N470: shock and mods (exam 4)
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
as a state of cellular and tissue hypoxia
shock
causes of shock (4)
1) reduced oxygen delivery
2) increased oxygen consumption
3) inadequate oxygen utilization
4) a combination of these processes
total amount of oxygen delivered to the tissues per minute
Global oxygen delivery (DO2)
Factors that affect how oxygen is delivered to tissues (3)
1) Hemoglobin
2) Cardiac Output (CO)
3) Arterial oxygen saturation
the total amount of oxygen removed from the blood due to aerobic metabolism
Oxygen consumption (VO2)
Factors that affect how oxygen is consumed (6)
1) Fever
2) Inflammation
3) Hyperthyroidism
4) Adrenergic drugs
5) Increased muscular activity
6) seizures, pain, vent weaning
oxygen extraction is...
based upon energy needs
where oxygen unloads from hgb to replenish tissues with low oxygen concentration
Oxygen Extraction
the "hold or grip" that the heme has on the O2 molecule.
Affinity
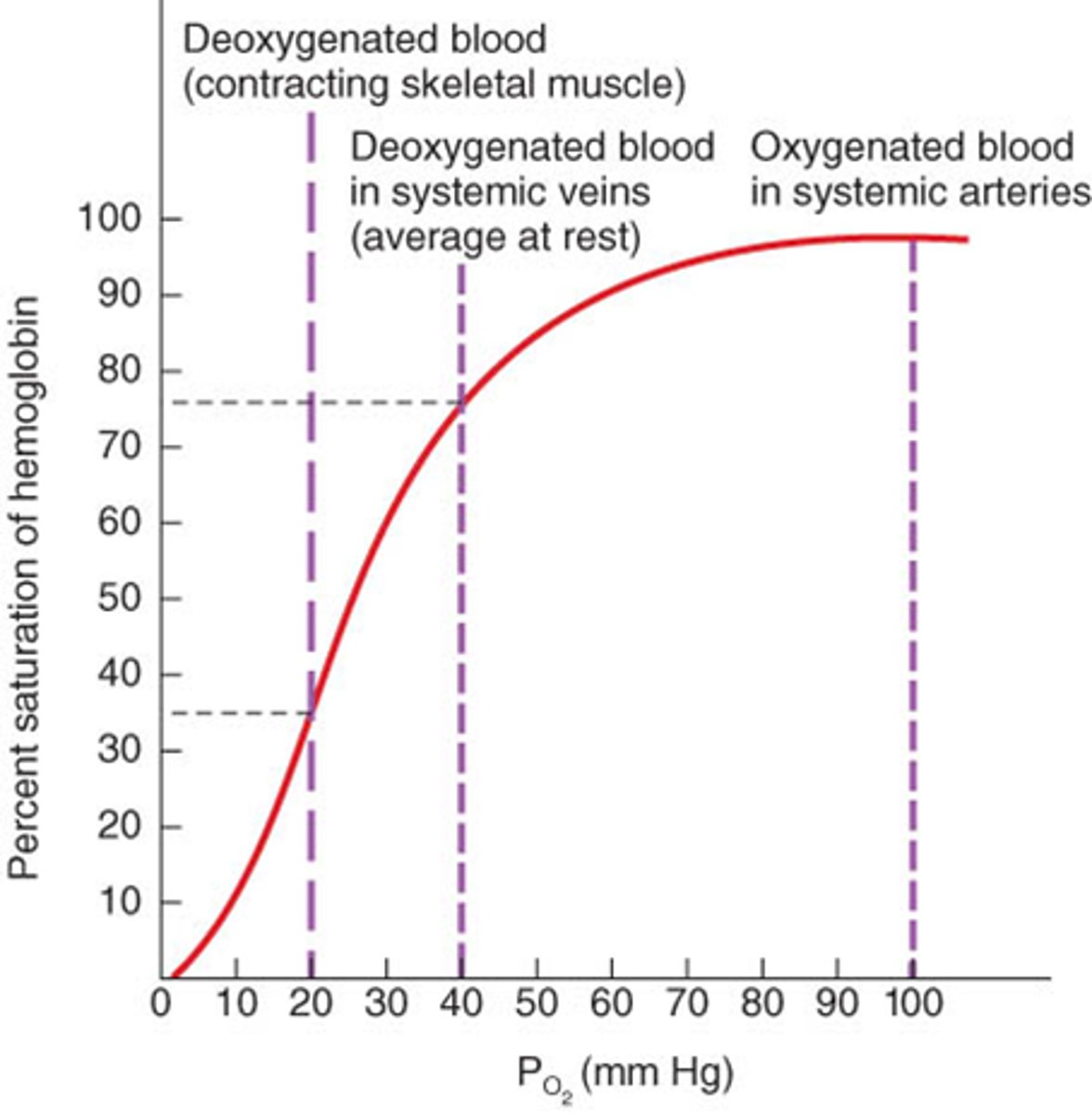
oxygen saturation vs. partial pressure
- both terms relate to oxygen levels in the blood
- oxygen saturation: the percentage of hemoglobin molecules in the blood bound to oxygen
- partial pressure: pressure exerted by oxygen gas within the blood, essentially representing the "available" oxygen in the blood
- a higher partial pressure of oxygen leads to a higher oxygen saturation, but the relationship is not linear and is depicted by the oxygen dissociation curve
Oxygen Extraction Ratio (O2 ER)
Ratio of O2 consumption (VO2) / (DO2)
O2ER of heart, liver, and kidneys
1) Cardiac O2ER = >60%
2) hepatic O2ER = 45-55%
3) Renal O2ER = <15%
A continuous measurement from the Pulmonary Artery. It measures the amount of oxygen returned to the right side of the heart after the organs/tissues have extracted O2
SVO2 Venous Oxygen Saturation
Low SVO2 indicates...
the supply of O2 is not meeting tissue or cellular demands- Increased Oxygen consumption
High SVO2 indicates...
inadequate oxygen extraction from the tissues
normal SVO2
70%
