Infection Control-Ch 19/TEST
1/72
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
acquired immunity
immunity that is developed during a persons lifetime
acute infection
infection of short duration that is often severe
anaphylaxis
extreme hypersensitivity to a substance that can lead to shock and life threatening respiratory collapse
artificially acquired immunity
immunity gained through vaccination or medical intervention.
blood borne disease
disease that is caused by microorganisms such as viruses or bacteria that are carried in blood
blood borne pathogens
disease causing organisms that are transmitted through contact with infected blood or other bodily fluids
chain of infection
conditions that all must be present for infection to occur
chronic infection
an infection of long duration
communicable disease
a condition caused by an infection that can be from person to person or through contact with bodily fluids
direct contact
touching or contact with a patients blood or saliva
droplet infection
infection that occurs through mucosal surfaces of the eyes, nose, and mouth
immunity
the ability of the body to resist infections and diseases through specific defenses, either innate or acquired.
indirect contact
touching or contact with contaminated surfaces or objects, which can transfer pathogens to an individual.
infection control
policies and practices designed to prevent the spread of infections in healthcare settings and to protect both patients and healthcare workers.
infection prevention
ultimate goal of all infection control procedures and policies
infectious disease
disease that is communicable
inherited immunity
immunity that is present at birth
latent infection
persistent infection that is not actively causing disease but can reactivate, “comes and goes”
naturally acquired immunity
immunity that occurs when a person has contacted an infectious agent and develops antibodies against it.
occupational exposure
any reasonably anticipated skin, eye, or mucous membrane contact or percutaneous injury involving blood or ant other potentially infectious materials
OSHA blood-borne pathogens (BBP) standards
guidelines designed to protect employees against occupational exposure to bloodborne pathogens
pathogens
microorganisms, such as bacteria or viruses, that can cause disease.
permucosal
contact with mucous membranes, such as eyes or mouth
personal protective equipment (PPE)
items such as protective clothing, masks, gloves, eyewear, used to protect employees
standard precaution
standard of care designed to protect healthcare workers from pathogens that can be spread by blood or any other bodily fluids via exertion or secretion; expands on the concepts of universal precautions
universal precautions
guidelines based on treatment all human blood and bodily fluids (also saliva) as if they were infectious
virulence
strengths of pathogens ability to cause disease or infection, also known as pathogenicity.
Chain of Infection
Infectious agent
Reservoir
Portal of exit
Mode of transmission
Portal of entry
Susceptible host
What is an infectious agent?
It is a pathogen (a microorganism that causes disease), these pathogens can be/are bacteria, virus, fungus, parasite, prion. They must be virulent to cause a serious disease.
what is a reservoir?
a place where the pathogen can live and reproduce. these places can be in a human, animal, food, water, bioburden (the total number of live microorganisms present on or in a product, such as a medical device or pharmaceutical, before it is sterilized), contaminated surfaces.
what is portal of entry?
The route in which how a pathogen enters into a body. ways of entry can be through being airborne, blood-borne, contact with mucous membranes, or breaks in the skin.
What is a susceptible host?
A person who is at risk of infection due to factors such as weakened immune systems, age, underlying health conditions, chronically fatigued, or under extreme stress. Susceptible hosts are more likely to become infected when exposed to pathogens.
What is mode of transmission?
The way in which a pathogen is spread from one host to another. This includes direct contact, droplets, airborne particles, or vectors such as insects.
what is portal of exit?
The route by which a pathogen leaves the host body, such as through respiratory secretions, blood, or other bodily fluids. This exit is essential for the spread of infection to new hosts.
