Leukaemia's, lymphomas and myelomas
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What does AML, ALL, CML, CLL stand for
–Acute myeloid leukaemia (AML)
–Acute lymphoblastic leukaemia (ALL)
–Chronic myeloid leukaemia (CML)
–Chronic lymphoid leukaemia (CLL)
What are two types of lymphoma
–Hodgkins lymphoma
–Non-hodgkins lymphoma
What is Myeloma
•Myeloma – cancer of clonal plasma cells in the bone marrow (B-cells)
What does a mutation in an oncogene cause
Promotes proliferation “gas pedal gets jammed”
What does a mutation in a tumour suppressor gene mean
The proliferation is unchecked and not slowed down or prevented “no brakes in the car”
What is is the difference between incidence vs prevalence
•Incidence = rate of new cases in a given time period, or the number (or %) of the population at risk of developing the condition
Prevalence = number of people with the condition.
What is Leukaemia
•Uncontrolled cell division of WBCs in the bone marrow, causing a raised circulating white cell count and overcrowding of the bone marrow (bone marrow failure).
What is the incidence and mortality of leukaemia
Cancer Research UK Stats:
•In the UK >9,900 people are diagnosed per year (2019).
•Incidence: 16.2:100, 000 (UK, 2019)
•Mortality: 7.6:100 000 (UK, 2019)
What is myelodysplasia
abnormal development of myeloid cells (pre-leukaemia)
What are the 4 main types of myeloproliferative diseases
CML = excess granulocytes
Essential Thrombocytosis = excess platelets
Polycythaemia Vera = excess RBCs
Primary myelofibrosis = replacement of the bone marrow with collagenous connective tissue
What defines acute leukaemia and chronic leukaemia
•Acute leukaemia: >20% blast cells in blood / bone marrow at clinical presentation (little or no maturation), rapid onset.
•Chronic leukaemia: <20% blast cells in blood / bone marrow (many maturing or mature WBCs), slower progression
Describe AML
AML: Leukaemia (uncontrolled growth of the white blood cells); myeloid (of the myeloid cell line); acute (>20% of nucleated cells are blast cells ie early in differentiation). In blood see elevated blast cells (>20% of nucleated cells) and promyelocytes.
Describe CML
CML: Leukaemia (uncontrolled growth of the white blood cells); myeloid (of the myeloid cell line); chronic (later in differentiation, more mature WBCs). In blood see more neutrophils and myelocytes than blast cells and promyelocytes. Problem is a disorder of the pluripotent stem cell (multipotent???), but see increased numbers of more differentiated cells.
Describe ALL
ALL: Leukaemia (uncontrolled growth of the white blood cells); lymphoblastic (of the lymphoid cell line); acute (>20% blast cells ie early in differentiation). In blood see more lymphoblasts (>20%) and prolymphocytes.
Describe CLL
CLL: Leukaemia (uncontrolled growth of the white blood cells); lymphoblastic (of the lymphoid cell line); chronic (later in differentiation, more mature WBCs). In blood 70-99% of WBCs appear as small lymphocytes. Problem is a disorder of the pluripotent stem cell (multipotent???), but results in increased levels of more differentiated cells.
What ages does AMl affect, what is the incidence rate and how is it categorised
•All ages (increased risk with age – median 60y, peak 85+)
•Incidence 4.6:100,000 (UK, 2019, CRUK stats)
•Categorised M0-M7
What are the signs/symptoms of acute myeloid leukaemia
Signs/symptoms:
•Acute, often critically ill
•Malaise, fever, sweats.
•Anaemia – signs & symptoms?
•Neutropenia - Infections
•Thrombocytopenia - Bleeding / DIC
How is acute myeloid leukaemia (AML) diagnosed
Blood tests / bone marrow biopsy:
•Over-production of myeloid blast cells results in over-crowding in bone marrow causing
–>20% WBCS are blast cells in blood film
–High (leukocytosis), low (leukopenia) or normal WBC count
–Often neutropenia (blast cells instead)
–Anaemia (normocytic, normochromic)
–Thrombocytopenia
–Blasts in peripheral blood film
•WBCs are MPO positive
What is the treatment for AML
Chemotherapy via PICC line or port e.g. cytarabine or stem cell transplant
What is a PICC line
PICC line = peripherally inserted central catheter (long thin tube usually into the arm veins with tip near the right atrium). Usually used over weeks.
