Physiology III - UNIT 1 (Part 2): Detailed Study of Cardiac Muscle and Conduction System
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
What are the 7 features of cardiomyocytes?
1) Striated
2) Short
3) Thick
4) Branched cells
5) One central nucleus surrounded by light-staining mass of glycogen
6) Repair of damage entirely by fibrosis (scarring)
7) Intercalated discs
What are the 3 features of intercalated discs?
1) Interdigitating folds
2) Mechanical junctions
3) Electrical junctions
What feature of the intercalated discs are the plasma membrane folded like the bottom of an egg carton in order to increase surface area and interlock cells?
Interdigitating folds
What feature of the intercalated discs tightly join the cardiomyocytes?
Mechanical junctions
Which of the two types of mechanical junctions are actin of the thin myofilaments that is anchored to the plasma membrane?
Fascia adherens/broad band
Which of the two types of mechanical junctions are mechanical linkages that prevent contracting cardiomyocytes form being pulled apart form each other?
Desmosomes
What feature of the intercalated disk allow ions to flow between cells and can stimulate neighbors so the entire myocardium of either two atria or two ventricles act like a single/unified cell?
Electrical junctions (gap junctions)
Which two features are on the transverse surface of the intercalated disc? Which two are on the longitudinal surface of the intercalated disc?
Transverse = Desmosome & Fascia adherens
Longitudinal = Gap junction
T/F: Cardiac muscle depends almost exclusively on anaerobic respiration to make ATP
FALSE
- almost exclusively on AEROBIC respiration
(rich in myoglobin & glycogen, and HUGE mitochondria)
T/F: Cardiac muscle is fatigue resistance sine it makes little use of anaerobic fermentation or oxygen debt mechanisms.
TRUE
What is the system composed of an internal pacemaker and "nerve-like" conduction pathways through myocardium that coordinates the heartbeat?
Conduction System
What are the 5 main features of the cardiac conductive system in order?
1) SA node
2) AV node
3) AV bundle (Bundle of His)
4) R/L bundle branches
5) Purkinje fibers
Where is the SA node located?
Near base of SVC in the right atrium
What other name is the SA node known as and why?
Pacemaker because it initiates heartbeat (automaticity) which determines heart rate (rhythmicity)
Where is the AV node located?
Near the right atria at lower end of interatrial septum (tricuspid)
What does the SA node signal to depolarize when it fires?
Stimulates atrial cardiomyocytes to depolarize and contraction of both atria
- anterior interatrial myocardial band (Bachmann's bundle) conducts the impulse to the left atrium for the symmetrical contraction of atria
What does the AV node signal to depolarize?
Stimulates ventricular depolarization and contraction of both ventricles
What fibrous skeleton in the AV node prevents what form occuring?
Its an insulator preventing currents from getting to ventricles by any other route
Why does the conduction signal slow down through the AV node?
pauses activity to allow time for ventricles to fill before contraction
What part of the conduction system forks into right and left bundle branches to pass through interventricular septum toward apex?
AV bundle (Bundle of His)
What part of the conduction system are the nerve-like processes spread through ventricular myocardium, where the cardiomyocytes then pass the signal cell to cell through gap juncitons?
Subendocardial conducting network
(Purkinje fibers)
What is the 5 step process of the conduction system?
1) SA node fires
2) Excitation spreads through atrial myocardium
3) AV node fires
4) Excitation spreads down AV bundle
5) Subendocardial conducting network distributes excitation through ventricular myocardium
Sympathetic nerves increase ____ & _____. This is because the fibers terminate in what 3 locations?
Increase Heart Rate & Myocardial contraction
Fibers terminate in:
1) SA nodes
2) AV node
3) atrial and ventricular myocardium
Parasympathetic nerves decrease ______. This is because fibers terminate in what 2 locations?
Decrease Heart Rate
Fibers terminate in:
1) SA node --> Right vagus
2) AV node --> Left vagus
NOTE: NO influence on contractile strength
What does systole mean? Diastole?
Systole = Contraction
Diastole = Relaxation
(when not specified, usually referring to ventricles)
What is the normal heartbeat triggered by the SA node and what is its range?
