Egan Ch 44
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
Understand the normal physiology of airway clearance.
Normal airway clearance is essential for maintaining healthy respiratory function and relies on three key components:
Patent Airway: The airways must be open and free from obstruction.
Functional Mucociliary Escalator: This system involves cilia (tiny hair-like structures) that continuously beat to propel a layer of mucus (which traps inhaled particles and pathogens) upwards from the lungs towards the pharynx, where it can be swallowed or expelled. This includes proper mucus production and transport.
Effective Cough: A vital reflex mechanism that can forcefully expel mucus and foreign material from the lower airways to the upper airway, allowing for its removal.
What is a cough and the phases of a cough?
A cough is a vital protective reflex and a primary mechanism for airway clearance, especially for secretions located in the central airways. It's a complex process involving a series of coordinated events.
The Four Phases of a Cough:
Irritation Phase: This is the initiation phase, where abnormal stimuli (such as inflammation, mechanical irritation, chemical irritants, or thermal changes) stimulate cough receptors located in the larynx, trachea, large bronchi, and sometimes even in the stomach or diaphragm.
Inspiration Phase: Following the irritation, a reflexively deep inspiration occurs. In adults, this typically involves inhaling a volume of 1 to 2 liters of air. This large inhaled volume is crucial for generating the force needed for expulsion.
Compression Phase: The glottis (the opening between the vocal cords) closes, and the expiratory muscles (like the abdominal and internal intercostal muscles) contract forcefully. This action rapidly increases the intrathoracic pressure. This phase is normally very brief, lasting about 0.2 seconds.
Expulsion Phase: The glottis suddenly opens, and the previously built-up high intrathoracic pressure creates a large pressure gradient between the airways and the atmosphere. This results in a violent, explosive flow of air out of the lungs, effectively expelling mucus and foreign material.
What is abnormal airway clearance?
Abnormal airway clearance occurs when any of the components of normal clearance (airway patency, mucociliary function, strength of breathing muscles, thickness of secretions, or cough reflex) are compromised.
What are the consequences of secretion retention?
Full Obstruction (Mucous Plugging): Can lead to atelectasis (lung collapse), resulting in hypoxemia due to shunting.
Partial Obstruction: Restricts airflow, increasing the work of breathing and potentially causing air trapping, lung overdistention, and V/Q (ventilation-perfusion) imbalances.
Can increase the WOB, cause air trapping, worsen V/Q imbalance, and increase incidence of infection.
What are the pulmonary diseases and conditions associated w/ abnormal clearance?
Internal or external compression of the airway lumen.
Cystic Fibrosis (CF): Characterized by thick, sticky mucus production.
Bronchiectasis: Chronic dilation and infection of the bronchi, leading to impaired mucus clearance.
Ciliary Dyskinetic Syndromes: Conditions where cilia do not function properly.
Neuromuscular Diseases: Can weaken breathing muscles, leading to an ineffective cough.
Musculoskeletal & neurologic disorders can impair coughing and lead to mucous plugging, airway obstruction, and atelectasis
Foreign bodies, tumors, congenital/acquired thoracic anomalies, asthma, chronic bronchitis, and acute infections
What are the causes of impaired mucociliary clearance in intubated patients?
Presence of an endotracheal or tracheostomy tube.
Frequent tracheobronchial suctioning.
Inadequate humidification of inspired gases.
High FiO2 values (fraction of inspired oxygen).
Certain drugs such as general anesthetics, opiates, and narcotics.
Underlying pulmonary disease.
Who primarily may benefit from ACT?
Patients with copious secretions (20 - 30 mL/day) or inability to mobilize and expectorate secretions may benefit from ACT
What is the primary goal of ACT?
Help mobilize and remove retained secretions, improve gas exchange, and reduce WOB
What are clinical signs consistent w/ retained secretions?
Ineffective cough, absent or increased sputum production, labored breathing pattern, abnormal or adventitious lung sounds (coarse crackles, decreased breath sounds), tachypnea, tachycardia, and fever
List the indications for airway clearance therapy.
Airway clearance therapy (ACT) is indicated for patients with conditions that cause abnormal secretion accumulation and impaired clearance.
Indications are broadly categorized as:
Acute Conditions:
Acute respiratory failure with copious secretions.
Acute lobar atelectasis (specifically due to mucous plugging).
Ventilation-perfusion (V/Q) abnormalities resulting from retained secretions.
Chronic Conditions:
Cystic Fibrosis (CF).
Bronchiectasis.
Ciliary dyskinetic syndromes.
COPD patients with retained secretions.
Other Patient Populations who May Benefit:
Patients on prolonged bed rest.
