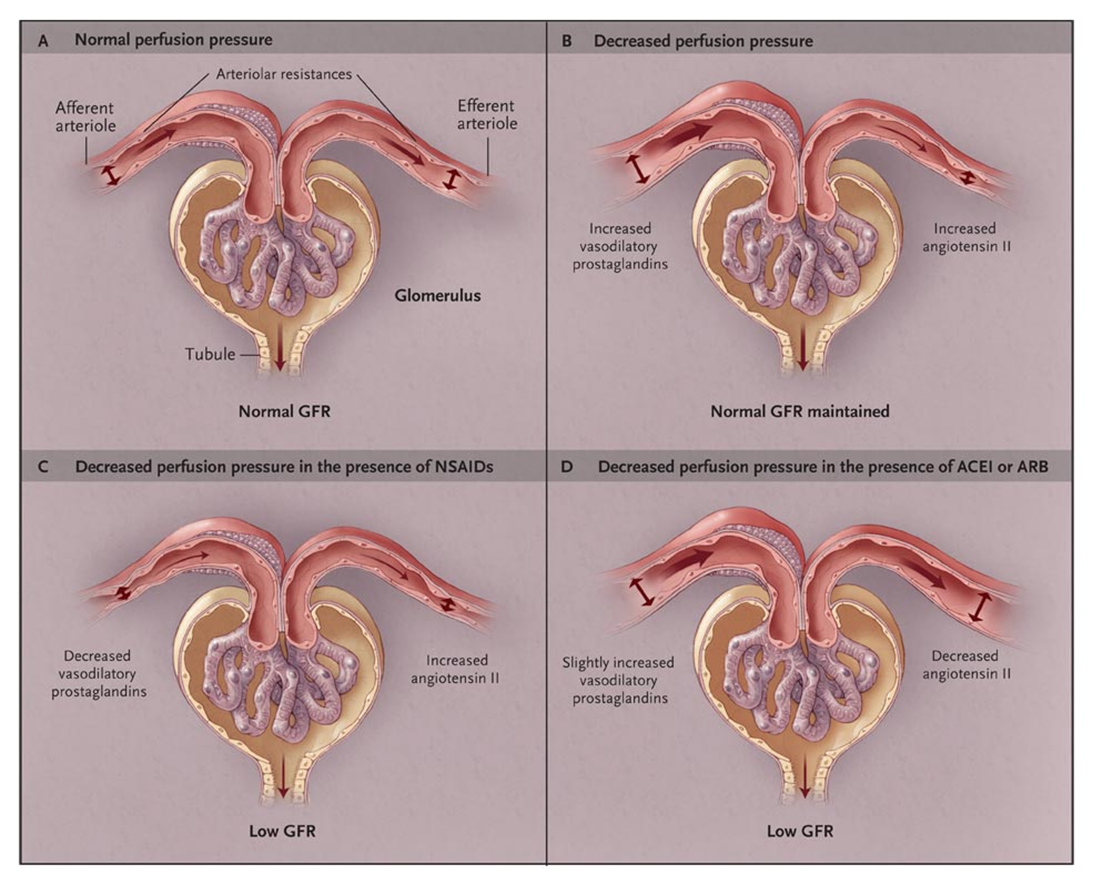
prostaglandins is what opens the afferent arteriole- needed to maintain the correct pressure in the glomerulus
ACE inhibitors
•EVIDENCE BASED KIDNEY PROECTION proteinuric renal disease, cardiovascular disease
–BUT…….
