Final - Biomedical Sciences (No Westburg)
1/299
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
300 Terms
Antibiotic Susceptibility Testing (AST)
when drugs are tested in vitro against a specific organism to determine a minimal inhibitory concentration
MIC (Minimal Inhibitory Concentration)
the lowest concentration of a drug that inhibits bacterial growth
MIC50
the drug concentration that inhibits 50% of the bacterial population
Susceptibility Breakpoint
the threshold of MIC or zine diameter used to categorize bacteria as susceptible, intermediate, or resistant to an antibiotic
How is culture and susceptibility testing conducted?
step 1 and 2:
- culture patient site and incubate sample until it turns positive
- gram stain and identification (takes up to 24-48 hours)
step 3:
- tak bacteria grown form the sample and inoculate/conduct susceptibility testing
- incubate 24-48 hours
advantages and disadvantages: broth microdilution
advantage: gold standard, automated testing, can test multiple strains
disadvantage: manual processes can be confusing; small volume.
advantages and disadvantages: agar dilution
advantage: quantitative, can test multiple strains
disadvantage: time-consuming, manually prepared, mainly for research
advantages and disadvantages: gradient diffusion strips
advantage: quantitative, faster than agar dilution
disadvantage: expensive, subjective reading, no clinical guideline recommendations
advantages and disadvantages: disk diffusion (Kirby-Bauer)
advantage: simple, inexpensive
disadvantage: qualitative only (no MIC values), limited by plate/bug/drug specifications
Susceptible
effective treatment likely at standard doses
Susceptible-dose-dependent (SDD)
effective only with higher or adjusted doses
Intermediate
moderate likelihood of treatment efficacy
Resistant
likely ineffective at normal doses
How is antibiotic therapy optimized based on AST results?
- after obtaining C&S results, determine the best antibiotic
- adjust dosing based on MIC proximity to breakpoints
- consider SDD drugs for higher dosing regimens or frequent administration
What is the role of breakpoints in antibiotic selection?
they are established based on clinical data and pharmacokinetics
How is pharmacodynamics helpful in antibiotic selection?
it helps define the concentration needed for effective therapy