Individuals with neuromuscular disorders affecting cough effectiveness.
Post-operative patients at risk for secretion retention.
Patients with chronic lung disease leading to secretion problems.
What is the description of chest physiotherapy (CPT)?
Involves the use of positioning, gravity, and mechanical energy to help mobilize secretions.
This includes manually striking the chest wall with cupped hands in a rhythmic fashion (percussion) and vibrating the chest wall with hands or a mechanical device (vibration).
The goal is to loosen secretions and propel them forward.
The patient is placed in various positions to allow gravity to assist in draining secretions from lung segments to larger airways.
Involves placing the segmental bronchus to be drained in a vertical position relative to gravity and holding the position for 3-5 minutes
How long should total CPT treatments last?
15 - 30 minutes
15 minutes for routine and 30 minutes for extended treatments
The positions are generally held for 3 - 15 minutes
What are the potential limitations when it comes to CPT?
Requires the help of a caregiver.
Effectiveness may depend on appropriate positioning.
Patients with shortness of breath may not tolerate the Trendelenburg position.
Patients are unable to perform concurrent aerosol therapy.
What are the contraindications for CPT?
Positioning is contraindicated for:
Head and neck injury until stabilized (A).
Active hemorrhage with hemodynamic instability (A).
Intracranial pressure (ICP) greater than 20 mmHg.
Recent spinal surgery or acute spinal injury.
Active hemoptysis.
Empyema.
Bronchopleural fistula.
Pulmonary edema associated with congestive heart failure.
Aged, confused, or anxious patients who do not tolerate position changes.
Pulmonary embolism.
Rib fracture, with or without flail chest.
Surgical wound or healing tissue.
Large pleural effusions.
What are the complications and recommended interventions for CPT? (Triple S Rule)
Whenever adverse effects or complications occur during postural drainage, stop the therapy, return the patient to the original resting position, and stay with the patient until they are stabilized.
Hypoxemia: Administer higher FiO2 if potential or observed. If patient becomes hypoxemic, administer 100% O2, stop therapy, return to original position, and consult physician.
Increased intracranial pressure: Stop therapy, return patient to original resting position, and consult physician.
Acute hypotension during procedure: Stop therapy, return patient to original resting position, and consult physician.
Pulmonary hemorrhage: Stop therapy, return patient to original resting position, call physician immediately, administer O2, and maintain an airway.
Pain or injury to muscles, ribs, or spine: Stop therapy associated with pain, exercise care in moving patient, and consult physician.
Vomiting and aspiration: Stop therapy, clear and suction airway, administer O2, maintain airway, return to previous resting position, and contact physician immediately.
How long after tube feeds/meals should CPT be scheduled to avoid GERD/vomiting?
treatment times should be scheduled before or at least 2 hours after meals or tube feedings to decrease the chance of vomiting or aspiration
What therapies make up CPT?
Postural drainage - head-down positions should exceed 25 degrees below horizontal. If the patient cannot be placed in appropriate positions for the areas affected, another ACT should be considered.
Percussion & Vibration - involve applying mechanical energy to the chest wall using hands or various electrical or pneumatic devices
Manual percussion - The RT performs manual percussion with their hands in a cupped position, with fingers and thumb closed and positioned parallel to the ribs. This technique compresses air between the hand and chest wall and should be applied against a thin layer of cloth
Mechanical Percussion & Vibration - Mechanical vibration is an alternative to manual percussion in acutely ill patients with chest wall discomfort or injury. Various electrical and pneumatic devices have been developed to generate and apply the energy waves used during percussion and vibration. Typically, these devices have both a frequency and a percussion force control. Most units provide frequencies between 20 and 50 cycles per second (20 to 50 Hertz [Hz]). Other sonic or acoustic devices may provide up to 120 Hz
What should we avoid percussing over?
Avoid tender areas or sites of trauma, surgery, chest tubes, and bony prominences, such as the clavicles, vertebrae, or sternum
Describe directed coughing
Description: A deliberate maneuver that is taught, supervised, and monitored, aiming to mimic features of an effective spontaneous cough.
Technique: Involves instruction on proper positioning, breathing control, and having the patient bear down against the glottis after a deep inspiration. Exercises to strengthen expiratory muscles may also be included.
Contraindications/Limitations: Not to be used in patients who are obtunded, paralyzed, or uncooperative. Good patient teaching and proper positioning are critical, and the technique may need modification for surgical patients, COPD patients, and those with neuromuscular disease.
Describe FET (“huff cough”)
Consists of one or two forced expirations of middle to low lung volume without closure of the glottis, followed by a period of diaphragmatic breathing and relaxation.
