1 Physiology of gaseous exchange and mechanisms of ventilation
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
Which muscles are active during inspiration?
Diaphragm
External intercostals
Accessory muscles:
Scalenes
Sternocleidomastoids
Contraction increases thoracic capacity
What happens during normal expiration?
Relaxation of inspiratory muscles
Decreases thoracic capacity
Due to elastic recoil of the lungs
Which muscles are active during forced expiration?
Abdominal muscles:
Internal & external oblique
Rectus abdominis
Transversus abdominis
Internal intercostals
Some muscles of the back and neck
Contraction further decreases thoracic capacity
What happens at the end of quiet expiration? respitory cycle 1
Respiratory muscles are at rest
Balance between:
Elastic recoil of the lungs (forces of collapse)
Elastic recoil of the chest wall (forces of expansion)
Thoracic cavity is at equilibrium
What happens during inspiration? 2 respitory cycle
Contraction of inspiratory muscles
↑ Thoracic volume
↓ Intrapleural pressure
↑ Lung volume
↓ Alveolar pressure
Air moves into the lungs
What happens during expiration? respitory cycle 3
ck:
Relaxation of inspiratory muscles
↓ Thoracic volume
↑ Intrapleural pressure
↓ Lung volume
↑ Alveolar pressure
Air moves out of the lungs to functional residual capacity
What happens during forced expiration? 4th resipitory cycle
Back:
Contraction of expiratory muscles
↓ Thoracic volume
↑ Intrapleural pressure
↓ Lung volume
↑ Alveolar pressure
Air moves out of the lungs below functional residual capacity
What are the two opposing forces involved in breathing?
Lung elasticity → wants to collapse the lungs
Rib cage anatomy → wants to expand the lungs
What happens at the end of normal expiration? (forces )
The two forces (lung collapse vs rib expansion) are balanced
Negative pressure in pleural cavity holds lungs open
What happens during inspiration?(forces)
Active process driven by the brain
Rib cage expands
↑ Negative intrapleural pressure → pulls lungs open
↓ Alveolar pressure → air flows into lungs
What happens during normal expiration?
Passive process due to lung elastic recoil
Inspiratory muscles relax
Lungs recoil inward
Creates positive pressure → air flows out of lungs
What does lung compliance mean?
How easily the lungs expand
High compliance → lungs stretch easily
Low compliance → lungs are stiff, harder to inflate
What keeps the lungs and chest wall “adhered” to each other?
Negative pressure in the pleural cavity
Acts like a vacuum between lungs and chest wall
Allows lungs to follow chest movements during breathing
What is intrapleural pressure approximately equal to?
Intrapleural pressure ≈ intrathoracic pressure
Does intrapleural pressure remain constant?
No, it is not constant
Changes during the respiratory cycle
What is the pleural cavity and what does it contain?
A virtual space between the two pleural membranes
Contains a thin layer of fluid acts as a lubricant for smooth lung movement
How does surface tension affect the pleural membranes and lung expansion?
Surface tension “holds” the parietal and visceral pleura together
When the chest expands, the parietal pleura moves outward
Due to surface tension, the visceral pleura follows the parietal pleura
This pulls the lung tissue, causing the lungs to expand
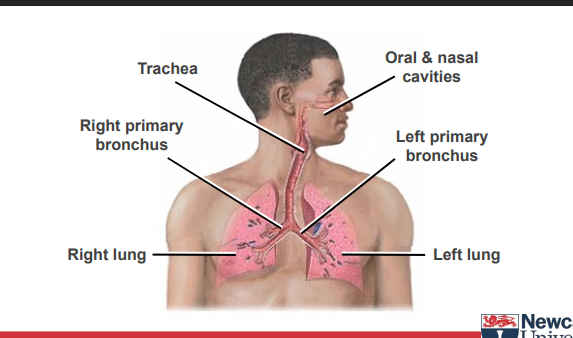
What are the two main types of airways?
Conducting airways: no gas exchange (“dead space”)
Respiratory airways: site of gas exchange
What structures make up the conducting airways?
Trachea and bronchi: cartilage + smooth muscle
Bronchioles: no cartilage, more smooth muscle (main site of obstruction in asthma)
What structures are involved in respiratory airways?
Respiratory bronchioles
Alveoli (major site of gas exchange)
What is the primary function of the airways?
Deliver O₂ to the blood and remove CO₂
Help maintain body pH by regulating arterial CO₂ (pCO₂)
Why do airways need defense systems?
Airway is an opening into the body
Must prevent harmful particles from entering the lungs
How do airways defend against particles?
Warm and humidify inspired air
Prevent particle entry
Remove or neutralize particles that enter
Mucociliary system and cough
Phagocytic cells
Inflammatory and immunologic responses
What are some other functions of the airways?
Metabolic functions
Vocalization
Olfaction (sense of smell)
What is an important structural feature of bronchioles?
No cartilage, so they can collapse
More smooth muscle than larger airways
How do bronchioles behave during breathing?
Inspiration: lungs expand → bronchioles pulled open
Expiration: bronchioles get smaller
At low lung volumes, bronchioles can close and trap gas
Why is bronchiole collapse clinically important?
Volume at which they collapse increases in lung diseases
Major site of smooth muscle contraction and obstruction in asthma
How close are alveoli to pulmonary capillaries?
Air and blood are very close (~5 µm)
Facilitates efficient gas exchange
What are the layers between alveolar air and blood?
Alveolar epithelium
Basement membrane
Interstitium (thin)
Basement membrane
Capillary endothelium
What are the main types of alveolar cells and their functions?
Type I cells: flat, primary lining, cover 95% of surface
Type II cells: tall/granular, 60% of cells cover 5% of surface, produce surfactant
What provides elasticity in alveoli?
Elastic fibers in interstitium
Produced by fibroblasts → allow lung recoil and expansion
What is the role of alveolar macrophages?
Scavenge particles
Remove excess surfactant
Are alveoli individual isolated sacs?
No, they form an interconnected honeycomb of cavities
Connected by shared interconnecting walls
How is mechanical stress transmitted in alveoli?
Stress on one alveolus is transmitted to neighboring alveoli
Interconnected walls allow stress to be shared across lung parenchyma
How does alveolar interconnection contribute to lung function?
Contributes to elastic recoil during lung distension
Helps resist collapse of individual alveoli (prevents atelectasis)