Egans CH 37 Exam 1 Mechanical Ventilation
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
139 Terms
Intubation
Process of placing an artificial airway into the trachea.
Endotracheal tube (ETT)
Artificial airway tube inserted through mouth or nose into the trachea.
Orotracheal intubation
Endotracheal tube passed through the mouth on its way into the trachea.
Nasotracheal intubation
Endotracheal tube passed through the nose first.
Artificial airway
Airways placed to maintain ventilation; through mouth/nose (ETT) or through the neck (tracheostomy tubes).
Pharyngeal airway
Airway device that extends only into the pharynx.
Nasopharyngeal airway (NPA) and how to place
Nasal airway to facilitate frequent nasotracheal suctioning; minimizes nasal mucosa damage; size is nose to tip of ear lobe, NPA diameter is smaller than pts nares; bevel toward septum; lubricated; flange rests at nostril.
Oropharyngeal airway (OPA)
Oral airway used in unconscious patients to maintain patient airway by preventing tongue obstruction and may serve as a bite block for pts w/ oral tubes.
How to place an OPA
OPA sized by measuring from center of mouth to angle of jaw, or corner of the mouth to earlobe; place oral airway in mouth w/ curved end towards roof or side of mouth, when inserting device and approaches posterior pharynx rotate device 180 degrees into correct position.
Laryngeal mask airway (LMA)
Supraglottic airway for quick, temporary ventilation in difficult to intubate patients or short surgeries.
i-gel
Brand of supraglottic airway (gel-like) used as an alternative to LMA.
Double-lumen endotracheal tube
ETT with two channels enabling independent lung ventilation.
Combitube
Esophageal–tracheal tube used for difficult intubations or when ventilation or intubation cannot be achieved.
Esophageal–tracheal Combitube
A Combitube designed to function in both esophagus and trachea for airway management in difficult cases.
Mac blade
Curved laryngoscope blade commonly used in adults.
Miller blade
Straight laryngoscope blade used for infants/children.
Magill curve
Curvature used in airway instrumentation (Magill curve radius referenced in equipment).
Bevel
Slanted, angled tip of an endotracheal tube.
Murphy Eye
Side hole near the distal end of an endotracheal tube.
Pilot balloon
Inflation/deflation balloon for the ETT cuff.
Cuff
Inflatable ring on the ETT that seals the airway when inflated.
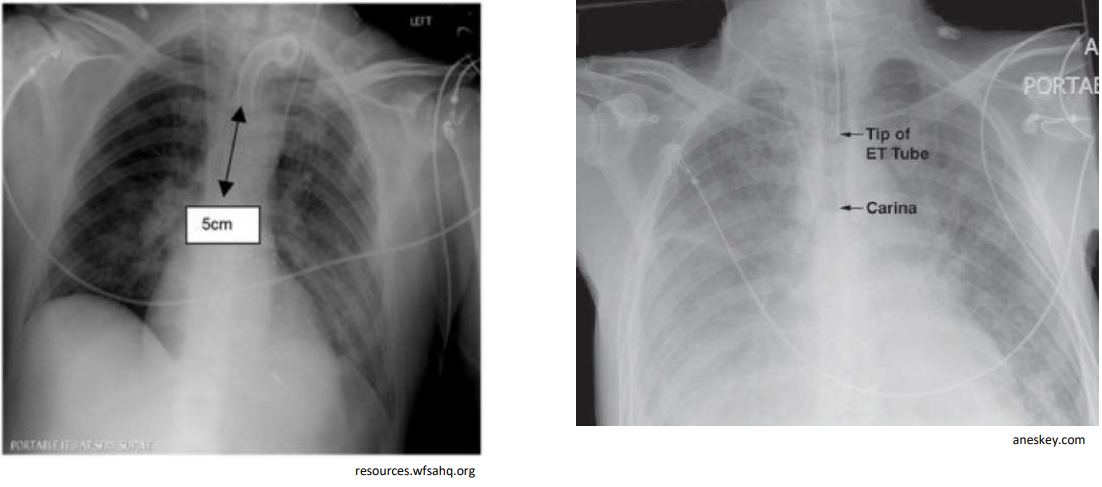
Carina
Bifurcation of the trachea into the left and right main bronchi; ETT tip should be 3–5 cm above it.
Glottis
Opening between the vocal cords.
Vocal cords
Vocal folds within the larynx; visualized during intubation.