Sinus Rhythm
(60-100 bpm)
What is the parasympathetic (vagus nerve/CN X) influence on sinus rhythm and what is its range?
Vagal tone
(70-80 bpm)
What are abnormal pacemaker sites outside the SA node that display automaticity?
Ectopic focus
What are some causes of Ectopic focus?
Hypoxia, electrolyte imbalance, stimulants, stress, lack of sleep
-- fire before SA node and set off extra heartbeat (Premature ventricular contraction (PVC))
What is the abnormal heart rhythm that originates from the AV node or bundle of His that may govern heart rhythm if SA node is damaged, and at what rate does it beat?
Junctional/Nodal Rhythm
- (40-50 bpm)
What rhythm is when both the SA and AV nodes are NOT functional and the AV bundle/purkinje fibers are present and firing?
intrinsic ventricular rhythm
If only the Purkinje fibers are present and functioning, what intervention is needed and why?
Need artificial pacemaker
-- 20-40 bpm and too slow to sustain life
T/F: The SA node has a stable resting membrane potential
FALSE
-- easily fires; not stable
(Starts at -60 mV)
What is the 6 step process of the Pacemaker Physiology (SA Node Action Potential)?
1) Starts at -60mV
2) SLOW Na+ inflow will cause gradual depolarization (slight drift upward in +) --> Pacemaker potential
3) When reaches -40mV (threshold), FAST Ca2+ & Na+ channels open
4) Faster depolarization occurs and peaks at 0 mV
5) At 0 mV, K+ channels open and K+ leaves cell (repolarization)
6) Once K+ channels close (@-60mV), pacemaker potential starts over
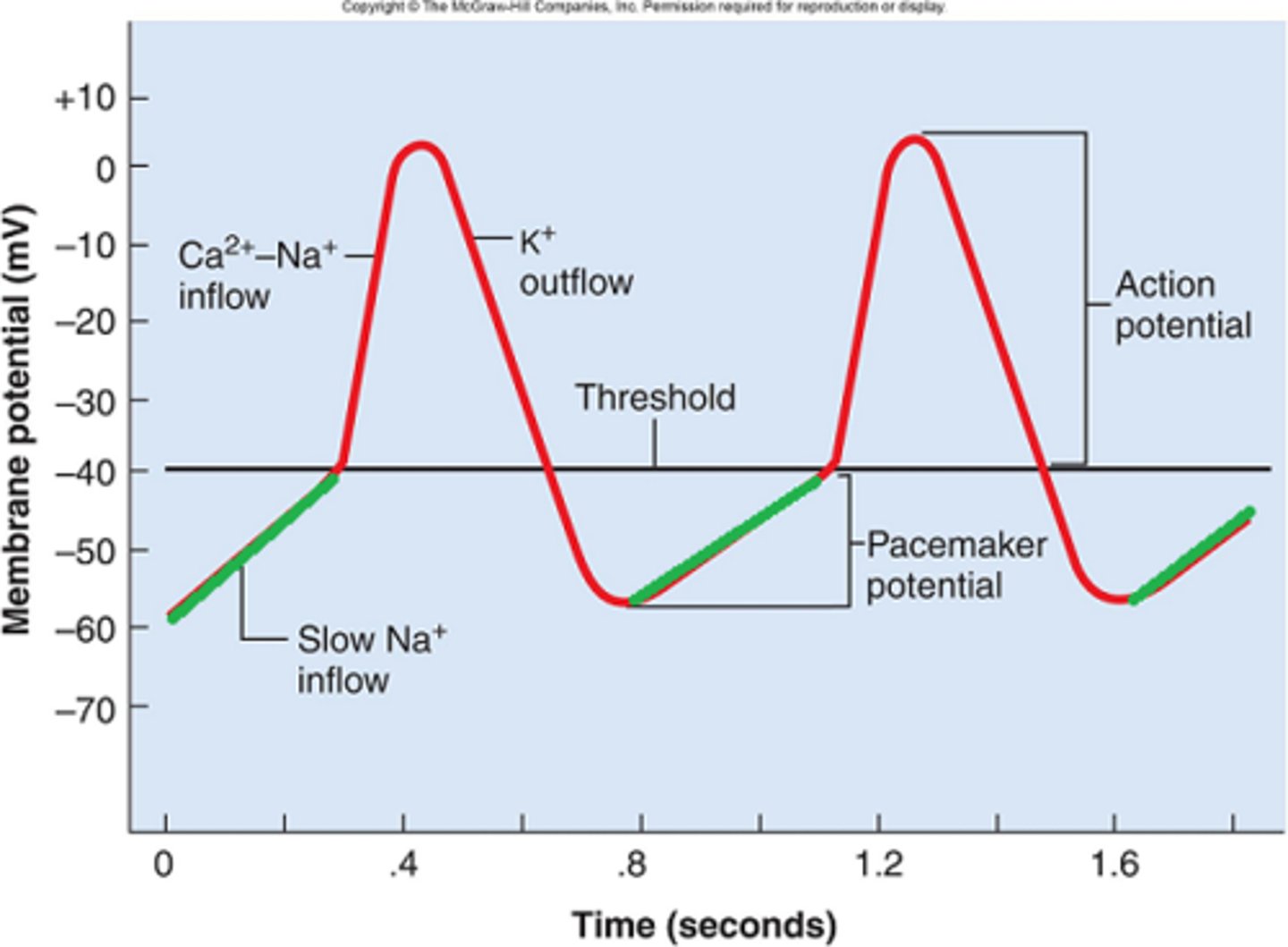