Types of infection
Acute infection: Symptoms are often quite severe and appear soon after the initial infection occurs
Chronic infection: present for a long period
Latent infection: Persistent infection in which symptoms come and go (e.g., cold sores)
Opportunistic infection: Caused by normally nonpathogenic organisms; occurs in individuals whose resistance is decreased or compromised
Modes of disease transmission
Direct transmission: Direct contact with the infectious lesion or infected body fluids (e.g., blood, saliva, semen, vaginal secretions)
Indirect transmission: Transfer of organisms to a susceptible person through, for example, the handling of contaminated instruments or touching of contaminated surfaces and then touching the face, eyes, or mouth
Airborne transmission: Known as droplet infection, involves spread of disease through droplets of moisture containing bacteria or viruses
Aerosols, sprays, and spatter: Contain saliva, blood, and microorganisms and are created with the use of the high-speed handpiece, air-water syringe, and ultrasonic scaler during dental procedures
Mists: Droplet particles larger than those in aerosol spray
Spatter: Large droplet particles contaminated with blood, saliva, and other debris
Happens during a dental procedure when the mucosa (mouth or eyes) or nonintact skin is splashed with blood or blood-contaminated saliva
Other modes of transmission
Parenteral transmission: Needle stick injuries, human bites, cuts, abrasions, or any break in the skin
Blood-borne transmission: Involves direct or indirect contact with blood and other body fluids
Food and water transmission: Contaminated food not cooked or refrigerated properly or water that has been contaminated with human or animal fecal material is consumed
Fecal-oral transmission: NOT handwashing after use of the toilet
The different types of immunity
Communicable disease: is one that can be transmitted from one person to another or by contact with the body fluids from another person
Inherited immunity: is present at birth
Acquired immunity: is developed over a person’s lifetime
Naturally acquired immunity: occurs when a person has contracted and is recovering from a disease
Active immunity: body fighting infection, forms antibodies
Passive immunity: fetus receives antibodies
Artificially acquired immunity: Example: Hep B vaccination, your body will develop antibodies through exposure to a vaccine.
Disease transmission in the dental office
Patient to dental team
Dental team to patient
Patient to patient
Dental office to community (including dental team’s family)
Community to dental office to patient
Disease transmission in the dental office: patient to dental team. Explain how it occurs and what you can do to prevent it.
Direct contact: touch of the patient’s blood or saliva
Droplet infection occurs through mucosal surfaces of the eyes, nose, and mouth. It can occur when the dental-team member inhales aerosol generated by the dental handpiece or air-water syringe
indirect contact: touch a contaminated surface or instrument
Ways to prevent it is by using gloves, handwashing, masks, rubber dams, and patient mouth rinses
Disease transmission in the dental office: dental team to patient. Explain how it occurs and what you can do to prevent it.
Very unlikely to happen
Can result if the dental team member has lesions on the hands, or if the hands are cut while in the patient’s mouth, permitting the transfer of microorganisms
Infection control measures that help to prevent team-to-patient transmission include:
Masks
Gloves
Handwashing
Immunization
Disease transmission in the dental office: patient to patient. Explain how it occurs and what you can do to prevent it.
No cases documented in dentistry
Contamination from instruments used on one patient must be transferred to another patient
Infection control measures that can prevent patient-to-patient transmission include:
Instrument sterilization
Surface barriers
Handwashing
Gloves
Use of sterile instruments
Dental office to community, how can contamination be spread to the community?
Microorganisms can leave the dental office and enter the community in a variety of ways
Contaminated impressions sent to the dental lab
Contaminated equipment sent out for repair
Transportation of microorganisms out of the office on the dental team’s clothing or hair
The following measures can prevent this type of disease transmission:
Handwashing
Changing clothes before leaving the office
Disinfecting impressions and contaminated equipment before such items leave the office
Community to dental office to patient. how can the contamination be spread?
Microorganisms enter the dental office through the municipal water that supplies the dental unit
Waterborne organisms colonize the inside of the dental unit waterlines and form biofilm
As water flows through the handpiece, air-water syringe, and ultrasonic scaler, a patient could swallow contaminated water
The role and responsibility of the CDC and OSHA in infection control
Federal agencies that play important roles in infection control for dentistry:
The Centers for Disease Control and Prevention (CDC)
The Occupational Safety and Health Administration (OSHA)
The CDC is not a regulatory agency, it establishes a standard of care for the dental profession
OSHA is a regulatory agency, it protect the health of employees. As a dental assistant, it is imperative to follow all of OSHA’s guidelines and recommendations
CDC ranks of evidence
Category IA
Category IB
Category IC
Category II
Unresolved issue
OSHA Blood-Borne Pathogens Standard (BBP)
The most important infection control law in dentistry!