Description: A modification of directed cough, also known as a "huff cough."
Technique: Consists of one or two forced expirations from middle to low lung volumes without glottic closure.
Goal: To clear secretions with less change in pleural pressure and less bronchial collapse.
Describe Vibratory positive expiratory pressure therapy
Description: A self-administered clearance technique involving active expiration against a variable-flow resistance. It incorporates flow interruptions during active expiration to create flow oscillations in addition to the Positive Expiratory Pressure (PEP).
Examples: Acapella, Aerobika, and Flutter devices
Types of Oscillatory PEP (OPEP) devices:
Flutter valves: Only oscillate.
Vibratory PEP devices: Oscillate with backpressure (most common now).
Steps to use an OPEP device:
Assemble the device.
Get in the correct position (Flutter valve held upright; Aerobika can be used in any position).
Take a deep breath.
Place the mouthpiece in your mouth and create a tight seal.
Exhale against backpressure, slightly faster than normal (actively, but not forcefully, with an inspiratory-to-expiratory ratio of 1:3 to 1:4).
Adjust the device to create the most vibrations felt in the lungs.
Repeat step 5 for up to 10 exhalation maneuvers.
Perform two or three "huff" coughs; rest as needed.
Repeat the process for four to eight cycles.
What are contraindications for Vibratory positive expiratory pressure therapy?
(relative; no absolute contraindications):
Untreated pneumothorax.
Intracranial pressure >20 mmHg.
Hemodynamic instability.
Active hemoptysis.
Recent facial trauma or surgery.
Patients with acute asthma or COPD.
Acute sinusitis.
Acute epistaxis.
Tympanic membrane rupture.
Acute nausea.
Not recommended for:
Children under 3 years old, as they cannot follow instructions.
Adults unable to take a deep breath and generate >10 to 12 mL/kg of expiratory pressure (needed for oscillations).
Mechanical insufflation-exsufflation (MIE)
Description: MIE devices deliver a positive-pressure breath (30 to 50 cm H2O) to the airway for 1 to 3 seconds, then abruptly reverse to a negative-pressure breath (-30 to -50 cm H2O for 2-3 seconds) A pause can be included.
Function: Positive expiratory flows generated by MIE exceed those developed by manually assisted coughing. Newer systems can also generate oscillatory positive pressure.
When used: Used in patients with neuromuscular conditions who are unable to generate a forceful expulsion.
patients who cannot demonstrate a peak cough flow greater than 160 L/min or generate an effective cough may benefit from MIE
High-frequency airway pressure devices (IPV, metaneb)
Description: These devices deliver a rapid series of pressurized gas mini-bursts to the airway.
Intrapulmonary Percussive Ventilation (IPV): A pneumatic device that delivers mini-bursts at rates of 100 to 225 cycles per minute (1.7 to 5 Hz).
Metaneb: A type of IPV device.
What are the instructions for IPV?
Connect IPV unit to a 50-psi air or oxygen source, ensuring the master switch is OFF.
Place the patient in an upright, comfortable position if possible.
Connect the short harness end to the IPV unit using correct color coding.
Connect the long harness end to the Phasitron and nebulizer using correct color coding.
Fill the nebulizer with prescribed medications and dilute to 15–20 mL. IPV therapy should not be administered without normal saline or other medications.
Rotate the frequency control knob fully counterclockwise to the “easy” position.
Rotate the source pressure control knob to a driving pressure of 15–20 psi.
Instruct the patient to inhale and exhale during the percussions ("active breathing cycle").
Maintain percussions during inspiration and expiration.
Instruct the patient to keep their lips sealed tightly around the mouthpiece.
Encourage slow deep breaths and assess for signs of hyperventilation.
Gradually increase the driving pressure to achieve effective percussions by assessing chest wiggle/chest wall motion.
Once an effective driving pressure is selected, gradually rotate the frequency control knob clockwise towards the “hard” position until the arrow matches the “12 Noon” calibration.
Assess patient comfort; rotate the frequency control counterclockwise if discomfort occurs.
Maintain these “Hard Settings” for approximately 5 minutes.
After 5 minutes, gradually turn the frequency control knob fully counterclockwise towards the “easy” position.
Assess the patient and maintain “Easy Settings” for 5 minutes.
During the 15–20 minute treatment, rotate the frequency control knob between “easy” and “hard” settings at 5-minute intervals.
Break the active breathing cycle, allowing the patient to rest.
Encourage the patient to cough and clear mobilized secretions.
Continue treatment until all medication has been delivered.
Periodically assess the patient and encourage slow deep breaths during the active breathing cycle.