High MIC values may indicate the need for __________ doses and ____________________ infusions.
higher/extended
Epidemiological Cutoff Values (ECV)
- represents the highest MIC in the wild-type (non-resistant) microbial population)
help assess microbial populations and resistance
Rapid Diagnostic Testing (RDT)
speed up diagnosis an susceptibility testing from days to hours
advantages and disadvantages of RDTs
advantages: timely antimicrobial optimization, improved patient outcomes, and reduced hospital costs
disadvantages: expensive, not widely used yet, and require significant teamwork and clinical intervention
What are bacterial pathogens that cause respiratory tract infections?
Haemophilus influenzae
Bordetella pertussis (whooping cough)
Moraxella catarrhalis
Streptococcus pneumoniae (Pneumococcus)
Pseudomonas aeruginosa
Legionella pneumophila
Klebsiella pneumoniae
Mycoplasma pneumoniae
Chlamydophila pneumoniae
Acinetobacter
Burkholderia
Stenotrophomonas
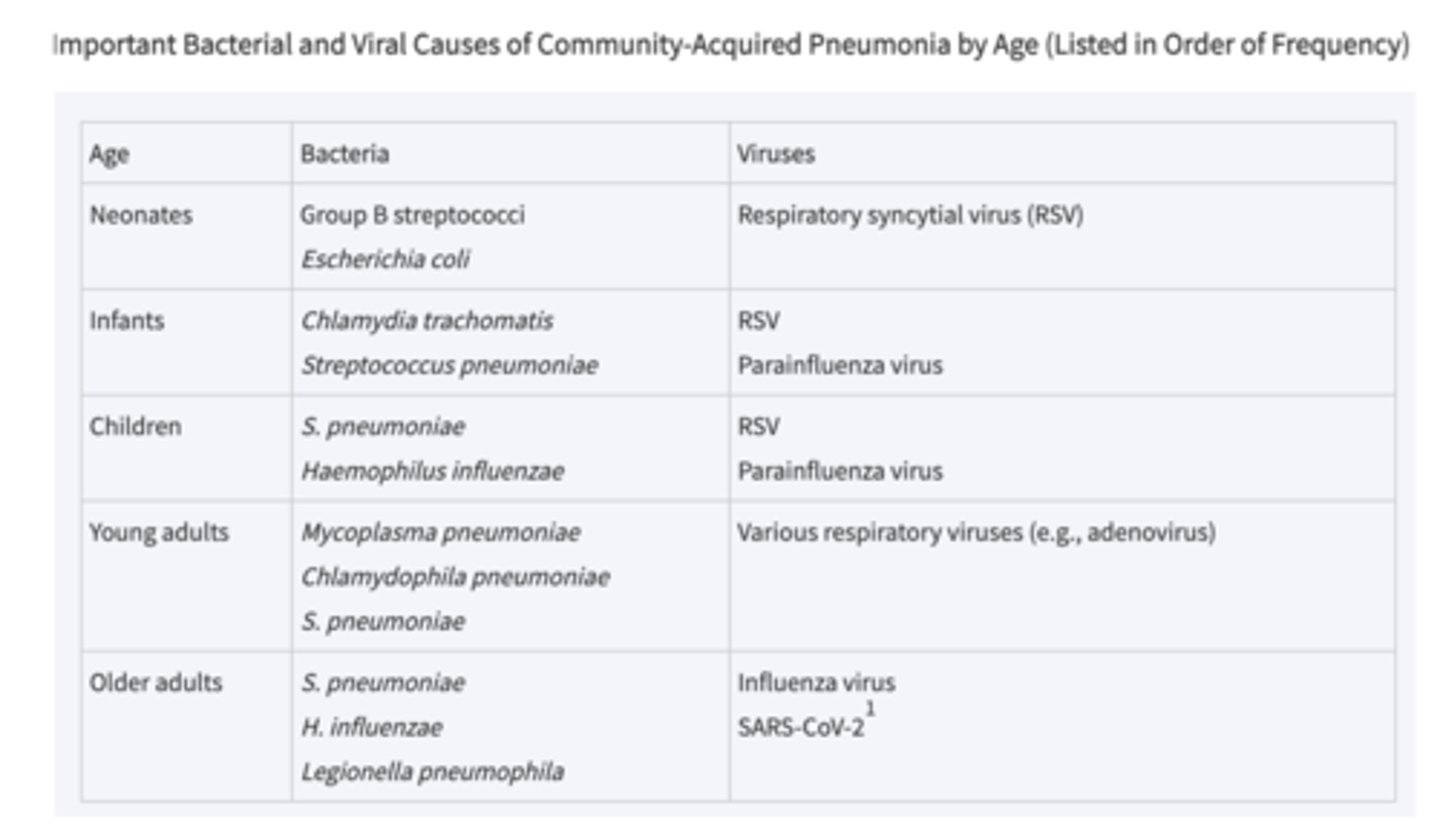
What are pathogens the cause community-acquired pneumonia (CAP)?
Streptococcus pneumoniae
Haemophilus influenzae
Mycoplasma pneumoniae
Chlamydophila pneumoniae
Legionella pneumophila
Moraxella catarrhalis
What are important bacterial pathogens that cause otitis media?
Streptococcus pneumoniae
Haemophilus influenzae
Moraxella catarrhalis
Klebsiella pneumoniae (in some cases)
Mycoplasmas
- unusual, self-replicating intracellular bacteria
- strict dependence on host for nutrients and refuge
- lacks a cell wall
Corynebacterium diphtheriae
- causes diphtheria
- symptoms of exudative pharyngitis with thick pseudomembrane on tonsils
- transmitted by inhalation or skin contact
- may cause obstructed breathing/suffocation, leading to mucosal cell death
Corynebacterium diphtheriae Pathogenesis
diphtheria toxin kills epithelial cells in the pharynx causing the pseudomembrane
- the important toxic effect are on the heart leading to heart failure
Atypical Pneumonia Charcateristics
- subacute onset
- nonproductive cough
- often less severe
- chest X-ray findings are often worse than the physical symptoms
What causes atypical pneumonia?
caused by Mycoplasma pneumoniae, Chlamydophila pneumoniae, and respiratory viruses
Typical Pneumonia Characteristics
- rapid onset
- productive cough
- more severe physical findings
What causes typical pneumonia?
caused by Streptococcus pneumoniae, Haemophilus influenzae, etc.