Epiglottis
Flap that covers the glottis; displaced during laryngoscopy to visualize the airway.
Vallecula
Anatomical space used as a landmark where the laryngoscope tip is placed to visualize the glottis.
Capnography
Real-time CO2 waveform used to confirm ventilation and correct tube placement.
Capnometry
Measurement of the concentration of CO2 in exhaled air.
End-tidal CO2
CO2 level at the end of expiration; used to verify ventilation and tube position.
CO2 detector / colorimetric
Color-changing device that indicates the presence of CO2 and helps confirm ETT placement.
Securement device
Device or method (e.g., adhesive tape) used to fix the ETT in place.
Extubation
Process of removing an endotracheal tube.
Nasal cannula
Oxygen delivery device inserted into the nostrils.
Pre-oxygenation
Preoxygenating the patient with high FiO2 before induction to extend safe apnea time.
Laryngoscope
Instrument with blades (Mac or Miller) used to visualize the larynx during intubation.
Pre-oxygenate and ventilate
Preoxygenate the patient and ventilate prior to laryngoscopy to optimize oxygenation.
Steps to intubation
Assemble & check equipment
Position pt.
Pre-oxygenate & ventilate pt.
Insert laryngoscope
Visualize glottis
Displace epiglottis
Insert tube
Assess tube position
Stabilize tube/confirm placement (Listen for equal & bilateral breath sounds as pt. ventilated)
Secure ETT
Steps of extubation
Assemble needed equipment
Suction ETT tube nad pharynx above cuff
Oxygenate pt.
Remove securement device
Deflat cuff
Remove tube
Apply appropriate O2 & humidity therapy (O2 w/ cool mist)
Assess/reassess pt. (check for good air movment via auscultation, check for stridor, check pts. skin color, check pts. SpO2)
Describe unplanned extubation
Assess pt. readiness for extubation, OG problem no longer present, quantity & thickness of secretions, upper airway patency, presence of intact gag reflex, ability to clear airway secretions
Equipment for intubation
ETT (stylet, 10 mL syringe, securement device), check cuff is not broken, place stylet inside ETT & full 10 mL syringe on pilot balloon
Bag/mask w/ O2 source
Laryngoscope (Mac for adults, Miller for infants/children)
Suction on & working
CO2 detector or capnography
Vent for after intubation
Sometimes OP airway & bougie
Equipment for extubation
Nasal Cannula
O2 source
Towel
Pulse ox & HR monitor
Suction inline & yankauer
Ambu-bag/mask
Re-intubation supplies on standby if previously diff. intubation
Racemic epinephrine, if known hx of laryngeal spasm (w/ nebulizer)
Suctioning
Application of negative pressure to airways through a collecting tube.
Upper airway suctioning
Suctioning of the oropharynx (upper airway).
Lower airway suctioning
Suctioning of the trachea and bronchi (airways below the larynx).
Tracheal suctioning through the mouth
Suctioning into the trachea via the mouth; should be avoided due to gagging/reflex irritation.
Coude tip catheter
Suction catheter with a bent tip to facilitate entry, and suction left mainstem bronchus.
Open endotracheal suctioning
Sterile technique with disconnection from the ventilator; one-time-use catheter, must maintain sterile technique.
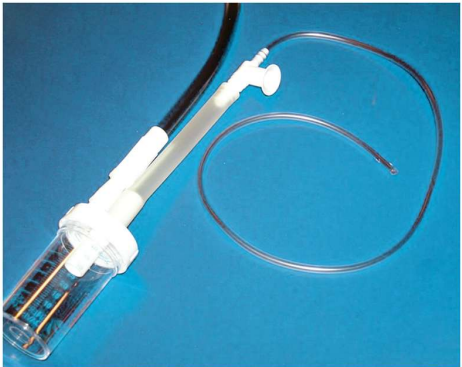
Closed endotracheal suctioning
Sterile, closed, in-line suction catheter attached to the ventilator circuit; allows reuse and no disconnection from ventilator and therefore O2.
In-line suction catheter
A suction catheter designed to stay in the circuit during suctioning.
Ballard suction catheter
A commonly used closed suction catheter platform.
What is step 1 of Endotracheal Suctioning?
Check the patient for indications for suctioning
When the patient cannot clear secretions (e.g., unconscious, sedated, paralyzed, intubated, trach); indicated by poor airway clearance and abnormal breath sounds.
Relative contraindication for endotracheal suctioning?