–ACEI associated with loss of renal function
•Bilateral renal artery stenosis
•Co-administered with NSAIDs or large volume diuretics
•When dehydrated or septic
–Angiotensin II – vasoconstriction of the efferent arteriole in attempt to maintain glomerular capillary pressure (ACEI prevent this)
[Medicines which protect kidneys]
correlate Sodium glucose cotransporter 2 inhibition and kidney function
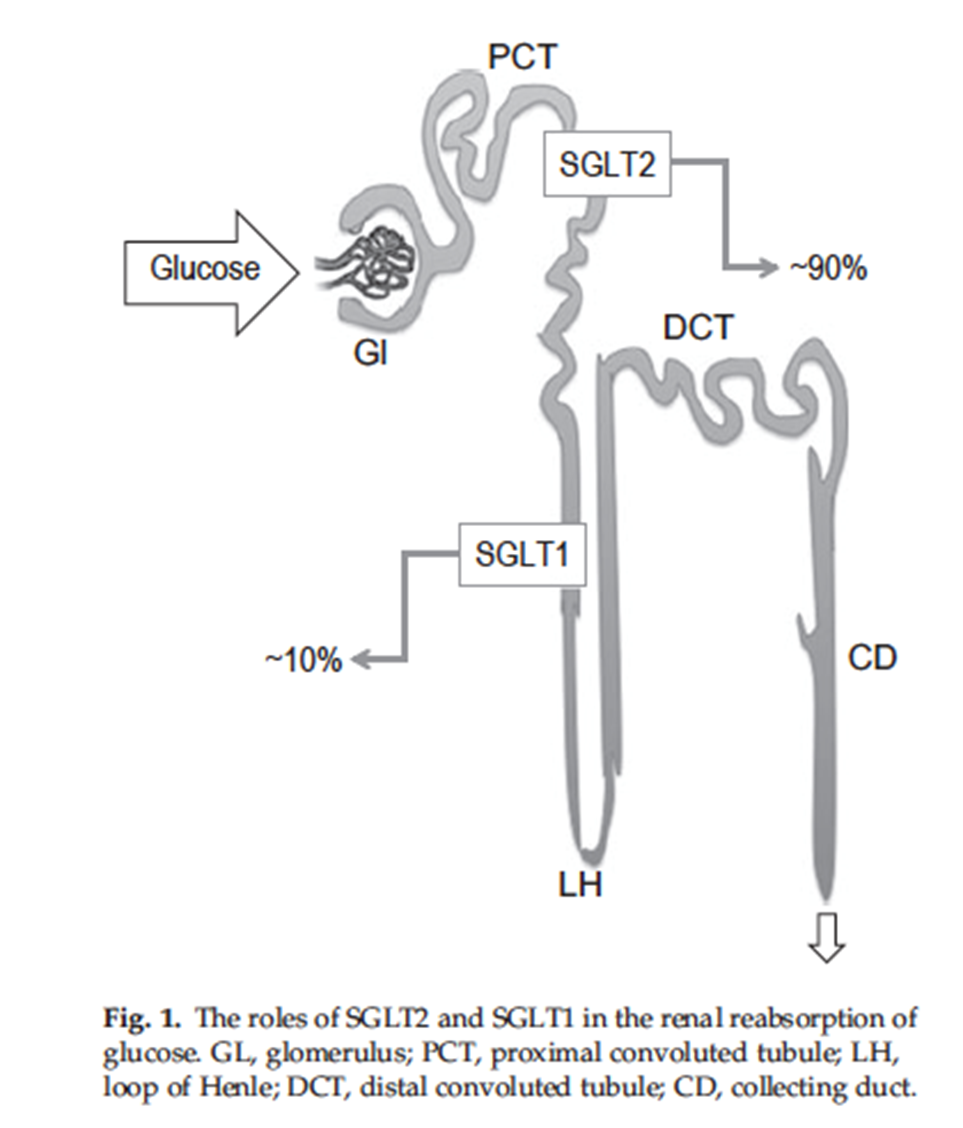
| SGLT1 | SGLT2 |
Expression | Small intestine, Kidney, Heart | Kidney, Ileum (less so) |
Mechanism for glucose transport | Active transport | Active transport |
Co-transport | Na/K (ATPase coupled) | Na/K (ATPase coupled) |
Capacity for glucose transport | Low | High |
% renal glucose reabsorption | Approx 10% | approx 90% |
SGLT2
•↑ distal delivery Na+
•TG feedback reduces GFR
•efferent arteriolar dilation, lowers intra-glomerular pressure
explain clinical acid-base disorders
•In all types of acid-base disorder there is a primary disturbance which tends to make [H+] abnormal
•The acute change will be buffered and there will be a compensatory response – so [H+] remains in or close to normal range, but at expense of abnormal HCO3, or CO2
•Clinical acid base disorders are classified as either
–Metabolic (tendency to perturb HCO3, H+)
–Respiratory (tendency to perturb CO2)
•Compensation can be
–Metabolic (renal) if the primary disorder is respiratory
–Respiratory (ventilation) if the primary disorder is metabolic (addition of H+, loss of HCO3)
outline the diagnosis of acid-base disorders
•In practice, given time the renal compensatory response may be complete, but respiratory compensation may be limited – there is a limit to how hard patients can drive ventilation without tiring, and they can’t stop breathing
•“osis vs aemia”
–More patients will be acidotic (abnormal HCO3) than acidaemic (↓pH)
•Diagnosing the acid-base disorder requires knowledge of H+, HCO3, CO2 (blood gases), electrolytes (Na, K, Cl) and a clinical history
•In many cases the diagnosis will be obvious – e.g. DKA
The suffix -osis (e.g., acidosis, alkalosis) refers to the underlying physiological process or disorder causing an accumulation or loss of acid or alkali in the body.