Describe how pneumonia pathogenesis occurs.
- pathogens are aspirated or inhales into the respiratory tract
- bacterial invasion leads to edema, infiltration of PMNs, RBCs, and macrophages
******Streptococcus pneumoniae causes no permanent tissue destruction, while S. aureus, enterobacteriaceae, and anaerobes cause permanent damage.
Transmitted via respiratory droplets
Haemophilus influenzae, Bordetella pertussis (Whooping Cough), Moraxella catarrhalis, Streptococcus pneumoniae (Pneumococcus), Mycoplasma pneumoniae, Chlamydophila pneumoniae
Klebsiella pneumoniae (from coughing or sneezing
Transmitted through contact with contaminated surfaces or medical equipment
Acinetobacter, Klebsiella pneumoniae, Pseudomonas aeruginosa, Burkholderia, Stenotrophomonas
Transmitted through aerosolized water droplets
Legionella pneumophila
found in environmental sources (e.g. soil and water)
Burkholderia species
found in aquatic environments
stenotrophomonas
skin and respiratory tract colonizer
Acinetobacter
Nosocomial (Hospital Acquired) Pathogens **Opportunistic
Acinetobacter, Klebsiella pneumoniae, Pseudomonas aeruginosa, Burkholderia, Stenotrophomonas
Which bacterial respiratory diseases are vaccine-preventable?
1. Streptococcus pneumoniae:
- vaccines cover 23 of the most common serotypes (adult vaccine) and 13 (childhood vaccine)
2. Haemophilus influenzae:
- Hib vaccine
- prevents meningitis, epiglottitis, and other infections
3. Bordetella pertussis:
- DTP vaccine prevents whooping cough
4. Corynebacterium diphtheriae:
- diphtheria vaccine
What are key aspects of bacterial pathogenesis in respiratory infections?
1. adherence
2. invasion
3. toxins
4. evasion of immune response
Adherence
bacteria attach to respiratory epithelial cells
Invasion
bacterial invasion of the alveoli causes inflammation, edema, and infiltration
Toxins
bacteria produce endotoxins or exotoxins that damage tissues and interfere with normal function
Evasion of Immune Response
bacteria use antiphagocytic capsules to evade immune system
Haemophilus influenzae Pathogenesis
- colonizes the upper respiratory tract and spreads via respiratory droplets
- produces endotoxins and antiphagocytic polysaccharide capsules, helping the pathogen evade immune defenses
Haemophilus influenzae causes
otitis media, sinusitis, bronchitis, pneumonia, meningitis, and epiglottitis
Bordetella pertussis Pathogenesis
- attaches to ciliated epithelial cells in the upper respiratory tract
- pertussis toxin interferes with cell signaling, leading to inflammation and cilial cell death
- causes persistent paroxysmal coughing, often leading to secondary complications like asthma exacerbations
________ treatment is most effective for treating Bordetella pertussis
early
Moraxella catarrhalis Pathogenesis
- transmitted via respiratory droplets and often causes otitis media in children
- can lead to bronchitis and pneumonia, particularly in older adults and immunocompromised individuals
- known for exacerbating chronic obstructive pulmonary disease (COPD) in adults
Acinetobacter causes
pneumonia, sepsis, and UTIs
- often in immunocompromised patients
Streptococcus pneumoniae (Pneumococcus) Pathogenesis
- colonizes the nasopharynx and can spread to the lungs, causing pneumonia
-produces a capsule that inhibits phagocytosis, a major virulence factor
Streptococcus pneumoniae (Pneumococcus) causes
otitis media, sinusitis, meningitis, and pneumococcal pneumonia
Streptococcus pneumoniae (Pneumococcus) i worsend by
pre-existing conditions like influenza or smoking
____________ is the key virulence factor and vaccine target the most common serotypes.
capsule
Which pathogen is resistant to beta-lactam antibiotics?
mycoplasma pneumoniae
Mycoplasma pneumoniae Pathogenesis
adheres to respiratory epithelial cells causing cilial dysfunction and necrosis
causes walking pneumonia
Mycoplasma pneumoniae
Legionella pneumophila Pathogenesis
- intracellular pathogen that infects macrophages and monocytes in the lungs
- endotoxins from bacterium cause inflammation and systemic responses
- leads to severe pneumonia
Legionella pneumophila causes
Legionnaire's disease
- high mortality in the immunocompromised and smokers
Klebsiella pneumoniae Pathogenesis
- capsule provides protection against phagocytosis
- bacterium can cause sepsis and bacteremia
**often antibiotic resistant
Pseudomonas aeruginosa Pathogenesis
- aerobe that infects CF patients and hospitalized patients on ventilators
- strong biofilm formation helps persist in the lungs and resist antibiotic treatment
What percentage of all acute morbidity in the US is due to respiratory disease, and how many of these are viral infections?