High intracranial pressure
There are no absolute contraindications; high ICP is a relative consideration.
Abnormal breath sounds indicating suction
Coarse crackles, rhonchi, or crackles suggesting need for suctioning.
Cough reflex as indicator
A need for suctioning is suggested when the patient should cough but cannot.
What is step 2 of Endotracheal Suctioning?
Assemble and check equipment
Catheter size formula (ID × 3)/2
Estimate proper suction catheter size in French; choose size equal to or smaller than (ID × 3)/2.
Example: 8.0 ETT → 12 Fr catheter
For ID 8.0, catheter size = (8 × 3)/2 = 12 Fr.
What is step 3 of Endotracheal Suctioning?
Hyperoxygenation
Give 100% oxygen before suctioning (30–60 seconds; neonates get 10% more).
Total suction time
Keep suctioning passage time to less than 15 seconds per pass.
Suction pressures (adult)
120–150 mm Hg for adults.
Suction pressures (child)
100–120 mm Hg for children.
Suction pressures (infant)
80–100 mm Hg for infants.
What is step 4 of Endotracheal Suctioning?
Insert catheter
Introduce the suction catheter into the endotracheal tube as part of the procedure.
What is step 5 of Endotracheal Suctioning?
Apply suction / clear catheter
Activate suction while withdrawing to collect secretions; clear catheter as needed.
<15 seconds total suction time
What is step 6 of Endotracheal Suctioning?
Re-oxygenation after the suctioning episode.
What is step 7 of Endotracheal Suctioning?
Monitor patient and assess outcomes
Repeat steps (3–7) as needed.
Tracheostomy suctioning
Similar to endotracheal suctioning but with a shorter, sometimes deeper, catheter; avoid deep suction with an open catheter use the tip of the tracheostomy tube.
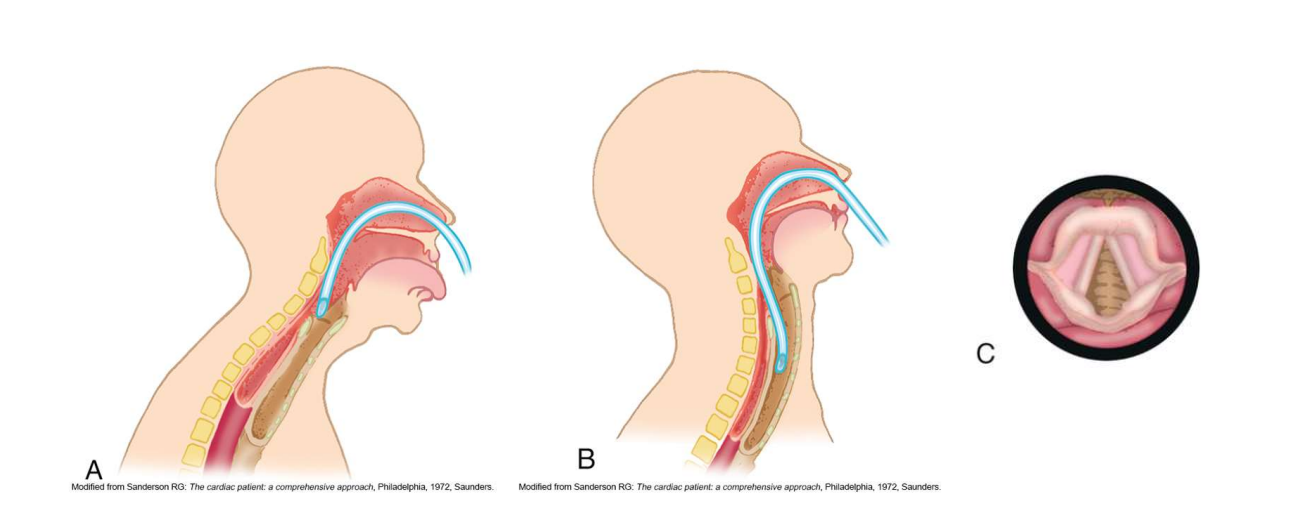
Sniffing position
Position used to facilitate nasotracheal suctioning; head position aids catheter passage.
Nasotracheal suctioning
Suctioning through the nose into the trachea for patients with secretions but no artificial airway.
May cause gagging or regurgitation; avoid after meals
Sputum sampling
Collection of sputum to identify airway organisms; use sterile technique.
