Chapter 44: "Child Maltreatment" and "Depression, Suicide, Bullying"
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Depression
Symptoms must persist for 1 year
Often overlooked in school-aged children
Due to their limited ability to express feelings.
Risk Factors:
Family history
Traumatic event (e.g., abuse, loss of a loved one, divorce).
Expected Findings:
Emotional Symptoms:
Sad facial expressions, tearfulness/crying, feelings of worthlessness, hopelessness, suicidal ideationBehavioral Symptoms:
Tendency to remain alone, withdrawal from family/friends/activities, lack of interest in school, drop in academic performancePhysical Symptoms:
Fatigue, ill feeling, weight loss or gain, alterations in sleep patterns, constipationCognitive Symptoms:
Statements of low self-esteem, lack of focus or attention
Depression Care
Individualized Care
Health History & Growth/Development information.
Substance Use Assessment
Risk Assessment
Suicide plan
Lethality of the plan
Means to carry out the plan
Coping Strategies
Peer Support
Encourage participation in:
Peer group discussions
Mentoring
Counseling sessions
Child Interview
Medication
Tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs)
Trazodone, sertraline, paroxetine, bupropion, venlafaxine
Tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs) Meds
Trazodone, sertraline, paroxetine, bupropion, venlafaxine
Tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs)
Nursing Actions
Monitor for adverse effects.
Monitor for suicidal ideation.
Client Education
Observe for adverse effects.
Therapeutic effectiveness can take up to 2 weeks.
Do not abruptly discontinue the medication.
Suicide Expected Findings
1. Behavioral and Verbal Clues
Monitor Carefully: Look for verbal and nonverbal signs of suicidal ideation.
Asking if they are thinking of suicide will not give them the idea.
Types of Suicidal Comments:
Overt (Direct): "There is just no reason for me to go on living."
Covert (Indirect): "Everything is looking pretty grim for me."
2. Assessing Plan
Key questions to determine risk:
Does the client have a plan?
How lethal is the plan?
Can the client describe the plan in detail?
Does the client have access to the intended method?
Has the client’s mood changed?
A sudden shift from sadness to calmness could indicate intention.
3. Physical Findings
Self-Harm Indicators:
Lacerations
Scratches
Scars that may indicate prior suicide attempts or self-harm behavior.
Maltreatment
Harmful behaviors towards infants and children, influenced by parental, child, and environmental factors.
Occurs across all economic, educational, and cultural groups.
Physical Abuse
Causing physical harm or pain.
Examples:
Shaken baby syndrome.
Fractures.
Factitious disorder imposed on another (e.g., Munchausen syndrome by proxy).
Sexual Abuse
Any sexual contact involving a minor, with or without consent.
Examples:
Sexual violence towards a minor.
Dating violence among adolescents.
Emotional Abuse
Behavior that humiliates, threatens, or intimidates a child, negatively impacting their sense of self-worth.
Neglect
Failure to provide basic needs.
Physical Neglect: Feeding, clothing, shelter, medical or dental care, safety, or education.
Emotional Neglect: Failure to provide nurturing, affection, attention, and stimulation necessary for normal development.
Neglect
Failure to provide basic needs.
Physical: Feeding, clothing, shelter, medical or dental care, safety, or education.
Emotional: Failure to provide nurturing, affection, attention, and stimulation necessary for normal development.
Emotional Abuse
Behavior that humiliates, threatens, or intimidates a child, negatively impacting their sense of self-worth.
Sexual Abuse
Any sexual contact involving a minor, with or without consent.
Examples:
Sexual violence towards a minor.
Dating violence among adolescents.
Physical Abuse
Causing physical harm or pain.
Examples:
Shaken baby syndrome.
Fractures.
Factitious disorder imposed on another (e.g., Munchausen syndrome by proxy).
Factitious disorder / Munchausen syndrome
A mental health condition where a person intentionally and deceptively creates or exaggerates physical or psychological symptoms to gain attention, sympathy, or medical treatment
Maltreatment Risk Factors
1. Caregiver Characteristics
Young age.
Having a partner unrelated to the child.
Social isolation.
Low-income situation.
Lack of education.
Low self-esteem.
Lack of parenting knowledge.
Substance use disorder.
History of having been abused.
Lack of support systems.
2. Characteristics of the Child
Increased risk for children:
1 year old or younger due to constant attention needs.
Unwanted or hyperactive children, or those with physical/mental disabilities.
Premature infants, due to potential parent-child bonding issues at birth.
3. Environmental Characteristics
Chronic stress.
Divorce, alcohol/substance use disorder, poverty.
Unemployment, inadequate housing, crowded living conditions.
Substitute caregivers.
Warnings Indicators Maltreatment Findings
Physical evidence
Vague explanations of injury.
Injuries unrelated to the stated reason for seeking care.
Delay in seeking medical care.
Statements or signs of possible abuse from the caregiver or child.
Inconsistencies:
Between caregiver's report and the child’s injuries.
Between the nature of injury and the child’s developmental level.
Repeated emergency visits for injuries.
Inappropriate responses from the parent or child.
Physical Neglect Findings
Failure to thrive, malnutrition.