Contributors to low SVO2
1) Low hemoglobin
2) Low Cardiac Output
3) Heart failure/ Pulmonary Emboli
4) Increased Oxygen demand
Contributors to high SVO2
1) Sepsis (High CO, low extraction)
2) Acidosis
3) Hypothermia
4) Excessive use of vasoactive drug
Blood comes from the jugular or subclavian vein and is measured intermittently. Measures blood return from the upper body (head and upper extremities)
ScvO2 Central Venous Oxygen Saturation
Normal ScvO2
65%-75%
What would a ScvO2 value < 65% represent?
increased consumption
What would a ScvO2 value > 75% represent?
decreased consumption
Activities that increase ScvO2 (7)
- nursing assessment
- positioning (big)
- dressing change
- bed bath (big)
- restlessness/agitation
- weight patient on sling bed scale (big)
- visitors (big)
Abnormally High O2ER= (2)
Decreased Oxygen delivery OR increased consumption
causes of abnormally high O2ER
- Hypoxia
- Anemia
- Shock states
- Shivering (can burn 100 kcal/15 min)
- MODS
When tissues are deprived of O2 anaerobic metabolism begins and this produces what byproduct?
Lactic acid
What affect does acidosis have on O2 affinity?
initially increases it then decreases as it becomes more severe
What would a low O2ER suggest?
Increased oxygen delivery (DO2) but decreased oxygen consumption (VO2)
Causes of a low O2ER
1) Malnutrition
2) Hyperventilation
3) Hypometabolism
- sedation
- hypothyroidism
- paralysis
the amount of base (HCO3) required to titrate 1 liter of arterial blood back to normal
Base Deficit
Objective Parameters of Shock
1) Arterial pH outside of norm
2) Serum Lactate (>2 mmol/L)
3) Base Deficit
4) Procalcitonin for Septic Shock and MODS
Types of shock (4)
1) cardiogenic
2) hypovolemic
3) obstructive (least common)
4) distributive (most common)
- septic
- neurogenic
- anaphylactic
Shock phases
1) initial (treatable)
2) compensatory (treatable)
3) progressive (dangerous)
4) refractory
which phase of shock?
decreased cardiac output, decreased perfusion, decreased oxygenation=anaerobic metabolism -> Lactic Acidosis
initial
which phase of shock?