Lukens trap
Sterile collection device used to collect sputum without contaminating the sample.
Sterile technique needs maintained when touching connection points on sterile Lukens trap
Securing the airway
ETT holders (ICU), tape (OR), commercial stabilizers, or cloth ties for tracheostomy to secure the airway.
How is proper placement of an ET or Tracheostomy tube confirmed?
Chest X-ray confirmation
Carina distance (ETT tip)
ETT tip should be 3–5 cm above the carina in adults, or between the second and fourth tracheal rings
Humidification
Artificial tracheal airways bypass upper airway humidification, filtration, and heating; device choice based on needs, assessment of airway, and volume and thickness of secretions/history of mucous plugging or tube occlusions of the pt.
Nosocomial infections
Pts. w/ ETT/Tracheal airways are susceptible to bacterial colonization and infection of lower respiratory tract
Risk of lower respiratory infection; emphasize hand hygiene and sterile technique during suctioning, and only aseptically clean/sterile respiratory equipment used for each pt.
Tube obstruction
Blockage of the airway tube; fix by repositioning head/neck or tube; suction as needed.
Kinking or biting tube
Tube obstruction from bending or biting; fixed by moving the pt’s head and neck or repositioning the tube.
Cuff herniation
Cuff protrudes over the tube tip; deflate cuff and/or pass suction catheter through tube if deflating cuff fails; reassess.
Mucus plugging
Obstruction due to mucus; clear with suction if instillation of sterile normal saline is not necessary.
Cuff leaks
Primary problem for pts receiving mechanical ventilation, causing reduction delivery of tidal volume
Leak around the cuff due to pilot/valve issues; may require tube change or ETT exchanger.
Endotracheal tube exchanger
Semirigid guide which damaged tube can be removed and new tube inserted.
Extubation
Process of removing an oral or nasal endotracheal airway.
Decannulation
Process of removing a tracheostomy tube.
Readiness for extubation/decannulation
OG problem is not present,assessment of secretions (quantity and thickness), upper airway patency, presence of gag reflex, and ability to clear secretions before removal.
What type of endotracheal suctioning is useful on high levels of PEEP?
Closed endotracheal suctioning
How do you minimize complications and adverse responses while suctioning?
Pre-oxygenation reduces inccidence of hypoxemia
Limit the amount of negative pressure used
Keep the time of suctioning duration low
Use appropriate size suction catheter
Avoid disconnection from ventilator
Use sterile technique during suctioning and manually ventilate pt. to minimize bacterial colonization
Don’t routinely instill sterile normal saline into artificial airway prior to suctioning unless needed to mobilize thick secretions
What do you do if secretions are thick and difficult to suction?
Ensure suction pressure in right range
Increase to maximum size suction catheter (not going over)
Increase suction pressure (not exceeding range)
Increase suction time
May also need to check canister of sputum, if too full will not suction properly
What is this picture of nasotracheal suctioning showing?
Sniffing position
What is this picture of sputum sampline showing?
Lukens trap
What type of tubes are these on the chest x-ray?
Left: Tracheostomy tube
Right: Endotracheal tube
Translaryngeal intubation
Endotracheal intubation passed through the larynx for airway ventilation (oral or nasal route); reevaluated daily with consideration of duration and potential transition to tracheostomy.
Extubation
Removal of the endotracheal tube; often planned within days of intubation; if extubation is unlikely, consider tracheostomy.
Tracheostomy
Surgical opening in the neck to access the trachea
Tracheotomy
Procedure of establishing access to trachea via neck incision, can be traditional surgical or percutaneous dilational, procedure best performed by physician/surgeon in surgical setting after pts airway is stabilized, tube selection depends on patient age, size, weight, and airway anatomy.
Tracheostomy tube
Tube placed via a tracheostomy to maintain airway; includes components such as outer cannula, flange, inner cannula, cuff, connectors, obturator, rounded tip, inflation tube, pilot balloon, & one way valve.
Outer cannula
The main, immovable tube that stays in the trachea to maintain the airway.
Inner cannula
Removable lumen inside the outer cannula; can be disposable or reusable and is cleaned/replaced as needed.
Cuff
Inflatable balloon on the tracheostomy tube used to seal the airway and secure ventilation.
Pilot balloon
Small balloon connected to the cuff used to monitor and adjust cuff inflation via the inflation tube.
Inflation tube
Channel connecting the pilot balloon to the cuff for cuff inflation and pressure monitoring.