The suffix -aemia (e.g., acidemia, alkalemia) refers to the actual abnormal blood pH value.
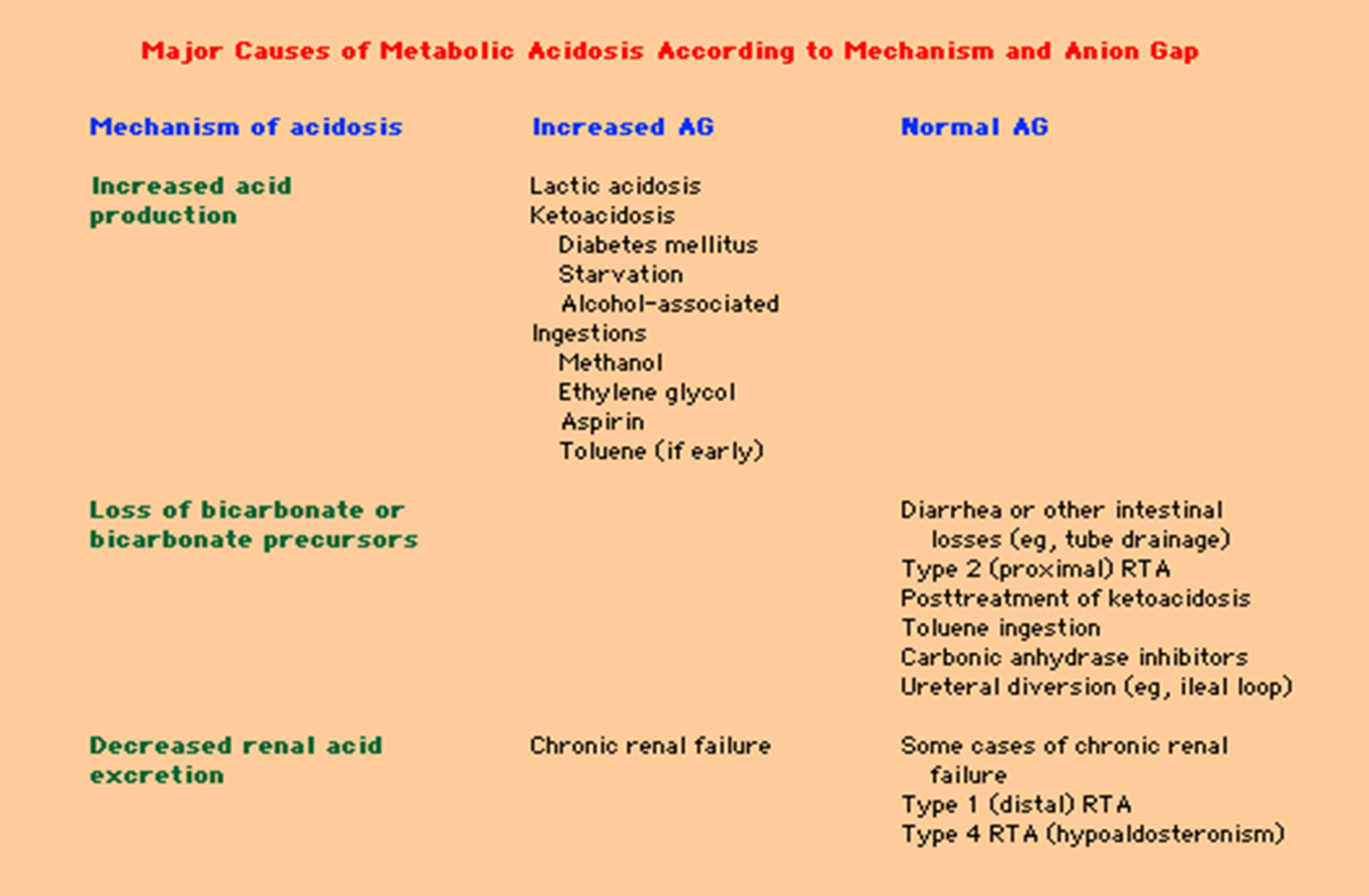
explain the causes of metabolic acidosis
•Causes:
–Too much H+
•Generation of organic acid through metabolism – lactic acidosis, keto-acidosis
•Ingestion of acid (e.g. methanol, ethylene glycol)
•Failure to excrete acid
Renal tubular acidosis
–Not enough HCO3
•Loss in stool (diarrhoea)
•Loss in urine - renal tubular acidosis
•Primary abnormality is fall in plasma HCO3
•Compensatory response is fall in pCO2 due to respiratory drive
•H+ may or may not be elevated
what are the systemic effects of metabolic acidosis?
•Specific symptoms relating to cause – e.g. DKA (diabetic Ketoacidosis)
•General
–CVS
=Arrythmias, ↓cardiac contractility, vasodilation, Hypotension
–Resp
=↑ventilation (Kussmaul’s breathing)
–Metabolic
=Protein wasting, resorption of Ca from bone
–Other
=Neutrophilia
•Presence of metabolic acidosis is a marker of severe physiological derangement – lactic acidosis
what’s the clinical approach to metabolic acidosis?
•Recognise presence of metabolic acidosis from history, biochemistry and blood gases
•Determine whether this is primarily addition of acid, or loss of HCO3
–Anion gap (AG)
•Determine whether compensation is adequate
•Need to know [H+], HCO3, pCO2, U+Es
•Calculate anion gap
–[Na] - [Cl + HCO3]
–Normal range 9-16
–beware ¯albumin - adjust AG ¯ by 2.5 for every 10g/l fall in [albumin]
Now, consider is the respiratory compensation adequate?
•Remember, respiratory compensation demands a fall in pCO2 – this is predictable
–pCO2 should fall 0.125kPa (from 5) for every 1mmol/L fall in bicarb (from 25)