What is a port in terms of chemotherapy
Port = a 2.5-4cm disc with a small reservoir (port) attached to it, that sits under the skin of the chest or arm, with a soft tube going from the port and the other end of the tube tip near the right atrium. Used for longer term delivery of IV meds (months to years).
What are some side effects of chemotherapy
Reduces haematopoiesis, possibly causing anaemia (S&S such as fatigue), neutropenia (risk of infections), thrombocytopenia (risk of bleeding).
Reduces turnover of cells lining the mouth and gut possibly causing risk of mouth ulcers, S&S of upset gut (nausea, sickness, diarrhoea).
Reduces cell division in the hair follicle possibly causing hair loss.
High doses can result in infertility.
What is the prognosis acute myeloid leukaemia
•Chemotherapy leads to complete remission (<5% blast cells in bone marrow) rates of 80-90% in younger patients, but cure rates lower, ~45%.
•Older patients tolerate chemotherapy less well, cure rarely achievable (5y survival rate ~15%).
What does ALL affect, what is it’s peak age, incidence and categorised
Uncontrolled proliferation of lymphoid stem cell resulting in large numbers of abnormal lymphoblasts in the bone marrow.
•Peak rate 0-4 years
•80% of childhood leukaemias
•Incidence 1.1:100,000 (UK, 2019, CRUK stats)
•85% B-cell, 15% T-cell
•Categorised L1 – L3
What are the signs and symptoms of acute lymphoblastic leukaemia (ALL)
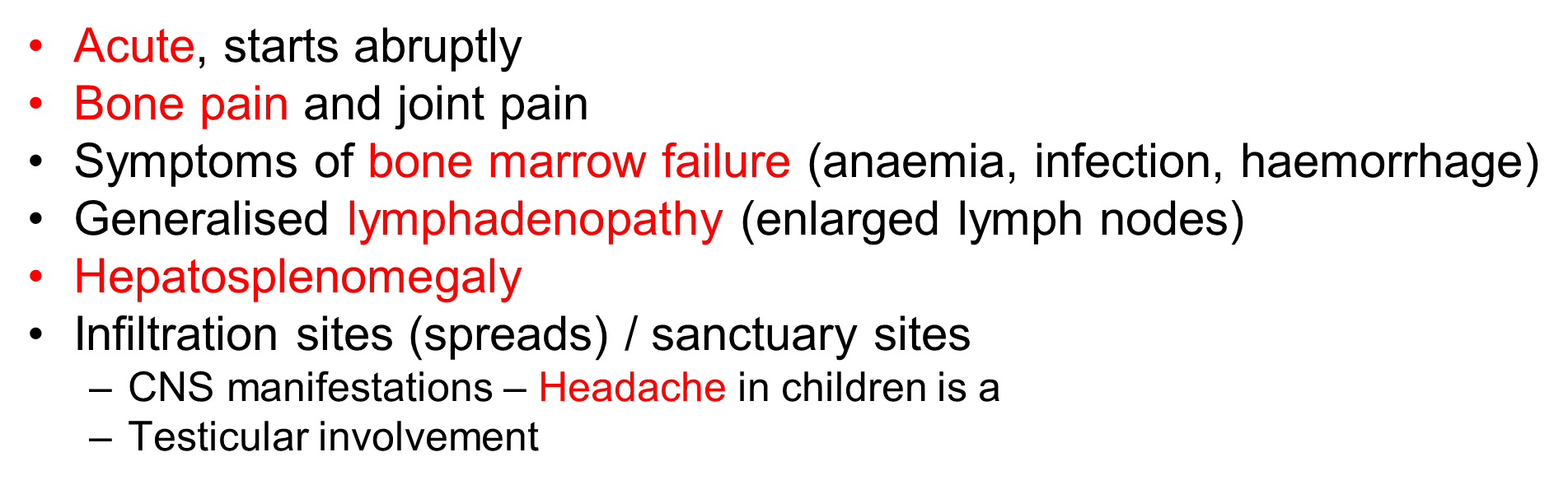
How is ALL diagnosed
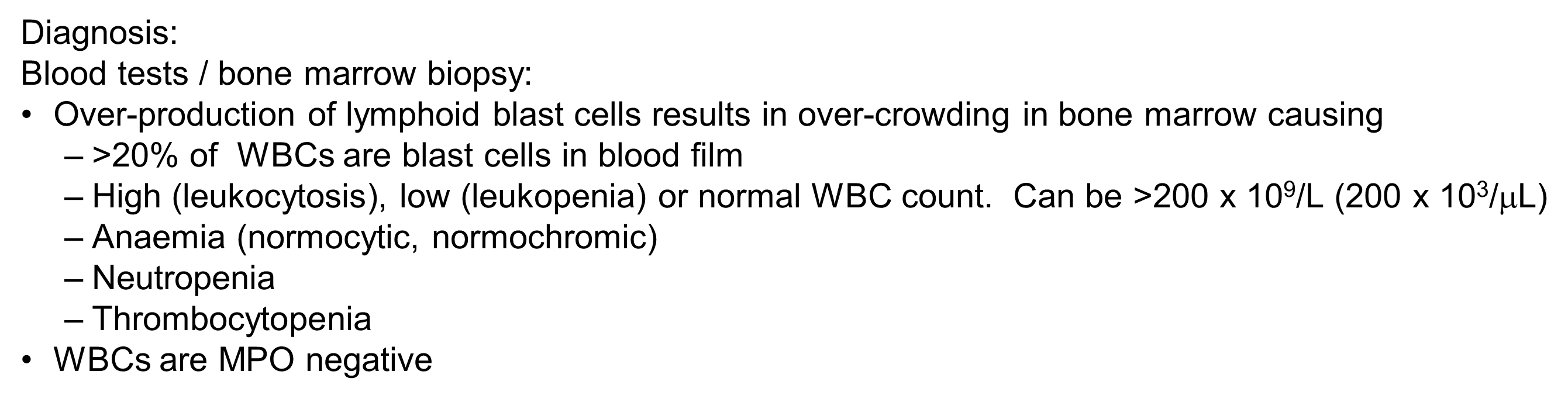
What are the ALL
What is the prognosis of ALL
Prognosis:
•Majority of children (90%) are curable with standard chemotherapy and CNS prophylaxis.
•Trials exploring new immunotherapies for resistant ALL.
•Cure in adults less frequent. Stem cell transplant may be considered. ~35% 5y survival (adults)
Describe CML and it’s peak onset and incidence
Uncontrolled proliferation of myeloid stem cell resulting in large numbers of circulating leukocytes, particularly neutrophils
•Peak onset 65-85 years.
•Males > females
•Incidence 1.3:100 000 (UK, 2019, CRUK)
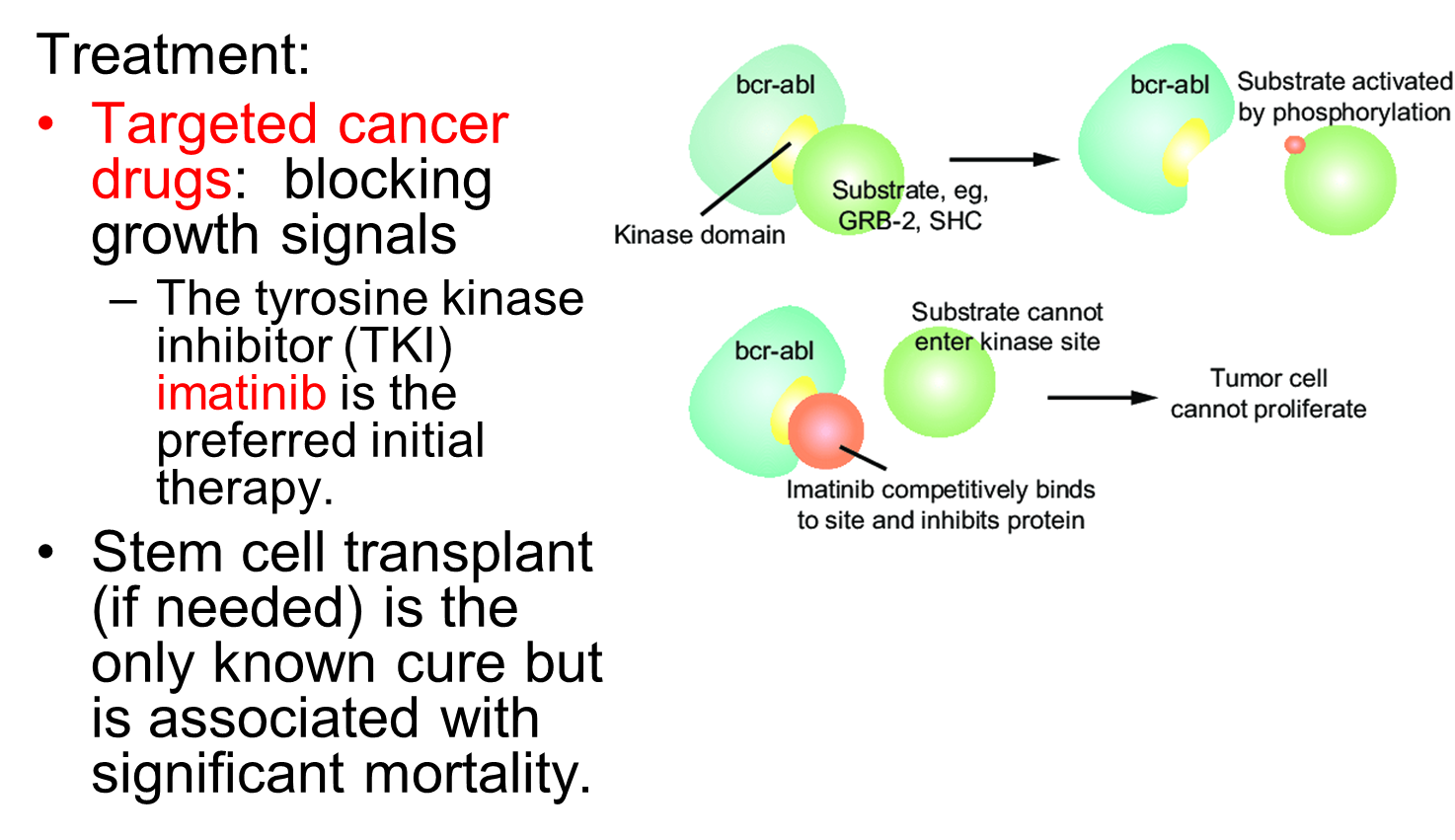
What is consistently associated with presence of a Philadelphia chromosome