When SA node fires, it sets off heartbeat. As the internal pacemaker, it typically fires every ________ seconds, setting the resting rate at ____ bpm
Fires every 0.8 seconds
-- 75 bpm
In the first part of the impulse conduction order, the signal from SA node (pacemaker) spreads to stimulate the two atria to depolarize almost simultaneously. What is the goal of this signal? How long does it take to reach the AV node?
Goal is for cells to contract!
-- Reaches AV node in 50 ms
In the second part of the impulse conduction order, when the spread of excitation reaches the AV node, the signal slows down through the AV node so the atria can contract. The thin cardiomyocytes with fewer gap junctions allows what important feature to occur?
Delays signal 100 ms which allows ventricles to fill
In the third part of the impulse conduction order, the excitation spreads rapidly throughout the ventricles via the purkinje fibers, causing what to occur?
Entire ventricular myocardium depolarizes and contracts in near unison
In the final part of the impulse conduction order, the ventricular systole progresses up from the apex of the heart so that what can occur?
Spiral arrangement of myocardium twists ventricles slightly
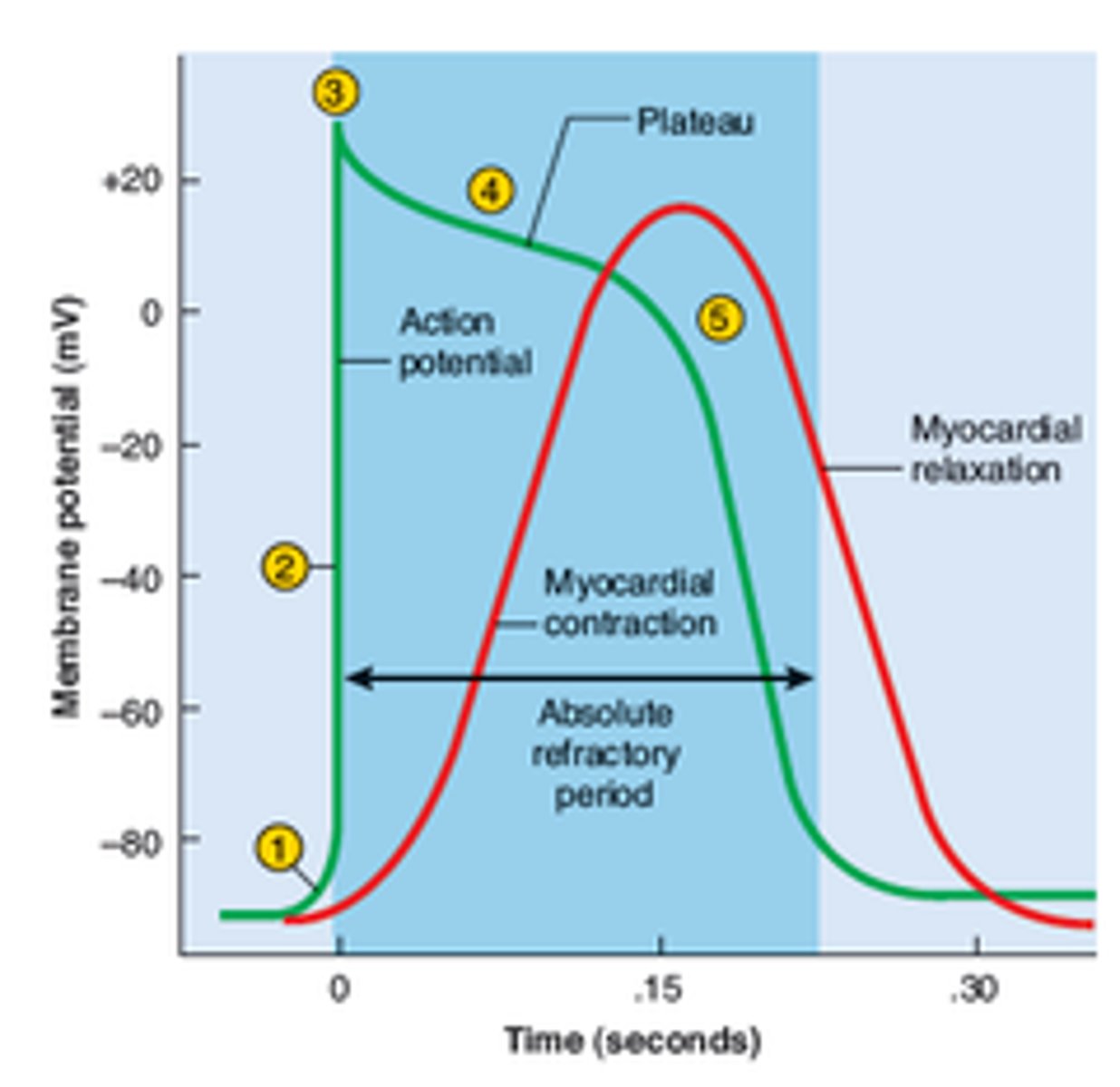
T/F: Cardiomyocytes have a stable resting potential.
TRUE
- depolarize ONLY when stimulated
(Membrane potential = -90 mV)
What are the 3 phases of the cardiomyocyte (atrium & ventricle) action potentials?
1) Depolarization
2) Plateau --> DIFFERENT from SA AP
3) Repolarization
What does the Plateau phase indicate in the cardiomyocyte action potential? How long does it last?
Represents CONTRACTION