–If pCO2 has not fallen sufficiently, there may be a co-existing respiratory acidosis
differentiate between High Anion gap and low AG
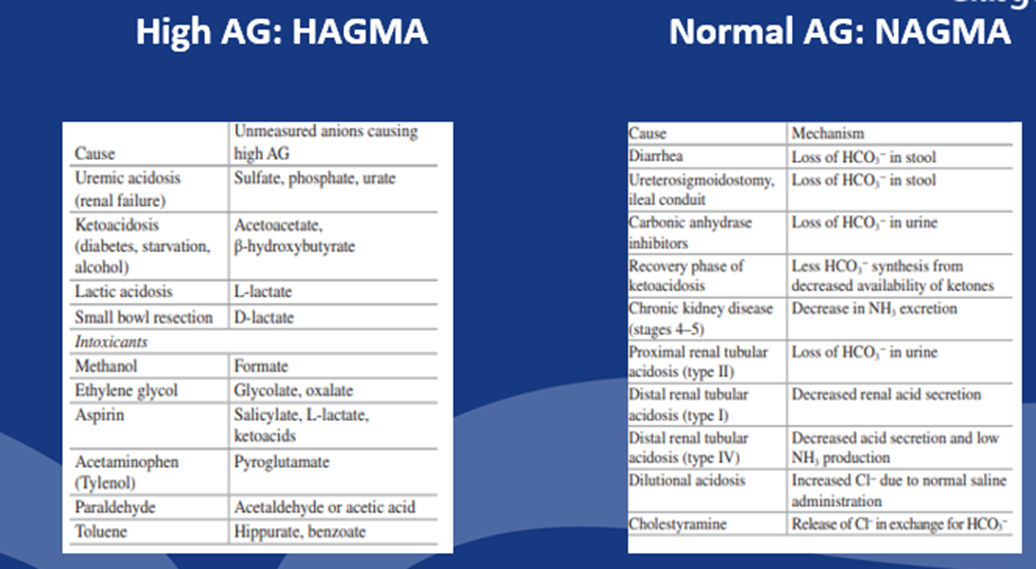

outline the causes of High Anion Gap
•Glycols
•Oxyproline (pyroglutamic acid)
•L-Lactic
•D-Lactic
•Methanol
•Aspirin
•Renal
•Ketoacids
describe Anion Gap
•Relates to difference between major cation (Na) and major anions – Cl-, HCO3- and reflects presence of unmeasured anions (albumin, organic anions etc)
•[Na+] – {[Cl-] + [HCO3-] = 9-16 mmol/l
•Must remain electroneutral – so if HCO3- ↓ an additional anion must be present – if this is Cl- then anion gap unchanged; if this is not Cl- then anion gap will rise
•Can be classified into high anion gap or normal anion gap
•Main reason to calculate anion gap is to identify likely cause of metabolic acidosis – especially lactic acidosis, or ingestion of acid
normal AG= 8-16
describe Lactic acidosis
•Lactic acid produced through glycolytic metabolism of pyruvate
•Lactic acid is buffered by HCO3 to lactate and then metabolised in liver (and kidney), releasing HCO3,with no net effect on acid/base balance
•Acidosis results either from
–Excessive production e.g from muscle in heavy exercise/convulsions
–Reduced Clearance e..g hypoperfusion and reduced hepatic clearance – major problem in sepsis
•Can occur due to drugs (metformin), liver failure, poisoning (cyanide, aspirin)
•High lactate levels are therefore marker of tissue hypoperfusion and important prognostic marker in Sepsis
explain acidosis of chronic renal failure
•As renal function declines, most patients become acidotic
•Initially this is a normal-AG acidosis due to reduced renal ammonium excretion