CML linked to Philadelphia Chromosome in 90% of cases, but ALL also linked to Philadelphia Chromosome in 15-30% cases.
ABL gene (a tyrosine kinase that is very active) translocates from chr 9 to fuse with the breakpoint cluster region (BCR) gene on chr 22. This increases the production and activity of the tyrosine kinase.
What are the signs/symptoms chronic phase of CML
•Chronic phase: Typically, asymptomatic for 4-5 years, but 90% cases diagnosed from incidental blood test findings.
What are the signs/symptoms accelerated phase
•Accelerated phase: Onset of symptoms, and ↑ in blast cells.
–Fatigue, weight loss, night sweats.
–Splenomegaly – sensation of fullness, hepatomegaly
–Gout, bruising.
–Leukostasis (clumping of leukocytes is often seen in leukaemia)
What are signs/symptoms of blast/acute phase
•Blast / acute phase: ↑ in blast cells and leukaemia transforms from CML to AML.
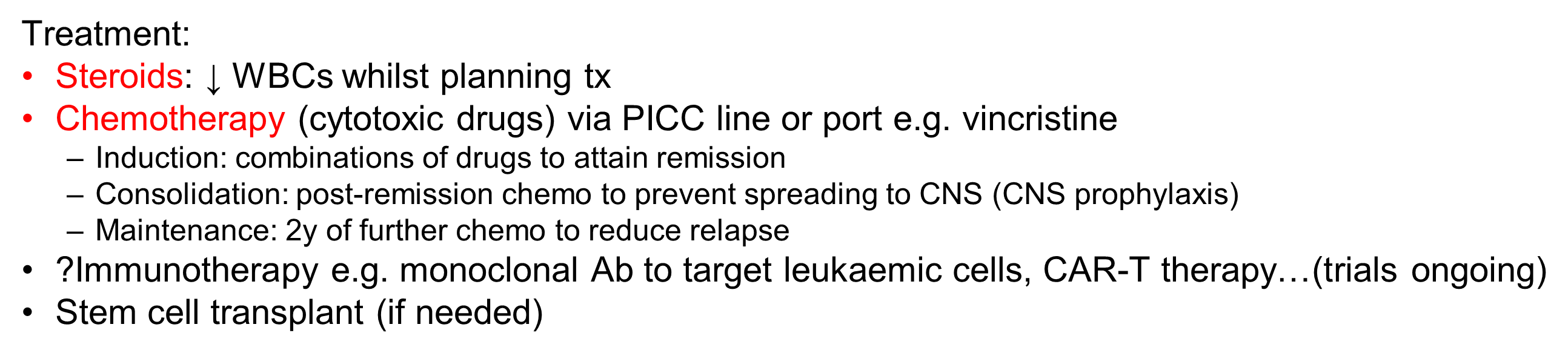
How is chronic myeloid leukaemia (CML) diagnosed
How is CML treated
What is the prognosis for CML
•TKI’s (imatinib) improved 5y survival from 33% to >90%, and 10y survival to 84% - many people reach near-normal life expectancy.