Is any ACT proven better than another?
No ACT has been proven better than another, but numerous factors must be considered in trying to select the best airway clearance strategy for a given patient
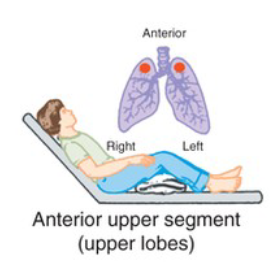
What CPT position is pictured, and when is it used?
Anterior upper segment (upper lobes)
Secretions are in the anterior segments of the upper lobes
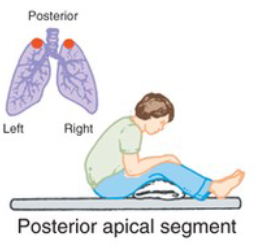
What CPT position is pictured, and when is it used?
Posterior apical segment
Secretions are in the apical/posterior segments of the upper lobes.
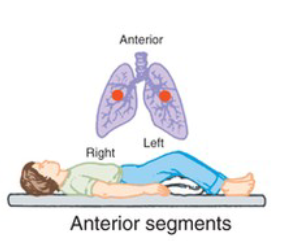
What CPT position is pictured, and when is it used?
Anterior segments
Secretions are in anterior upper lobe segments, both lungs
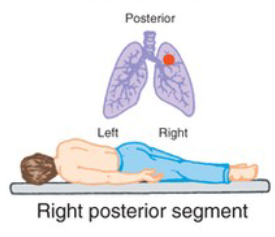
What CPT position is pictured, and when is it used?
Right posterior segment
Secretions are in the posterior segment of the right upper lobe
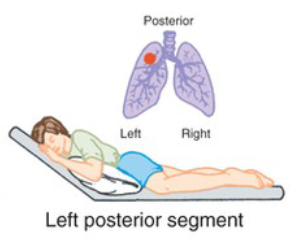
What CPT position is pictured, and when is it used?
Left posterior segment
Secretions are in posterior segment of the left upper lobe
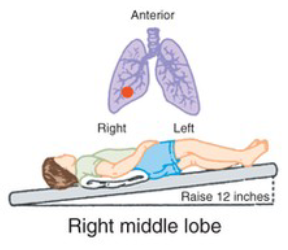
What CPT position is pictured, and when is it used?
Right middle lobe
Secretions are in medial and lateral segments of the right middle lobe
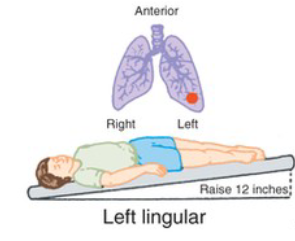
What CPT position is pictured, and when is it used?
Left lingular
Secretions are in the superior/inferior segments of the left lingula
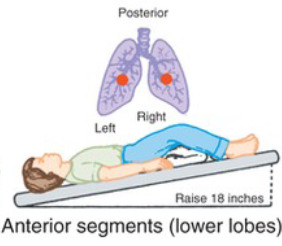
What CPT position is pictured, and when is it used?
Anterior segments (lower lobes)
Secretions are in anterior basal segments of lower lobes
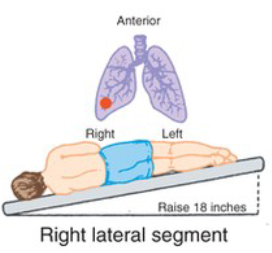
What CPT position is pictured, and when is it used?
Right lateral segment
Secretions are in lateral basal segment of right lower lobe
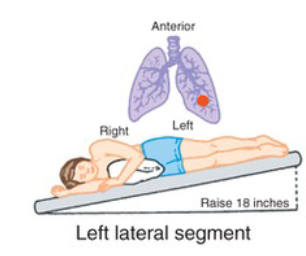
What CPT position is pictured, and when is it used?
Left lateral segment
Secretions are in lateral basal segment of left lower lobe
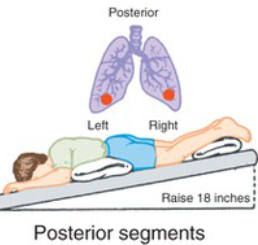
What CPT position is pictured, and when is it used?
Posterior segments
Secretions are in posterior basal segments of both lower lobes
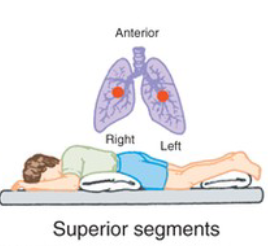
What CPT position is pictured, and when is it used?
Superior segments
Secretions are in superior segments of lower lobes