- respiratory disease accounts for 80% of all acute morbidity in the US
- 80% are viral
What are the two parts of the respiratory system?
Upper Respiratory Tract:
- conditions air and brings it into the lungs
Lower Respiratory Tract:
- where gas exchange occurs, including the respiratory bronchioles, alveolar ducts, and alveoli
What are terminal bronchioles, respiratory bronchioles, alveolar ducts, and alveoli?
Terminal bronchioles (TB) branch into respiratory bronchioles (RB), which branch further into alveolar ducts (AD) and individual alveoli (A).
Where does gas exchange between air and blood occur in the respiratory system?
occurs at the membranous barrier between each alveolus and the surrounding capillaries
What types of infections are common in the upper respiratory tract?
infections caused by viruses like influenza, parainfluenza, and rhinoviruses.
Which pathogens are common causes of infections in the lower respiratory tract?
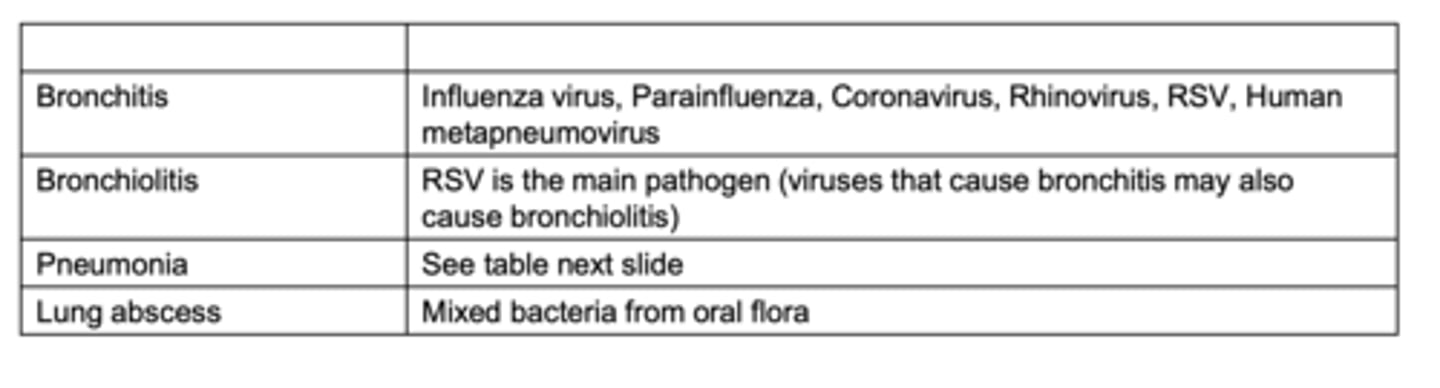
What are the causes of CAP? (virus focused)
SARS-CoV-2 Overview
- coronavirus
- ssRNA
- transmitted via respiratory droplets
- causes COVID-19 with potential for ARDS, cytokine storm, and viral sepsis
What is the general structure and mutation rate of coronaviruses?
Coronaviruses are single-stranded (+)-RNA viruses that mutate and recombine frequently.
They can exchange genes if they infect the same cell.
What respiratory conditions are caused by coronaviruses?
Most coronaviruses cause common cold symptoms. Some cause severe respiratory diseases like SARS, MERS, and COVID-19.
SARS - CoV1, highest death rates, very infectious, WIPED OUT
MERS - high likelihood of death if infected but difficult to transmit
How is SARS-CoV-2 transmitted?
via respiratory droplets
Where did SARS-CoV-2 originate?
from an animal source, specifically from viruses found in pangolins and bats
What is the general lifecycle of SARS-CoV-2?
infects cells through the ACE-2 receptor, replicates, and spreads throughout the body
Which cells does SARS-CoV-2 infect?
tissue in the nose, lung, and ileum
**predominantly infects the nose
**the ileum is where the virus replicates
What are the common signs and symptoms of COVID-19?