Designed to protect employees against occupational exposure to blood-borne pathogens, such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV)
Employers are required to protect their employees from exposure to blood and other potentially infectious materials (OPIM) in the workplace and to provide proper care to the employee if an exposure should occur
The BBP applies to any type of facility in which employees might be exposed to blood and/or other body fluids, which include:
Dental and medical offices
Hospitals
Funeral homes
Emergency medical services
Nursing homes
OSHA requires that a copy of the BBP be present in every dental office and clinic
Standard and Universal Precautions
Universal Precautions are based on the concept that all human blood and body fluids (including saliva) are to be treated as if known to be infected with one of the blood-borne diseases, HBV, HCV, or HIV
The CDC expanded the concept and changed the term to Standard Precautions
Standard Precautions apply to contact with
blood,
all body fluids,
non intact skin
mucous membranes
Hepatitis B Immunization
OSHA requires the dentist to offer the hepatitis B virus (HBV) vaccination series to all employees whose jobs include category I and II tasks
Vaccine must be offered within 10 days of employment
The dentist/employer must obtain proof from the physician who administered the vaccination
Employees have the right to refuse the HBV vaccine; however, they must sign an informed refusal form that is kept on file in the office
The vaccine is administered in a series of three injections
Most common vaccination schedule is 0, 1, and 6 months
The preferred injection site is in the deltoid muscle (on the arm)
Postvaccine Testing
Between 1 to 2 months after the series has been completed, a blood test should be performed to ensure that the individual has developed immunity.
Employee Medical Records
The dentist/employer must keep a confidential medical record for each employee
These records are confidential and must be stored in a locked file
The employer must keep these records for 30 years
Preventing Needle Sticks
Never recap used needles by using both hands or any other technique that involves directing the point of a needle toward any part of the body
Always use the single-handed scoop technique or some type of safety device
Hand Hygiene: Handwashing Guidelines
Wash your hands each time before you put on gloves and immediately after you remove gloves
Wash your hands when you inadvertently touch contaminated objects or surfaces while barehanded
Always use liquid soap during handwashing
Bar soap should never be used because it may transmit contamination
For most routine dental procedures, such as examinations and nonsurgical procedures, an antimicrobial soap can be used
For surgical procedures, you should use a germicidal surgical scrub product
Dry hands well before donning gloves
Personal Protective Equipment (PPE)
OSHA requires the employer to provide employees with the appropriate PPE without charge to the employee
Examples of PPE
Protective clothing
Surgical masks
Face shields
Protective eyewear
Disposable patient-treatment gloves
Heavy-duty utility gloves
Handling Contaminated Laundry
Protective clothing may be laundered in the office
Contaminated linens that are removed from the office for laundering should be placed in a leakproof bag with a biohazard label or an appropriately color-coded label
Guidelines for the Use of Gloves
All gloves used in patient care are a single use
These gloves may not be washed, disinfected, or sterilized; however, they may be rinsed with water to remove excess powder
Latex, vinyl, or other disposable medical-quality gloves may be used for patient examinations and dental procedures
Torn or damaged gloves must be replaced immediately
Do not wear jewelry under gloves
Change gloves frequently
Remove contaminated gloves before leaving the chairside during patient care and replace them with new gloves before returning to patient care
Hands must be washed after glove removal and before regloving
Overgloves
Also known as food handler gloves; are made of lightweight, inexpensive clear plastic
These may be worn over contaminated treatment gloves (overgloving) to prevent the contamination of clean objects handled during treatment
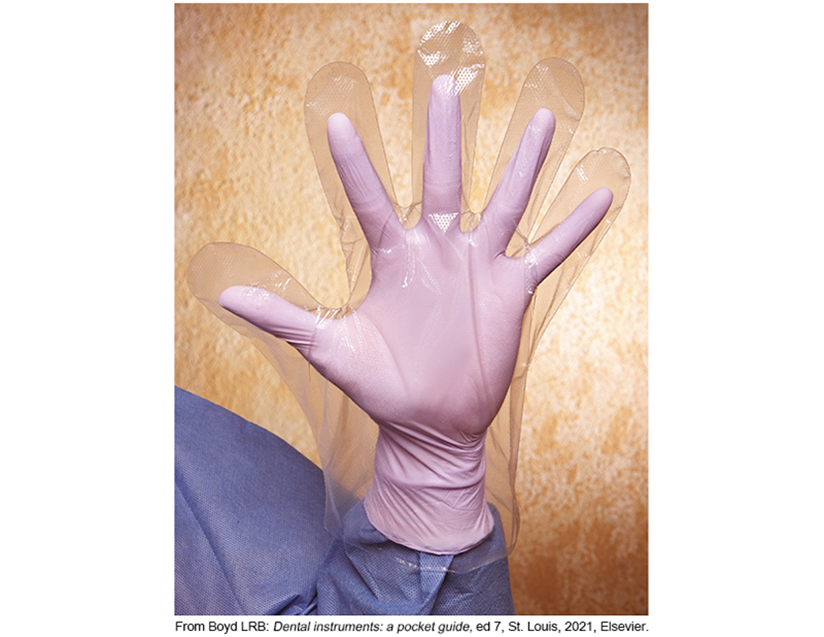
Guidelines for Use of Overgloves
Overgloves are not acceptable alone as a hand barrier or for intraoral procedures
Overgloves must be worn carefully to avoid contamination during handling with contaminated procedure gloves
Overgloves are donned before the secondary procedure is performed and removed before the patient treatment that was in progress is resumed
Overgloves are discarded after a single use
Sterile Surgical Gloves