--contraction sustained for expulsion of blood from heart for 200-250 ms
Why does the Cardiomyocyte action potential have a long absolute refractory period? How long is it?
Prevents wave summation and tetanus which would stop the pumping action of the heart
-- 250 ms
What are the 6 steps of the Cardiomyocyte action potential?
1) Start at -90 mV
2) Stimulus opens Na+ channels and Na+ rushes in for a RAPID depolarization
3) Action potential peaks at +30 mV and the Na+ gates close quickly
4) SLOW Ca2+ channels open, triggering SR Ca2+ channels to open to bind to troponin and trigger contraction (200-250 ms) & some K+ entering.
5) Ca2+ channels close and K+ channels open RAPIDLY
6) Returns to resting potential (-90 mV) and undergoes an absolute refractory period (250 ms)
What is a composite recording of nodal & myocardial cells electrical activity/current during the cardiac cycle producing a graph in voltage vs time?
ECG/EKG (Electrocardiogram)
-- measures potential difference across surface of myocardium w/ respect to time
T/F: Action potentials initiate contraction which can determine heart rate.
TRUE
What wave is produced on the ECG/EKG when the SA node fires and depolarizes the atria?
P-wave
-- Atrial systole begins 100 ms after SA signal
What is occurring at the P-R segment? Where does this start & end?
The slowing of the action potential through the AV node so the ventricles have time to fill
-- Starts at onset of P wave and ends at onset of QRS complex (time period form start of atrial depolarization to start of ventricular depolarization)
What are the 3 important features that occurs during the P-wave?