•Titratable acid excretion initially preserved due to ↑PO4 excretion and ↓ PO4 reabsorption in PCT
•Eventually patients may develop high AG eg.PO4 (phosphate) and other anions accumulate
explain Pyroglutamic acidosis
•Rare but important to spot
•Due to depletion of Glutathione
–Tripeptide involved in aa transport
•Glutathione def drives production of pyroglutamic acid
•Occurs in sepsis, often malnourished patients, treated with certain Abx, esp flucloxacillin, and paracetamol
•High AG metabolic acidosis, normal lactate
•Diagnose by checking urine organic acids (↑pyroglutamic acid/5-oxoproline)
describe metabolic alkalosis
•Primary abnormality is ¯ H+ and HCO3
•Compensatory response is hypoventilation – thus PCO2
•Main causes are:
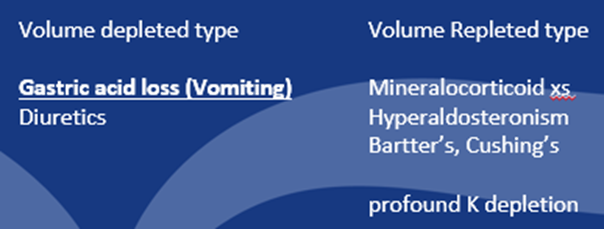
FACTORS CONTRIBUTING to metabolic alkalosis:
•Response to alkalosis should be to excrete HCO3 (equivalent to retaining H+)
•Maintenance of alkalosis due to failure to excrete HCO3
–Occurs as HCO3 is reasorbed with Na, when there is a deficiency of Cl
•Volume depletion
–Na reabsorption drives HCO3 reabsorption (to remain electroneutral). Also promoted by aldosterone
•Chloride depletion
–HCO3 reabsorption in DCT requires Cl secretion – if tubular CL reduced, gradient to reabsorb HCO3
•Potassium depletion
–Not clear why – probably combination factors
–e.g. distal tubule H secretion occurs with K transport in opposite direction – in trying to retain K, H will be excreted leading to alkalosis
•Treatment – fluid resuscitation – 0.9% NaCl (for vomiting), treat cause
what’s the difference in the kidneys compared to the liver in an Ultrasound, in normal and abnormal kidneys?