Sterile gloves should be worn for invasive procedures involving the cutting of bone or significant amounts of blood or saliva, such as oral surgery or periodontal treatment
Provided in Prepackage form
Utility Gloves
Utility gloves are not used for direct patient care
Utility gloves must be worn:
When the treatment room is being cleaned and disinfected between patients
While contaminated instruments are being cleaned or handled
For surface cleaning and disinfection
Utility gloves may be washed, disinfected, or sterilized and reused
Used utility gloves must be considered contaminated and handled appropriately until they have been properly disinfected or sterilized
Are utility gloves used when contaminated instruments are prepared for sterilization
yes
Maintaining Infection Control While Gloved
During a dental procedure, it may be necessary to touch surfaces or objects such as drawer handles and material containers
If you touch these objects with a gloved hand, both the surface and glove become contaminated
To minimize the possibility of cross-contamination, use an overglove when it is necessary to touch a surface
Computer keyboard with a smooth surface allows for effective cleaning and disinfection, yes or no
Yes
are disposable sleeve used for high-tech devices like the ipad or remotes
Yes
what is irritant dermitits?
A skin condition caused by contact with irritants, leading to inflammation, redness, and discomfort. It can occur from exposure to chemicals, soaps, or materials without proper protection.
Type IV (4) Allergic Reaction
The most common type of latex allergy
Is a delayed contact reaction and involves the immune system
It may take as long as 48 or 72 hours for the red, itchy rash to appear
Reactions are limited to the areas of contact and do not involve the entire body. Caused by chemicals the permeate the gloves irritating the skin.
An immune response is produced by the chemicals that are used to process the latex used in manufacturing the gloves, not by the proteins in the latex
Type I Allergic Reaction
Most serious type of latex allergy; can result in death
Anaphylaxis is the most severe form of immediate allergy reaction, death can result from closure of the airway caused by swelling
Waste Management in the Dental Office
Dental practices are subject to a wide variety of federal, state, and local regulations concerning waste management issues
The Environmental Protection Agency (EPA):
1. Do not categorize saliva or saliva soaked items as infectious was.1
2. CDC guidelines and OSHA regulations consider saliva in dentistry a potentially infectious body fluid
Classification of Waste
1. General waste
All nonhazardous, nonregulated waste should be discarded in covered containers
Examples include disposable paper towels, paper mixing pads, and empty food container
2. Contaminated waste
Waste that has had contact with blood or other body fluids
Examples include used barriers and patient napkins
3. Hazardous waste
Poses a risk to human beings and the environment
Toxic chemicals and materials are hazardous waste
Examples include scrap amalgam, spent fixer solution, and lead foil from x-ray film packets
4. Infectious or regulated waste (biohazard)
Contaminated waste that is capable of transmitting an infectious disease
Some items like extracted teeth with amalgam restoration may be both hazardous waste (because of the amalgam) and infectious waste (because of the blood)
Most dental offices are exposed to the following types of infectious waste:
Blood and blood-soaked materials
Pathologic waste
Sharps
Additional Infection Control Practices
OSHA Blood-Borne Pathogens Standard
Never eat, drink, smoke, apply cosmetics or lip balm, or handle contact lenses in any area of the dental office where contamination is possible, such as the dental treatment rooms, dental laboratory, sterilization area, or the area for the processing of x-rays
Never store food or drink in a refrigerator that contains any potentially contaminated items
You can minimize the amount of splash and spatter contamination produced during dental procedures with the skillful use of a dental dam and high-volume evacuation
CDC Guidelines: Special Considerations
Saliva ejectors
Do not advise patients to close their lips tightly around the tip of the saliva ejector to evacuate oral fluids
Many patients have become accustomed to closing their lips around the suction
CDC Guidelines: Preprocedural Mouth Rinses
Intended to reduce the number of microorganisms released in the form of aerosol or spatter
Can decrease the number of microorganisms introduced into the patient’s bloodstream during invasive dental procedures
CDC Guidelines: Mycobacterium tuberculosis (TB)
For patients with known or suspected active TB, the CDC recommends that elective dental treatment be delayed until the patient is noninfectious