•Indolent (slothful) chronic phase, followed by period of acceleration and a final, generally fatal, acute leukaemic phase (CML→AML).
What is the only known cure for CML
•Stem cell transplant is the only known cure but is associated with significant mortality (rarely used for CML).
What is CLL and what’s the peak onset and incidence
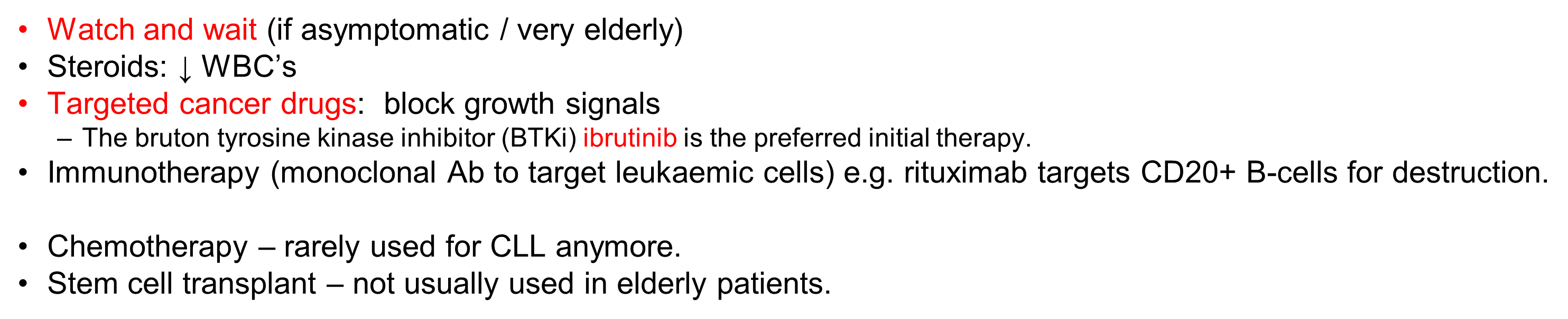
Uncontrolled clonal proliferation of B-lymphocytes.
•Disease of the elderly (typically >50 years, peak 90y+).
•Males > females
•Incidence 6.3:100 000 (UK, 2019, CRUK) (? Commonest leukaemia in Western World)
•Almost all are B-cells
•Considerable overlap with the lymphomas.
What are the signs and symptoms of CLL
•Indolent (slothful) - often asymptomatic (diagnosed from incidental blood test findings). Many Pts survive long periods with minimal symptoms - Elderly pts more likely to die from other causes.
•Symmetrical and painless enlargement of lymph nodes is most common clinical sign
•May have symptoms of anaemia.
•Immuno-suppression resulting in bacterial infections in early stages and viral/fungal infections later.
•Weight loss
How is CLL diagnosed
What is the treatment for CLL
What is the prognosis for CLL
Prognosis:
•~70% 5y survival (NB. Elderly pts)
•Initially indolent, patients often die of other causes.
•Becomes more aggressive in advanced stages.
What is lymphoma
•Cancer of lymphoid tissue.
•Lymphoid tissue
–Lymph nodes, tonsils, adenoids, spleen, thymus
•Results in swollen lymphoid tissue (e.g. lymph nodes) filled with T or B-cells.
What is the breakdown between Hodgkin’s and non hodgkin’s lymphoma
•40% Hodgkin's lymphoma
–Giant malignant B-cells called Reed-Sternberg cells visible
•60% non-Hodgkin’s lymphoma
–Malignant T or B cells, but no Reed-Sternberg cells
•Biopsy node and stain for lymphocytes.
What is Hodgkin’s lymphoma
Malignant B-cells that accumulate in the lymph nodes, however the malignant cells (Reed-Sternberg cells) form only a minority of the tumour, the majority comprising inflammatory cells.