Neuroendocrine begins to augment cardiac output, blood flow and restoring blood volume
compensatory
which phase of shock?
Compensatory changes not working= poor perfusion, low blood flow, metabolic waste, Multiorgan Dysfunction Syndrome ( MODS
progressive
which phase of shock?
Cellular destruction, not responsive to vasopressors, hypoxemic despite Oxygen therapy, circulatory failure, impending death
refractory
physio occurring in initial phase of shock
- decreased CO
- decreased tissue perfusion
assessment findings in initial phase of shock
- high cap refill
- high HR
- low BP
physio occurring in compensatory phase of shock
- neurogenic response
- high glucocorticoids
- high catecholamines
- high vasopressin
physio occurring in progressive phase of shock
- persistent hypotension (Systolic <90, MAP < 65)
- Compensatory mechanisms (neuroendocrine) are failing, hyporesponsive to catecholamines
- Oxygen delivery (DO2) and Oxygen consumption(VO2) are now imbalanced
- Increasing Lactic Acid levels
- Hypoxia, cellular death, Multiple Organ Dysfunction Syndrome (MODS) begins
priority nursing actions in progressive phase of shock
1) give O2
2) fluids, pressors
physio occurring in refractory phase of shock
1) Significant vascular volume loss
2) Cellular ischemia and tissue death
3) Oxygen Delivery and Oxygen Consumption are not corrected with interventions
4) Multiple Organ Failure (MOF)
5) Disseminated Intravascular Coagulation (DIC)
6) Death is most likely immanent
what are the priorities in shock?
1) Optimize Oxygen delivery (DO2) to hypoxic tissue
2) fluid resuscitation
How to Restore preload and cardiac output in shock
- Initially Crystalloids (NS or LR) (Initial infusion 20mL-30mL/kg IV rapid infusion)
- RBCs
how to Restore Interstitial and Intravascular volume in shock
Colloids, Albumin, Starches, Dextrans
Shock priorities* (8) (ABCDEE,FGHI)
1) Airway Breathing Circulation or CAB (Stop bleeding and start two IVs)
2) D- Disability (neuro, alert oriented? PERRLA)
3) E- Environment (temp control)
4) E- Expose patient (look for bleeding or injury)
5) F- Five adjuncts/Focused Assessment- Xray, ABG, NG/OG, Labs, Monitor Family
6) G- give comfort
7) H-History
8) I- Inspect (this is your head to toe*)
How to determine type of shock
- pt history
- physical exam
- diagnostics
patient history to determine shock type (7)
1) Recent illness
2) Fever/hypothermia
3) Chest Pain
4) Traumatic Injury
5) Toxins/Ingestions
6) Recent hospitalization
7) Environmental Exposure
Diagnostic tests for shock
1) Physical Exam
2) EKG Chest
3) X Ray
4) CT
5) Infectious source?