1) SA node fires
2) Atrial depolarization (+)
3) Atrial systole (contraction)
T/F: The flat line between the end of the P-wave and the onset of the QRS complex reflects the atrial contraction.
FALSE
-- reflects the slow impulse conduction through the AV node
What is going on int he heart during the QRS complex of the ECG/EKG?
Ventricular depolarization
During what part of the ECG/EKG are the ventricles in systole (contraction)? What part of the myocardial action potential graph does this correspond to?
During ST segment/interval
-- corresponds to the Plateau phase
What occurs in the myocardial cells during the T wave?
Ventricles myocardial cells are repolarizing and ventricles relax
What would the absence of a P wave on the ECG/EKG mean?
Indicates SA node did not fire (SA node block)
-- atria would not depolarize normally and not contract normally
-- P wave absence also seen in atrial fibrillation or atrial flutter
Where is atrial repolarization buried within the ECG?
QRS complex
The Q wave specifically indicates the depolarization of _______, while the S wave indicates the depolarization in the __________.
Q wave = Septum depolarization
S wave = Purkinje fibers
What does the U wave indicate on the ECG?
Purkinje system repolarization
The absence of what on the ECG/EKG would indicate that the SA node did not fire (SA node block), and the atria would not depolarize normally & not contract normally?
Absence of P wave
The absence of what on the ECG/EKG would indicate disruption of ventricular depolarization due to a block somewhere between the AV node and ventricles (second degree AV block)
Absence of QRS complex
What is any abnormal cardiac rhythm or rate due to a failure in the conduction system to transmit signals due to impulse initiation or impulse propagation disturbances
Arrhythmia
What are the 4 main reasons that an Arrhythmia can occur?
1) Myocardial infarction (MI)
2) Abnormalities in conduction pathways
3) Heart enlargement (linked to Afib)
4) Electrolyte and hormone imbalances
What is it called when the electrical signal travels to the ventricular myocardium randomly and the ventricles contract rapidly and in an uncoordinated manner and an inability to pump blood?
Ventricular fibrillation
Ventricular fibrillation is a hallmark of what condition?
MI
-- kills quickly if not stopped
What is a strong electrical shock with intent to depolarize the entire myocardium and resent the heart to sinus rhythm, but is NOT a cure, just allowing time for other corrective action?
Defibrillation
What is it called when there is uncoordinated contraction of the atria due to an electrical conduction or heart tissue issue causing the atria and ventricles to not work together and poor pumping?
Atrial fibrillation
T/F: Atrial fibrillation is more dangerous than ventricular fibrillation
FALSE
- ventricular fibrillation more dangerous; atrial not immediately dangerous
-- may resolve on own, but increased risk of heart attacks, stroke, and blood clots due to blood pooling/thickening
What is the condition in which the atria beat regular but faster and more often than the ventricles? What is the ratio of beats between the atria and ventricles in this condition?
Atrial flutter
- 4 atrial beats per 1 ventricular beat
NOTE: seen most with hypertension and coronary vascular disease
The absence of what on the ECG/EKG can be seen during atrial fibrillation? Too many of what feature on the ECG/EKG can be seen during atrial flutter?
Atrial Fibrillation:
Absence of P wave
Atrial Flutter:
Excessive P waves (too many)
What is the condition in which there is an obstruction/block/delay of the hearts electrical pathway from the atria to the ventricles through the AV node, usually as a result of disease or degeneration? How many degrees of this condition are there?
Heart Blocks
-- First degree, Second degree Type 1, Second degree Type 2, Third degree
Which type of Heart block is when the signal from the Sa node to the AV node is slowed, but all the signal reaches the ventricles? What does this change on the ECG/EKG?
First Degree
- Longer P-R intervals
Which type of Heart block is when none of the electrical signal reaches the ventricles?
Third Degree
Which type of Heart Block is when electrical signals form the SA node to the AV node are slowed more and more until a signal is completely blocked and a beat is missed completely? What does this change on the ECG/EKG?
Second degree type 1
-- prolongation of P-R interval and a dropped QRS complex
Which type of Heart Block is when some of the electrical signal does not reach the ventricles?
Second degree type 2