● Normal – Liver is more ‘echobright’ than kidney
● Abnormal – Kidney more ‘echobright’ than liver – implies pathological change
differentiate between Non-contrast and contrast CT imaging
•Non-contrast imaging:
–Information on renal stones – location +/- type
•Contrast-enhanced imaging:
–IV iodinated contrast
–Information on arteries / veins / perfusion / neighbouring structures / excretion of contrast
–Potentially nephrotoxic
~ weigh up risk v benefit with eGFR <30mL/min
~ risk may be lowered by pre-hydration strategies
define nephrogenic systemic fibrosis
rare, serious, and progressive disorder where skin thickens and hardens, and internal organs can be damaged.
It occurs in people with advanced kidney disease, most often after exposure to certain gadolinium-based contrast agents (GBCAs) used in MRI and MRA scans.
Symptoms include thickening and tightening of the skin, joint contractures, and pain, but the condition can also affect organs like the lungs, heart, and muscles.
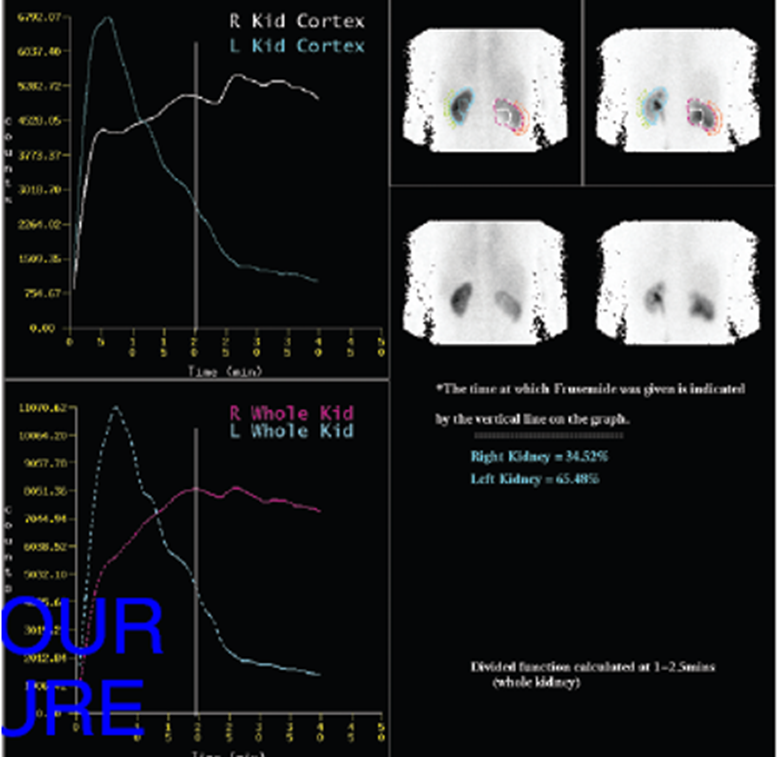
how can Isotope scanning help in kidney transplant?
for living donors, by providing crucial functional information, primarily the split renal function and glomerular filtration rate (GFR) of each individual kidney.
summarise imaging
•Ultrasound is often the first port of call for most things
(anatomical issues/blood flow/obstruction/stones/tumours)
•
•Thereafter:
•
–Plain CT for stones / plain MRI for tumours (detailed evaluation)
–Contrast CT / contrast MR for angiography (consideration where eGFR<30).
–Weigh up risks/benefits of contrast-exposures in patients with poor renal function, and mitigate risks through local protocols.