6) Lab: CBC, Blood Cultures, UA/ Urine Drug Screen/ Urine HCG, Complete Metabolic Panel, Lactate and or Procalcitonin (sepsis), Coagulation, ABG, Lumbar Puncture
compensatory mechanism for shock
1) Increased heart rate (except in neurogenic)
2) Increased Respiratory rate
3) Increase Glycolysis
4) Decreased urine output
5) Decreased flow to internal organs
6) Decreased peristalsis (ischemic bowel)
7) Cool skin
8) Diaphoresis
causes of hypovolemic shock
1) Profound Dehydration
2) Plasma loss related to increased capillary permeability as in the case of burn injury
3) Blood loss- trauma, GI bleed, intracranial hemorrhage
Clinical manifestations of hypovolemic shock (7)
1) Tachycardia
2) Narrowed pulse pressure
3) Hypotension
4) Increased Respiration Rate
5) Decreased Urinary Output
6) Pale, cool, clammy skin
7) Delayed cap refill
A result of Spinal Cord Injury, Spinal anesthesia, Anoxic Brain Injury, Depressive Drugs which disrupt the Autonomic nervous system
neurogenic shock
symptoms of neurogenic shock
1) Decreased Blood pressure
2) Bradycardia (No reflexive tachycardia)
3) Increased Respirations
4) Warm Dry Skin
5) Decreased Cardiac Output
6) Inability to regulate core body temperature (Poikilothermia) they will take on the temperature of the room
Symptoms of anaphylactic shock
1) Tachycardia
2) Wheezing /Stridor
3) Rash/Hives/ Swelling
4) Vomiting
5) Decreased Cardiac Output
6) Hypotension (Systemic Vascular Resistance
Treatment for anaphylactic shock (9)
1) AIRWAY and BREATHING
2) Epinephrine IM 1:1000
3) Epinephrine IV 1:10,000
4) Vasopressors (possibly)
5) Diphenhydramine 50mg-100mg IV
6) H2 Blocker- Famotidine IV
7) Solu-Medrol or Dexamethasone
8) IV NS or LR Bolus
9) Continuous monitoring for rebound
Clinical manifestations of septic shock (7)
1) Tachycardia and Hypotension
2) High Cardiac Output with Low Systemic Vascular Resistance
-High CO Heart Failure 3) Wide Pulse Pressures
4) Bounding pulses
5) Fever or Hypothermia
6) Increased SVO2
7) Decreased CVP (decreased preload)
Would a septic shock patient have a high or low SVO2?
initially high, then progressively low
causes for obstructive shock (3)
1) tension pneumo
2) cardiac tamponade
3) pulmonary embolism
signs of cardiac tamponade*
Becks Triad - Hypotension, Increased CVP (JVD), Muffled heart tones
causes of cardiogenic shock (4)
1) Acute MI
2) Cardiomyopathy
3) Myocardial contusion
4) Myocarditis
symptoms of cardiogenic shock
1) Tachycardic, dysrhythmias
2) Decreased Cardiac output
3) Tachypnea
4) Crackles Weak and thready pulses
5) Diminished heart sounds
6) Decreased urine output
MODS can result from...
injury or infection
patho of MODS
1) Hypoxia
2) Anaerobic metabolism
3) Lactic Acidosis
4) Unregulated apoptosis due to inflammation
5) Disrupted blood flow -> micro vascular coagulopathy (DIC)
MODS nursing actions
1) ASSESS and REASSESS
2) Control Infection
3) Enhance perfusion
4) Initiate renal replacement therapy (CRRT)
5) ECMO
6) Heparin
7) Mechanical Ventilation
8) Glucose Control and Enteral Feeds
9) Educate Family
10) Prognosis 40-80% mortality
Arterial Oxygen Saturation (SaO2)
percent of oxygen dissolved into arterial blood; 95-100%; pressure O2 in ABG
______ changes at low pO2 (partial pressure O2) leads to _______ changes in oxygen saturation
small changes at low pO2 (partial pressure O2) leads to large changes in oxygen saturation
shift to the right
- affinity for O2 by Hgb decreased
- occurs in tissues
- causes: low ph (acidosis), fever, high DPG
- tissue: muscles
oxygen dissociation curve- X axis and Y axis
- X axis: pO2 (mmHg)
- Y axis: O2 saturation (%)
factors that shift the oxyhemoglobin dissociation curve
1) ph
2) temp
3) 2,3 DPG
shift to the left
- higher affinity of O2 to hgb
- causes: high ph (alkalosis), hypothermia, low DPG
- tissues: lungs
What affects DPG?
hypertonic IV solutions (NS 3%)
describe the neuroendocrine response in the compensatory shock phase
epinephrine alters the neuro system
what does a lumbar puncture reveal during shock?*
- high bacteria, WBC
- low glucose (eaten by bacteria)
- high protein (pooped out by bacteria)
- looks for infection and bleeds from trauma
Symptoms of obstructive shock (3)
1) hypotension
2) JVD
3) muffled heart sounds (tamponade)