What are the peak ages for Hodgkin’s lymphoma and incidence rate
2 peak ages: 15-35 years and over 50 years
Incidence 3.3:100 000 (UK, 2019, CRUK)
Males > females
What are the signs and symptoms of Hodgkin’s Lymphoma
How is Hodgkin’s lymphoma diagnosed
Diagnosis:
•FBC to exclude leukaemia / mononucleosis
•Normochromic, normocytic anaemia is most common. Bone marrow involvement is unusual in early disease.
•Eosinophilia (high eosinophil count), neutrophilia.
•Normal or increased platelet count in early disease.
•Advanced disease – lymphopenia, thrombocytopenia.
•Lymph node biopsy to diagnose
–CD15 is a marker of Reed-Sternberg cells so can help in differentiating Hodgkin’s vs Non-Hodgkin’s
•PET-CT scan – used for staging / monitoring Hodgkin’s (4 stages of Hodgkin’s)
How is Hodgkin’s Lymphoma treated
What is the prognosis of Hodgkin’s Lymphoma
What is non-Hodgkin’s Lymphoma
Large group of lymphoid tumours (B-cell most common) with more variable presentation and history than Hodgkin’s lymphoma.
•11th most common cancer in the UK.
•Incidence 21.5:100 000 (UK, 2019, CRUK) - Highest incidence of all the haematological cancers.
•Increased risk with age, typically >45y, peak 70-85y.
What are the signs and symptoms of non-hodgkins lymphoma
Signs/symptoms:
•Asymmetrical painless lymphadenopathy (swollen lymph nodes).
•Less fever, night sweats and weight loss than with Hodgkin’s.
•Sore throat (oropharyngeal involvement).
•Acute abdominal symptoms due to spleen / liver enlargement and involvement of GI tract.
•Unexplained itching.
•Symptoms of anaemia, thrombocytopenia or neutropenia with infections.
How is Non-Hodgkin’s Lymphoma diagnosed
•Normocytic, normochromic anaemia, but maybe autoimmune haemolytic anaemia.
•In advanced disease with marrow involvement get neutropenia, thrombocytopenia.
•Lymph node biopsy – no Reed-Sternberg cells.
•Cytogenetics (chromosome mapping).
•Various scans / -oscopy’s to assess different locations of lesions.
•PET-CT scan – used for staging / monitoring Non-Hodgkin’s (4 stages like Hodgkin’s)
How is Non-Hodgkin’s Lymphoma Treated
Treatment (varies with type):
•Steroids: ↓ WBC’s
•Chemotherapy:
–Varies with type of NHL e.g. CHOP combo
•Immunotherapy (monoclonal Ab to target leukaemic cells) e.g. rituximab targets CD20+ B-cells for destruction.
•Radiotherapy: sometimes daily tx with radiotherapy for several weeks with high energy x-rays targeted at the lymphoid tissue – mask / tattoo
•Targeted cancer drugs
Stem cell transplant
What is the prognosis of Non-Hodgkin’s Lymphoma
Prognosis
•55% 10-year survival rate
•Depends on type of NHL
–Indolent (slothful) NHL responds well to chemotherapy, but cure is elusive.
–Aggressive NHL may be cured with chemotherapy combined with rituximab.
•Stem cell transplants are increasingly used.
What is multiple myeloma
Cancer of clonal plasma cells in the bone marrow (B-cells).
•Ab secreting B-cells that secrete a single homogeneous Ig called a paraprotein (detectable in serum and/or urine).
What are the ages and incidence of multiple myeloma
Rare before 40 years, peak 70-89 years
Incidence 9.9:100 000 (UK, 2019, CRUK)
Males > females
African Americans > Caucasian
What are the signs and symptoms of multiple myeloma
Signs/symptoms:
•Bone pain, fractures most common presenting symptom
•Symptoms of anaemia and thrombocytopenia and leukopenia
•Symptoms of hypercalcaemia
•Renal failure – hypercalcaemia / amyloidosis (deposition of abnormally folded proteins)
What is done to diagnose multiple myeloma
What is the treatment and management of multiple myeloma
What is the prognosis for multiple myeloma
Prognosis
•29% 10-year survival (better for younger, worse for older patients)
•Incurable disease, chronic relapsing and remitting pattern. Treatment aims to control rather than cure it, maximising quality of life.
•
Good palliative care (pain relief) crucial