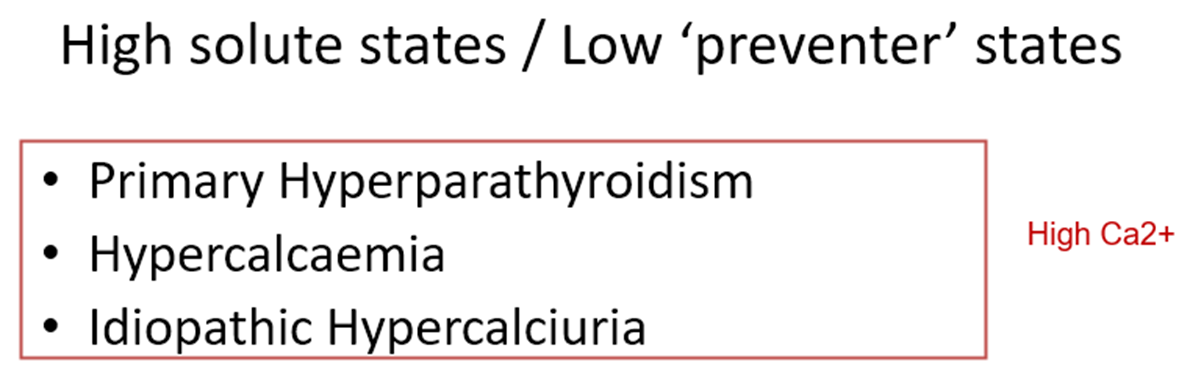
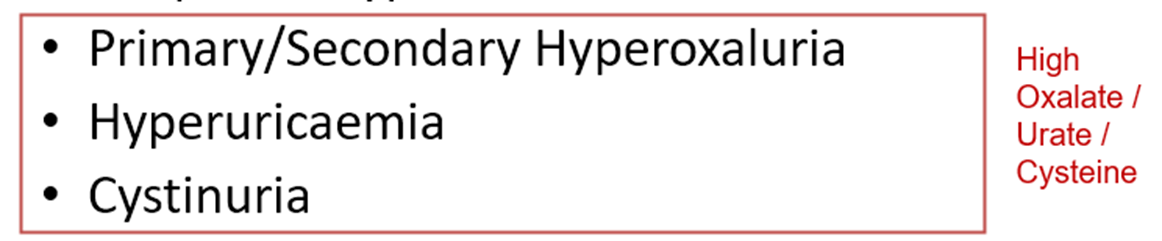
define kidney stones and outline why they are formed?
•Kidney stone = renal calculus = nephrolithiasis
•A solid concretion of crystal aggregate formed within the urinary space.A lot of solute…
- Calcium
- Oxalate
- Urate
- Cysteine
…not enough solution.
- Filtrate / urine
what are the renal stones classifications?
•By location:
- Kidney / nephrolithiasis
- Ureter / ureterolithiasis
- Bladder / cystolithiasis
•By composition:
- calcium-phosphate / calcium oxalate
- urate / cysteine / struvite etc.
what are the risk factors for kidney stones?
•Genetic factors:
- 50% have genetic component
- Positive family history = RR 2.5
•Environmental factors – (EPIC data n=65,000 UK):
- BMI >27 (RR 2.0) / immobile or sedentary / dehydration / UTI
(protective factors)
- Vegetarian (RR 0.5)
- High fruit (RR 0.6)
- High fibre (RR 0.6)
•Rise in obesity + metabolic syndrome (DM / HBP) have caused an increase in uric acid stones.
outline the composition of renal stones
•Calcium containing (80%)
–Calcium Oxalate
–Calcium Phosphate
•Magnesium Ammonium Phosphate – Struvite (5-10%)
•Uric Acid (5-10%)
•Cystine (1-2%)
•Mixed Stones
how is a risk of kidney stones evaluated?
•History
–Renal Colic / Passage of stones / Haematuria / Infection
–Family History
–Diet
•Examination
–Flank tenderness / Signs of infection on urinalysis
–Obesity / Hypertension / Gouty tophi / Diabetes Mellitus
•Investigations
–Imaging
•Non-contrast CT
–Cystine – low density
–Magnesium Ammonium Phosphate - low density
–Calcium stones – high density
•Associated with nephrocalcinosis (normally CaPO)
•Calcification at Cortico-medullary Junction- medullary sponge kidney – either CaOx or CaPO
–Serum and Urine Biochemistry
Serum Biochemistry Tests…
•Serum Calcium
•Serum Phosphate
•Serum PTH
•Serum Urate
•Serum Bicarbonate
Urinary Biochemistry Tests…
•Urine Volume
•Urinary pH •(normal range 4.6 to 8.0)
[•May be helpful in guiding diagnosis/treatment
–Calcium stones precipitate pH >7.0
–Struvite stones precipitate pH >7.0
–Uric acid + cystine stones precipitate pH <6.0]
•Urinary
–Calcium
–Sodium
–Oxalate
–Citrate
–Creatinine
–Uric Acid
–Cystine
define and differentiate between Nephrocalcinosis (CaPO deposition) & Medullary Sponge Kidney (CaPO/CaOx)
Nephrocalcinosis (CaPO deposition)= calcium deposits in the microtubules
Medullary Sponge Kidney (CaPO/CaOx)= A congenital disorder of the kidneys characterized by cystic dilatation of the collecting tubules, predisposing to stone formation
explain the treatment for stones in the kidney
< 2 cm – expectant management or offer extracorporeal shock wave lithotripsy (ECWL)
> 2cm or multiple stones – expectant management or percutaneous ultrasonic lithotripsy (pul)
•Large branched stones “staghorn” may require pul and eswl.