Poor hygiene.
Frequent injuries.
Delayed healthcare seeking.
Dull emotional affect.
School absences.
Self-stimulating behaviors (e.g., rocking, head-banging).
Physical Maltreatment Findings
Bruises or welts in different stages of healing.
Bruises in non-mobile children (indicative of concern).
Multiple fractures at various stages of healing.
Burns, fractures, lacerations.
Fear of parents.
Lack of emotional response or inappropriate emotional reactions.
Superficial relationships (difficulty forming attachments).
Withdrawal or aggression.
Emotional Neglect and Abuse Findings
Failure to thrive.
Eating disorders.
Enuresis (bedwetting).
Sleep disturbances.
Self-stimulating behaviors (e.g., rocking, head-banging).
Withdrawal and lack of social interaction (e.g., infant's lack of smile).
Delayed development.
Extreme behaviors or attempts at suicide.
Caregiver Behaviors: Rejecting, isolating, terrorizing, ignoring, verbally assaulting, or over-pressuring the child.
Sexual Abuse Findings
Bruises, lacerations.
Bleeding from genitalia, anus, or mouth.
Sexually transmitted infections (STIs).
Difficulty walking or standing.
Urinary Tract Infections (UTI).
Regressive behaviors (e.g., bedwetting, thumb-sucking).
Withdrawal or personality changes.
Bloody, torn, or stained underwear.
Unusual body odor.
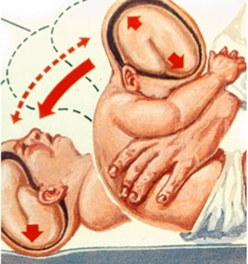
Abusive head trauma (ART) or shaken baby syndrome
May have no visible injuries.
Vomiting, poor feeding, listlessness.
Respiratory distress.
Bulging fontanels (soft spot on infant’s skull).
Retinal hemorrhages.
Seizures, posturing.
Altered levels of consciousness or unresponsiveness.
Apnea, bradycardia (slow heart rate).
Blindness.
Important Note: Bruising in infants under 6 months requires immediate investigation.
Laboratory Tests for Maltreatment
CBC, urinalysis, and other tests that assess for sexually transmitted infections or bleeding
Diagnostic Procedures for Maltreatment
Depend upon the assessment findings and injuries.
Radiograph
Computed tomography or magnetic resonance imaging scan
Nursing Priorities for Maltreatment
Remove the child from the abusive situation.
Mandatory reporting: Report all suspected cases of child maltreatment as required by law.
Assessment Guidelines for Maltreatment
Interview
Conduct interviews with the child and guardians individually
Provide safety and reduce risk for the victim.
Use open-ended questions to gather detailed information.
Use clear, age-appropriate language.
Be direct, honest, and professional.
Ensure the child feels understood and supported.
Avoid leading or probing questions.
Inspect for unusual bruising (abdomen, back, buttocks) with attention to:
Shape, size, and color.
Patterns like belt buckles or specific objects.
Observe for burns:
Stocking-like burns (hands or feet) could indicate immersion in hot liquid.
Small, round burns (possible cigarette burns).
Note fractures: Spiral fractures (indicative of twisting injuries) and multiple fractures at different stages of healing.
Evaluate for head injuries: Assess level of consciousness, pupil reaction, and nausea/vomiting.
Documentation
Use diagrams to record injury location.
Clearly describe findings, including size and characteristics of injuries.
Photograph injuries with consent (include measuring tools for scale).
Risk Factors for Bullying
For Perpetrators:
Male sex.
Depression.
Decreased academic performance.
Reduced social involvement with peers.
Exposure to family violence (e.g., spouse or partner violence).
Conduct problems.
Criminal acts.
Dropping out of school.
For Recipients:
Low self-esteem.
Loneliness.
Somatic complaints (e.g., headaches, stomachaches).
Anxiety.
Depression.
Care for Bullying
Be Observant: Look for signs of behavior or its effects.
Support System: Encourage family involvement and emotional support.
Referrals:
Refer to counseling or prevention programs.
Suggest mental health evaluations, as it may signal or contribute to mental health issues.
Action Steps:
Teach procedures for investigating and reporting incidents.
Emphasize the importance of addressing it early to prevent its escalation.
A nurse is teaching a group of caregivers about abusive head trauma (AHT) or shaken baby syndrome.
What manifestations should be included in this presentation?
Underlying Principles: Include seven manifestations.
Vomiting
Caused by increased intracranial pressure or brain swelling.
Respiratory Distress
Difficulty breathing or abnormal respiratory patterns due to brain injury.
Seizures
Uncontrolled muscle movements resulting from brain trauma.
Altered Level of Consciousness (Lethargy or Unresponsiveness)
Infants may appear unusually sleepy, unresponsive, or have difficulty staying awake.
Retinal Hemorrhages
Bleeding in the eyes, often visible during an eye examination, which is a hallmark sign of AHT.
Bulging Fontanels
Swelling of the soft spots on an infant's head due to increased pressure within the skull.
Bruising in Non-Mobile Infants
Unexplained bruising, especially in non-mobile infants, may indicate external injury consistent with shaking or abuse.