Fever, cough, difficulty breathing, loss of taste or smell, fatigue, muscle aches.
ARDS
adult (acute) respiratory distress syndrome
How does SARS-CoV-2 cause ARDS?
infection induces inflammation and cell death in the alveoli, causing edema and reduced oxygen exchange across the blood-gas barrier, leading to ARDS
What happens during a cytokine storm in SARS-CoV-2 infections?
the body thinks every tissue is being attacked which leads to an overactive immune response, causing widespread tissue damage and organ dysfunction, contributing to viral sepsis
How do COVID-19 tests work?
measure protein levels in nasal secretions using monoclonal antibodies that detect SARS-CoV-2 antigens
Influenza Overview
- segmented ssRNA
- transmitted by respiratory droplets
- causes URIs and LRIs
- can lead to secondary bacterial infections
What are the key properties of the influenza virus?
- orthomyxovirus with a segmented ssRNA genome
- has hemagglutinin (H) and neuraminidase (N) spikes on its surface
- infects many animal species
How is the influenza virus transmitted?
via respiratory droplets
Antigenic Drift
small, gradual changes in the virus's surface proteins (associated with seasonal flu epidemics)
Antigenic Shift
major genetic reassortment, often resulting in new, more dangerous strains (associated with pandemics)
What are the symptoms and complications associated with influenza infection?
Symptoms include:
- chills, fever, muscle aches, drowsiness
Complications include:
- pneumonia, bacterial superinfection, viral pneumonia with asphyxia
How does the influenza virus infect the respiratory tract?
- hemagglutinin binds to receptors on respiratory cells
- neuraminidase helps the virus release
- virus invades epithelium of URI and LRI
- leads to necrosis of ciliated and mucus-producing respiratory epithelial cells
- leads to secondary infections with viruses and bacteria
- can cause viral sepsis
Why are bacterial co-infections important in respiratory virus infections like influenza?
Influenza-induced damage to the respiratory epithelium increases susceptibility to bacterial colonization, making secondary bacterial infections more likely.
How does influenza cause local and systemic damage?
It causes local damage to lung tissue through cell necrosis and inflammation. Systemically, viral sepsis occurs due to the massive release of cytokines.
True or False: Both the SARS-CoV-2 and Influenza viruses can mutate leading to new strains.
True
What are the major genera of Gram-positive facultative cocci?
Staphylococcus, Streptococcus, and Enterococcus
What types of infections are caused by S. aureus?
- skin: boils, impetigo, cellulitis, mastitis
- bone and joint: osteomyelitis, septic arthritis
- necrotizing pneumonia, abscesses, sepsis
- toxinoses: gastroenteritis, food poisoning, toxic shock syndrome, scalded skin syndrome
What is a typical lesion caused by S. aureus?
Abscess (pus-forming) lesion
- can form externally or internally and is characterized by necrosis at the center
How does S. aureus cause damage at the cellular level?
It binds to epithelial cells using a binding protein expressed on the surface of the bacterial cell. It then releases a pore-forming toxin that damages the cells and attracts neutrophils to the infection site.
What is a furuncle and what causes it?
A furuncle (boil) is an infection of the hair follicle caused by S. aureus.
How does Methicillin-resistant Staphylococcus aureus (MRSA) resist antibiotics?
MRSA possesses genes that alter the target protein's (PBP) binding site. This prevents beta-lactam antibiotics from binding and inactivating the penicillin-binding protein (PBP).
What is the purpose of the sebaceous gland of a hair follicle?
It produces sebum which covers the skin and hair.
What is impetigo and how is it caused?
Impetigo is a superficial skin infection caused by either Streptococcus or S. aureus, characterized by weeping skin erosions and occasional bullous lesions.
How does S. aureus cause mastitis?
Mastitis often begins from cracks in the skin during nursing, leading to deep tissue infections and abscess formation.
What is osteomyelitis and how is it caused?
Osteomyelitis is an infection of the bone caused by S. aureus, typically leading to inflammation and pus accumulation in the bone.