•Cystine stones pul or open nephrolithotomy
explain the treatment for stones in the ureter
•Small ureteral stones with good chance of passage (<7 mms)
–allow time to pass (2-4 weeks)
–lower ureter= ureteroscopic stone removal
–mid-upper ureter= eswl (extracorporeal shock wave lithotripsy)
•Large ureteral stones (>7mms)
–eswl
–ureteroscopic stone fragmentation
–open surgery
when would ureteric stenting be used?
–drain obstructed kidney thereby alleviating pain
–dilate ureter perhaps facilitate passage of stone
–facilitate performance of eswl and ureteroscopic procedures
what’s the secondary prevention for the different types of renal stones?
it it’s the first stone or infrequent (ie >10 years) no work up needed.
•Otherwise:
–Monitor stone burden with periodic imaging
–FLUID – aim for >2.0L/24hr
–Stone-type specific advice:
•Calcium phosphate
–Increase fluid
–If HPTH / Sarcoid / RTA (hyperparathyroidism, sarcoidosis, and renal tubular acidosis) type 1 then treat the cause
–Consider citrate, and if hypercalciuric consider a thiazide
•Calcium oxalate
–Increase fluid
–Treat the cause (low oxalate diet)
–Consider citrate, and if hypercalciuric consider a thiazide
•Uric Acid stones
–Increase fluid
–Treat the cause (hyperuricaemia) with xanthine oxidase inhibitors (allopurinol / rasburicase).
–If polycythaemic / tumour then treat the cause
–Alkalinise the urine to target pH >6.0 (bicarb or citrate)
•Cystine stones
–Increased fluid intake – 3-4 L per 24 Hours.
–Treat the cause (cystinuria - reduce protein/sodium diet).
–Alkalinise Urine to target pH > 7.0 (bicarb or citrate)
•Magnesium Ammonium Phosphate (Struvite):
[direct result of urinary tract infections (UTIs) caused by specific urease-producing bacteria]
–Debulk where possible (complete surgical removal)
–Treat the cause (aggressive treatment of UTI)
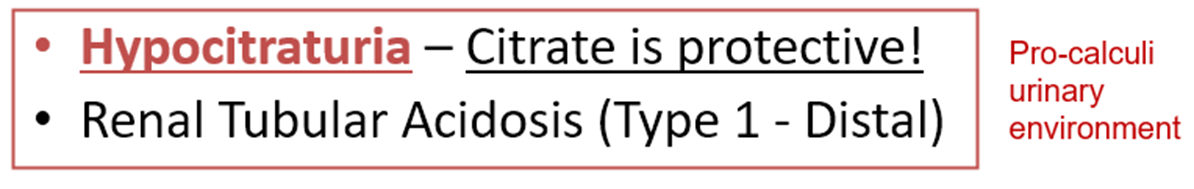
explain why Citrate is beneficial for calcium stones?
•Most important inhibitor of calcium stone formation.
•Can be increased by low Na diet / treatment of acidosis.
•Several mechanisms of action:
–Reduces urinary supersaturation of calcium salts by forming soluble complexes with calcium ions and by inhibiting crystal growth and aggregation.
–Increases the activity of some macromolecules in the urine (eg. Tamm-Horsfall protein) that inhibit CaOx aggregation.
–Alkalinising effect which inhibits urate and cystine stones.